brainstem and motor cortex
contralateral innervation
right side of brain goes with left sides movements and vice versa
brainstem
houses reticular activation formation
cranial nerves synapse with CNS (UMNs to LMNs) at cranial nerve nuclei (III-VII)
superior to inferior: midbrain, pons, medulla
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
38 Terms
contralateral innervation
right side of brain goes with left sides movements and vice versa
brainstem
houses reticular activation formation
cranial nerves synapse with CNS (UMNs to LMNs) at cranial nerve nuclei (III-VII)
superior to inferior: midbrain, pons, medulla
midbrain
superior section of brainstem
houses afferent and efferent pathways
houses cranial nerve nuclei
houses substantial nigra
controls pupil size, auditory reflexes, and reflexive eye movement
substantia nigra
part of brain that produces a neurotransmitter called dopamine (brain needs this to function normally
pons
middle structure of brainstem
houses afferent and efferent pathways
houses cranial nerve nuclei
houses respiratory center
swallow center
controls autonomic rhythm of respiration
medulla
Inferior section of brainstem
Houses afferent and efferent pathways
Houses cranial nerve nuclei
Point of decussation of UMNs coursing to spinal nerves.
Also Swallow Center
Also houses Respiratory Center
Controls: Autonomic respiratory activity, Heart rate, Blood pressure
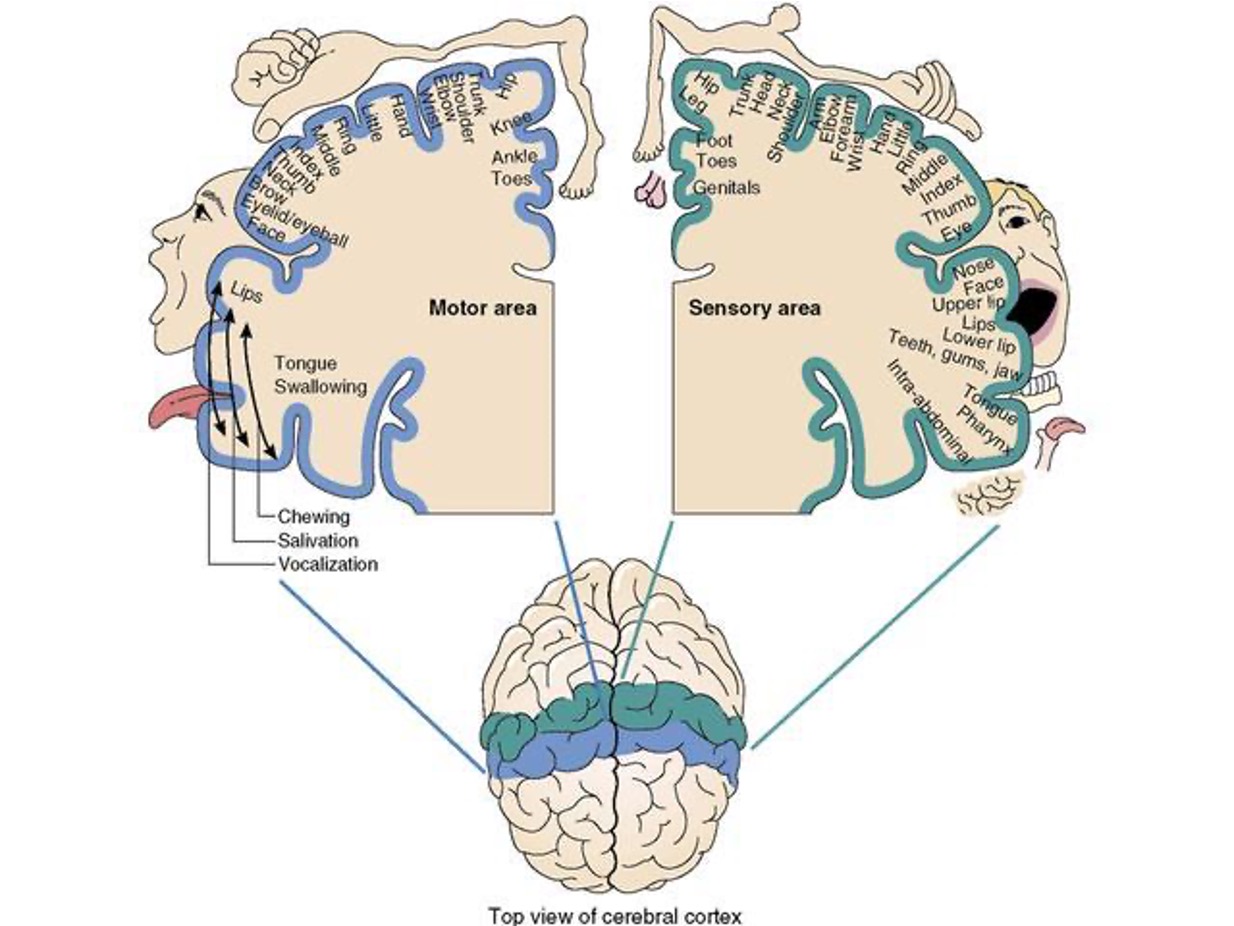
cortical representation of body
The finer the movement of the body parts- the more cortex is dedicated/needed to generating motor plans for this body part.
The more gross the movement of the body parts- the less cortex is dedicated/needed to generate motor plans.
closed head injury
the skull was not penetrated – brain has been damaged inside the skull (generally large parts of the brain have been damaged ex: car wrecks, falls, etc.)
open head injury
skull has been penetrated, and the brain has been damaged (generally impacts a certain area only, ex: gunshot wound to the head)
what is the cerebellum often called
little brain
role of the cerebellum
Equilibrium (eyes, ears, brain), posture, and…
Timing of movement
Synchronization individual components of movements
Scales and Coordinates muscle contractions in both:
Stereotyped (repetitive) movement (e.g., gait)
Non stereotyped movement (e.g., reaching for something)
Error Control Device
Monitors ongoing motor plans
Compares intent of movement, with motor plans, afferent info, and makes adjustments
Corrects for overshooting and undershooting; compensates forerrors before they occur. (as in reaching for something).
Receives ongoing sensory information concerning activity and compares that information to intention and makes corrections as needed. (compares action to intent)
The more rapid, alternating, sequential, or precise the activity the more cerebellar function is required
For speech - allows smooth flow of movement from one articulatory position to the next.
cerebellar anatomy
Two hemispheres
Cerebellar hemispheres have contralateral connections to thalamus and cerebral hemispheres.
Connect at midline - Vermis
Attached at Pons via peduncles
Information arrives via middle and inferior cerebellar peduncles, connects to pathways from: the spinal cord, vestibular system, motor control areas
Superior cerebellar peduncle- Purkinje cells- primary cerebellar output
Output from cerebellum travels via superior cerebellar peduncle to reach the spinal cord, thalamus, and cerebral cortex.
CVA
vertobrobasilar artery supplies cerebellar arteries
toxicity in cerebellar pathologies
hypercapnia
chronic ETOH
progressive cerebellar degeneration
Friedrich’s
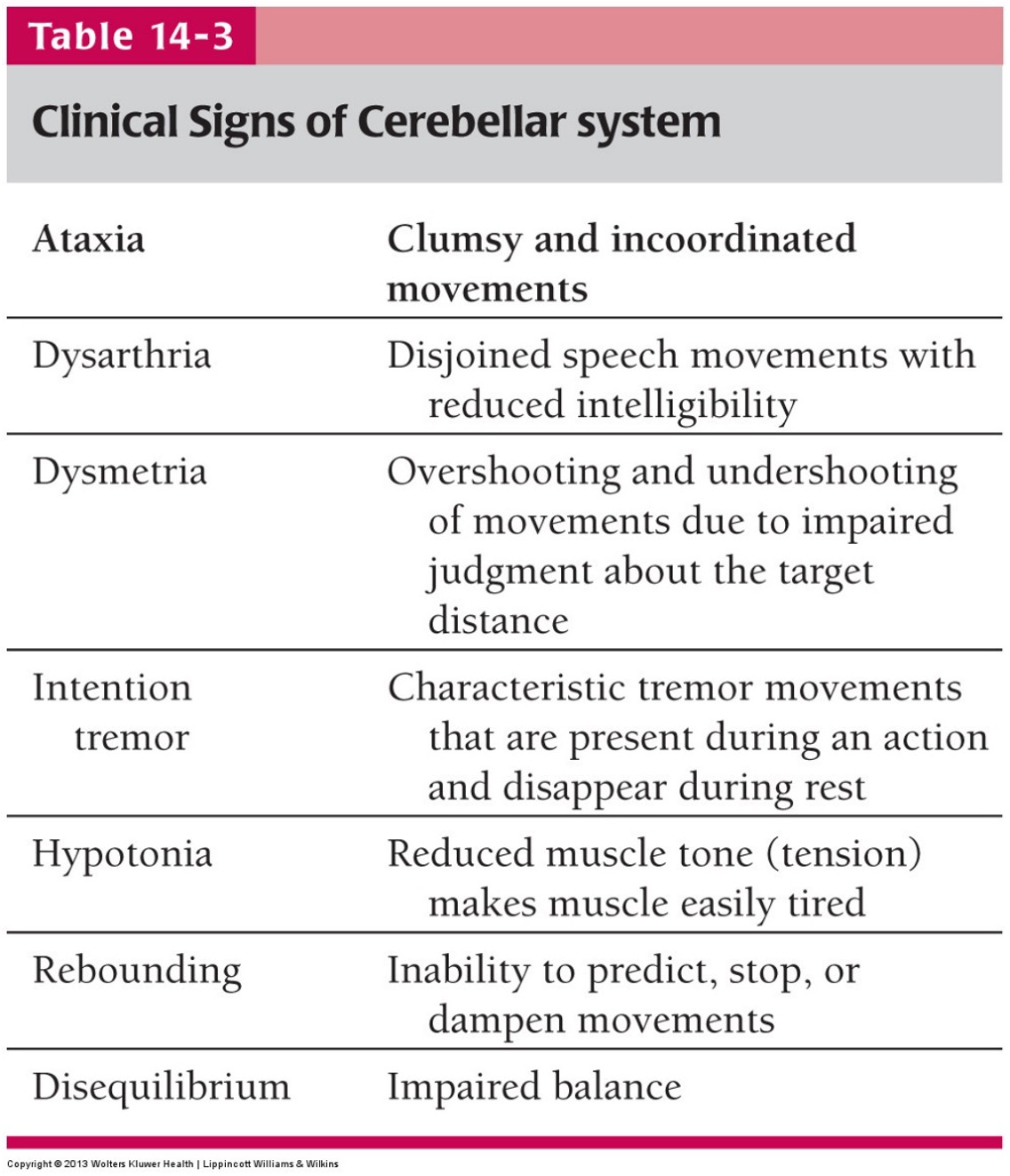
Cerebellum lesion effects
Decomposition of movement into component parts
Errors in rate and range of movement
Errors in speech are likely when you have cerebellum lesions
Dysmetria: Patients overshoot or undershoot what they’re reaching for
Cerebellar Lesion Effects
Speech may sound as if person is inebriated
Ataxic dysarthria*- damage to the cerebellum
Difficulty regulating movement, but not paralysis
Broad based discoordinated gait
Hypotonia(low muscle tone)
ataxic dysarthria
damage to the cerebellum
signs of ataxia
clumsy and uncoordinated movements
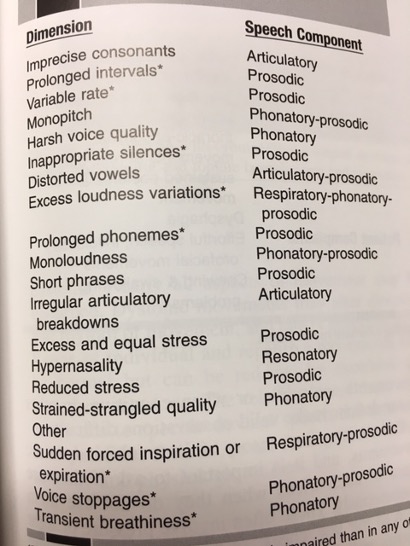
ataxic dysarthria speech characteristics and patient complaints
drunk sounding speech
biting tongue or cheek
speech deteriorates inordinately with alcohol
Speech Characteristics:
excessive loudness
irregular articulatory breakdowns
irregular AMRs
Distorted vowels - tongue not in right place
excess/equal stress
prolonged phonemes
role of basil ganglia
Assist in regulating/refining raw motor plans assembled at cortex
Inhibit extraneous involuntary movements
Modulate automatic movement
Arm swinging during gait
Automatic facial expressions
Postural stretch reflexes (anti-gravity reflexes)
primary functions of basal ganglia
(IAP)-Regulate muscle tone.
(IAP)-Posture- static muscle contraction.
(DAP)-Dampen/modulate extraneous movements in raw volitional motor plans.
Also involved in new motor learning and motor initiation
anatomy of the basal ganglia
Has functional connections to substantia nigra
Three primary components
Striatum
1. Caudate nucleus
2. Putamen
3. Globus Pallidus
Internal
External
clinical manifestations of basil ganglia involvement
Clinical manifestation (fig 15-1)
vary depending on specific structures or loops affected
Which varies according to specific pathology (etiology)
Damage to BG or circuitry
Not spastic or flaccid paralysis
Loss of automatic BG inhibition of motor control
Release of hyperkinesias (INVOLUNTARY MOVEMENT)
Athetosis, ballism, chorea, tremor, dystonia, myoclonus, etc…
Hypokinesia- Inappropriate inhibition (reduction in tone, force, ROM) of volitional movements.
hypertonia
too much muscle tone
hypotonia
too little muscle tone
hyperreflexia
too many reflexes
hyporeflexia
too little reflexes
hyperkinesia
too much involuntary movement
hypokinesia
too little volitional movement
hyperkinetic dysarthria
speech disorder caused by too much involuntary movement
hypo kinetic dysarthria
speech disorder caused by too little volitional movement
some diseases of the basil ganglia
parkinson’s disease
huntington’s chorea
Wilson’s disease
progressive supra nuclear palsy
Parkinson’s Disease
Death of substantia nigra
Dysfunction of BG
Onset usually unilateral
Release of involuntary tremors (hyperkinesia)
Prognosis varies but usually about 10-15 years post onset
Overinhibition of voluntary movements (hypokinesia)
Parkinson’s disease characteristics
Shuffling gait
Tremors present
Hypomimia- blank facial expression
Hypokinetic dysarthria
hypokinetic dysarthria
Dysarthria is something that you hear, you can’t see itbut you might see the hypokinesia that causes it but cannot see the dysarthria. Dysarthria is a speech disorder.
More homogenous presentation than hyperkinetic dysarthria
speech characteristics of hypokinetic dysarthria
Monopitch
Monoloud
Breathy voice*
Low pitch
Reduced Stress
Variable rate
Short rushes of speech*
Increase rate of speech*
Imprecise consonants
Articulatory blurring
hyperkinetic dysarthria
Damage to the basal ganglia can lead to this
Any hyperkinesia which interrupts or inhibits normal speech
Will vary according to the hyperkinesia type and intensity that is affecting speech.
Can present in a myriad of ways
General dysarthria characteristics:
mixed hypo-hyperkinetic dysarthria
Combined
Hypokinesia- reduction in volitional movement affecting speech
Hyperkinesia- Addition of nonvolitional movement speech