Lecture 17 - Immunity at Mucosal Surfaces
1/94
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
95 Terms
the mucosal immune system
protected by an epithelial barrier
enormous antigen load
key mucosal sites
GI tract (largest immune organ)
Respiratory tract
urogenital tract
lacrimal, salivary, mammary glands
the mucosal immune system
covers ~400m2 of surface area (vs 2m2 of skin)
constantly exposed to food ags, commensals, pathogens, and environmental particles
requires tight epithelial barrier function
must balance tolerance (food/microbiota) and immunity (pathogens)
core challenges of the mucosal immune system
enormous ag load
risk of inflammation → tissue damage → loss of barrier
different types of epithelium line barrier tissue
mucosae - simple columnar epithelium, pseudostratified columnar epithelium, nonkeratinized stratified squamous epithelium
skin - keratinized stratified squamous epithlium
what does the type of epithelium a tissue uses tell us
the type of epithelium a tissue uses is the first clue to the kind of immune defenses it needs - different types depending on the organ
all epithelia face what
enormous ag load - pathogens, food ags, commensal bacteria (friendly ags)
what type of epithelium does the intestine have and what are some features
intestine has simple columnar epithelium
microvilli increase absorption
goblet cells secrete mucus
what type of epithelium does the respiratory tract have and what are some features
respiratory tract has pseudostratified columnar epithelium
ciliated epithelium + mucus clearance
what type of epithelium does the oral cavity and esophagus have and what are some features
nonkeratinized stratified squamous epithelium
protects against friction, non-drying surfaces
what type of epithelium does skin have and some features
keratinized stratified squamous epithelium
tough, water-resistant outer layer
distinctive features of the mucosal immune system
anatomic features
effector mechanisms
immunoregulatory environment
examples of anatomic features of the mucosal immune system
intimate interactions between mucosal polarized epithelia and lymphoid tissues
discrete compartments of diffuse lymphoid tissues and more organized structures such as peyer’s patches, isolated lymphoid follicles, and tonsils
specialized antigen-uptake mechanisms, e.g. M cells in Peyers patches, adenoids, and tonsils
broad surface area in contact with environmental agents/microbes
examples of effector mechanisms of the mucosal immune system
activated/memory T cells predominate even in the absence of infection
multiple activated ‘natural’ effector/regulatory T cells present
production of mucins and mucus
secretory IgA antibodies
production of antimicrobial peptides (AMPs)
presence of distinctive microbiota
examples of immunoregulatory environment in mucosal immune system
active down-regulation of immune responses (e.g. to food and other innocuous antigens) predominates at homeostasis
inhibitory macrophages and tolerance-inducing dendritic cells
high number of FoxP3+Treg cells and FoxP3-Tr1 cells
mucosal infections are one of the biggest global health problems true or false
true
why are mucosal infections one of he biggest global health problems
many major pathogens enter through mucosal surfaces:
respiratory tract (influenza, SARS-CoV-2, RSV, TB)
gastrointestinal tract (cholera, rotavirus, norovirus)
urogenital tract (HIV, HPV, gonorrhea, chlamydia)
most infectious diseases that kill humans do so how
because they breach a mucosal barrier first
Organization of the Mucosal Immune System
MALT (Mucosa-associated lymphoid tissues)
NALT
tonsils, adenoids
strong Th1/Th17 responses to respiratory viruses
BALT
inducible in adults
site of TB priming in lung
GALT
peyers patches, isolated lymphoid follicles, and appendix
oral tolerance, IgA, defense against enteropathogens
where else is MALT present
also present in urogenital tract (HIV entry & STI immunity), mammary gland, conjunctiva
induction sites of the mucosal immune system
where the mucosal immune response is initiated
GALT
BALT
NALT
urogenital tracy
lacrimal glands
salivary glands
mammary glands
Effector sites of the mucosal immune system
where the mucosal immune response is carried out
lamina propria (plasma cells, T cells, ILCs)
epithelium (intraepithelial lymphocytes, goblet cells, Paneth cells)
IgA-producing plasma cells
mucus secretion, AMP production, barrier fortification
peyers patch → induction →
villus/crypt regions → effector response
specialized epithelium overlying intestinal lymphoid tissues takes up particulate antigens - examples
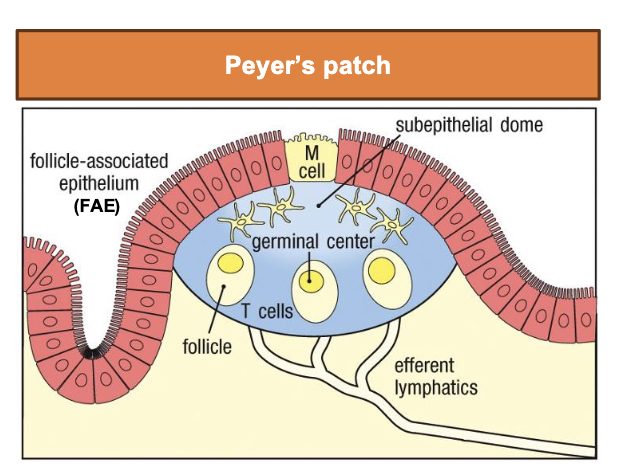
Peyer’s Patch
M cell: microfold cell - transport ag from lumen
FAE (follicle associated epithelium) lack thick mucus → easier to access for ag sampling
subepithelial dome rich in DCs and lymphocytes
leads to activation of B and T cells in germinal centers
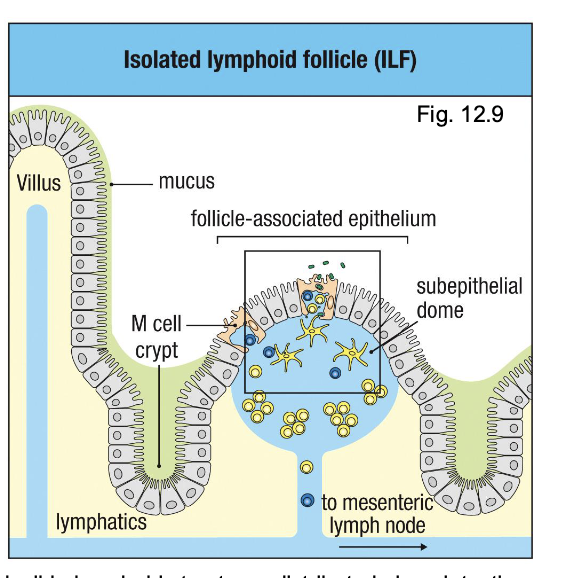
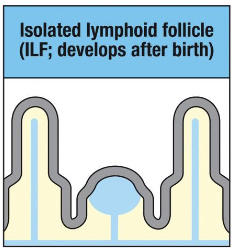
Isolated Lymphoid follicle (ILF)
smaller inducible lymphoid structures distributed along intestine
also contain M cells overlying lymphoid follicles
sample ag and deliver it to underlying DCs
connect to mesenteric lymph nodes via lymphatics
isolated lymphoid follicles mech
smaller inducible lymphoid structures distributed along intestine
also contain M cells overlying lymphoid follicles
sample ag and deliver it to underlying DCs
connect to mesenteric lymph nodes via lymphatics
Peyer’s patch mech
M cell: microfold cell - transport ag from lumen
FAE (follicle associated epithelium) lack thick mucus → easier to access for ag sampling
subepithelial dome rich in DCs and lymphocytes
leads to activation of B and T cells in germinal centers
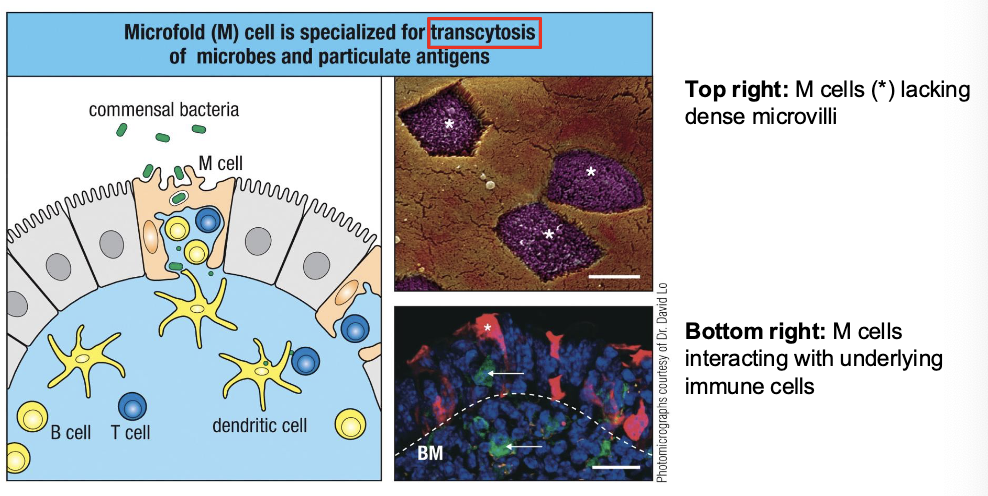
what do M cells do
take up commensal bacteria, pathogens, and particles from the gut lumen
transport (transcytose) them across the epithelium
deliver ags directly to B cells, T cells, and DCs in the subepithelial dome
enable rapid initiation of mucosal immune response
inductive sites of GALT
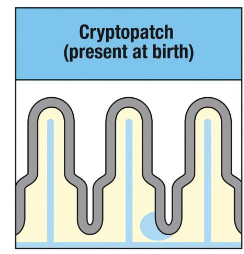
cryptopatches
ILFs
Peyers patches
cryptopatches of GALT
(present at birth)
small clusters of DCs and lymphoid tissue-inducer (LTi) cells
ILFs of GALT
develop after birth
expand in response to microbial colonization
Peyers patches in GALT
present at birth but grow and mature postnatally
require microbial signals for full development
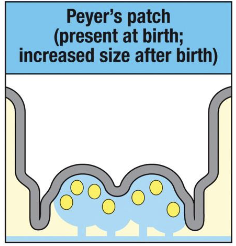
Germ-free mice have what
poorly developed Peyer’s patches
no ILFs
decreased IELs
decreased IgA-secreting plasma cells
decreased AMPs
decreased immune mediators (cytokines)
maturation of GALT is driven by what
acquisition of commensal microbiota
what may impair GALT impairment
early-life antibiotics may impair GALT development
cesarean delivery alters initial microbial colonization
dysbiosis can drive IBD, food allergies, asthma (systemic effects)
effector sites of GALT
intestinal epithelium
lamina propria
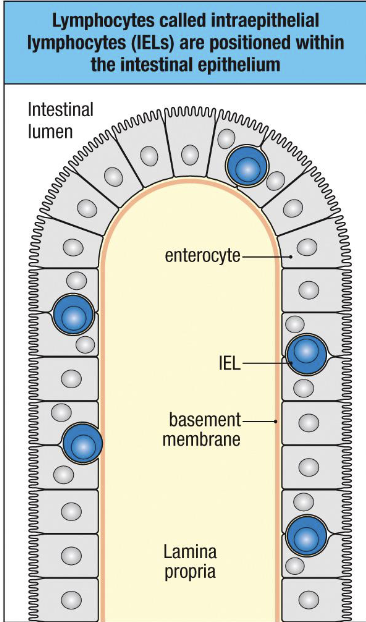
intestinal epithelium
(single cell layer)
IELs (or IETs) - mostly CD8+, no B cells, ILCs
produce AMP, cytokines
interacts directly with commensals, sIgA, nutrients
lamina propria
Rich in innate cells (macrophages, DCs, ILCs), CD4+ and CD8+ T cells
B cells and IgA-secreting plasma cells
Tregs
site of most IgA production and immune effector activity
which of the following is a characteristic feature of mucosal surfaces
a) low antigen exposure
b) highly keratinized epithelium
c) constant exposure to food and microbial antigens
d) absence of immune cells
c) constant exposure to food and microbial antigens
what is the major function of M cells
a) produce antimicrobial peptides
b) facilitate antigen transport to immune cells
c) maintain tight junctions
d) secrete mucus
b) facilitate antigen transport to immune cells
goblet cell-associated antigen passages primarily promote:
a) Th1 immunity
b) IgG class switching
c) Oral tolerance
d) viral cytotoxicity
c) oral tolerance
innate immune defenses of intestinal immune system
absorptive subsets
secretory subsets
absorptive subsets
a. enterocytes (nutrient absorption, sense microbes via TLRs, secrete cytokines)
b. M cells
Secretory subsets
a. goblet cells - mucus
b. paneth cells - AMPs
c. enteroendocrine cells - hormones and neuropeptides
d. tuft cells - cytokines and lipid mediators - imp. in parasite response and type 2 immunity
mucus in the gut is
viscous, slippery and sticky
negatively charged → retains sIgA and AMPs
substrate for commensals
major component - mucins (MUC2)
mucus in small int. compared to mucus in large int.
in small: thin
in colon: much thicker and organized into two layers:
inner layer: highly cross-linked, dense, and impenetrable to bacters
outer layer: looser, less cross-linked, and supports commensal (good) bacteria
glycocalyx
carbohydrate rich layer directly coating epithelial cells
intestinal epithelium is not just a barrier, but
an active immune organ composed of specialzed innate cell types
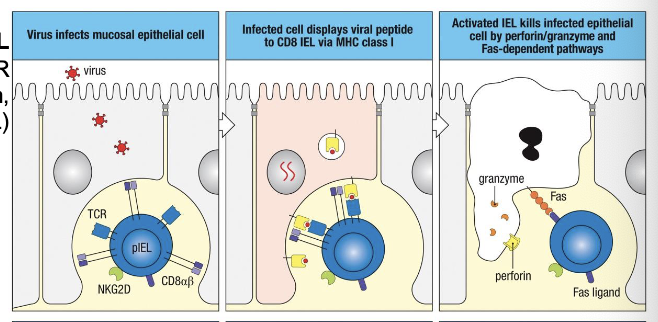
IELs provide what
rapid, front-line defense at the mucosal barrier
include conventional CD8+ T cells and unconventional (innate-like) T cells
Type A IEL
function like CTL (TCR activation → perforin, granzyme, FasL
Type B IEL
function like NK cells (act independently of TCR activation through NKG2D)
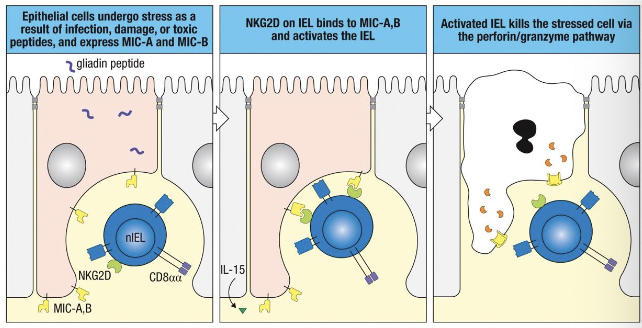
loss of dysfunction of IELs contributes to
Celiac disease
chronic infections
barrier breakdown in IBD
lymphocytes called intraepithelial lymphocytes (IELs) are positioned where
within the intestinal epithelium
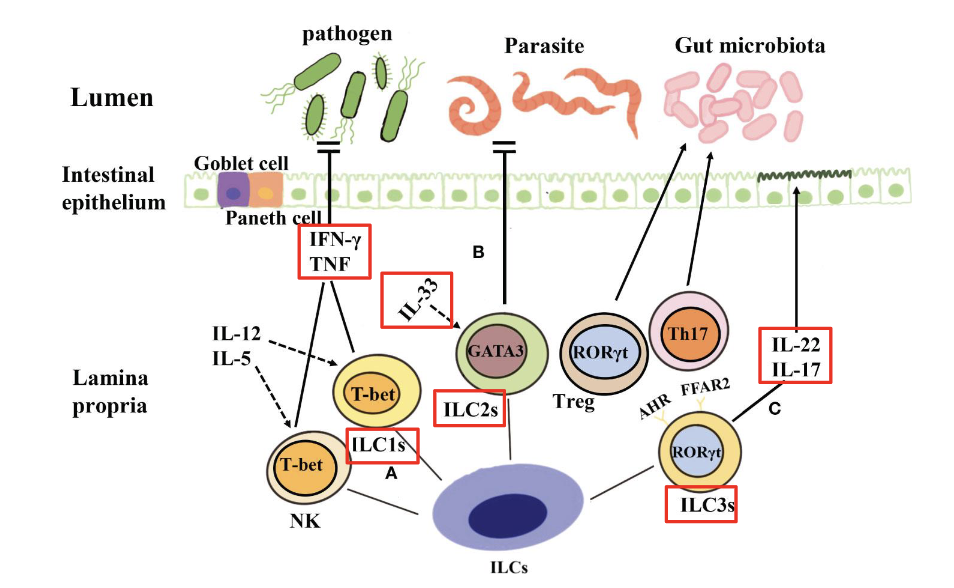
ILCs in GALT respond to what
microbes that breach epithelium
ILCs
abundant in mucosal tissues (especially intestine)
mirror helper T cell subsets in cytokine profiles
activate without antigen-specific TCRs (respond to cytokines + epithelial signals)
excess ILC1 →
chronic inflammation, Crohn’s disease associatin
Excess ILC2 →
allergies, asthma, eosinophilic GI disease
excess ILC3 →
IL-17 driven inflammation, IBD
reduced ILC3 →
loss of IL-22 → weak barrier → dysbiosis
mucosal immune system establishes & maintains what
tolerance to harmless Ags
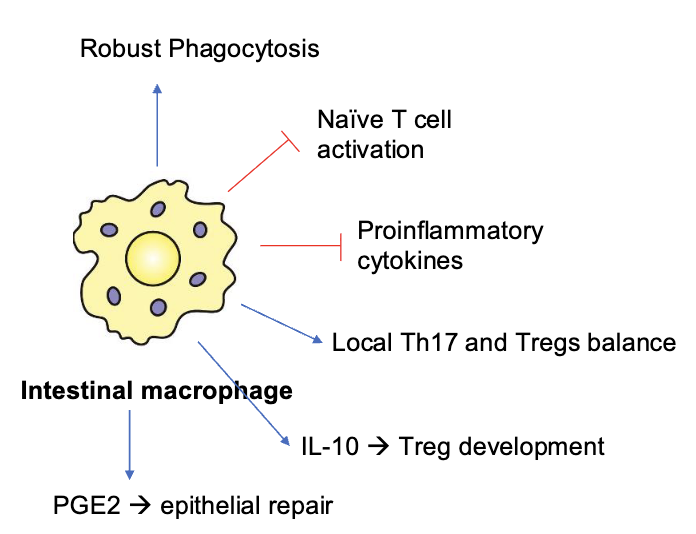
what do intestinal macrophages do
robust phagocytosis
they’re excellent at engulfing bacteria and debris
But, they don’t trigger inflammation
they don’t activate naïve T cells (red inhibitory lines)
they produce very little proinflammatory cytokines
instead, they promote tolerance
how do intestinal macrophages promote tolerance
they produce IL-10, which:
encourages Treg (regulatory T cell) development
helps maintain balance between Th17 and Treg cells
they produce PGE2, which
helps with epithelial repair (healing the gut lining)
overall, intestinal macrophages do what
overall, intestinal macrophages clean up microbes while preventing unnecessary inflammation
gut dendritic cells what do they do?
capture food antigens and commensal bacteria
present these antigens to CD4 T cells in a non-inflammatory way (teaches immune system these are safe)
promote
Treg differentiation → more regulatory T cells = more tolerance
IgA class switching in B cells → B cells make IgA, the antibody specialized for the gut → IgA coats microbes and food antigens without causing inflammation

tolerogenic phenotype
both macrophages and DCs in the gut are designed to prevent overreaction.
promote IL-10, Tregs, and IgA
avoid inflammation
maintain gut homeostasis
tolerate harmless substances (food + commensals)
this protects you from chronic inflammation and allows peaceful coexistence with the microbiome
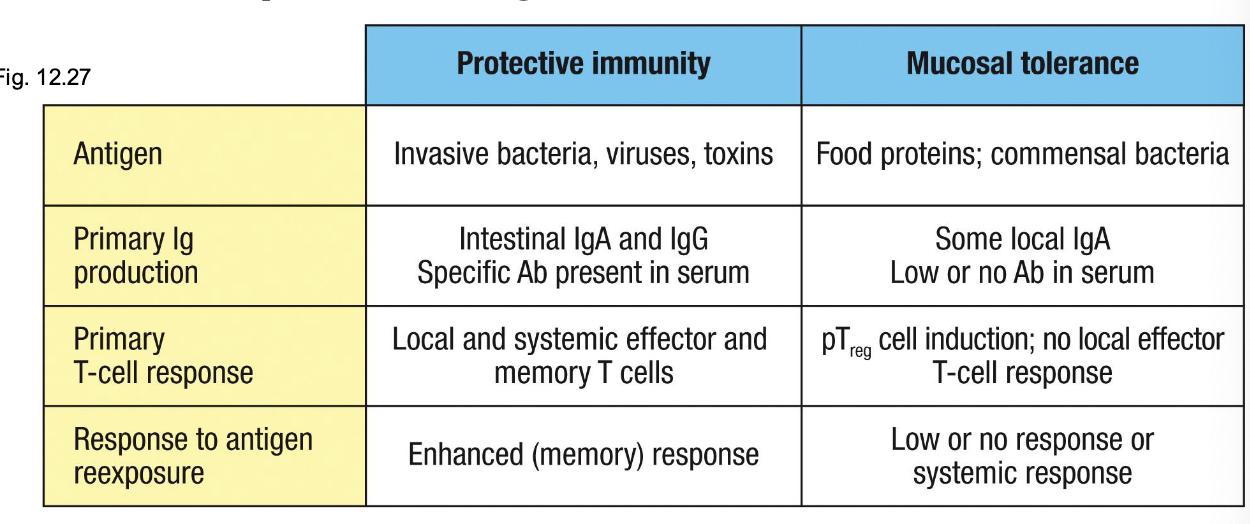
immune priming and tolerance are what
different outcomes of intestinal exposure to Ag
the same ag delivered orally can generate immunity or tolerance depending on what
danger signals and context
Pathogens → PAMPs → danger → immunity
Food + commensals → no PAMPs → steady-state DC signals → tolerance
why commensals don’t trigger inflammation even though they have PAMPs
spatial segregation: mucus, sIgA, and AMPs keep commensals away
epithelial TLRs are compartmentalized
specialized tolerogenic phagocytes
microbial metabolites instruct tolerance
absence of contextual danger - danger is not just pathogen or PAMP, true danger: PAMP/DAMP + barrier breach + inflammatory cytokines
intestinal epithelial cells express TLRs in strategic, non-reactive ways:
TLR5 on basolateral surface only
TLR9 can produce tolerogenic signals (IL-10) when signaling from apical side
TLR4 is often low or absent on apical membrane
Thus, commensal PAMPs hitting apical TLRs → tolerance, not inflammation
routes of antigen uptake in the intestine
*the gut does NOT rely on just one mechanism to sample antigens; it uses multiple, highly specialized routes depending on ag type
M cells
Paracellular transport
FcRn: neonatal Fc receptor
Goblet cells
Apoptosis-Dependent Transfer
TEDs
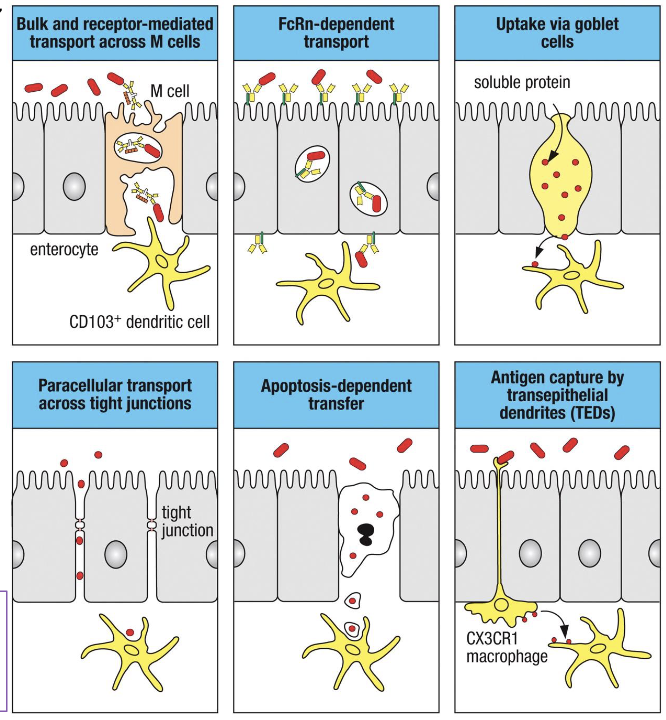
M cells
bulk and receptor-mediated transcytosis of microbes and particles.
deliver ags to CD103+ DCs beneath
FAE
paracellular transport
limited ag diffusion between epithelial cells
occurs when tight junction sare physiologically ‘open’ or mildly loosened
controlled, not pathological
FcRn: neonatal Fc receptor
transports IgG-ag complexes across enterocytes
allows sampling of luminal antigens bound to maternal IgG (neonates) or endogenous IgG
goblet cells
can deliver soluble proteins to underlying tolerogenic DCs
important for oral tolerance to food ags
apoptosis dependent transfer
IECs undergoing apoptosis release antigenic material
phagocytosed by local DCs & macrophages
TEDs
CX3CR1+ macrophages extend dendrites between epithelial cells into the lumen
capture bacteria or particles directly
important for commensal sampling and early pathogen sensing
Tregs in mucosal Tissue balance what
active immunity vs. immunological tolerance

during pathogenic exposure
pathjogens trigger innate and adaptive immune activation
effector T cells, ILCs, macrophages, and antibodies clear infection
Tregs prevent excessive tissue damage during the response
during exposure to innocuous Ags
Tregs enforce tolerance and suppress unnecessary inflammation
prevent local and systemic immune reactivity
protect epithelial barrier integrity
Tregs suppress effector responses through:
IL-10 (suppresses DCs, Th1, Th17, macrophages)
TGF-B (promotes IgA class switching + epithelial repair)
CTLA-4 (removes co-stimulatory molecules from DCs)
IL-2 consumption (starves effector T cells)
Amphiregulin (creates tissue repair microenvironment)
loss of mucosal Treg function contributes to
IBD
celiac disease
food allergy
autoimmune disorders
chronic infections
HIV mucosal dysfunction
which cytokines are characteristic of ILC3 responses?
a) IFN-gamma and TFN
b) IL-5 and IL-13
c) IL-22 and IL-17
d) IL-10 and TGF-B
c) IL-22 and IL-17
oral tolerance is primarily mediated by which cell type
a) Th1 cells
b) FoxP3+ Tregs
c) NK cells
d) ILC1
b) FoxP3+ Tregs
Transcytosis of IgA across epithelia is mediated by what
polymeric Ig receptor (pIgR)
steps of transcytosis of IgA across epithelia
binding (basolateral surface) - Dimeric IgA (with J chain) binds to plgR on the basolateral side of epithelial cells
Endocytosis - The plgR-IgA complex is internalized into the epithelial cell
Transcytosis - vesicles move the complex across the cell toward the apical surface
release (apical surface) - plgR is cleaved, IgA is released into the lumen as secretory IgA (sIgA). sIgA = IgA dimer + secretory component (cleaved part of the pIgR), which protects IgA from proteolysis
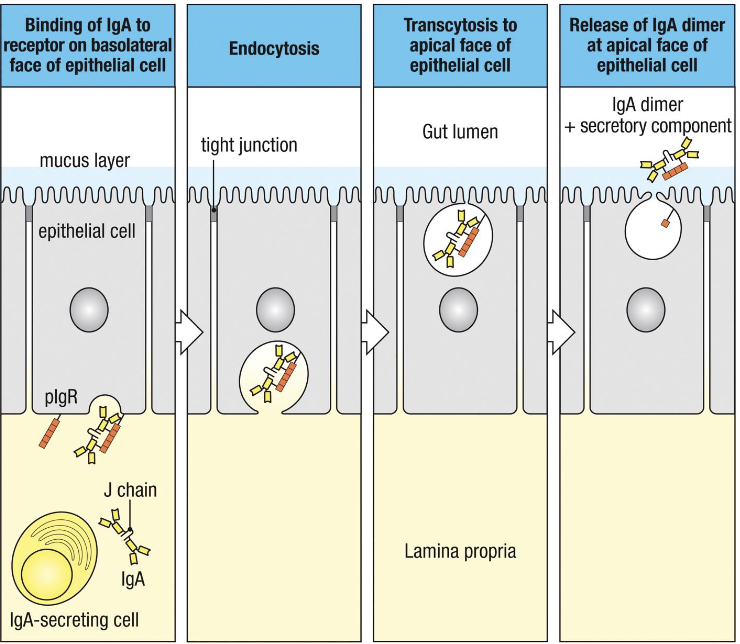
secretory IgA (sIgA):
IgA dimer + pIgR secretory component (soluble in lumen)
mucosal IgA has many functions
prevents microbial attachment to epithelial cells
blocks intracellular spread of viruses, toxins, and bacteria taken up by IECs
Helps remove toxins/pathogens already present in tissues
enhances ag sampling and promotes IgA class switching + immune surveillance
secretory IgA (sIgA) consists of:
a) monomeric IgA only
b) Dimeric IgA plus the secretory component
c) IgA bound to IgG
d) IgA attached to FcRn
b) dimeric IgA plus the secretory component
IgA provides protection at mucosal surfaces primarily by:
a) activating complement
b) neutralizing pathogens without inflammation
c) triggering mast cell degranulation
d) killing bacteria directly
b) neutralizing pathogens without inflammation