Week 4: Elimination
1/80
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
81 Terms
Cognition
comprehensive term used to refer to all the processes involved in human thought; they relate to reception of sensory input, its processing, its storage, its retrieval, and its use
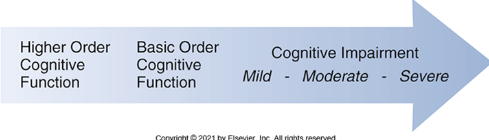
Scope of Cognition
Ranges from Higher order cognitive function to cognition impairment which can be mild moderate or severe
Attributes of cognition
consciousness
memory
executive function
confusion
Consciousness
Patient’s state of awareness of self and environment, including the ability to respond to stimuli appropriately
monitor critical to detecting neurological decline or acute conditions such as hypoxia, stroke or head injury
assessed through levels of alertness (eg drowsy, alert, stuporous, comatose) and orientation (person, place, time, situation)
Memory
cognitive function that allows patient to encode, store, and retrieve information. Impaired memory can affect a pts ability to follow treatment plans, take medications correctly, or participate in self care
assess by asking for short-term, long-term, and working memory recall
Confusion
State of impaired cognition characterized by disorientation, difficulty focusing, poor memory and altered perception of reality
assessed in context of acute or chronic conditions such as delirium, dementia, infection or medication effects
Executive function
higher-order thinking processes that regulate goal-directed behavior such as planning decision making, problem solving, impulse control, and judgement — future oriented used to anticipate, predict, organize and carry out function
Perception
interpretation of the environment; dependent on sensory input
Motor Function
observing the patient’s ability to follow commands, perform purposeful movements, and maintain coordination and balance
Language
conducting observational assessments, administering standardized screening tools like Mini-Mental State Examination (MMSE), CAM, and Mini-Cog, evaluating receptive and expressive language abilities and gathering information from patients and their families
Learning and memory
the ability to retain and recall past experiences and learning— mini mental state examination (MMSE), CAM, and Mini-Cog
Social Cognition
direct observation, structured cognitive screening tools, and specific social cognition tests that evaluate abilities like theory of mmind, emption recognition, and social reasoning
complex attention
test concentration, orientation, and memory and by observing pateitn responses to multi-step commands or tasks that require sustained focus
Populations at risk
elderly and children
independent risk factors
substance abuse, trauma, chronic and acute condition (eg uncontrolled diabetes)
Prenatal risks
genetics
intrauterine infections can damage brain development
intrauterine toxin exposure from alcohol, drugs, and nicotine
poor maternal diet - inadequate nutrition, folic, acid, B12, eating deli meats
neonatal risks
birth risks like birth trauma
premature birth
hypoxia
neonatal infection if mother has herpes or syphilis and baby is born vaginally
newborn hypoglycemia
newborn jaundice
exposure to phenylketonurics if newborn has PKU sensitivity
Situational risks
acute or chronic stress
interpersonal violence and abuse
Personal high risk behavior
Traumatic brain injury (TBI) if lack of hear protection
toxin consumption (eg alcohol, ilicit drugs, smooking)
High risk sexual behavior (syphilis leads to neurological issues)
risky driving: not using seat belt, speeding
Health condition risks
chronic diseases that reduce blood flow (ischemia) leading to decrease oxygen delivery (hypoxia)
common underlying conditions linked to delirium: electrolyte imbalance, pain, infection, hypoxia, low blood sugar, medication SE
Diabetes, cardiovascular disease, COPD, Chronic Kidney disease, Hypertension, HIV, liver disease, obstructive sleep apnea
Delirium
Acute confusion
onset: hours to days
fluctuating consciousness
reversible
cause: medical illness or meds
delirium is a symptom of an underlying cause including infection, pain, hypoxia, dehydration , hypoglycemia, medication side effect, or environmental factors: sleep deprivation, psychosocial factors, emotional distress.
once we treat/alleviate the underlying cause, the delirium should go away
Dementia
Chronic Confusion
onset: months to years
progressive and irreversible decline in mental abilities
Cause: physical changes in the brain from diseases like alzheimer’s, vascular dementia, and lewy bodies
wandering behavior associated with unmet needs like hunger, need to eliminate, pain or anxiety
Restraints, least to most restrictive
mittens
wrist restraints
vest restrain
arm and leg restraints
leather restraints
Preventative measures for restraints
patient education about behaviors that indicate need for restraints
moving IV and things out of sight
having sitter to watch pt
Does a nurse need orders to use restraints
Yes— complete doctors order is need except under extreme emergency circumstances
How often will a nurse need to monitor patient with restraints?
Initially - every 15 minutes
Adult - every 4 hours
pediatrics - every 2 hours for 9-17yo; every hour for less than 9
Where can a nurse attach a restraint
The non moveable part of the bed— moves with patient but not an insecure part
Chemical restraint use?
indicated as last resort for dangerous uncontrolled aggressive violent behavior to ensure pt and care giver safety
What does HEENT stand for?
Head, ears, eyes, nose, throat
What does PERRLA acronym stand for?
Pupils Equal Round Reactive to Light and Accommodating
PERRLA Assessment
P- size of each pupil in mm comparing left to right; clear or cloudy, any rapid abnormal mvmnt
E - bilateral comparison
R - shape of pupils, circular or oval?
R/L - pupil should constrict bilaterally when light shown
A - focus on distant object and shifting focus to a closer object; pupil constriction when focusing closer
When is Mini-Cog used?
used when doing a quick screening for general cognitive impairment and dementia, especially when concerns for memory and thinking
When would a Confusion assessment Method (CAM) be used?
used when suspicion of delirium— more in hospital and acute care than in long term care
Alert and Oriented
person, place, time, situation; additionally care giver identity
Where do you check a pusle
Posterior tibial pulse, pedis dorsalis pulse, radial pulse
temporal used for temp
in baby: take pulse at brachial and femoral pulses
Why do we check pulses multiple places and bilaterally?
in order to make sure that the entire body is receiving blood at the same rate— inequal pulses or absent pulses indicate injury or blood vessel obstruction and needs further assessment
Elimination
removal, clearance, and excretion or waste products
Elimination attributes
output, sensible & insensible
Lifespan considerations/Populations at risk
infants & toddlers: lack of control
holding it in because having fun
wetting bed
pregnant women: urinary frequency due to pressure on bladder, increased volume due to vascular changes, slowed peristalsis can lead to constipation or hemorrhoids
increased risk for UTI
dehydration
older adults: reduced renal blood flow and function, decrease bladder capacity and urethral tone, reduced smooth muscle tones, neural impulses, and mucus secretions
nocturia
slowed peristalsis
Individual risks
Drug and alcohol use
narcotics slow body systems → constipation
antidiuretics and diuretics
Sedentary Lifestyle
slows peristalsis because nor moving
increase risk for UTI → not able to wipe as well, not moving a lot, not wanting to get up and go to bathroom
Post-operative
Ozempic type meds decrease hunger — in surgery can cause aspiration vomiting
decrease movement → stall in peristalsis
What consistency is constipated stool?
separate hard lumps = very constipated
lumpy and sausage like = slightly constipates
What consistency is normal stool
sausage with cracks
smooth soft sausage or snake
What consistency is stool when you lack fiber
soft blobs with clear-cut edges
What is stool consistency when GI inflammation
mushy with ragged edges
What consistency is stool with GI inflammation and diarrhea?
liquid consistency with not slid pieces
Impaction
large, hard mass of stool gets suck in the colon or rectum
causes: chronic constipation, inadequate fluid or fiber, prolonger immobility, medications, neurological disorder, ignoring urge to defecate
Sx: liquid stool, loss of apetite, no pooing even with urge to defecate, nausea/vomiting, distention, cramping, rectal pain
Constipation can cause:
Fecal incontinence
poor quality of life
hemorrhoids
urinary retention
pelvic floor dysfunction
rectal prolapse
Dehydration can cause
UTI
seizure that can lead to coma
hypovolemic shock
Responses to GI Concerns
Non-invasive
Bowel and bladder training
Pharmalogical - diuretic and laxatives
patient education
increase or decrease in fluids depending on problem
exercise/movement
lateral side lying
constipation - left
diarrhea - right
diet changes
abdominal massages
Invasive
enema
Stoma
manual disimpaction
suppository
Types of urinary incontinence
Stress incontinence: due to increase abdominal pressure under stress (weak pelvic floor muscles)
Urge Incontinence: due to involuntary contraction of the bladder muscles
Overflow incontinence: due to blockage of urethra
Neurogenic incontinence: due to impaired functioning of the nervous system
CAUTI
catheter associated urinary tract infection
these are preventable and often the fault of the caregivers that are supposed to be taking care of them
Responding to UTI
Bladder exercise (kegel exercise)
proper wiping technique
sterile technique when dealing with catheter
patient education
increase fluids
intake and output recording
antibiotics
Expected intake per day
Men: ~15.5cup
Women: ~11.5 cups
Expected Measurable Output per day
~800-2000 mL per day
0.5ml/kg/hr
How much unmeasurable fluid is lost per day
~30-50% of water
perspiration: ~300-400mL/day
respiration: ~300-400mL/day
Indication that intervention for UTI worked
regular output
normal color and odor
5-6 times per day
no dysuria
What would a nurse ask before GI assessment?
Pain, flatus, when eat, what/how much ate, any nausea or vomiting, content (shape, color, odor) of last BM, when was last BM, any pain or discomfort
steps of abdominal assessment in the right order?
inspection, auscultation, percussion, palpation
Direction of palpation of colon?
RLQ, RUQ, LUQ, LLQ
Reasons a person may need a bedpan?
Immobile or bed bound, fall risk, convenience, clean catch
Keep in mind with bed pan
pressure sores, hyperextension of spine, cleanliness
Reasons for enema?
constipation/impaction with hard stool stuck in the rectum, cleaning/washing rectum for procedure, medication administarion
Pre-enema assessments?
Allergies? Ask patient if they need to go to the bathroom, Assess GI status noting bowel sounds and any distension, any recent surgeries
Position of patient receiving enema?
left side with knees bent or knee to chest position with anus exposed
Why may someone need a foley catheter?
urinary retention, incontinence, surgery
How can nurses prevent CAUTI
perform hand hygiene, regularly performing catheter hygiene
Sx tht indicate CAUTI
Dysuria, burning, fould smelling cloudy urine, confusion, dehydration, catheter leakage or blockage, fever and chills, sepsis
Pre-catheter questions?
Genital sweelling concerns, inflammation, pain, itching; pain urinating, change in urination, recent sexual activity
What should be assessed with Foley?
color, clarity, unusual odor, drainage, leakage, or irritation around urethral meatus
Where is NG tube placed?
Through nose down into stomach
Why might pt get NG tube?
unable to feed themselves, test for GI bleeding, medication administration
Salem Sump Tube vs Levin Tube
Salem Sump
Used for gastric decompression
Double lumen NG tube
main lumen drains stomach
air vent lumen allows suction without damaging gastric mucosa
Levin Tube
used for gastric decompression and feeding
Single lumen NG tube
soft and flexible
What does NG maintenance include?
Assessment of tube not being kinked or coiled, flushing the tube with sterile water or normal saline, assessing skin around the nose for irritation
How does nurse confirm NG tube placement?
X ray confirmation, checking pH of aspirate gastric contents
What if gastric tube has no drainage?
checking system to make sure that suctioning is on at the right pressure, assessing tube position and make sure there is no dislodging
when would someone need a close wound drain?
to prevent fluid build up, reduce infection risk, reduce pressure and pain, and promote healing
Purpose of close wound drain?
make sure that fluid build up inside the wound are flushed out
How often should a closed wound drain be emptied?
every 4-8 hrs, when ½ - 2/3 fullWh
What should nurse assess when emptying the closed wound drain?
amount of drainage, color, consistency, how it has changed over time
What can net intake and output tell a nurse?
if the pt is getting adequate amounts of liquid, if the pt is eliminating the proper amount per day, if pt has imbalance of input and output
mL → oz
30mL=1oz