CPCR
1/72
Earn XP
Description and Tags
CPR
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
73 Terms
What does CPCR stand for?
Cardiopulmonary cerebral resuscitation
What does RECOVER stand for?
Reassessment Campaign on Veterinary Resuscitation
What is RECOVERs aim? (3)
Improve outcomes for patients using evidence-based guidelines
Improve training for vet professionals
Improve return of spontaneous circulation (ROSC) and survival to discharge
% of ROSC using RECOVER
28-44
% of survive to discharge using RECOVER
3-10
When has cardiopulmonary arrest occurred? (8)
Mentation (unresponsive patient)
Changes in breathing
Altered MM colour
No pulse
Changes in HR or rhythm
Capnography (decreasing ETCO2)
Absence of bleeding
Pupillary dilation
How long should assess the unresponsive patient take?
Under 10 seconds
First steps if patient is unresponsive? (2)
Shake and shout
Call for help
Unresponsive patients and ABC exam
A - airway (obstruction?)
B - breathing (watch chest rise)
C - no longer check circulation as people misidentified pulse
What is basic life support (BLS)? (2)
Chest compressions
Ventilation
BLS - check compressions (3)
100-120 compressions per min
1:1 cycle
Allow chest to fully recoil
BLS - Ventilation
1 breath/6 seconds
BLS - Ventilitation and no. rescuers
single - can’t intubate, use tight fitting mask
multiple - intubate
Why compressions for 2 minutes? (4)
Maximises blood flow
takes one min for for compressions to reach best cariac output
only 1/3 of normal cardiac output
Every break = losses blood flow and never reach peak
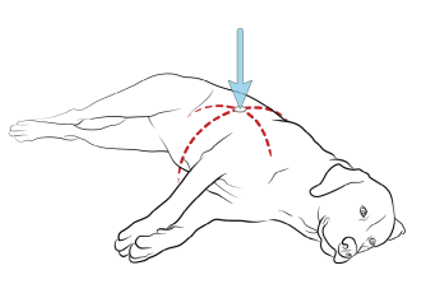
Chest compressions - standard round chest (3)
Place hands over the highest point of the chest
Utilises the thoracic pump mechanism
Compressions ½ to a 1/3 of chest width
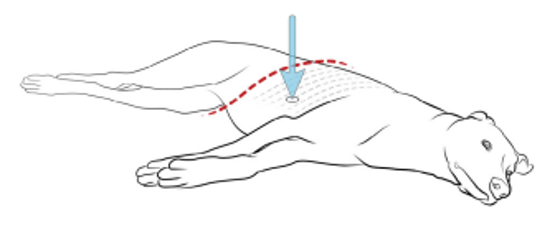
Chest compressions - keel chested (greyhounds) (3)
Place hands directly over the heart
Utilises the cardiac pump mechanism
Compressions ½ to a 1/3 of chest width
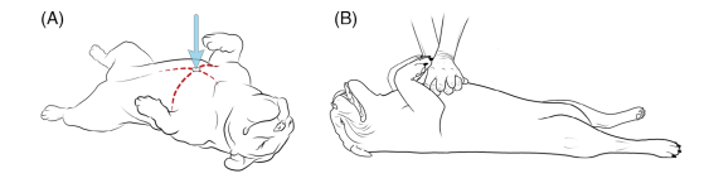
Chest compressions - wide-chested (bulldogs) (3)
Place hands over sternum
Patient in dorsal
Compressions ¼ chest depth
Chest compressions - small dog/cat (4)
Directly over heart, hold sternum in palm, brace dorsum with non-dominant hand
Use flat thumbs and fingers
Utilises the cardiac pump approach
Can use one hand over heart
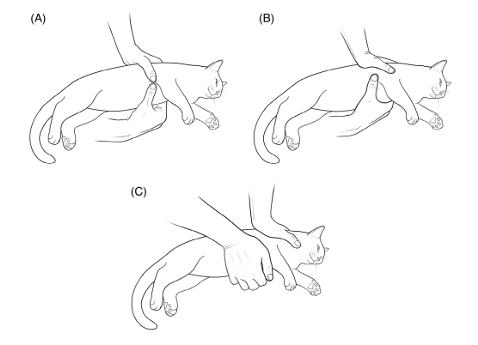
Chest compressions - small dog/cats notes (3)
10-15kg
Can use 2 thumb approach where you wrap hands around the whole animal
Do not use 2 hands - overcompression can damage heart
Chest compressions - hand position (3)
One over the other
Heel over heel
Hands interlocked

Chest compressions (3)
Shoulders over hands
Lock elbows
Use core and abdominal muscle and bend at the waist
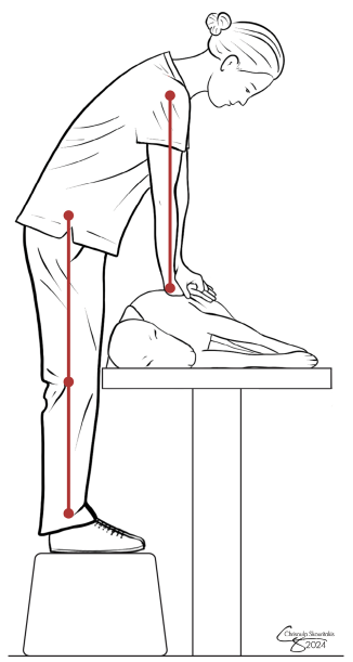
What if the table is too short? (4)
Use stool
Get on table
Drop table height
Put patient on floor
Why use interposed abdominal compressions? (2)
Increases return from caudal vena cave
Better blood flow and perfusion
When to use interposed abdominal compressions? (2)
Larger dogs, where capnograph isn’t reading well
Seesaw with other compressions
How to place ventilation? (2)
laryngoscope to ensure correct placement
capnography best indicator of placement
Ventilation timing (2)
1 breath every 6 seconds, 1 second inspiratory time
don’t over-ventilate
When would a tracheostomy be necessary?
If mouth/throat is blocked e.g. tennis ball
What does ALS stand for?
Advanced life support
When to start ASL?
Can be done same time as BLS if enough people
What does ALS consist of? (3)
monitor
IV access
reversals
What is involved in ALS monitoring? (2)
capnography
ECG
ALS monitoring - capnography (3)
monitors how effective chest compressions are
aim for ETCO2 >18mmHg
best indicator of ROSC
ALS monitoring - ECG (2)
diagnose an arrest rhythm
guides drug therapy
ALS IV Access (3)
IV access best – superior to IO
cephalic
jugular
ALS Access options (3)
intravenous
intraosseous
intra-tracheal
Drugs given through the trachea must be….
double the IV dose
What drugs are safe to give intra-tracheal? (5)
naloxone
atropine
vasopressin
epinephrine
lidocaine
NAVEL
Patient is under anaesthetia when CPCR is needed. What do we do first? (2)
turn of anaesthetic, flush oxygen, empty bag
administer reversal agents
What reverses opioids?
naloxone
What reverses Alpha-2?
atipamezole
What reverses benzodiazepines?
flumazenil
How quickly should BLS and ALS be performed?
2 minutes
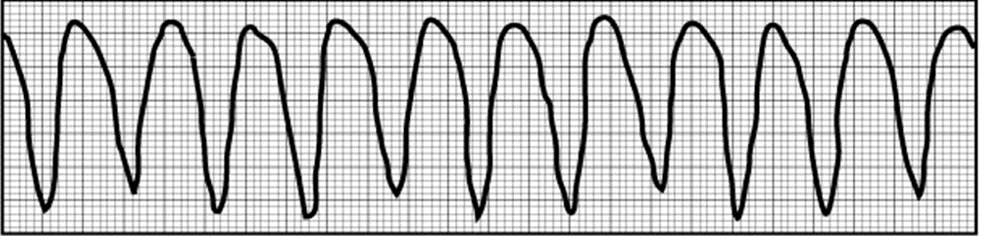
What are the two shockable rhythms?
pulseless ventricular tachycardia (pulseless VT)
ventricular fibrillation (VF)
Pulseless ventricular tachycardia (pulseless VT) (3)
no pulse
fast, rapid electrical activity
generates a very high HR >200
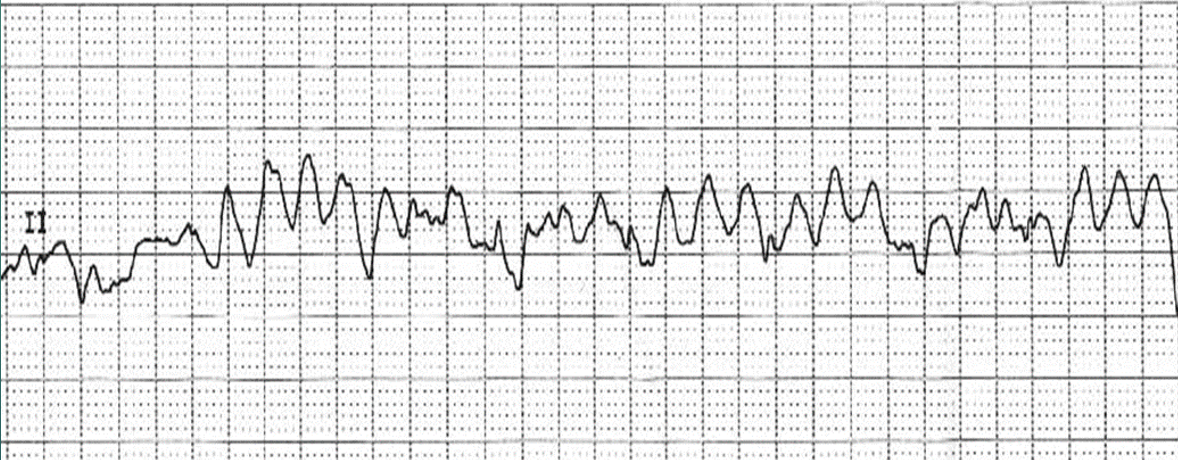
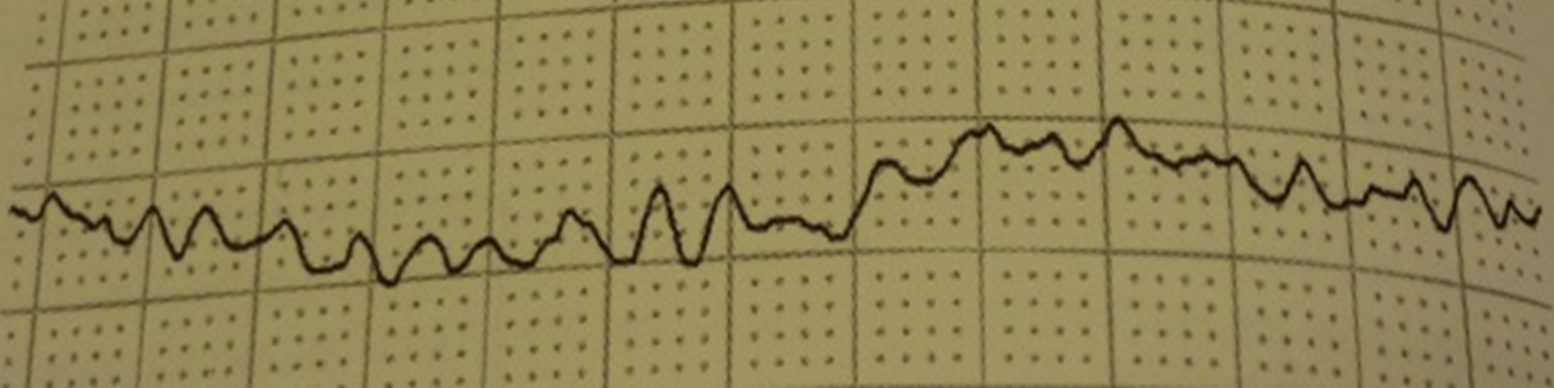
Ventricular fibrillation (VF) (4)
no pulse
heart muscle ‘quivering’
rapid, discordant electrical activity
no significant mechanical function or normal looking waveform
What are the two non-shockable rhythms?
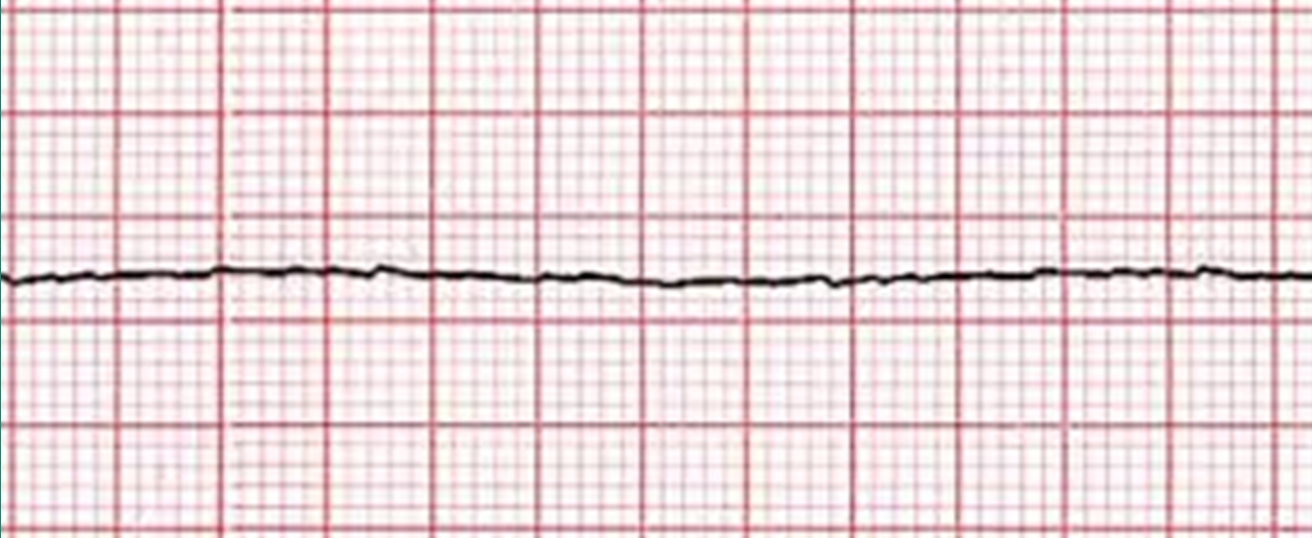
asystole
pulseless electrical activity (PEA)
Asystole (2)
no pulse, electrical or mechanical activity
flat line
Pulseless electrical activity (PEA) (3)
no pulse or mechanical activity
residual electrical activity
will see something on the waveform
No pulse shockable rhythm response (2)
defibrillator (electrical)
precordial thump (mechanical)
Defibrillator (2)
stops heart to ‘reset’ it
stops myocytes to allow it to beat normally
Precordial thump (2)
replacement for defibrillator
poor prognosis
Defibrillation positioning (2)
patient in dorsal
paddles on opposite sides of heart
Defibrillation technique (2)
don’t touch dog or table - shout ‘CLEAR’
use electrode gel on paddle
If first defibrillator shock doesn’t work…
double dose for all future shocks
Option for non-shockable rhythm
drug therapy
Drug therapy options
epinephrine (adrenaline)
vasopressin
atropine
Giving drug therapy…. (3)
use vasopressors to cause potent vasoconstriction
makes compressions more effective
stimulate alpha-1
Aim of drug therapy (3)
redirect blood flow from periphery to core
maximise blood flow to brain & heart
help BLS (excellent compressions only getting 30% normal CO)
Epinephrine (3)
catecholamine
non-specific
high dose epinephrine no longer recommended
may come back but don’t often make it to discharge
Epinephrine targets (3)
Α1 receptors – peripheral vasoconstriction
Β1 receptors – ↑ cardiac contractility and rate
Β2 receptors – vasodilation & bronchodilation
Most beneficial target for CPR
A1 receptor
Vasopressin (2)
antidiuretic hormone
very expensive
Vasopressin targets (3)
acts on the V1 receptor, so no beta effects
causes peripheral vasoconstriction
no effect on heart
Atropine (4)
anticholinergic
no harm in giving, but there is no strong evidence that it benefits
only give once
½ life 20-30mins
What does PCA stand for?
Post cardiac arrest algorithm
What is involved in PCA
monitoring
fluid therapy
oxygen supplementation
PCA - fluid therapy (2)
only if needed, only if reason for crash was hypokalaemia
monitor while on fluids
PCA - oxygen supplementation
achieve normal saturation
Importance of the team (3)
whole team approach
someone needs to be team leader
ideal world – 5-6 people
Team roles (6)
chest compressions (priority)
airway and IPPV
monitoring
IV access
record keeping and timer
runner (if enough people)
How to be prepared? (3)
ASA score – highlight any at risk patients undergoing anaesthesia
CPR Training & refreshers
crash box
Importance of crash trolley (3)
easy to access
not out of date
stocked and organised
Crash trolley contents (7)
IV catheters, bungs/T-ports
syringes & needles (some pre-prepared)
drugs and dose charts
ET tubes with tie + laryngoscope
fluids + giving sets
airway access, urinary catheter, suction
defibrillator