Physiology Exam 3 Lecture 10B [Respiratory gas exchange and transport: Harata]
1/94
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
95 Terms
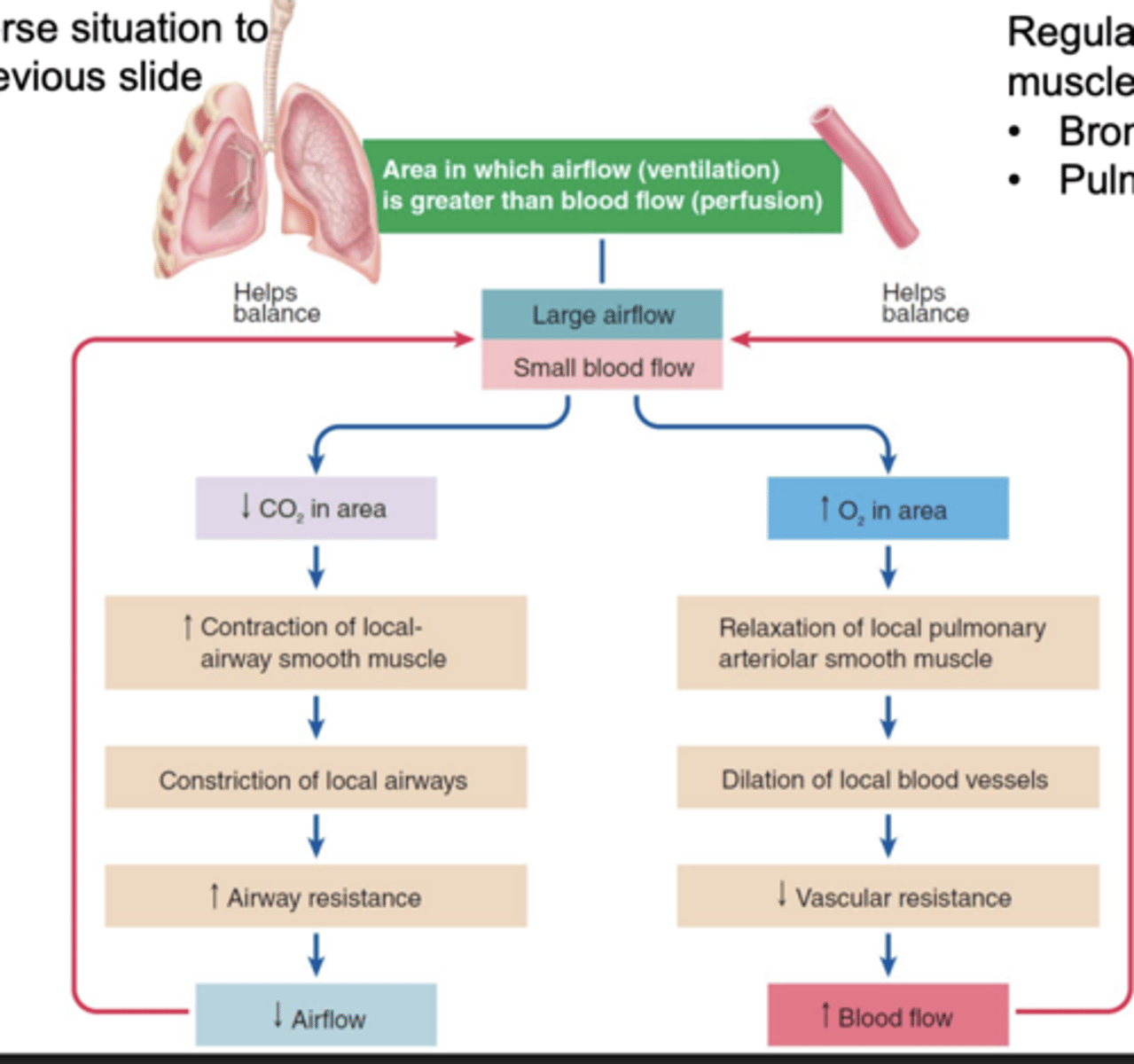
Airflow is regulated by
smooth muscle of the bronchiole
Blood flow is regulated by
Pulmonary arteriole (Smooth muscle)
If there is large blood flow and small airflow

If there is large airflow and small blood flow
Pulmonary circulation makes
gas exchange efficient
Systemic circulation matches
blood supply to metabolic needs
Pulmonary arterioles: Decreased O2
Vasoconstriction
Pulmonary arterioles: Increased O2
Vasodilation
Systemic arterioles: Increased O2
Vasoconstriction
Systemic arterioles: Decreased O2
Vasodilation
Ventilation-perfusion ratio (V/Q ratio)
The efficiency of oxygenation
Ventilation (V) = rate of air flow to alveoli
Perfusion (Q) = rate of capillary blood flow to alveoli
Normal V/Q ratio
0.8 ~1.0
Change from the normal V/Q ratio is called
V/Q mismatch
Ventilation and perfusion flows are not the same across
the lungs
Differences at top and bottom of lungs
Flow rate either airflow or blood flow varies at different lung regions, because of gravity effects, creating a non-constant V/Q ratio
The variable V/Q ratio is considered physiological at the local level. at the level of individual alveoli
Pathological V/Q mismatch cannot be compensated by
local controls
Normal V/Q ratio allows
efficient oxygenation of blood
Decreased V/Q mismatch is often caused by
decreased airflow due to block of alveolar ventilation in pulmonary problems leading to shunting blood flow
- Chronic obstruction pulmonary disease (COPD)
- Pneumonia
Increase V/Q ratio is often caused by
Decrease blood flow due to block of alveolar blood perfusion in vascular problems, leading to functional dead space in airways
- Pulmonary embolism
- Heart failure
Good schematic image V/Q ratios
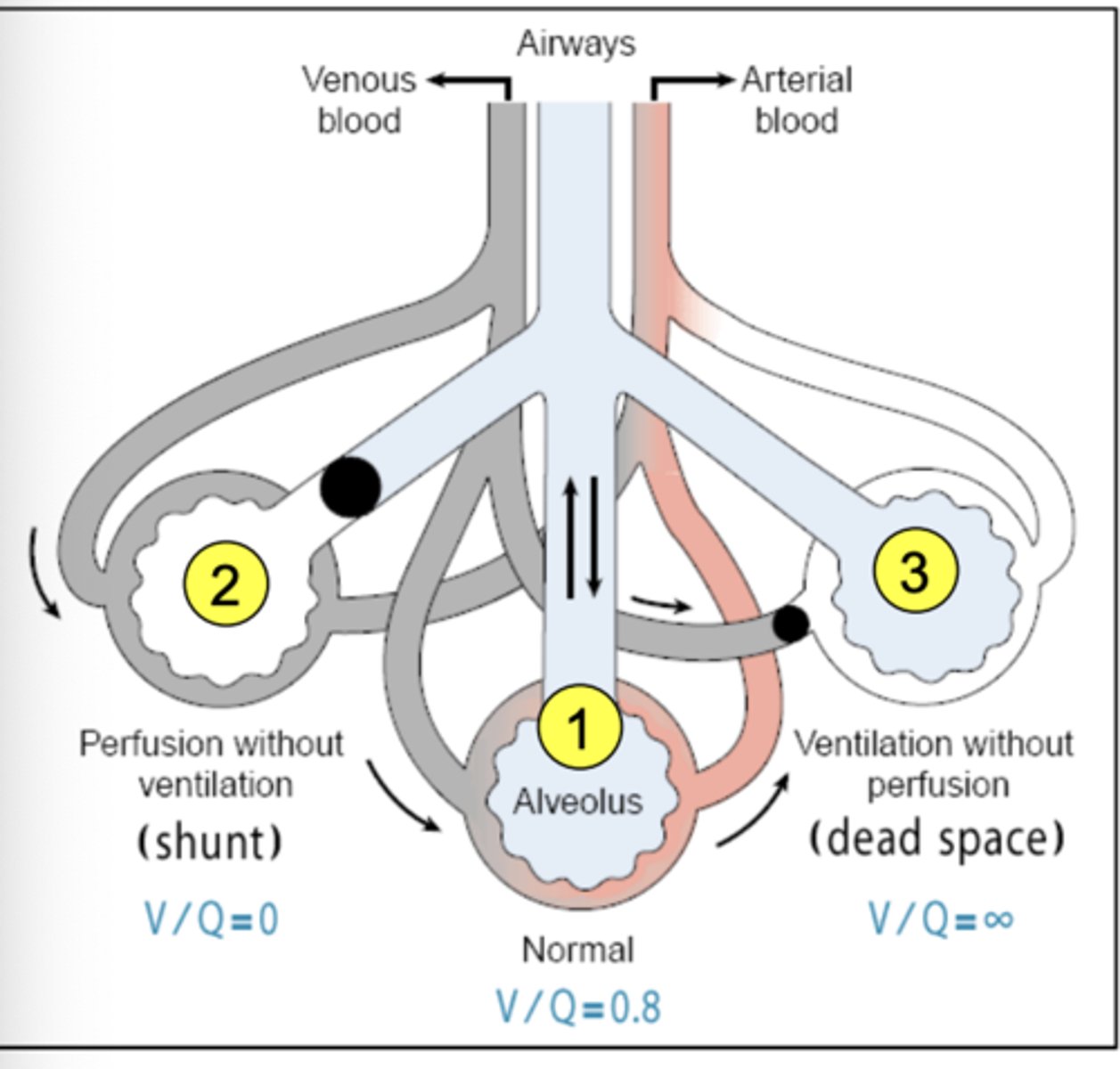
SUMMARY: Physiological changes in ventilation and perfusion can be regulated locally in lung areas, by
bronchiolar and arteriolar smooth muscles, respectively
SUMMARY: The efficiency of blood oxygenation can be expressed as the
ventilation-perfusion ratio (V/Q)
SUMMARY: In V/Q mismatch, the ratio of air flow is not similar to that of
blood flow
SUMMARY: Pathological, low V/Q ratio can be produced by
block of alveolar ventilation. this condition results in shunting of blood flow
SUMMARY: Pathological, high V/Q ratio can be produced by
blocking of alveolar blood perfusion. This condition results in functional dead space in airways. Dead space is the conducting respiratory passageway that does not contribute to gas exchange in the alveoli
Partial pressure
pressure exerted by each gas in a mixture
total pressure x fractional composition of the gas in mixture
Px = Partial pressure of gas x
Henry's law states that the
amount of dissolved gas is proportional to its partial pressure in the gas phase
Each gas within a mixture exerts its own
partial pressure essentially independently of other gases in the mixture
Henry's law: The higher the partial pressure
the higher the concentration of physically dissolved gas
Gas exchange involves simple passive diffusion of
O2 and CO2 down their own partial pressure gradients. From the high to low partial pressure compartments
No active transport mechanism exist for these gases (O2, CO2)
very very very true
Gotta know this figure
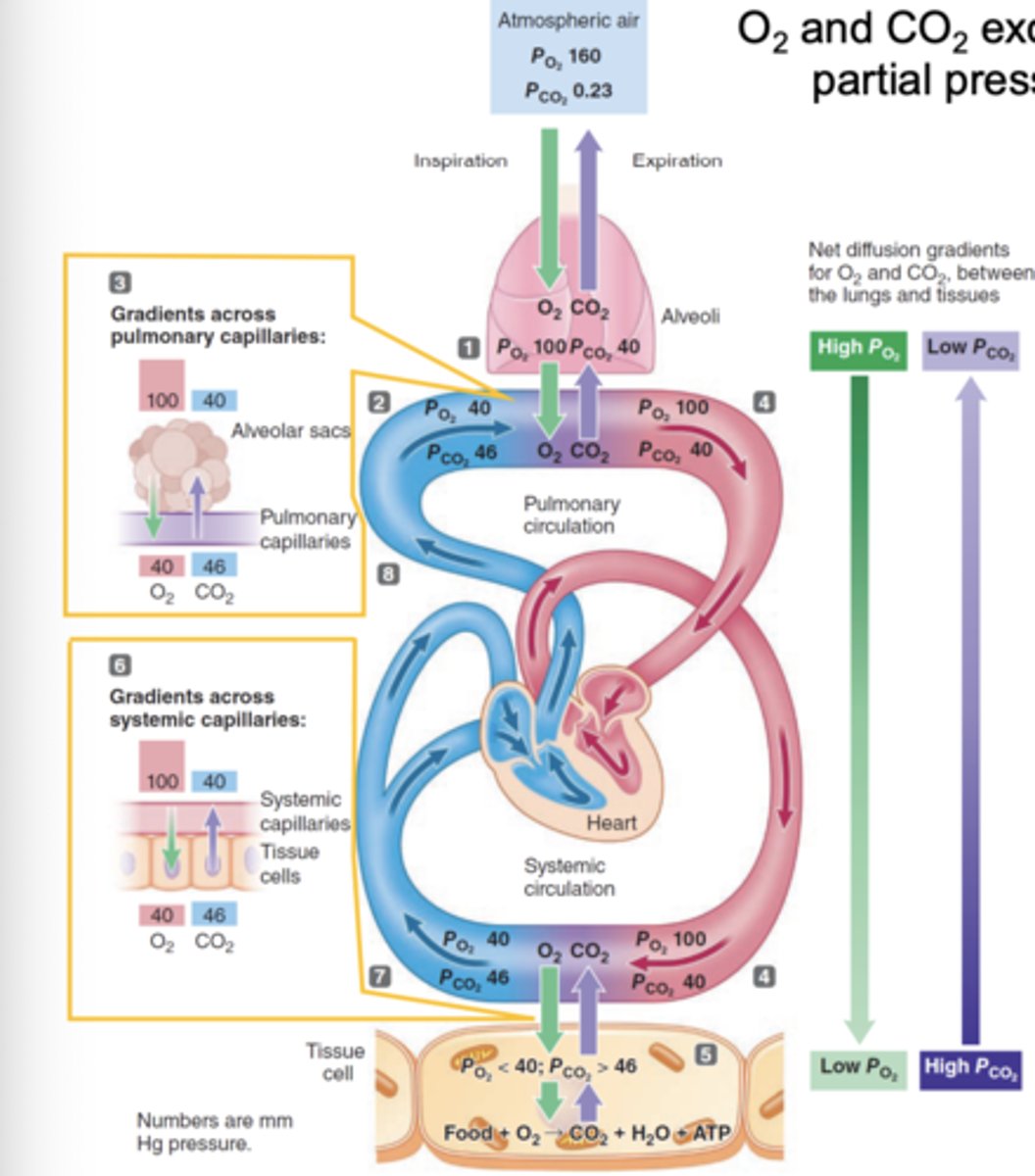
8 Steps of O2 and CO2 exchange caused by partial pressure gradients
1. Alveolar P(O2) remains relatively high and alveolar P(CO2) remains relatively low because a portion of the alveolar air is exchanged for fresh atmospheric air with each breath
2. In contrast the systemic venous blood entering the lungs is relatively low in O2 and O2 and high in CO2 having given up its O2 and picked up CO2 at the systemic capillary level
3. The partial pressure gradients established between alveolar air and pulmonary capillary blood induces passive diffusion of O2 into the blood and CO2 out of the blood until the blood and alveolar partial pressure becomes equal
4. The blood leaving the lungs is thus relatively high in O2 and low in CO2. it arrives at the tissue with the same blood-gas content as when it left the lungs
5. The partial pressure of O2 is relatively low and that of CO2 is relatively high in the O2 consuming, CO2 producing tissue cells
6. Consequently, partial pressure gradients for gas exchange at the tissue level favor the passive movement of O2 out of the blood into the cells to support their metabolic requirements and also favor the simultaneous transfer of CO2 into the blood
7. Having equilibrated with the tissue cells, the blood leaving the tissues is relatively low in O2 and high in CO2
8. The blood then returns to the lungs to once again fill up on O2 and dumb off CO2
Ficks law of gas diffusion

Fick's law: (P1 - P2) Partial pressure gradient
Rate of transfer increases as partial pressure gradient increases
Comment:
Major determinant of rate of transfer
Fick's law: Surface area of the alveolar capillary membrane (A)
Rate of transfer increases as surface area increases
Comment:
Surface area remains constant under resting conditions
Surface area increase during exercise
Surface area decrease with pathological conditions such as emphysema and lung collapse
Fick's law: Thickness of alveolar capillary membrane (T)
Rate of transfer decreases as thickness increases
Comment:
Thickness normally remains constant
thickness increases with pathological conditions such sa pulmonary edema, pulmonary fibrosis, and pneumonia
Fick's law: Diffusion constant (D)
Rate of transfer increases as diffusion constant increases
Comment:
Diffusion constant for CO2 is 20 times that of O2 offsetting smaller partial pressure gradient for CO2; therefore approximately equal amounts of CO2 and O2 are transferred across the membrane
Emphysema
Destruction of alveoli
- Decrease in Surface area
- Increase of thickness
= decrease gas exchange rate
SUMMARY: Exchange of O2 and CO2 between alveoli and capillaries is driven by
partial pressure gradients for each gas
SUMMARY: Dissolved gases flow down their
partial pressure gradients, just as ions flow down their concentration gradients
SUMMARY: The rate of gas transfer across alveolar membranes depends on
Fick's law of gas diffusion
SUMMARY: Fick's law involves four factors
1. Partial pressure gradient of the gas
2. Surface area available for transfer
3. Thickness
4. Diffusion constant of the gas
SUMMARY: The four factors of fick's law are affected upon
various disease conditions
O2 method of transport in the blood
Physically dissolved: contributes to P(O2)- 1.5 %
Bound to hemoglobin - 98.5 %
CO2 Method of transport in the blood
Physically dissolved: contributes to P(CO2) - 10%
Bound to hemoglobin- 30%
As bicarbonate - 60%
Hb is the protein contained in
Red blood cells
Hb is responsible for
delivery of O2 to the tissue
Hb contains _ heme molecules each of which contains an iron ion
4
Each iron can bind
one O2
Each Hb can bind ___ O2
4
When not combined with O2, Hb is referred to as
reduced hemoglobin of deoxyhemoglobin
P(O2) is a primary determinant of percent
hemoglobin saturation with O2
Hb affinity for O2 increases as more O2 molecules become bound this is known as
cooperatively
- Sigmoidal curve
The O2 bound to Hb does not
contribute to P(O2) of the blood
Binding O2 of Hb removes O2 from the
blood
O2 binding Hb reduced P(O2) and maintains
the partial pressure gradient that drives O2 from alveoli into the blood
Hb increases the total content of
O2 in the blood
Oxygen-Hemoglobin dissociation curve is
sigmoidal because the O2-Hb binding is cooperative
A rightward shift of the O2-Hb dissociation curve is due to
Increase P(CO2)
Increase Acid (H+)
Increase Temperature
Increase 2,3-Bisphosphoglycerate
With a rightward shift affinity for O2 is
reduced
O2 saturation decreases slightly at high
P(CO2)
O2 saturation decreases at a large extant at
Low P(O2)
More O2 is unloaded from Hb at a low
P(O2)
2,3-Bisphosphoglycerate production is increased in red blood cells when
Arterial HbO2 is chronically below normal
Ex/
- living at high altitudes
- suffering from disease such as anemia
A leftward shift in the O2-Hb saturation curve is due to
Increased Carbon Monoxide
A leftward shift =
increase Affinity of Hb to O2
Co has 240 times higher affinity for Hb than
O2
Co-hemoglobin is called
Carboxyhemoglobin
When Hb-CO: _________ oxygen is unloaded in the tissues, even when PO2 becomes low. This causes hypoxic tissue injury
Little
CO is _________ because it is odorless, colorless, tasteless, and nonirritating
not detectable
SUMMARY: 98.5% of O2 in blood is transported in a form
bound to hemoglobin
SUMMARY: hemoglobin is a tetrameric heme-containing protein that can bind
4 O2 molecules per hemoglobin complex
SUMMARY: binding of O2 to Hb removes it from the blood thus
reducing PO2. this helps maintaining the pressure gradient to drive O2 from alveoli into the blood
SUMMARY: Oxygen Hemoglobin dissociation curve describe how
O2 is bound to Hb at alveoli and how O2 is unloaded to tissue
SUMMARY: Hb affinity for O2 is reduced when
Increase PCO2
Increase Acid
Increase Temperature
Increase 2-3-BPG
Leads to a rightward shift of the curve and to efficient unloading of O2 at peripheral tissues
SUMMARY: The effect increase PCO2 and Increase H+ on the O2-Hb dissociation curve is known as the
Bohr effect
SUMMARY: CO induces a
left-ward shift of the O2-Hb saturation curve, and inability of Hb to unload O2 at tissues
Approximately 6-% of CO2 is carred in the blood as
bicarbonate ion
In RBC the enzyme _______ catalyzes the rapid conversion of CO2 and H+ and Bicarbonate
carbonic anhydrase
Spontaneous reaction in the blood of CO2 and H2O is
Catalyzed reaction in RBC of CO2 and H2O is
Slow
Fast
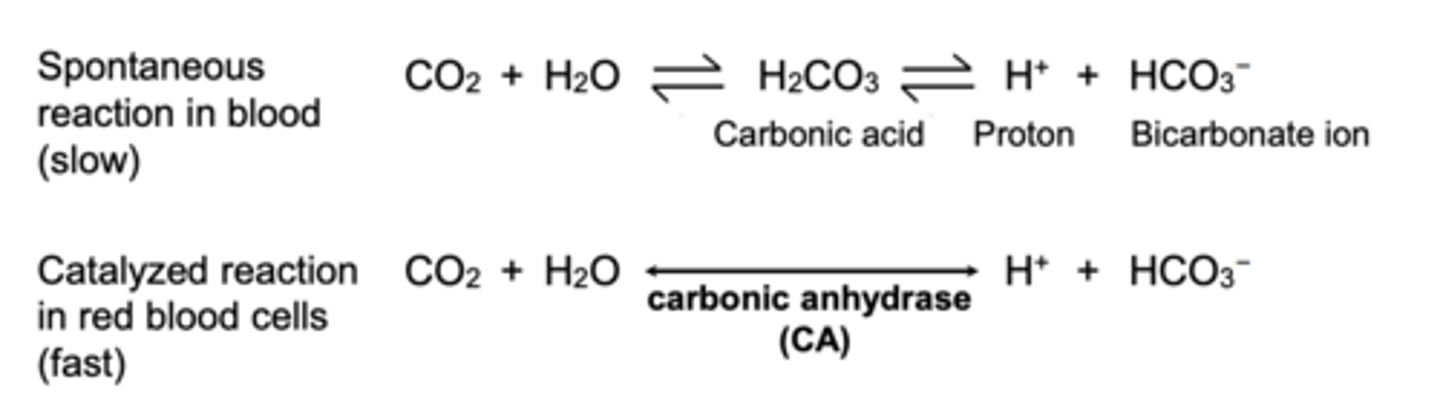
Law of mass action
If the concentration of one substance involved in a reversible reaction is increased the reaction is driven toward the opposite side
Conversely, if the concentration of one substance is decreased the reaction is driven toward that side
Three ways of transporting CO2 from tissues to lungs
Bohr effect: Increased O2 unloading by Increase CO2 and H+
Haldane effect: Hb binding with CO2 and H+ inducing O2 unloading
Hb passengers: O2 to tissue; CO2 and H+ to lungs
SUMMARY: CO2 is produced in the tissue, diffuses into the bloodstream and is transported to the lungs for excretion
yea true
SUMMARY: CO2 is transported in the blood primarily as
HCO3 (bicarbonate) or bound to Hb.
Only 10% is dissolved in plasma
SUMMARY: Since CO2 is quickly converted to bicarbonate by ________, this reaction allows for the continued uptake of CO2 into the blood, down its concentration gradient
Carbonic anhydrase
SUMMARY: Hb plays a key role: Hb carries O2 and CO2, and binds H+ that results from
bicarbonate production
SUMMARY: CO2 bound directly to Hb is called
Carbaminohemoglobin
SUMMARY: The Bohr effect
describes the role of increased CO2 and H+ in tissue, in inducing the unloading of O2 from Hb
SUMMARY: The Haldane effect
Describes the role of the unloading of O2 from Hb in freeing Hb to bind with CO2 and H+, allowing them to be carried to their common destination: lungs
Chronic Obstructive pulmonary disease (COPD) includes
emphysema and chronic bronchitis and they often occur together
COPD is a chronic inflammatory lung disease that causes
obstructed airflow from the lungs and breathing-related problems
COPD symptoms include
Breathing difficulty
Cough
Mucus production
Wheezing
COPD is typically caused by
long-term exposure to irritating gases or particulate matter, most often from cigarette smoke
Emphysema
a condition in which the alveoli are destroyed
Chronic bronchitis
inflammation of the lining of the bronchi and bronchioles. Characterized by daily cough and mucus (sputum) production