Patho ch 25 - cardiovascular system
1/122
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
123 Terms
main function of cardiovascular system
transport (oxygen, nutrients, waste products, electrolytes, hormones, immune substances)
also helps regulate temp via dilating/constricting vessels
this holds the heart in a fixed position and provides a barrier to infection and physical protection
pericardium
the outer layer of the pericardium is called the ___ and is attached to ___
fibrous pericardium
central tendon of diaphragm
inner layer of the pericardium is called ___ and has (one/multiple) layers
serous pericardium
multiple layers (visceral and parietal)
visceral pericardium
layer of the inner layer of the pericardium, aka epicardium (lines the heart)
epicardium
the visceral layer of the serous (inner) layer of the pericardium
contents of pericardial cavity
30-50 mL of serous fluid to minimize friction during contraction and relaxation of the heart
myocardium relies heavily on ___ for contraction
extracellular calcium ions
the sarcoplasmic reticulum of cardiac muscle isn’t as well defined as the SR of skeletal muscle (can’t store a lot of calcium)
this regulates the calcium-mediated contraction of cardiac muscle
tropomyosin-troponin complex
endocardium has how many layers
3 (innermost, middle, outermost)
innermost layer of the endocardium lines the (heart chambers/myocardium)
heart chambers
innermost layer of endocardium is made of (connective tissue/endothelial cells)
endothelial cells - continuous with the blood vessels that enter and leave the heart
middle layer of endocardium is made of (dense/irregular) connective tissue
dense - contains elastic fibers
outer layer of endocardium is continuous with the (heart chambers/myocardium)
myocardium
outer layer of endocardium is made of (dense/irregular) connective tissue
irregular - contains the conducting system and blood vessels
mitral valve location
between LA and LV
bicuspid
tricuspid valve location
between RA and RV
semilunar valves
aortic valve (between LV and aorta)
pulmonic valve (between RV and pulmonary artery)
___ provides structural support and isolating force for ___ impulse in the heart
fibrous skeleton; electrical
the fibrous skeleton provides support for the ___ and insertion for ___
attachment of valves
insertion of cardiac muscle
the period during which ventricles are contracting
systole
the period when ventricles are relaxed and filling with blood
diastole
end diastolic volume (definition and approximate amount)
the amount of blood present in the ventricles at the end of diastole (maximum fill)
~120 mL
isovolumetric period of ventricular systole begins with closure of (AV/SL) valves
AV valves
ejection period of ventricular systole occurs when the ___ pressure is greater than ___ pressure
ventricular > artery (causing SL valves to open)
S1 heart sound
closure of AV valves (beginning of isovolumetric ventricular systole)
normal to hear
ventricular diastole begins with closure of (AV/SL) valves
SL valves - no more blood leaving ventricles
S2 heart sound
closure of aortic and pulmonic valves (SL valves)
normal to hear
S3 heart sound
sound of ventricular filling (occurs during ventricular diastole)
normal to hear in young children, pregnant women; otherwise pathological (CHF)
describe what happens in the 3 thirds of ventricular diastole
rapid filling (S3 sound)
middle third - filling continues
last third - atrial contraction to complete filling (S4 sound)
S4 heart sound
sound of atrial contraction
pathological to hear - only in stiff, noncompliant ventricles (HTN, ventricular hypertrophy)
state of AV/SL valves in ventricular diastole (open/shut?)
AV valves are open
SL valves are shut
end diastolic volume
the amount of blood increase in the ventricles during diastole (~120 mL)
end systolic volume
amount of blood left in the ventricles after contraction (systole) (~50mL)
stroke volume
EDV - ESV (amount of blood ejected from the LV during each heartbeat)
ejection fraction
% of blood in the left ventricle that is ejected with each heartbeat (55-75%)
SV/EDV
test used to measure end diastolic volume
ECHO
average cardiac output in an adult
4-6 L/min
cardiac output calculation
SV x HR
cardiac reserve
the maximum % increase in CO that can be achieved above a person’s normal resting level
higher in younger adults, athletes (max 300-400%)
force of heart contraction is greatest when fibers are stretched to ___x their normal resting length
2.5
preload is largely determined by (arterial/venous) pressure
venous pressure/venous blood return
situations that increase preload (physiologic and pathologic)
exercise, excitement
hypervolemia (increased blood volume), regurgitation of heart valves, heart failure
exercise (increases/decreases) preload of the heart
increases - increases venous pressure to increase venous return to the heart
Frank-Starling Mechanism
the greater the volume of blood in the heart before contraction, the greater the volume of blood ejected from the heart (due to increased stroke volume)
HOWEVER - eventually the elastic limit of the heart is reached and causes thinning of heart walls (dilated cardiomyopathy) which is bad
afterload
the pressure the heart needs to generate to eject blood from the chamber
factors that increase afterload of the heart
aortic stenosis (increases resistance in the aorta)
HTN (increased total peripheral resistance of all vessels, especially the arteries)
the resistance the left ventricle must overcome to circulate blood: __
afterload
cardiac workload is increased with (increased/decreased) afterload
increased
valve regurgitation effect on preload
increases preload because blood flows back into the chamber (atria or ventricle) and increases the amount of blood that needs to be pumped out; then this happens again and again and causes a backup of blood in the chamber which increases the load on the heart
contractility refers to the changes of the force of heart contraction due to ___
calcium ions
positive inotropic effects
(affect contractility)
sympathetic stimulation (increases calcium availability)
oxygen (more ATP/energy)
negative inotropic effects
(affect contractility)
hypoxia - anaerobic respiration, lack of ATP (and buildup of lactic acid)
increased HR (increases/decreases) cardiac output
decreases - because there is less time available for ventricular (diastolic) filling
→ decreases SV and therefore CO
right heart is (pulmonary/systemic) circulation
pulmonary
left heart is (pulmonary/systemic) circulation
systemic
capacitance vessels
veins (collections and storage vessels)
central circulation includes blood in the ___ and ___
heart and pulmonary circulation
peripheral circulation is blood outside of ___ and ___
the heart and pulmonary circulation
pulmonary circulation is (high/low) pressure
low (12 mmHg)
systemic circulation is (high/low) pressure
high (90-100 mmHg)
fraction of blood volume in the arterial system
1/6
fraction of blood in the venous system
2/3
pressure is (proportionately/inversely) related to volume
inversely (higher volume = lower pressure, ex. veins)
blood flow is determined by ___ and ___ of the blood vessel
pressure difference between the 2 ends; resistance
equation of blood flow
F = (change in P) / R
blood flow in the circulatory system is represented by (heart rate/cardiac output)
cardiac output
laminar blood flow
characterized by plasma on the edges and cells in the center of the vessel; so flow is smooth (prevents clotting factors from coming into contact with the vessel wall, reduces frictional forces)
layering of components in the center of the bloodstream
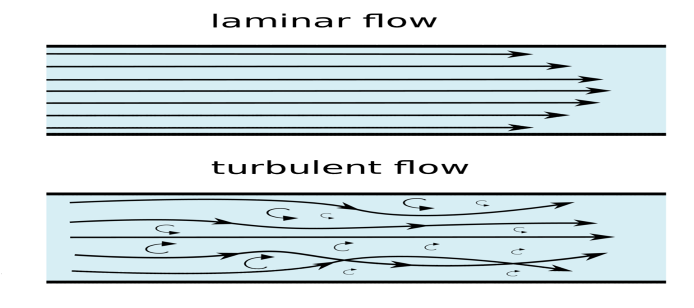
turbulent blood flow
disordered; the blood moves crosswise and lengthwise
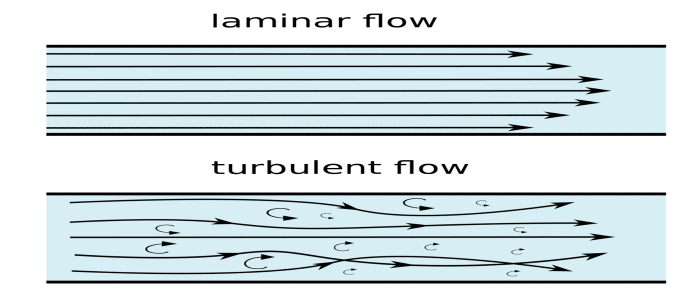
(laminar/turbulent) blood flow requires more pressure to push the blood through the vessel
turbulent
turbulent blood flow can be caused by:
- (increased/decreased) velocity
- (increased/decreased) vessel diameter
- (high/low) blood viscosity
increased velocity
decreased vessel diameter
low blood viscosity (as seen in anemia, because it allows faster BF)
(longer/shorter) vessel length increases resistance
longer
(larger/smaller) radius increases resistances
smaller
decreased temperature results in (increased/decreased) blood viscosity
increased
(increased/decreased) blood viscosity causes increased resistance
increased - friction of molecules in the fluid
wall tension is the force in the vessel wall that opposes ___
distending pressure inside the vessel
law of Laplace (describing relationship between wall tension, intraluminal pressure, and radius)
P = T/r → T = P x r (to describe the effect of radius on wall tension)
as the radius increases, wall tension becomes (greater/lesser)
greater - important concept for aneurysms
smaller radii require (more/less) pressure to dilate
more
wall tension (increases/decreases) as vessel walls become thinner
increases (and so decreases as the walls become thicker)
(veins/arteries) are more compliant
veins - 24x more than its corresponding artery
(arteries/veins) are more distensible
veins
tunica externa/adventitia is made of (smooth muscle/fibrous connective tissue/endothelial cells)
fibrous connective tissue
function of tunica externa
protect the vessel and anchor it to surrounding structures
tunica media is made of (smooth muscle/fibrous connective tissue/endothelial cells)
smooth muscle
function of tunica media
regulate the diameter of the vessel
thicker in arteries than veins
tunica intima is made of (smooth muscle/fibrous connective tissue/endothelial cells)
endothelial cells - with minimal elastic layer to join them to the tunica media
these cells are adjacent to the blood
arteries (do/do not) have properties of stretch and recoil during systole and diastole
do - due to large amount of elastic fibers
__ are resistance vessels for the circulatory system
arterioles
tissues (are/are not) able to regulate blood flow without input from the CNS
are
- do this as a result of changes in flow to the tissue or local tissue factors (oxygen, metabolite concentration)
metabolites that can affect local control of blood flow
accumulation of lactic acid, potassium, hydrogen ions
reactive hyperemia increases local blood flow due to ___
occluded blood supply (once the occlusion is removed)
(functional hyperemia is increase in BF due to increased activity)
endothelial control of blood flow: NO
causes vasodilation - normally released by endothelial cells and can be increased by Ach, histamine, bradykinin, thrombin, stress on endothelium
NO effect on platelets
inhibits aggregation to protect against thrombosis and the resulting vasoconstriction
endothelial control of blood flow: examples of vasoconstrictors
endothelin-1, angiotensin II, vasoconstrictor prostaglandins (F)
long term regulation of blood flow occurs via (autoregulation/collateral circulation)
collateral circulation - anastomotic channels and angiogenesis
cells important for angiogenesis
fibroblasts - produce VEGF, angiotensin, other important growth factors
histamine effect on blood flow
increases due to vasodilation
also increases cap permeability
serotonin effect on blood flow
causes vasoconstriction (S-2 receptors)
bradykinin effect on blood flow
causes vasodilation of arterial smooth muscles, increased permeability of capillaries, constricts venules