endocrin ii lab med
1/40
Earn XP
Description and Tags
endocrin ii lab med
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
41 Terms
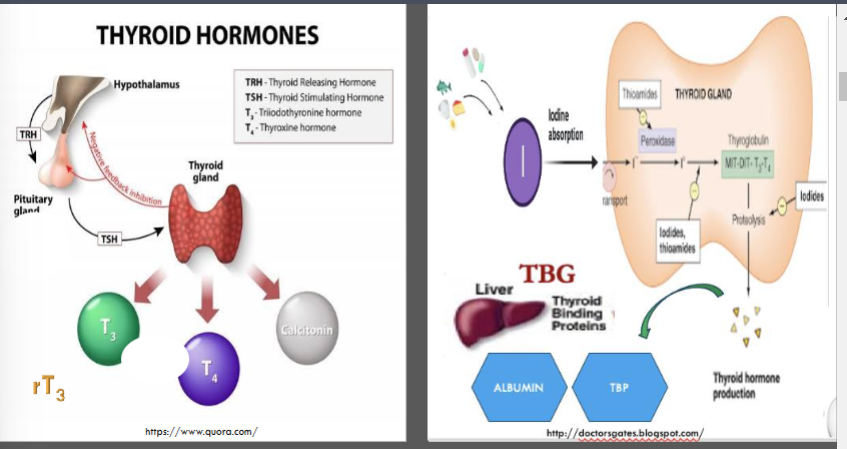
thyroid function
negative feedback
trh comes from hypo then stimulatses the tsh to release t3,t4,calcitonin
iodine is important to release thyroid hormones, it comes from salt , otherwise can cause goiter
carries thyroids to blood
albumin
tbp
and tbg
what does the thyroid gland test?
How is ithe feedback regulated?
what does the hypothalamus hormone come from and stimulate?
What about tsh?
what are the 3 hormones relase?
What mineral is required for thyoird hormone release? where does it come from?
what does thyroglobulin do
what are the three important binding proteins in the blood?
t3 is more active than t4 t4 is in the thyroid and t3 is in the periphery once iodine is removed
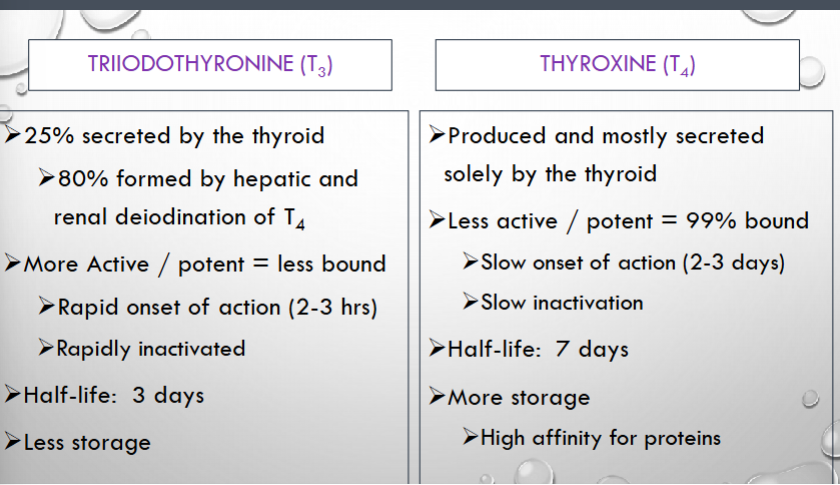
how is t3 formed? in what form is it more active? what is the half-life?
how is t4 secreted? is it more bound or potent? what is the half-life and what does this mean for storage?
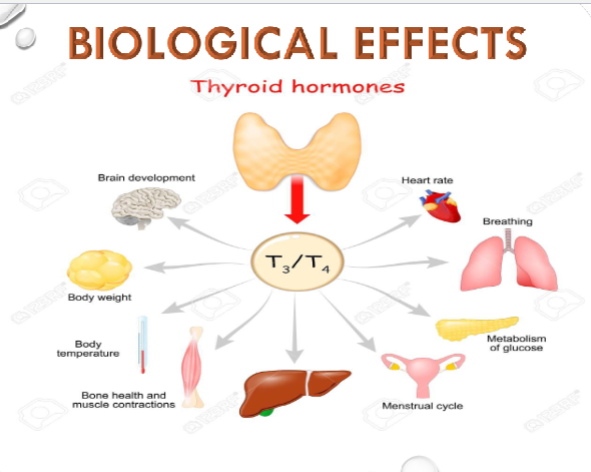
what are the 9 functions of thyroids?
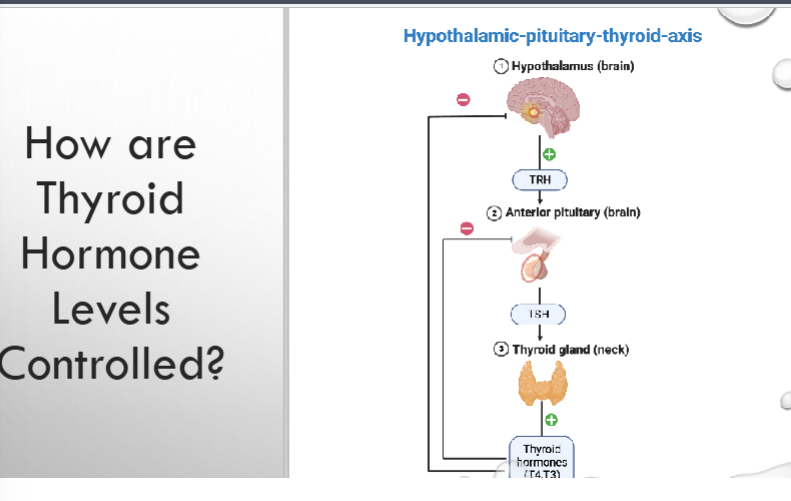
TRH- controlled by negative feedback
the more thyroid hormone relationship the less _____ is release, they have an inverse relationship
hyper; metabolism going up, quicker metabolism, losing weight quickly
hypo: cant lose weight, hair loss.
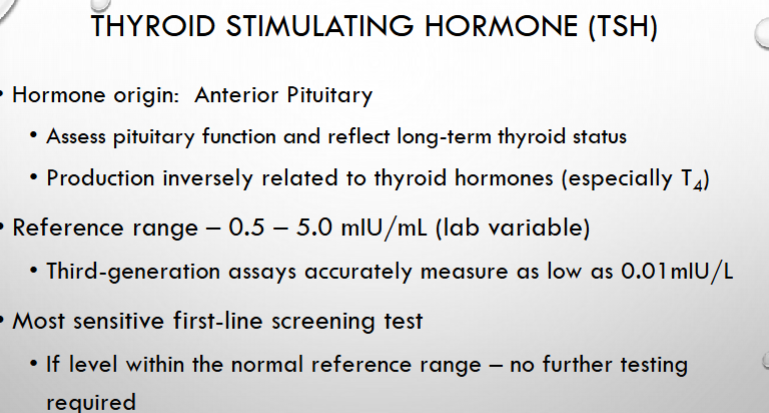
pituitary is the first test: to test for tsh
these are controlled by TBG (how many sites do they have available)
NO* but tsh does tell you if the function is normal
hyperthyroid vs hypo?
what is the first test to run? what about further tests? what are these tests controlled by?c
can they be used as the SOLE measure of thyroid function? ***
note this is a special chemistry panel
nah this is a good screening and testing tool
low-HYPER low-hyper-check
• Use
• Screening
• Therapeutic monitoring
• Hypothyroidism – normalization of TSH within age-specific reference range =
effectiveness of thyroid hormone replacement
• Essential for monitoring suppression therapy in patients with a TSH-responsive
thyroid tumor
• If, TSH is outside of the reference range = a free T4 is obtained
where does tsh come from?
what does it assess the function of?
what the TSH a reference range?
is this test sensitive? is more testing required?
what are uses?
what occurs if tsh is low what could that be?
If tsh is high what should be obtained?
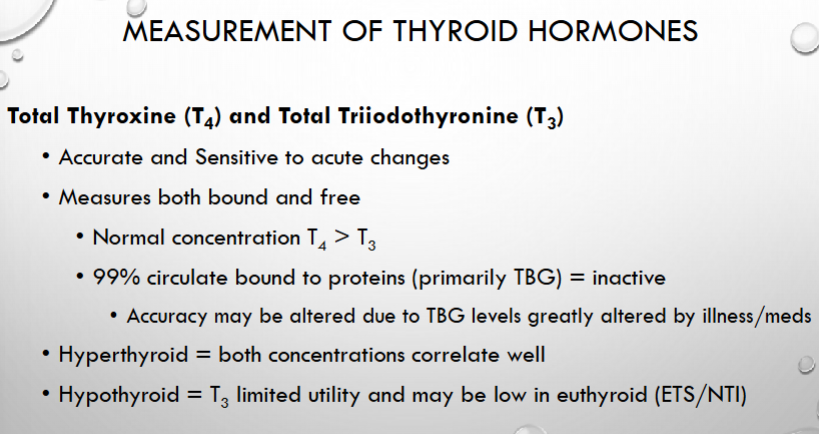
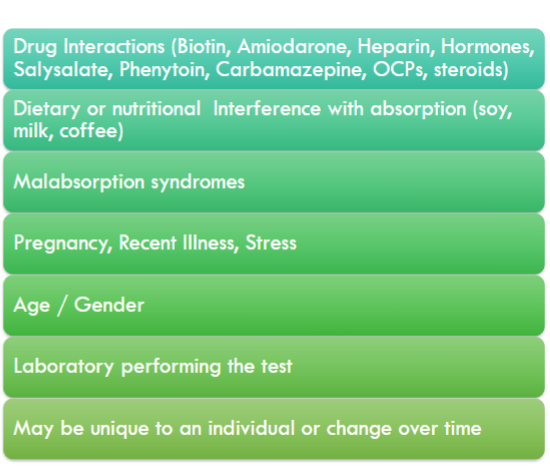
proteins: if affected like stress,illness,medications will affect the thyroglobulin protein level. tbg
hyper: tsh low, t4 and t3 high
hypo: tsh high t4 low t3 normal
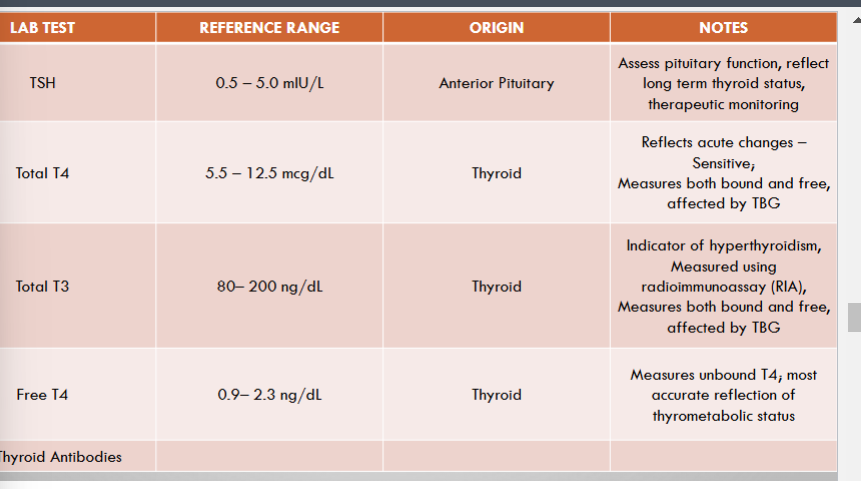
what does the total t4+t3 measure?
what is a normal total t4+t3ratio?
what can mess the total t4+t3 ratio up?
when can the hypo vs hyper thyroid levels be messed up?
what does the free t4/t3 help measure? why would this indicate thyroid status better?
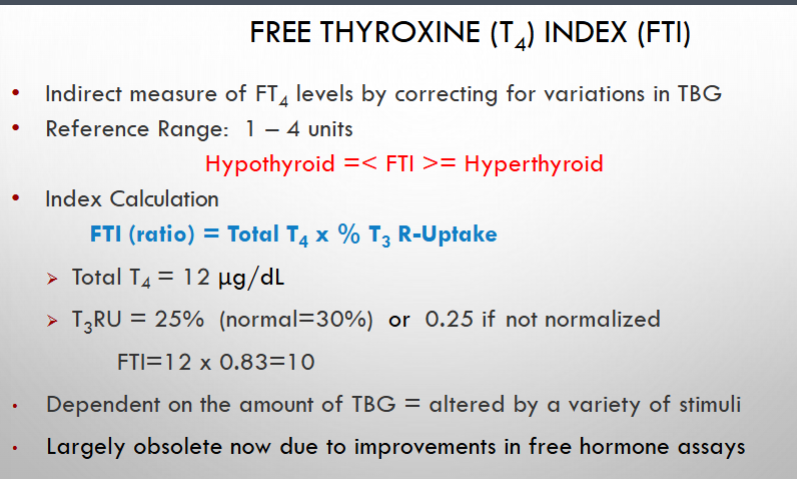
what is FT4/FTi for?
what is the reference range? what do they levels high or low indicate?
what does this depend on therefore may give you an erroneous result?
basically a t3 particle with some radioactive tracers
Value reported as % tracer bound to resin
• Varies inversely with the number of
available free TBG binding sites
• Number of free binding sites is determined
both by levels of binding protein and
endogenous hormone production
• Alterations: thyroid dz, pregnancy, kidney
dz, TBG excess/deficiency
• Rarely used due to improved FT4 assays
Reference Range 25-38%
High % = Hyperthyroid
Low % = Hypothyroid
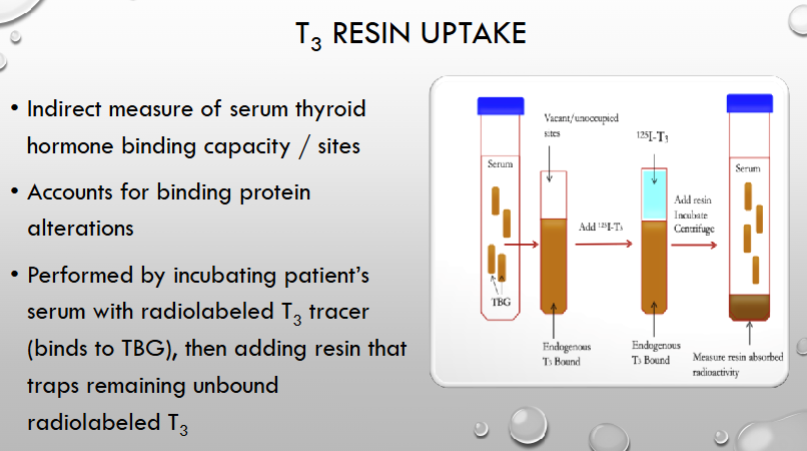
t3 resin uptake is an indirect measure of what?
what does it account for?
what is T3 percentage inversely proportional to?
what could cause an odd T3 resin Uptake besides thyroid issue?
what is the reference range for t3?
what would a high or low percentage indicated?
* Repeat TSH & FT4 in 6-8 wks after starting or changing therapy to check if its working
what two test would you want to repeat in 6-8 weeks and why?
can cause erroneous results; send them to endocrine
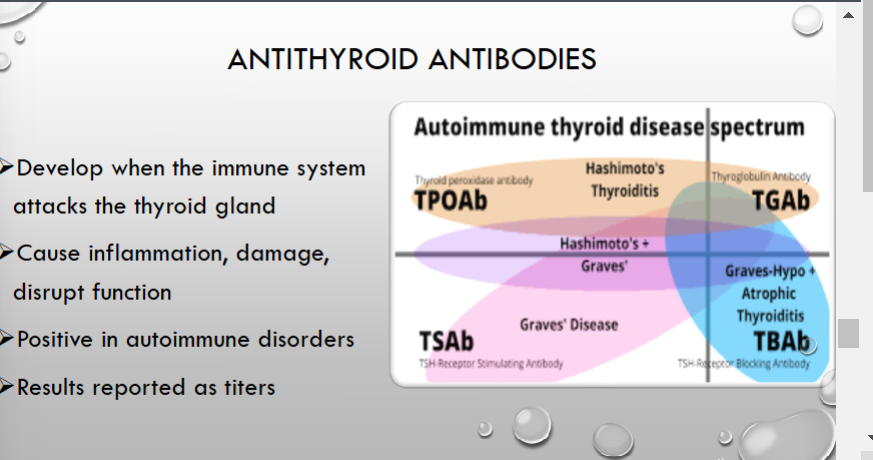
what are antithyroid antibodies? what can they cause? where would they be positive?
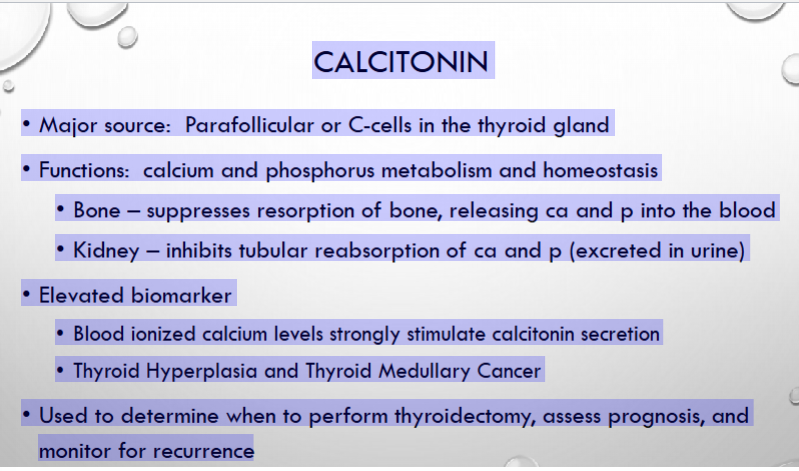
• Used to determine when to perform thyroidectomy______ if high a metastatic cancer occured or some was left behind, assess prognosis, and
monitor for recurrence
what is the source of calcitonin?
what main functions does calcitonin have in regards to minerals, bones, and kidneys?
what can an elevated biomarker indicate?
what can this be used to determine?
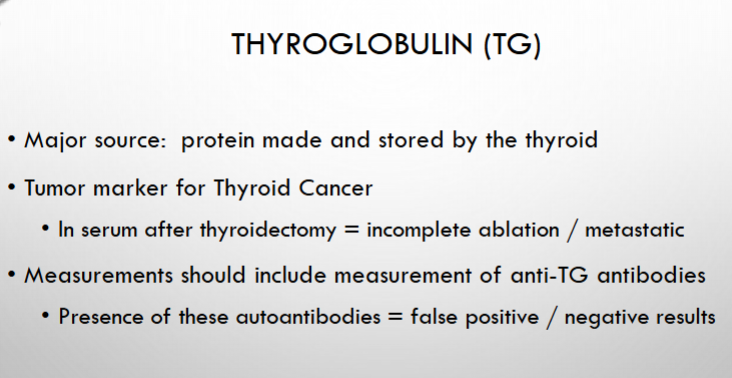
also run an antiglobulin test
thyroglobulin is a protein made and stored by the ________?
this is a good tumor marker for _____ and can be found after removal therefore indicating ________/______
what can throw it off so you should run?
Patient risk factors: autoimmune disease, contact with pets/animals, monoclonal Ab,
recent immunizations or transfusions
thyroid immunoassays are still very ideal: what 7 things can throw this off?
when should you suspect immunoassay interference?
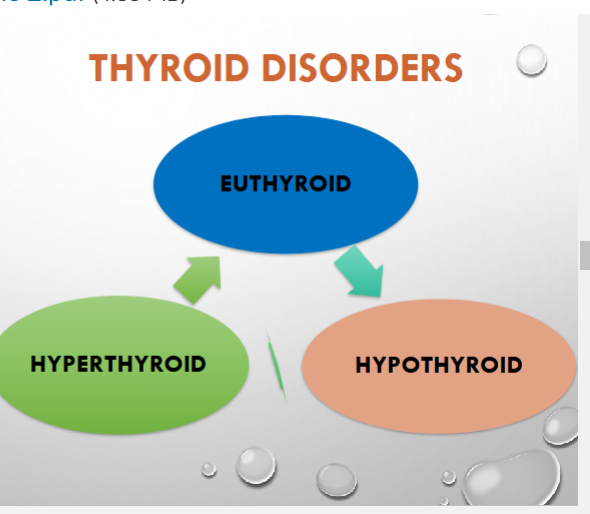
most common in women; euthyroid normal
what does euthyroid mean?
what levels of tsh and t3/t4 would you expect in the hyper vs hypthyroid?
if that doesnt work ft4!
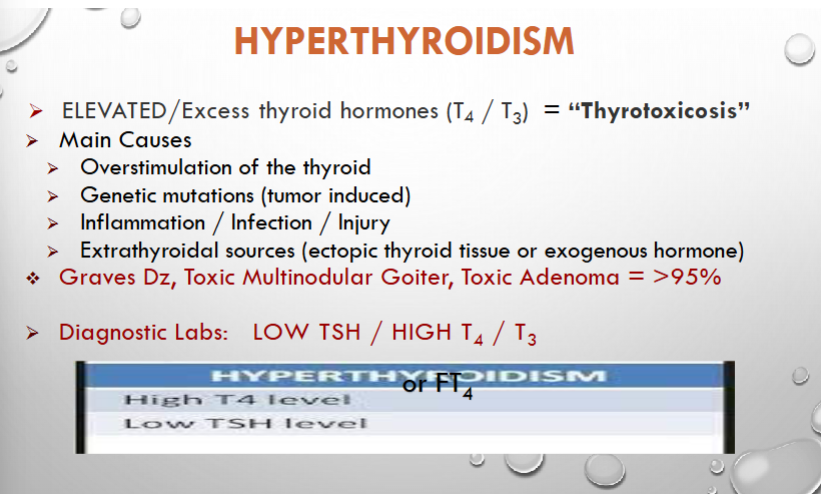
hyperthyroidism is aka _____? it is defined by the excess hormones______?
what are 4 main causes?
what are the main 3 dx:
what are the tests you do and would expect to find on them?
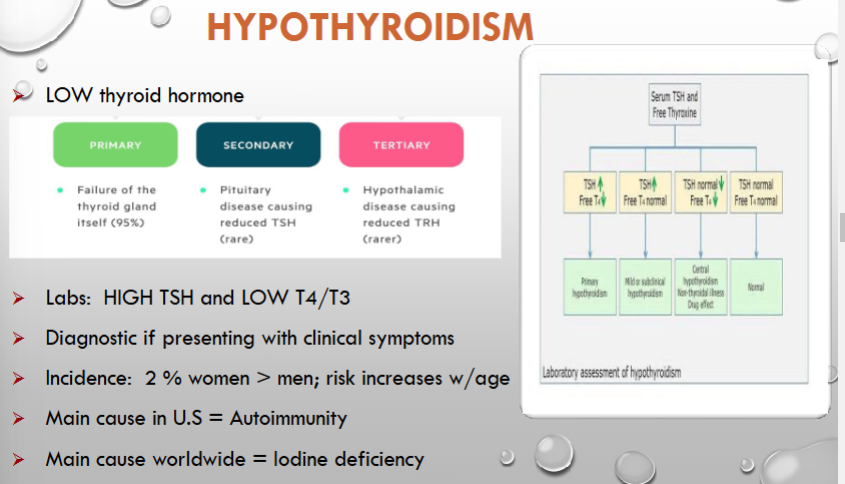
primary: always in the thyroid
labs+ clinical symptoms
trh,fsh, lh additionally?
what are the three types of hypothyroidism?
Primary vs Secondary vs Tertiary
Are symptoms in hypothyroidism diagnostic?
How do labs present in hypothyroidism?
what is the main cause in the us vs worldwide?
more common in what gender?
is now part of neonatal screening
what is cretinism?
when does it occur?
some can be sporadic or )______?
why should it be dx quickly?
what would you expect to be elevated for:
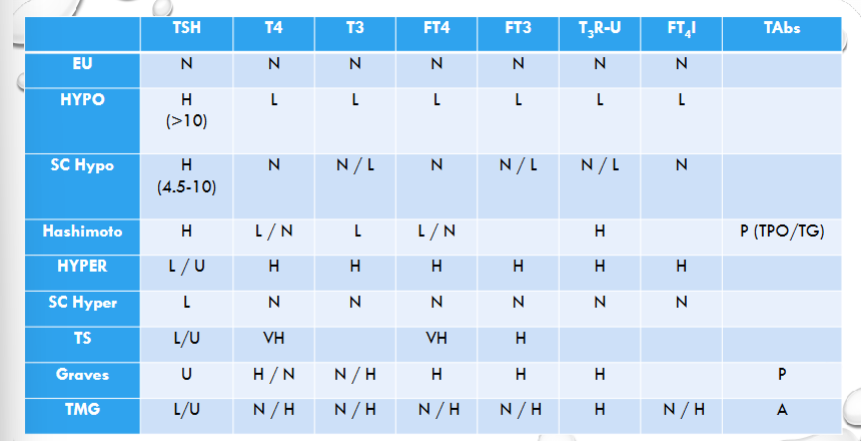
euthyroid: all normal levels
Hypothyroidism: TSH high (>10) everything else low
subclinical hypothyroidism: TSH high (4.5-10) everything low/normal
Hashimoto’s: (TSH high) everything else low + TPO/TG antibodies present
Hyperthyroidism: TSH low, everything else high
Subclinical hyperthyroidism: TSH low, everything else normal
Thyroiditis: TSH low/undetected, everything else VERY high
Graves disease: TSH undetected, everything else high with antibodies present
toxic multinodular goiter: TSH undetected everything else normal/high NO antibodies present
what would you expect to be elevated for
euthyroid ,Hypothyroidism, subclinical hypothyroidism
Hashimoto’s, hyperthyroidism, subclinical hyperthyroidism,
thyroiditis, graves disease, toxic multinodular goiter
increase that if they develop a problem if they have risk factors?
when should it be done? vs how often its done?
thyroid?
what are other thyroid tests ?
do US, then FNA, then biopsy
why would you do a fine needle aspiration?
why would you do a thyroid nodule biopsy?
cortisol=adrenal gland
aldosterone= renin angiotensin
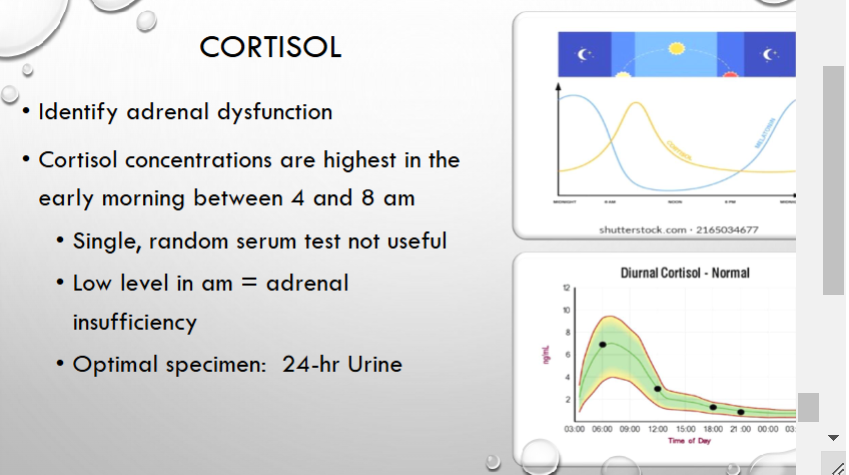
can go up and down throughout the day
if its decrease between 4-8 there’s probably an adrenal insufficiency
cortisol can identify what type of dysfunction?
when is it highest?
can it go up and down ?
what time would you want to measure cortisol
what is the optimal specimen?
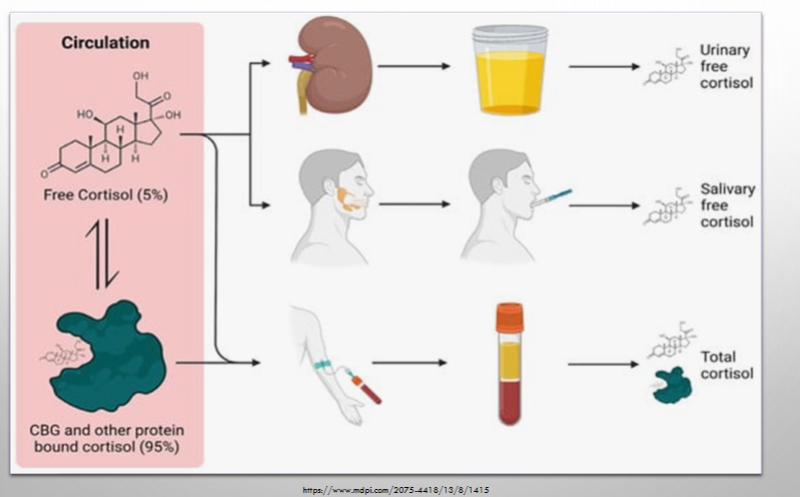
what are three types of cortisol test?
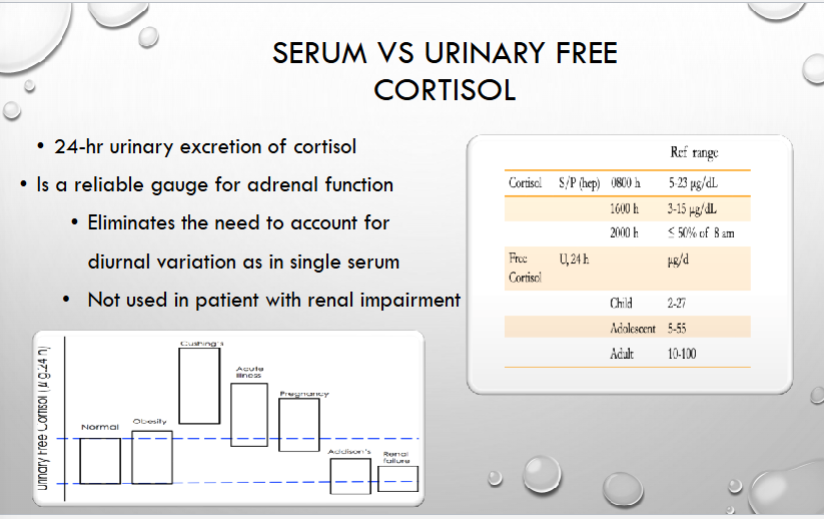
why is urinary cortisol better than serum cortisol?
what patient would you not use it in?
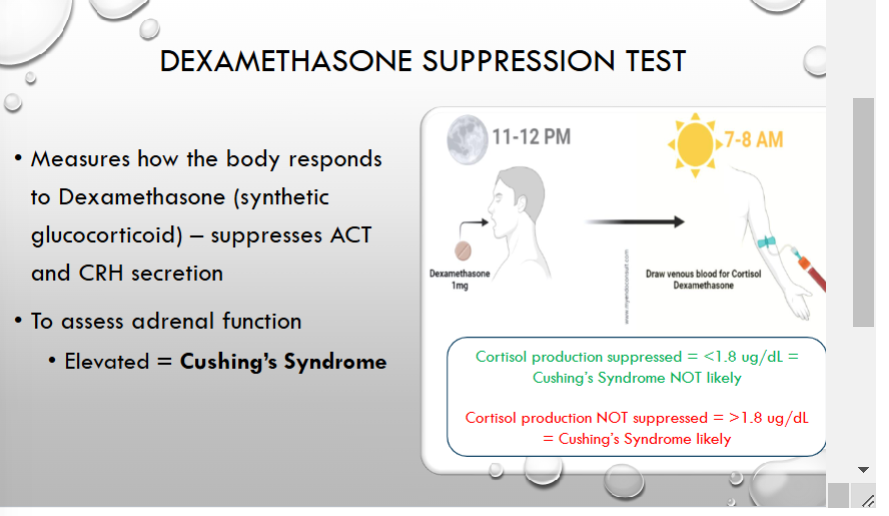
dexamethasone assess adrenal function, if elevated, greater than 1.8 then cushings dx is likely
Dexamethasone is a synthetic corticosteroid that mimics cortisol. Under normal circumstances, the body uses a negative feedback mechanism to control cortisol production. The hypothalamus releases corticotropin-releasing hormone (CRH), which signals the pituitary gland to produce adrenocorticotropic hormone (ACTH), stimulating the adrenal glands to release cortisol. When cortisol levels are high, this feedback loop should reduce CRH and ACTH, thereby lowering cortisol production.
Dexamethasone Suppression Test:
In a normal person:
If dexamethasone is given, it mimics cortisol and causes a decrease in CRH and ACTH production.
This leads to a reduction in the body's own cortisol production.
what is the dexamethasone suppression test?
what would an elevated dexamethasone test reuslt in?
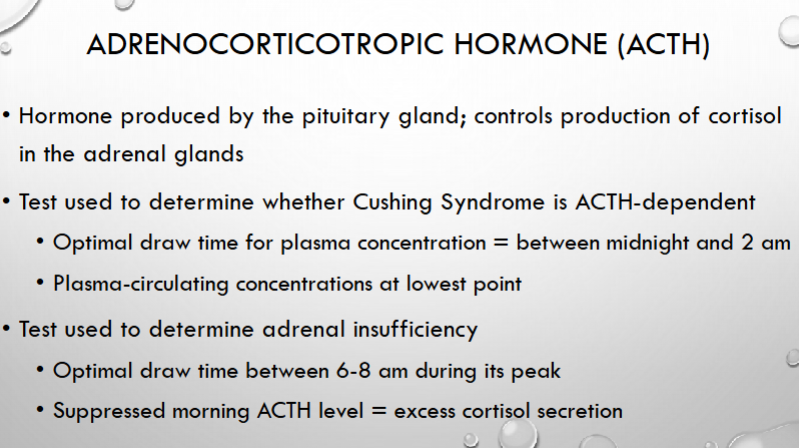
at lowest 12-2 so should be low not high; hence for cushings syndrome
at highest 6-8 so you should be testing the adrenal gland is working properly
what is ACTH produced by? what does it control in the adrenal gland?
what is it used to distinguish? when is the optimal draw time?
what is it used to determine?
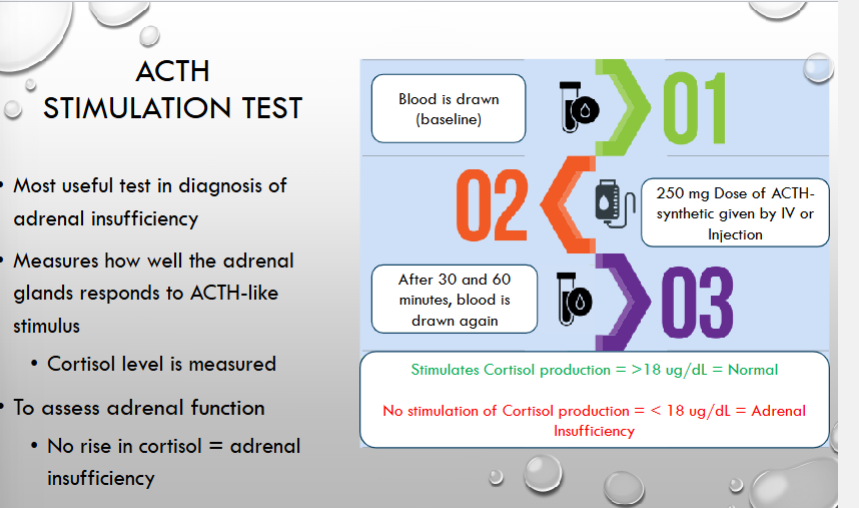
Stimulates Cortisol production = >18 ug/dL = Normal
No stimulation of Cortisol production = < 18 ug/dL = Adrenal
Insufficiency
Stimulates Cortisol production = >18 ug/dL = Normal
No stimulation of Cortisol production = < 18 ug/dL = Adrenal
Insufficiency
what is the most usefull test in dx of adrenal insufficiency?
what does it measure?
what does no rise in cortisol what does this indicate? what range would be evident of this?
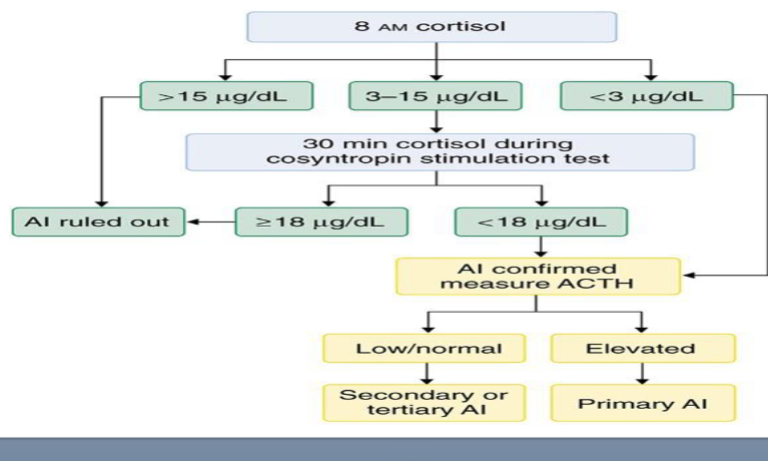
if you run the 8am Cortisol and it results in
15 ?
3-15?
< 3?
x: what is measured next and what if it results low or elevated?
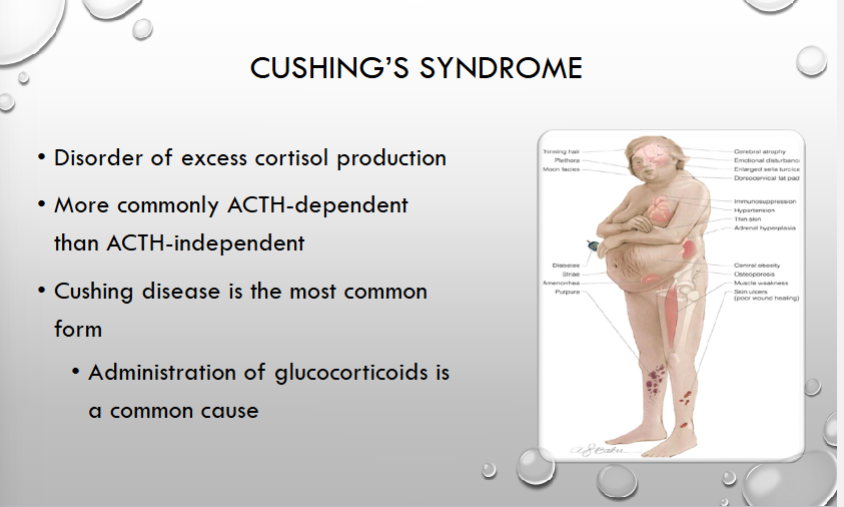
syndrome: usually due to steroids
cushings syndrome vs cushings disease?
acth dependent or independent?
what is the most common cause of the syndrome
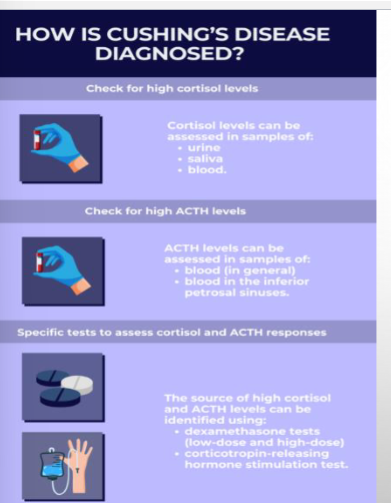
how do you dx cushings>
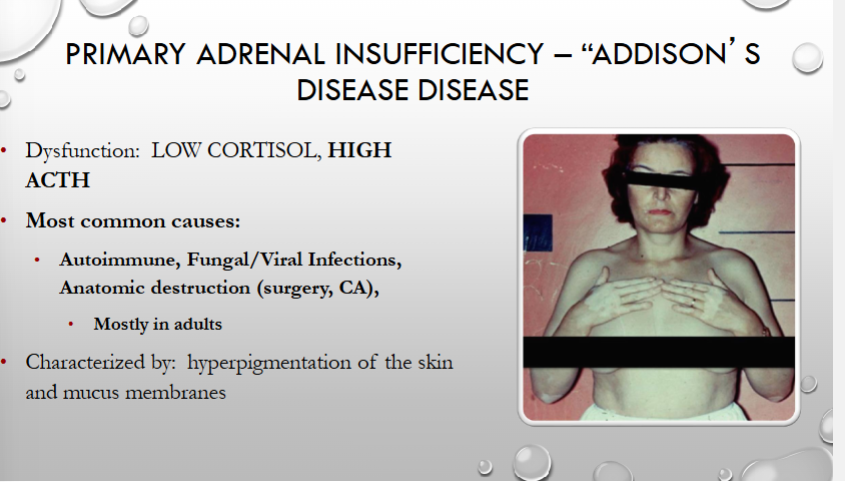
what is the primary adrenal insufficiency known as? what levels would be high or low?
what is the most common causes? what age group is it most likely to be found?
common symptoms
Dx: ☑ cortisol levels, ACTH levels, special test → ACTH stimulation test
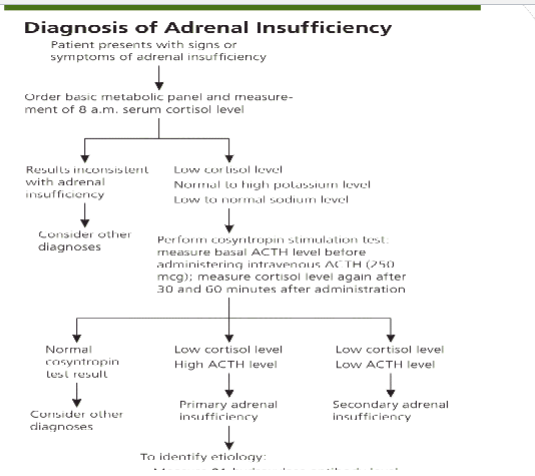
1° (adrenal): LOW 8 am serum cortisol → HIGH ACTH level & LOW cortisol after ACTH stimulation
2° (pituitary): LOW 8 am serum cortisol → LOW ACTH level & LOW cortisol after ACTH stimulation
how is adrenal insufficiency dx?
peein a lot and very thirsy, argining vasopression insufficieny
no releiveing thirst and manage out put
what is diabetus insipidus an dysfunction of?
is there a cure?
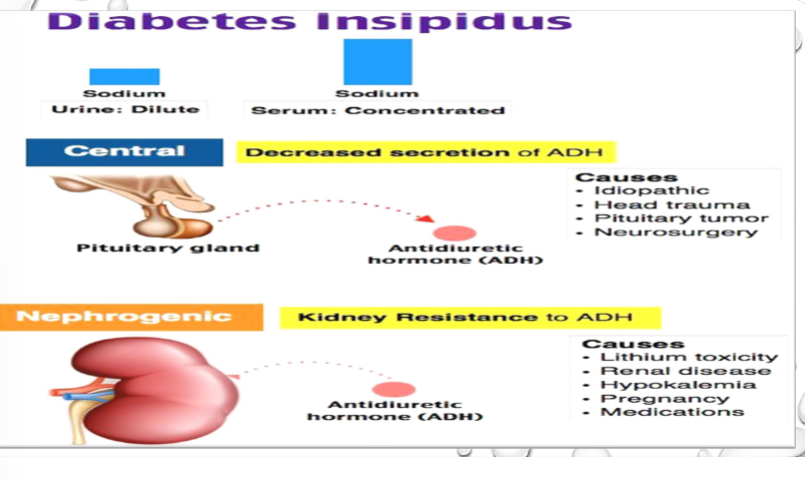
what is the difference between central and nephrogenic diabetes insipidus?
what are the different causes>
how would the urine vs serum present?
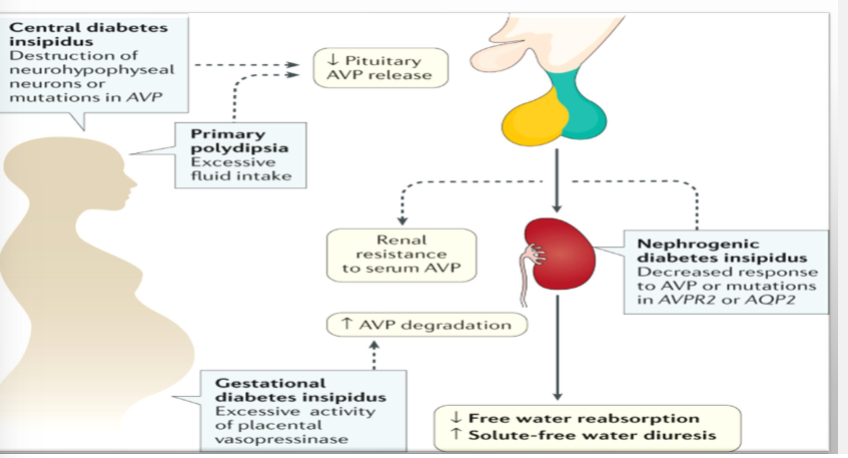
how can diabetes insipidus present in gestation?A
serum/plasma, adh test to distinguish between kidney and pituitarty gland
water deprivation tests, bun, electrolytes, osmolalit
what test should be run for di?
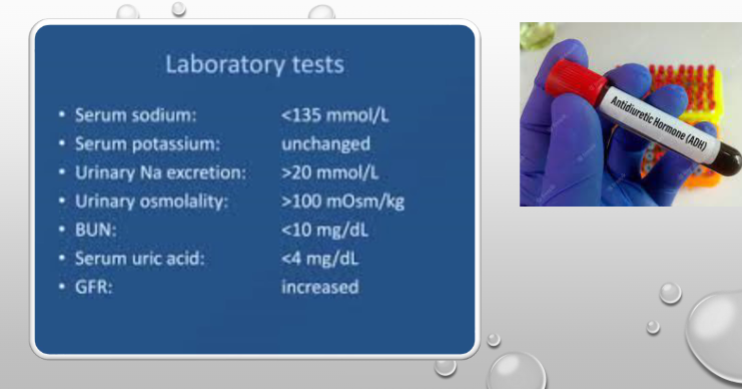
how would the lab tests show for DI?
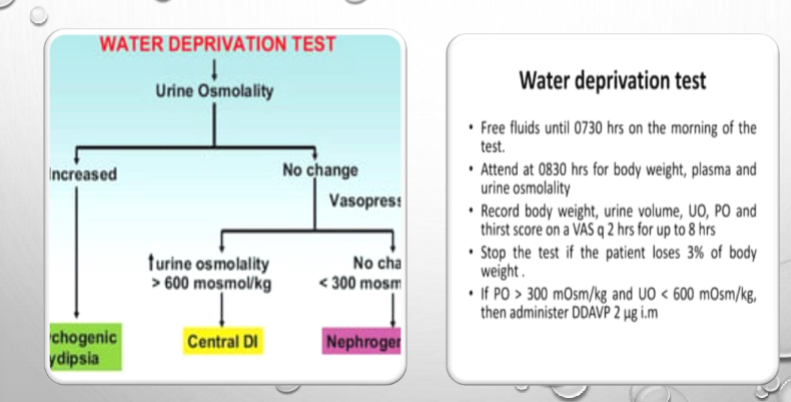
Decrease fluid intake if there is no change in urine osmolality, run a vasopressin challenge test
what does the water deprivation test do?
Increased?
no change? —> give them vasopressin and if the urine osmolality goes up? what if theres not change or it goes down?
which would be central or nephrogenic di?