Perio II Midterm COMBINED
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
64 Terms
What is Non-Plaque Induced Gingivitis
It is gingival inflammation with pseudo-pocket, meaning there is no associated bone loss
may be mediated by systemic or local risk factors such as pregnancy or drug influenced
GENETIC
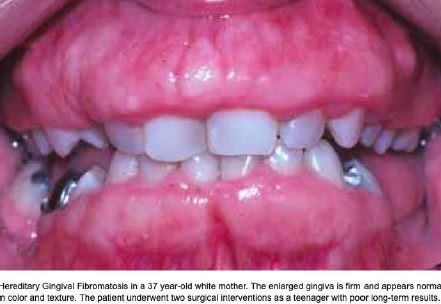
Hereditary Gingival Fibromatosis
Clinical Signs
Location
Etiology
Treatment
Clinical Signs: Rare gingival benign enlargement in various degrees
Location: Tuberosities, anterior free/attached gingiva, retromolar pad areas
Etiology: Hereditary gene mutation; can occur in isolation or as part of a syndrome
Treatment: Excisional (remove piece) biopsy (for diagnosis); recurrence expected

SPECIFIC INFECTIONS
Necrotizing Periodontal Disease
Clinical Signs
Etiology
Treatment
Clinical Signs: Ulceration of papillae ("punched out"), painful bleeding gingiva, severe halitosis, systemic signs (fever, malaise, lymphadenopathy)
May be gingivitis (no bone loss) or periodontitis (bone loss)
May be Stomatitis: ulceration >1cm, from gingival margin including tissue beyond mucogingival junction
Etiology: Bacterial (e.g., spirochetes, Prevotella intermedia); often seen in HIV patients
Treatment: Gentle debridement, 0.12% CHX rinse,
→ If poor response: metronidazole ± amoxicillin/clindamycin, analgesics, antifungals if HIV-positive

SPECIFIC INFECTIONS
Gonorrhea (oral)
Clinical Signs
Etiology
Treatment
Clinical Signs: Ulcer or fiery red mucosa halo with white pseudo-membrane inside ± symptoms, painful sore throat, lymphadenopathy
Etiology: Neisseria gonorrhoeae *(bacteria)
Treatment: Referral to physician

SPECIFIC INFECTIONS
Syphilis (oral)
Clinical Signs
Etiology
Treatment
Clinical Signs: Fiery red edematous ulcerations, mucous patches, or atypical inflamed gingivitis
Etiology: Treponema pallidum (bacteria)
Treatment: Referral to physician

SPECIFIC INFECTIONS
Hand-Foot-Mouth Disease
Clinical Signs
Etiology
Treatment
Clinical Signs: Small vesicles rupture to leave fibrinous ulcers; affects mucosa, gingiva, hands, feet; mainly in children
Etiology: Coxsackie virus
Treatment: Self-limiting (7–10 days); topical analgesics for pain
SPECIFIC INFECTIONS
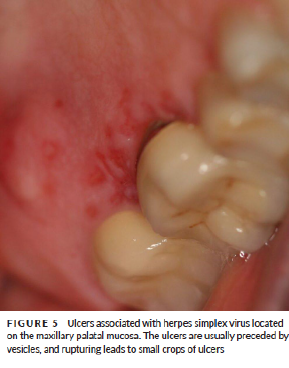
Herpetic Gingivostomatitis
Clinical Signs
Location
Etiology
Treatment
Clinical Signs: Vesicles that coalesce and leave ulcer coated by fibrin; affects keratinized gingiva/hard palate; contagious
Etiology: Herpes Simplex Virus (Type 1 oral / Type 2 genital)
Treatment: Self-limiting; antivirals may speed healing

SPECIFIC INFECTIONS
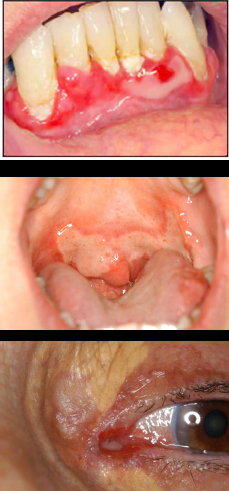
Varicella zoster: Chickenpox (top)/ Shingles (bottom)
Clinical Signs
Etiology
Treatment
Clinical Signs:
Chickenpox (children): yellowish Vesicles rupture into ulcers
Shingles (adults): Unilateral ulcers with possible vision impairment
Etiology: Varicella-zoster virus
Treatment: Antiviral medication; refer to ophthalmologist if ocular involvement

SPECIFIC INFECTIONS
Squamous Cell Papilloma
Clinical Signs
Etiology
Treatment
Clinical Signs: Asymptomatic exophytic papillomatosis
Verrucous or cauliflower-like lesion
Etiology: Human Papillomavirus (HPV)
Treatment: Biopsy

SPECIFIC INFECTIONS
Candidosis→ Pseudomembranous (top) and Erythromatous (bottom)
Clinical Signs
Etiology
Treatment
Clinical Signs:
Pseudomembranous: White removable plaques
Erythematous: Seen with steroid use, dentures, or HIV
Etiology: Candida albicans
Treatment: Antifungals (e.g., fluconazole)

HYPERSENSITIVITY RXN
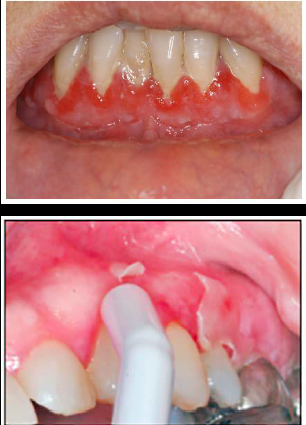
Plasma Cell Gingivitis(Top) / Contact Allergy (Bottom)
Clinical Signs
Etiology
Treatment
Clinical Signs:
Contact allergy: Redness
Plasma cell gingivitis: Velvety erythematous gingiva, usually anterior maxilla
Etiology: Allergic reaction to toothpaste, mouthwash, dental materials
Treatment: Eliminate causative agent; biopsy to confirm
AUTOIMMUNE
Pemphigus Vulgaris (top is vesiculobullous and bottom is desquamative)
Clinical Signs
Etiology
Treatment
Clinical Signs: Desquamative gingivitis (white patch shedding) or vesiculo-bullous lesions; intraepithelial bullae rupture to form erosions; positive Nikolsky sign, pain
Etiology: Autoimmune disease; Autoantibodies against desmosomes in epithelial layer
Treatment: Systemic steroids, immunosuppressants; refer to dermatologist
AUTOIMMUNE
Pemphigoid
Clinical Signs
Etiology
Treatment
Clinical Signs: VERY RED Desquamative gingiva, bullae from rubbing (NEGATIVE OR positive Nikolsky sign); painful; scarring can cause blindness if ocular lesions present
Etiology: Autoimmune disease; Autoantibodies against basement membrane desmosomes
Treatment: Systemic steroids, immunosuppressants; refer to ophthalmologist

AUTOIMMUNE
Lichen Planus
Clinical Signs
Etiology
Treatment
Clinical Signs:
Reticular: White lace-like striae (not painful)
Atrophic: Erythematous, painful, desquamative gingivitis
Etiology: Inflammatory reaction to unidentified antigen in basement layer of the epithelium → HAS PREMALIGNANT POTENTIAL!
Treatment: Steroids, topical analgesics

AUTOIMMUNE
Lupus Erythematosus
Clinical Signs
Etiology
Treatment
Clinical Signs: Butterfly rash on face (nose/cheeks), photosensitivity
Etiology: Autoimmune inflammatory reaction to unidentified antigen in basement membrane
Treatment: Avoid sun, NSAIDs, immunosuppressants, steroids

GRANULOMATOUS (but technically also autoimmune)
Crohn’s Disease
Clinical Signs
Etiology
Treatment
Clinical Signs: Cobblestone oral mucosa, GI symptoms like abdominal pain, fever, altered bowel habits
Etiology: Autoimmune; a form of IBD
Treatment: Nutritional support, corticosteroids, anti-inflammatory meds

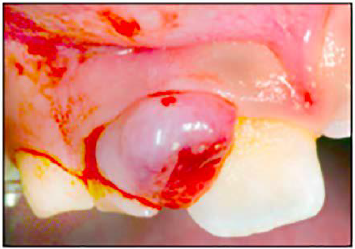
REACTIVE PROCESSES: EPULIDES
Pyogenic Granuloma
Clinical Signs
Location
Etiology
Treatment
Clinical Signs: Red/pink, painless, fast-growing, compressible, painless gingival mass; common during pregnancy
Etiology: Hormonal changes or irritation/minor injury
Treatment: Biopsy; high chance it may recur
REACTIVE PROCESSES: EPULIDES
Peripheral (soft tissue) or Central (osseous) Giant Cell Granuloma
Clinical Signs
Etiology
Treatment
Clinical Signs: Purple/blue-brownish soft mass; resembles pyogenic granuloma, mainly in gingiva but can be in mucosa
Etiology: Reaction to irritation
Treatment: Biopsy

PRE-MALIGNANT NEOPLASMS
Leukoplakia
Clinical Signs
Location
Etiology
Treatment
Clinical Signs: Fully White lesion (smooth, corrugated, or verrucous); not removable; premalignant
Location: Tongue, floor of mouth, buccal mucosa
Etiology: Often linked to tobacco/alcohol
Treatment: Biopsy

PRE-MALIGNANT NEOPLASMS
Erythroplakia
Clinical Signs
Location
Etiology
Treatment
Clinical Signs: Red, velvety, sharply demarcated lesion; higher premalignant potential than leukoplakia
Location: Floor of mouth, soft palate
Etiology: Often linked to tobacco/alcohol
Treatment: Biopsy

PRE-MALIGNANT NEOPLASMS
Squamous Cell Carcinoma
Clinical Signs
Location
Etiology
Treatment
Clinical Signs: Painless masses, red/white patches, non-healing ulcers; may spread to lymph nodes; higher malignant potential
Location: Gingiva, floor of mouth, tongue
Etiology: Often linked to tobacco/alcohol
Treatment: Biopsy and urgent referral
NUTRITIONAL
Vitamin C Deficiency (Scurvy)
Clinical Signs
Location
Etiology
Treatment
Clinical Signs: Gingival bleeding, ulceration, swelling
Etiology: Lack of ascorbic acid (affects connective tissue)
Treatment: Vitamin C supplementation and balanced nutrition

TRAUMATIC
Frictional Keratosis
Clinical Signs
Location
Etiology
Treatment
Clinical Signs: White, sharply demarcated lesion; painless; non-removable
Location: Facial attached gingiva; buccal mucosa (linea alba)
Etiology: Local trauma
Treatment: Remove irritant

Chemical Insult or Thermal
Clinical Signs
Etiology
Treatment
Clinical Signs: Sloughing or ulceration of gingival surface
Etiology: Overuse of CHX, aspirin, hydrogen peroxide, whitening agents, etc.
Treatment: Resolves once irritant is removed

Gingival Pigmentation (Melanoplakia)
Clinical Signs
Location
Etiology
Treatment
Clinical Signs: Brown-black diffuse pigment; symmetrical
Location: Gingiva, buccal mucosa, lips, tongue
Etiology: Physiologic (common in darker skin); can occur in systemic diseases such as Addison’s disease (Hypocortisolism)
Treatment: Laser/scalpel depigmentation (optional)

Amalgam Tattoo
Clinical Signs
Etiology
Treatment
Clinical Signs: Small bluish/grey/black localized pigmentation; flat
Etiology: Amalgam particles embedded during restorations
Treatment: Biopsy if diagnosis is uncertain
What are the 3 factors causing plaque induced gingivitis?
Plaque biofilm
Systemic Factors : smoking, diabetes hyperglycemia, nutrition, Sex steroid hormones (puber, pregn, menst, contracept) Hematological conditions
Drug-influenced: Phenytoin, Cyclosporine, CCB
Predesposing vs Modifying Factors
Predisposing factors: agents or conditions that contributes to the accumulation of plaque; anatomy, position, restorations
Modifying factors: agents or conditions that alters the way in which and individual RESPONDS to subgingival plaque accumulation; smoking, systemic cond, medications
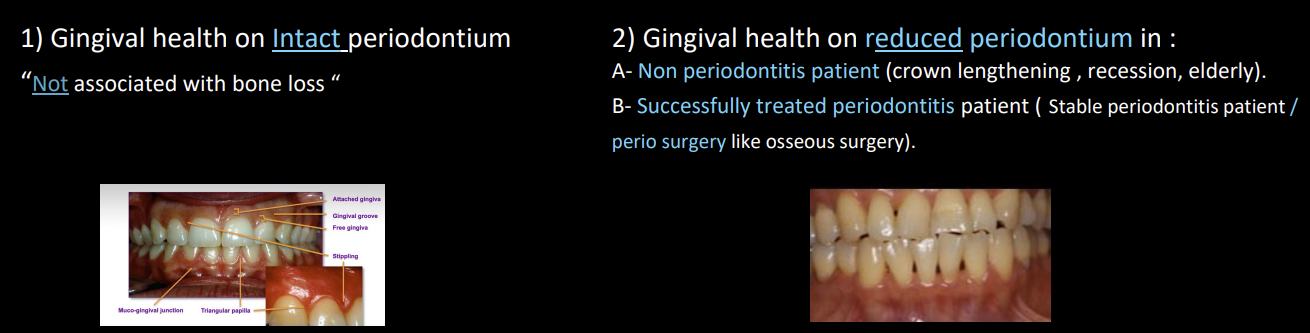
Categories of Periodontal Health
Pristine Gingival health: TOTAL absence of clinical inflammation and physiological immune surveillance on periodontium. Not likely observed clinically
Clinical periodontal health with intact/reduced periodontium: absence or minimal levels of clinical inflammation in a periodontium with normal support
<10% BOP sites with probing depths <_3mm
Reduced periodontium non periodontitis patient like crown lengthening, recession, elderly OR successfully treated periodontitis pt that is stable
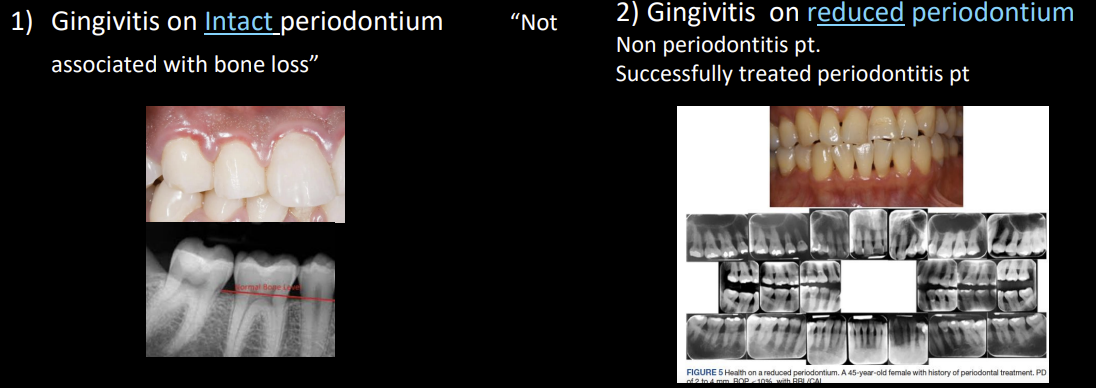
Categories of Gingivitis
>_10% BOP sites with probing depths <_3mm, swelling, loss of knife edged gingival margin, blunting of papillae, redness, discomfort on gentle probing, halitosis
Gingivitis on intact periodontium
Gingivitis on reduced periodontium
What are the 3 forms of periodontitis
Necrotizing Periodontitis Diseases
Periodontitis as manifestation of systemic disease
Periodontitis
How do you determine the normal alveolar crest level?
0.4 to 1.9mm from CEJ to alveolar bone crest in bitewing
Clinical features of Necrotizing Periodontal Disease
Papilla necrosis (punched out)
Bleeding
Extremely foul smelling breath
Host immune impairment
Severe malnourishment, severe viral infection, severe living cond, stress, tobacco and alcohol
Periodontitis as a manifestation of Systemic Disease can be due to what conditions
Disorders causing bone loss
Genetic disorders
Down syndrome
Papillon-Lefevre Syndrome
SLE
Acquired immunodeficiency
HIV
Inflammatory diseases
Inflammatory Bowel Disease
Diabetes mellitus
Obesity
Osteoporosis
Stress and depression
Smoking
Oral squamous cell carcinoma
Giant cell granulomas
Hyperparathyroidism
Define the Periodontitis Diagnosis
Chronic (calculus frequent finding) or aggressive (pt younger than 25 with bone loss associated with first molars and incisor teeth
3 Components to form periodontitis diagnosis
Identify pt as a periodontitis case by finding:
Interdental CAL detectable at 2mm or >2 non adjacent teeth OR buccal/Lingual CAL 3 or >3mm and 3 or + mm PD in 2 or > teeth
CAL cannot be due to non-perio causes such as recession due to trauma, caries extending to cervical area, CAL on distal of 2nd molar, malpositioning or extraction of 3rd molar, endodontic lesion draining, occurrence of vertical root fracture
Identification of the specific form of periodontitis
Periodontitis, Periodontitis due to systemic disease and necrotizing periodontitis
Description of the presentation and aggressiveness of the disease by stage and grade
How deep should the probe penetrate into JE
0.5mm, stopping 0.4 coronal to termination of JE
What is CAL
CAL is the distance between CEJ and base of the sulcus, calculated as:
PD (GM to base of pocket) + Recession (CEJ to GM)
In health = 0
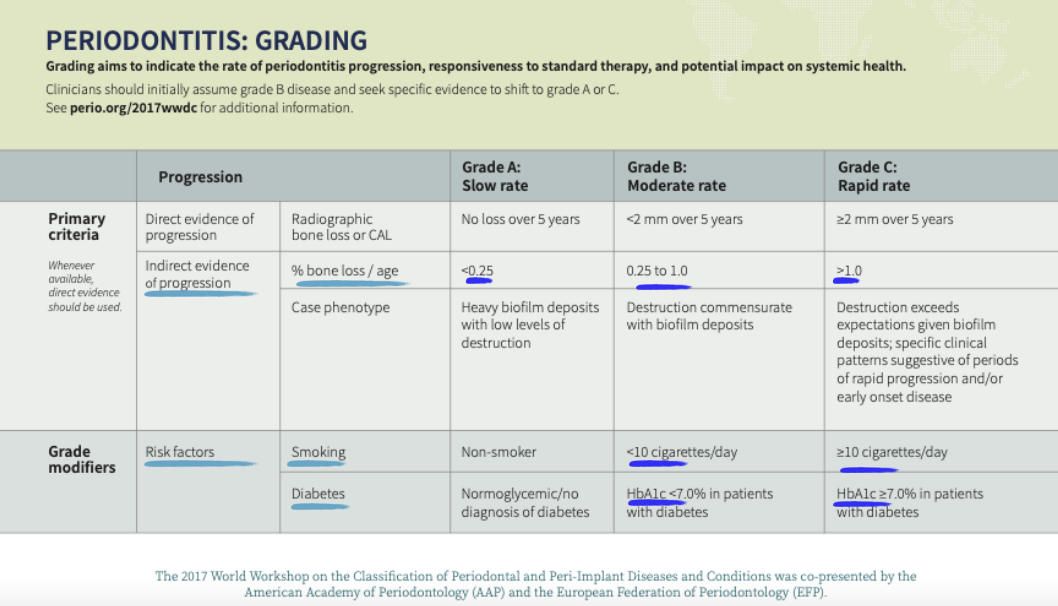
Explain What staging and grading means
Staging = Severity of disease at presentation + Complexity of disease management
Grading = Information on biological features of disease + Rate of progression + Risk assessment
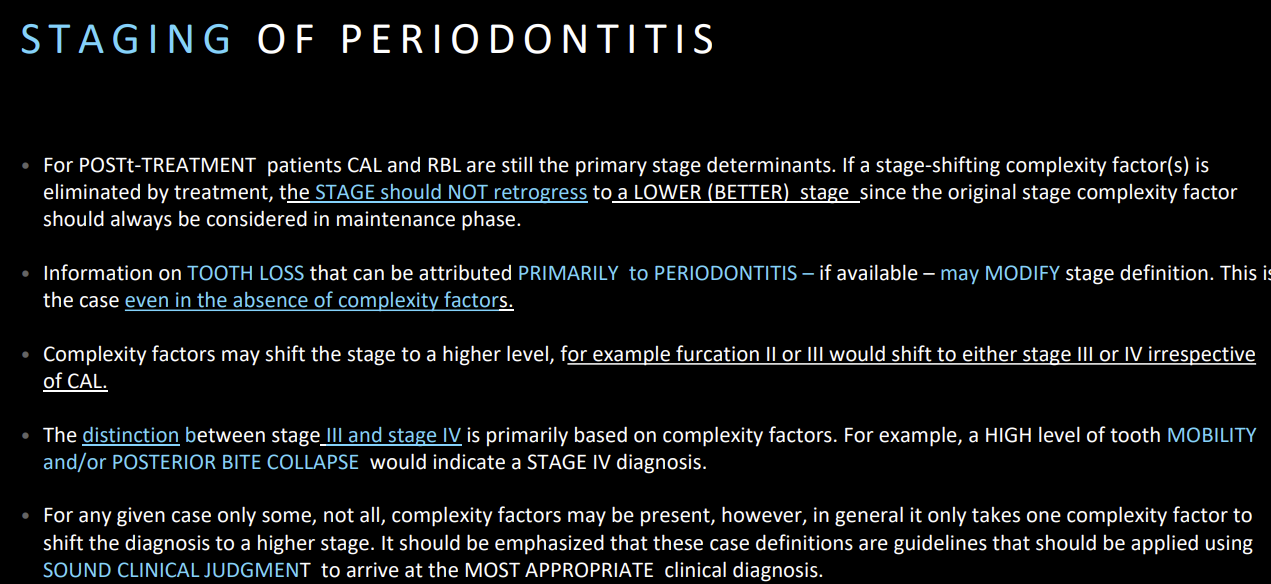
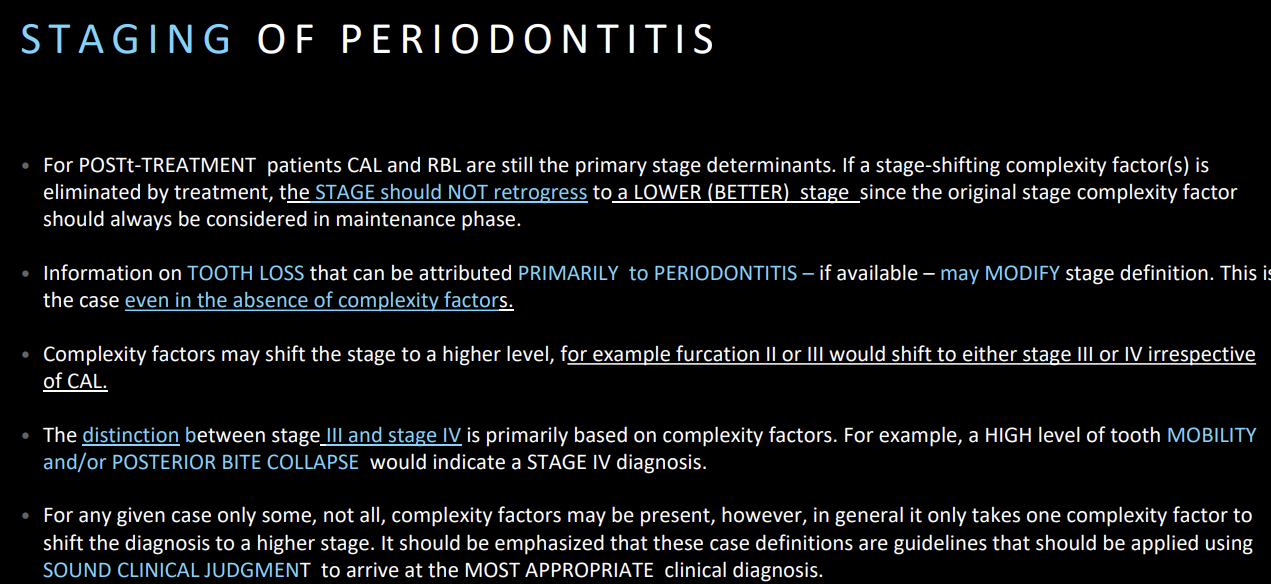
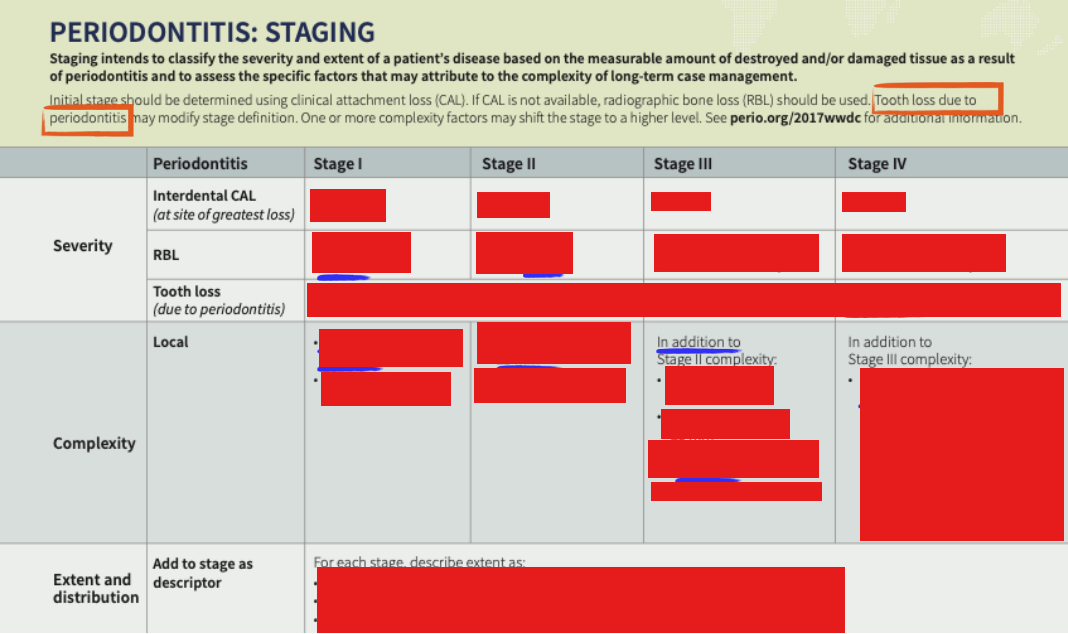
Staging
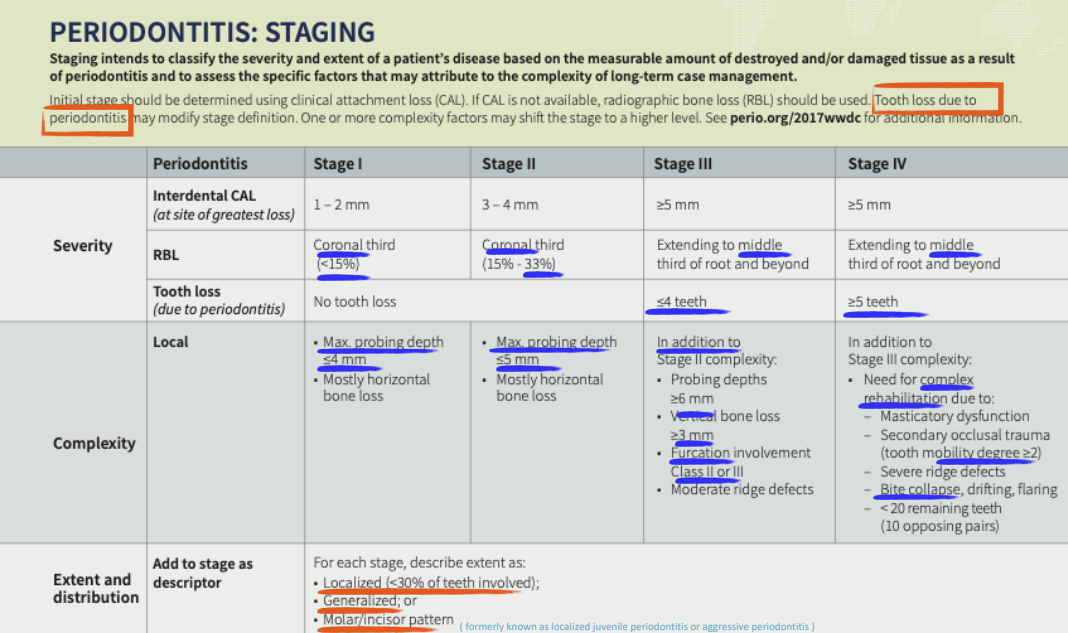
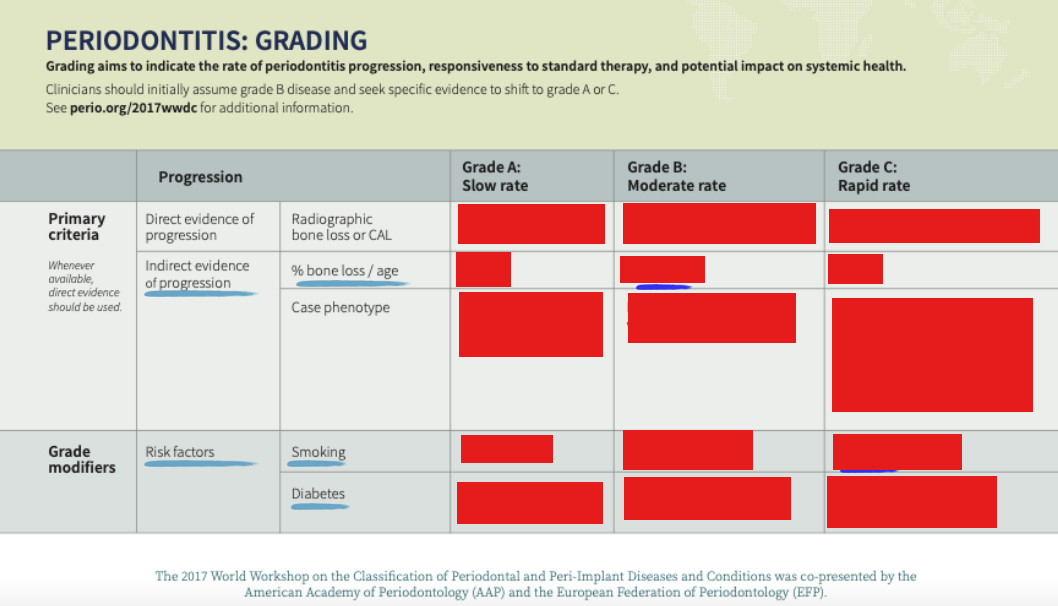
Grading
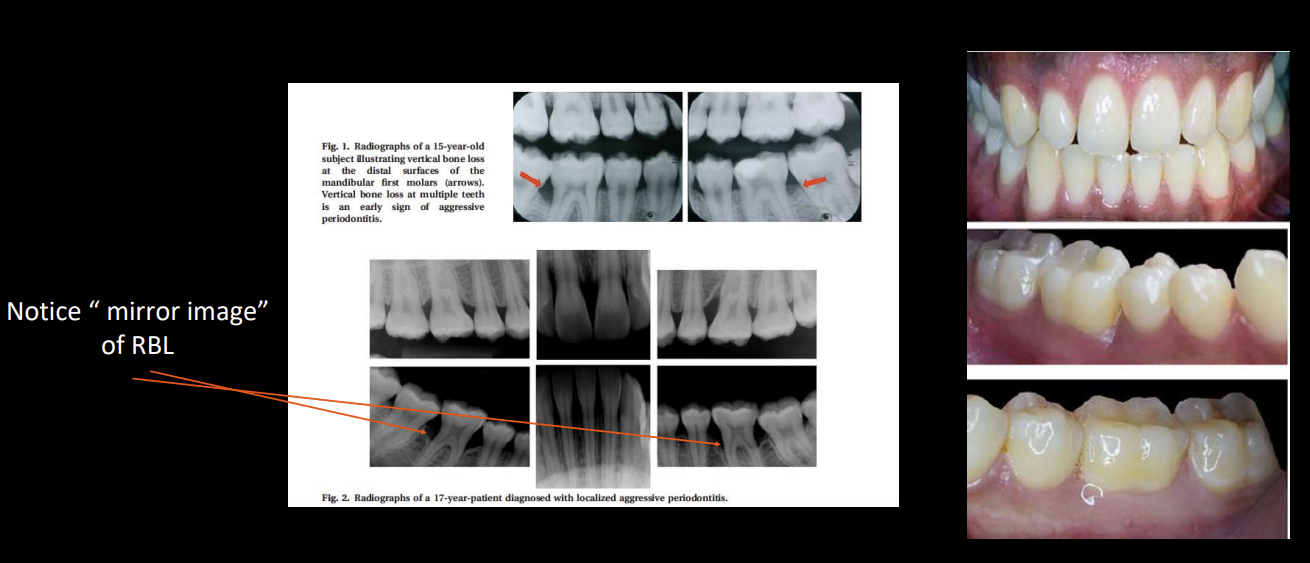
Molar incisor pattern Periodontitis
Genetic
Due to P. gingivalis and A.A bacteria
3:1 female to male ratio
30 years or younger patient
Usually stage 3 grade C, rapid sudden disease and gross deposits of calculus are uncommon
Mirror images of RBL
Refer to PG Perio for amoxicillin + metronidazole adjunct treatment to SRP
Can a patient have periodontitis even if there is no discernible bone loss?
Yes, if there is enough CAL; Clinical bone loss appears before RBL
Signs and Symptoms of Periodontal abscesses
Signs: suppuration, gingival ovoid elevation, increased PD, tooth mobility/elevation, regional lymphadenopathy
Symptoms: pain, tenderness to palpation, lateral percussion, fever and malaise
Tx: antibiotics if systemic involvement (fever/malaise, lymphadenopathy)
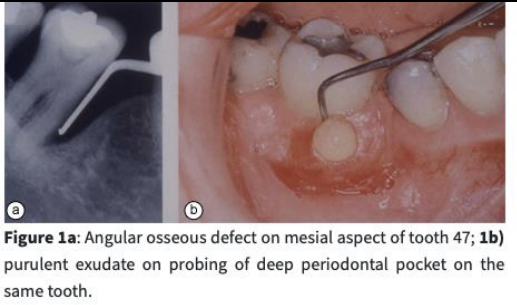
Classifications of Periodontal abscess in perio pt vs non-perio pt
Perio: can be acute exacerbation or after treatment
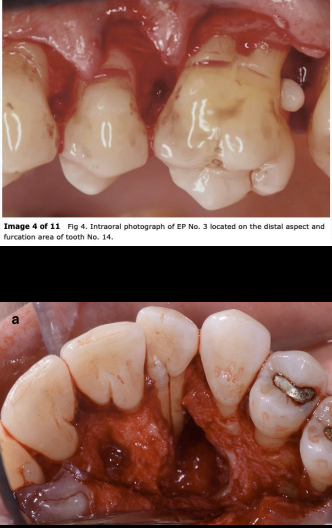
N-Perio: due to harmful habits, ortho, impaction, alteration of root surface, perforation, enamel pearl, fissure/fracture
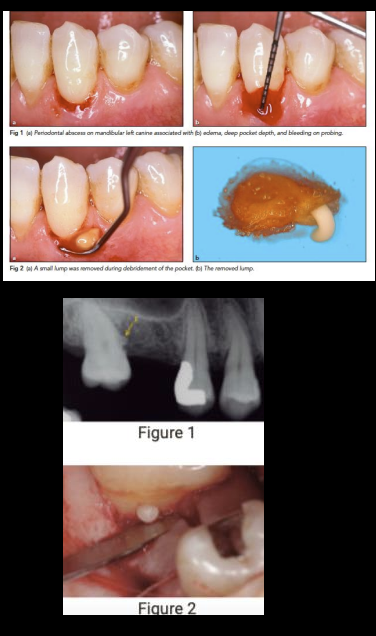
How to identify Perio-Endo Abscess??
There is a periodontal pocket reaching the apex of the root AND there is absence of pulp vitality, sensitive to percussion and palpation
Could also be bone resorption at apex, spontaneous pain, purulent exudate, mobility, sinus tract
an be primarily endo, perio or combined
root damage has poor prognosis
Always do endo first

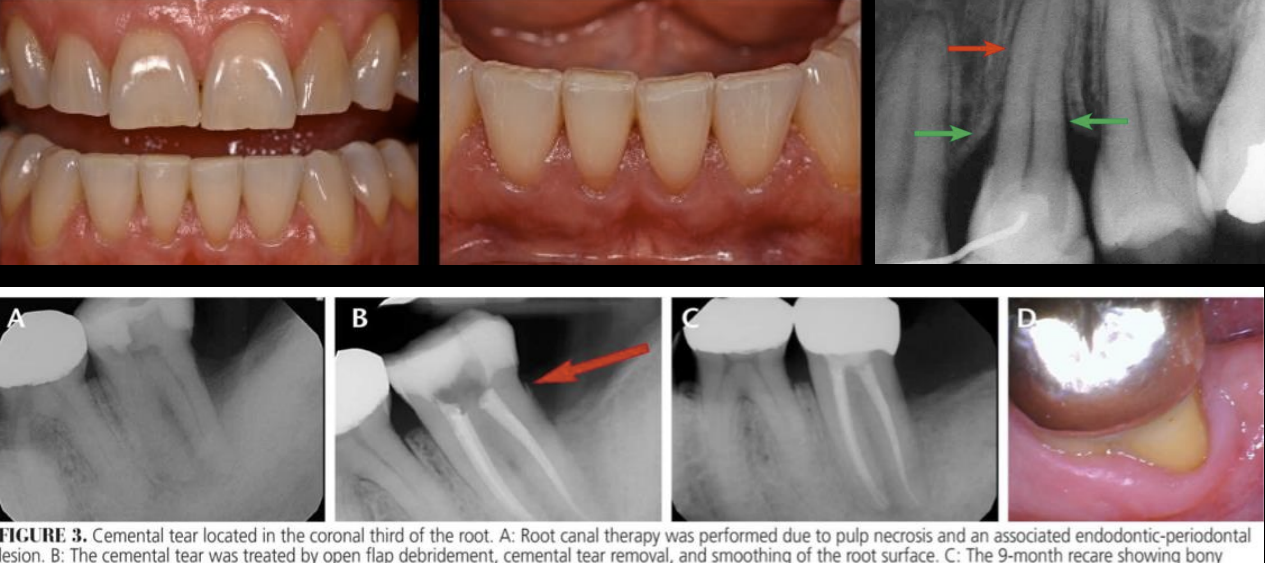
Indicators of Traumatic Occlusal forces: treat and improve pdl or reduce by 0.1 per year
fremitus
Mobility
occlusal discrepancies
Wear facets
Tooth migration
Fracture
Thermal sensitivity
Discomfort when chewing
Widened PDL space
Root resorption
Cemental tear
Types of Traumatic occlusal forces
Primary: trauma applied to a tooth with normal periodontal support
Secondary: trauma applied to tooth with reduced periodontal support
Orthodontic forces: sometimes can adversely affect periodontium and result in root resorption, pulpal disorders, recession and alveolar bone loss
Crown margins/restorations may be placed up to ___mm inside the gingival sulcus, if not CAL can appear as well as bone loss and recession within ____ weeks
T/F There is evidence to suggest that tooth supported/retained restorations and their design, fabrication, delivery, and materials can be associated with plaque retention and loss of clinical attachment
Crown margins may be placed up to 0.5mm inside the gingival sulcus, if not CAL can appear as well as bone loss and recession within 0-8 weeks
T/F There is evidence to suggest that tooth supported/retained restorations and their design, fabrication, delivery, and materials can be associated with plaque retention and loss of clinical attachment

What are some tooth related factors that can cause periodontitis
Cervical enamel projections, developmental grooves
Position, root proximity, root resorption, root fracture

What is the name of the Prognosis System and what is the purpose of it
KWOK and CATON 2007 PROGNOSIS is based on the prediction of future stability of the periodontal supporting tissues
Local Factors
Objective findings in the mouth contributing to periodontal disease
Pocket depths >5mm
Plaque retentive factors such as furcation involvement, enamel pearls, palatal groove, root proximity, open contacts, overhang restorations
Trauma from occlusion causing progressive mobility
General Factors
Factors that contribute to progression of the disease
Pt compliance
Smoking
Uncontrolled diabetes
History of periodontal disease
Systemic disease
Explain each prognosis category in KWOK and CATON system
Favorable: Tooth will be stabilized with comprehensive perio tx and PMT, loss of periodontal supporting tissues is unlikely
Questionable: Local/systemic factors may or may not be able to be controlled. periodontium can be stabilized with comprehensive perio treatment and maintained only is these factors are controlled, otherwise breakdown may occur
Unfavorable: Local and systemic factors cannot be controlled> Perio breakdown is likely even with comprehensive periodontal tx and maintenance
Hopeless: Tooth must be extracted

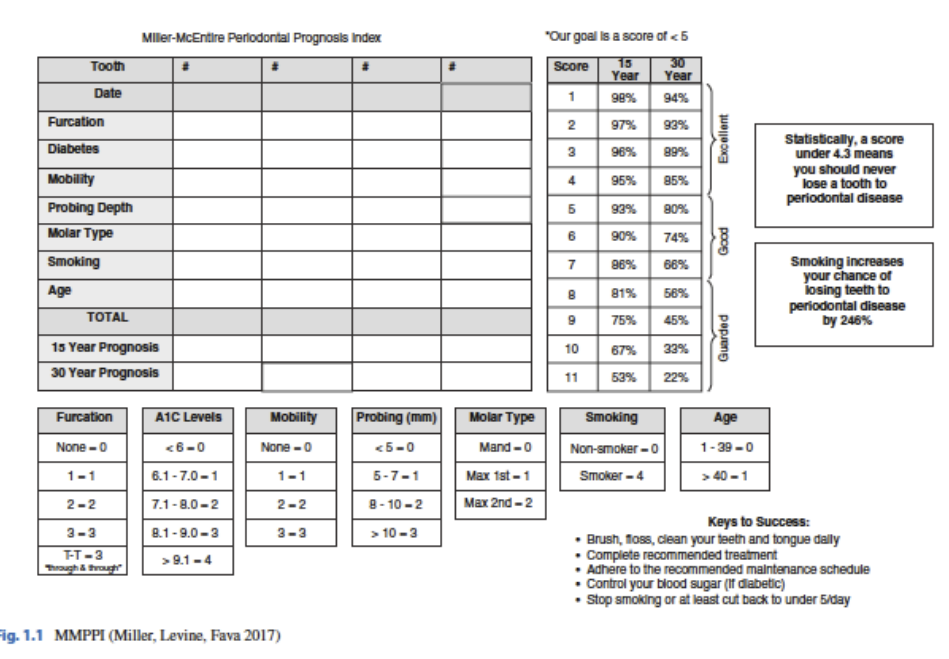
7 factors Miller McEntire Periodontal Prognosticator Index for Molar Teeth (MMPPI)
Include goal scores
Pocket Depth
Mobility
Furcation involvement
HbA1C levels
Molar type
Smoking
Age
Scores: 1-4 = Excellent, 5-8 = Good, 9-11=Guarded
<5 is the target
Gingivitis : Prophylaxis
D1110
Scaling for Gingivitis
D4346
Scaling for Gingivitis with re-eval
D0171P
SRP: 3 or less teeth involved in the quadrant
D4342
SRP: 4 or more teeth involved in the quadrant
D4341
SP with prophy
N1110
Periodontal Re-evaluation after SRP
D0171P but can also just do prophy
PMT
D4910