antimicrobial stewardship: start SMART then FOCUS
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
what is antimicrobial stewardship
an organisational and system-wide approach to promoting and monitoring the use of antimicrobials by
optimising therapy for individual patients
preventing the overuse and misuse of antimicrobials
minimising the development of resistance at patient and community levels
what is the antimicrobial stewardship clinical management algorithm
evidence-based guidance for secondary care clinicians and leaders (inpatient care settings)
designed to reduce the risk of antimicrobial resistance whilst safeguarding the quality of care for patients with infection
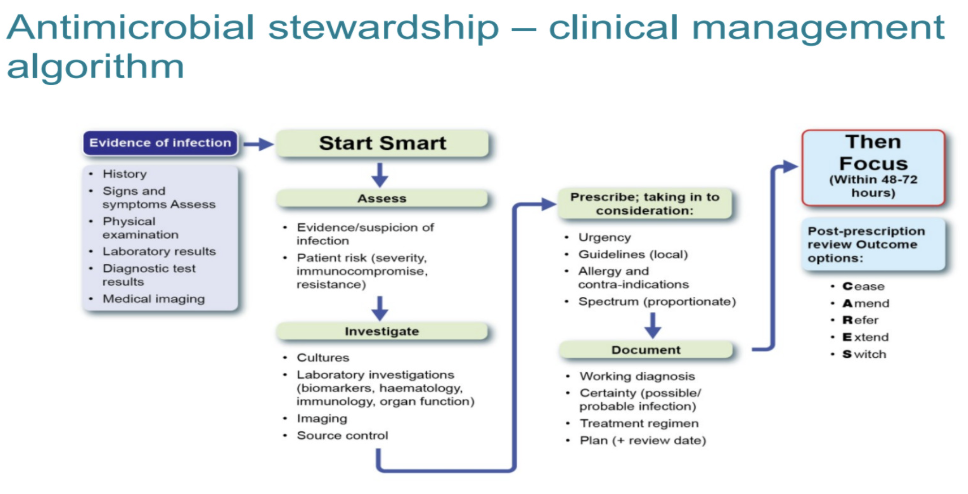
in start SMART, what is Assess
is the antimicrobial needed? is there evidence of infection? → DO NOT START ANTIMICROBIAL THERAPY UNLESS THERE IS CLEAR EVIDENCE OF INFECTION
Assess patient for clear evidence of infection
Perform a comprehensive patient assessment to guide selection of
proportionate treatment and determine the appropriate care environment.This includes considering disease severity, immunocompromised
patients, likelihood of resistant pathogen, prior exposure to antimicrobials, and patients with factors commonly associated with health inequalities where appropriate
what is the importance of clinicians ensuring that patients clinically require an antimicrobial prior to starting therapy
preserves the effectiveness of antimicrobials by keeping antimicrobial resistance in check
the unnecessary use of antimicrobials produce strong selective pressure, which drives the evolutionary response in microbes
how does antimicrobial therapy disrupt the gut microbiota
reduction in their microbial diversity → alters the function and formation of antimicrobial resistant strains → patients more susceptible to infection with opportunistic pathogens
example: C. dificil
what is the importance of patient and infection specific factors when reviewing patients with infection
includes considering patient vulnerability e.g.
if a patient is immunocompromised
if their using immunosuppressant medications
their vaccination status
infection severity
risk of mortality
in start SMART, what is investigate
Obtain appropriate specimens for culture prior to commencing therapy where possible, including blood cultures before starting IV treatment if appropriate (but do not delay treatment in cases of severe sepsis)
helps identify the infection source and organism susceptibility → clinicians can treat resistant pathogens effectively in the event of subsequent deterioration
cultures and sensitivities help support de-escalation from broad to narrow spectrum antibiotics
helps decide whether we can stop therapy when cultures are negative
Follow local guidelines for ordering appropriate laboratory investigations
biochemistry (C-reactive protein), haematology (WBC count), immunology
organ function
medical imaging where available to find out location and severity of infection
implement any required source control interventions as soon as medically/surgically practical → reduces risk of treatment failure
for example an infected abscess on the chest would need to be drained and removed before antibiotics can actively treat the infection, or removing an infected catheter
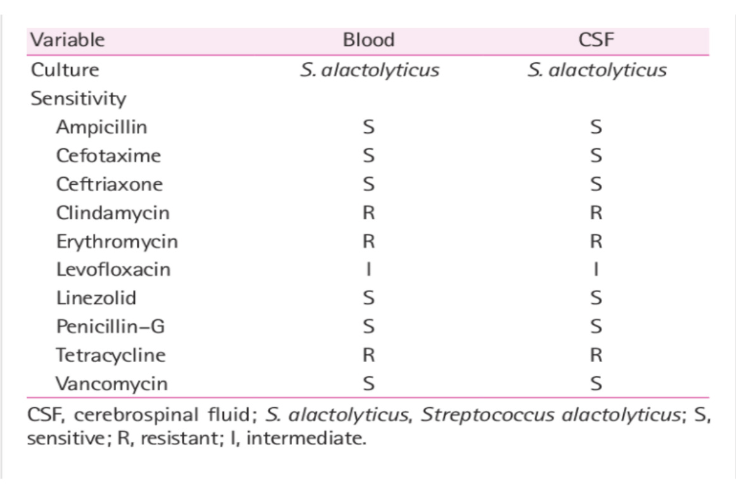
how are cultures obtained
Any body tissue or fluid evaluated in the laboratory using culture techniques to detect and identify infectious processes. Culture techniques can be used to determine sensitivity to antibiotics.
A sensitivity test checks to see what kind of medicine, such as an antibiotic, will work best to treat the illness or infection.
Links with “FOCUS” as sensitivities usually take 48 to 72 hours to come back
Due to advances in rapid diagnostics it may be possible to review prior to 48 hours after first dose.
what is the CRP (C-reactive protein) test
measures level of CRP in the blood
CRP plays a key role in the body’s immune response by acting as a signal for inflammation, as well as
assess the risk of heart disease
track inflammatory conditions like rheumatoid arthritis or lupus
evaluate how well the body responds to treatment
viral infections can increase CRP levels
in start SMART, what is prescribe
Initiate prompt antimicrobial treatment for patients with severe sepsis or life-threatening infections based on local guidelines/scores → reduces avoidable morbidity and mortality.
Comply with local antimicrobial prescribing guidance e.g. formularies
Take a thorough drug allergy history, make sure it is a true allergy
Avoid inappropriate use of broad-spectrum antibiotics
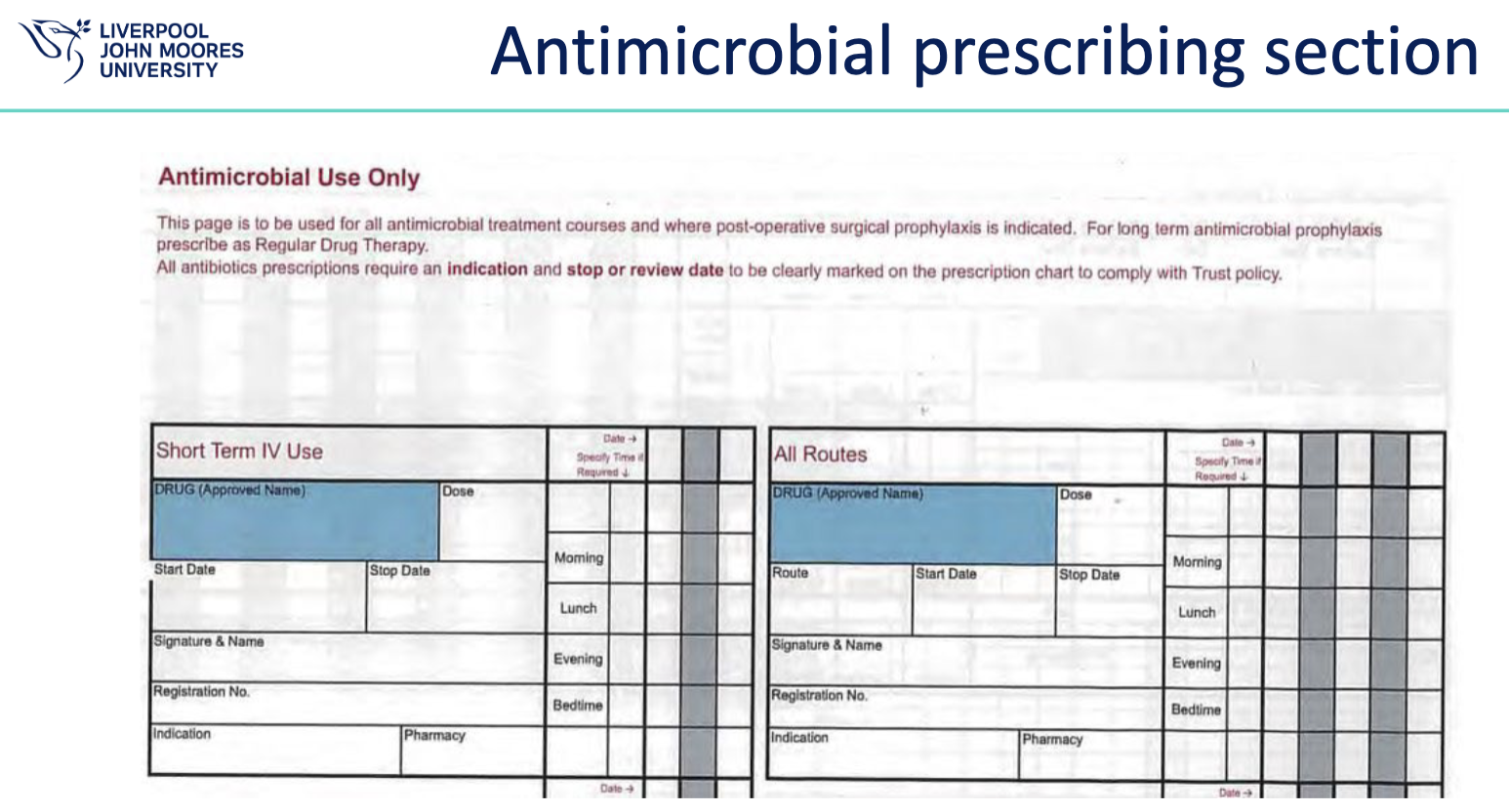
in start SMART, what is document
Document evidence of infection, working diagnosis (clinical indication) and disease severity, drug name, dose, formulation, and route on the prescription chart and in the clinical notes → in accordance with
good clinical record-keeping.Include treatment duration where possible or specify a review date → avoids unnecessarily prolonged treatment as colleagues know when to change or stop therapy
Record a clear clinical plan for patient management to ensure safe handover of care between clinical teams.
Provide exact indication on the drug chart for medical prophylaxis
what is allergy status
On paper charts the allergy status of a patient has to be written on the front of the drug card.
Some hospital policies prohibit the nurse from administering any medication, unless the allergy status of the patient is documented on the front of the drug chart.
In the EPMA system the allergy status has to be entered into the system, which can prove difficult at times.
if the allergy status of the patient is not done properly, warning signs to alert the prescriber about an allergy do not necessarily appear and cause patient safety issues.
how do we avoid inappropriate use of broad-spectrum antibiotics
should only be used when indicated by the person's clinical condition, however you MUST consider sepsis or life-threatening conditions.
Need to be reserved to treat resistant disease.
They should generally be used only when narrow-spectrum antibiotics are ineffective because they increase the risk of MRSA, Clostridium difficile and resistant UTIs
what is empirical therapy
Treatment given without knowledge of the cause or nature of the disorder and based on experience rather than logic
Sometimes urgency dictates empirical treatment, as when a dangerous infection by an unknown organism is treated with a broad- spectrum antibiotic while the results of bacterial culture and other tests are awaited
how is the prescribing decision documented
Document on drug chart and in clinical notes
Evidence of infection
Clinical indication /working diagnosis (and disease severity)
drug name
Dose
formulation
route
include review/stop date or duration
hospital A recording of clinical indication and documentation error
In Hospital A, the EPMA system used mandatory fields to force the prescriber to
document the clinical indication of the stipulated medications, by not allowing
them to continue with the prescribing process unless the information was
completed.Mandatory field, can lead to “workarounds” where prescribers enter a full stop
or “not known” to navigate past and complete the prescription. Drop down lists can
facilitate but they must be user friendly
hospital B recording of clinical indication and documentation error
In Hospital B, the clinical indication of stipulated medications was done by
completing a “note” within the electronic prescription, this was not compulsory
and therefore the system did not enforce the prescriber to provide this
information.A note to be completed, not mandatory, but must specifically click on “note” to
enter the detail
hospital C recording of clinical indication and documentation error
In Hospital C, on the paper drug chart there was a specific box requiring the
clinical indication to be completed, like the rest of the prescription, manuallyPaper prescription chart – prescriber can complete at any time quite quickly. Colleagues can also update the CI on the prescription
documenting antibiotic course length
A three day antibiotic course length can be automatically populated within the EPMA system or can be pre-printed for three days of administration on the paper chart.
These design features of the prescribing systems are in place to facilitate antibiotic review and discontinuation in a timely fashion.
Both paper and EPMA systems have their difficulties regarding this area → Ultimately it comes down to the prescriber putting in the right information in the first place, showing an area of prescribing more susceptible to human error
stop dates in the EPMA system
It was considered how EPMA might change the discontinuation of antibiotics, possibly leading to the prescription never being stopped.
The EPMA systems are able to counteract the potential problem of antibiotics never being stopped, by utilising automatic stop dates within the system.
However, the EPMA system may overcompensate, if the stop date is inappropriate, leading to patient safety issues.
what is ‘then FOCUS’ the antimicrobial stewardship clinical management algorithm
reviewing the clinical diagnosis and the continuing need for antibiotics at 48-72 hours and documenting a clear plan of action, which is called the ‘antimicrobial review outcome’. the five ‘antimicrobial review outcomes’ options are to (CARES):
CEASE antimicrobial treatment if there is no evidence of infection
AMEND antibiotics → ideally to a narrower spectrum, or broader if required
REFER to non-ward-based services → Outpatient Parenteral Antibiotic Therapy (OPAT)
EXTEND antimicrobial treatment and document next review date or stop date
SWITCH antibiotics from intravenous to oral (IVOS)
example of a culture and sensitivity report
what is REFER ( ‘antimicrobial review outcomes’)
Refer appropriate patients to non-ward antimicrobial therapy services when available. Options include
OPAT (Outpatient Parenteral Antimicrobial Therapy)
COPAT (Complex Outpatient Antimicrobial Therapy)
virtual wards if available.
These services enable timely discharge, reduce healthcare-associated infection risk, and maintain safe, monitored treatment outside hospital settings
what is EXTEND (‘antimicrobial review outcomes’)
Extend antimicrobial prescription and document next review date or
stop date for IV and oral antimicrobials → avoids inappropriately prolonged treatment.Balance risk versus benefit
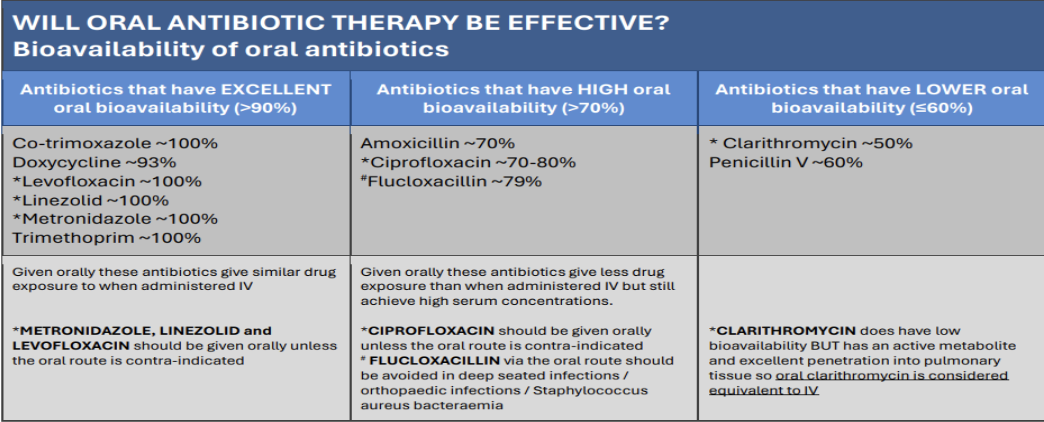
what is Intravenous-to-oral SWITCH (IVOS) (‘antimicrobial review outcomes’)
The national antimicrobial IVOS criteria for prompt switch contains 24 IVOS criteria in 5 sections. There are different guidelines for adults and paediatrics see canvas.
The 5 sections are
Timing of intravenous antimicrobial review (within 48 hrs 1st dose)
Clinical signs and symptoms of infection improving
Infection Markers
Enteral route
Special considerations
what infection markers need to be considered
Temperature has been between 36 to 38°C for the past 24 hours.
Early Warning Score is decreasing.
White Cell Count is trending towards the normal range.*
C-Reactive Protein is decreasing.*
these infection markers could also indicate inflammation or be affected by, for example, steroid treatment; ‘Prompt for switch’ or ‘Assess for switch’ may still occur if they are the only markers not met.
what are the considerations for enteral route
Gastrointestinal tract must be functioning with no evidence of
malabsorption.is itsSafe to swallow or is there enteral tube administration.
availability of suitable oral switch option available, considering oral bioavailability, any clinically significant drug interactions or patient allergies.
No significant concerns over patient adherence to oral treatment.
No vomiting within the last 24 hours
summary of oral bioavailability of different antibiotics
what are special considerations
deep-seated infection
infection requiring high tissue concentration of antimicrobial
infection requiring prolonged intravenous antimicrobial therapy
critical infection with high risk of mortality
what are specific infections for special consideration
bloodstream infection
empyema
endocarditis
meningitis
osteomyelitis
severe or necrotising soft tissue infections
septic arthritis
undrained abscess