Week 4 - Weakness/Syncope/Sudden Death/Paresis/Paralysis
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
83 Terms
- Sudden loss of postural tone - not necessarily loss of consciousness
Define collapse.
- No; A subset of collapse
Is syncope the same thing as collapse?
- Sudden, transient Loss of Consciousness (TLOC) with spontaneous recovery due to transient, global cerebral hypoxia and hypotension
What is syncope?
- 10s
Loss of consciousness occurs within ___________ of cessation of blood flow.
- State of lacking strength
Define weakness.
- Partial loss of consciousness
What is pre-syncope?
- Cardiogenic syncope
- Neurocardiogenic syncope
What are the two types of syncope?
- Neurologic (seizure activity)
- Respiratory (upper airway obstruction, pulmonary hypertension)
- Narcolepsy
- Exercise-induced collapse
- Neuromuscular disease
- Metabolic (hypoglycemia)
What are some forms of non-syncopal collapse?
- Intermittent, profound, abrupt hypotension and marked reduction in cerebral blood flow
What is the primary mechanism behind cardiogenic syncope?
- Reduced CO (arrhythmias, obstruction to outflow, poor contractility, backwards flow)
- Reduced venous return (pericardial effusion/tamponade, obstruction to inflow)
- Cyanotic heart disease (mixing of oxygenated and deoxygenated blood)
What are causes of cardiogenic syncrope?
- Vasovagal syndope
- Neurally mediated syncope
- Vasodepressor syncope
- Reflex syncope
What are synonyms for neurocardiogenic syncope?
- Sudden autonomic nervous system failure
What is neurocardiogenic syncope caused by?
- Excitement, coughing, GI illness
- Significant vasodilation
- +/- bradycardia
What are triggers of neurocardiogenic syncope?
- 6-8 seconds
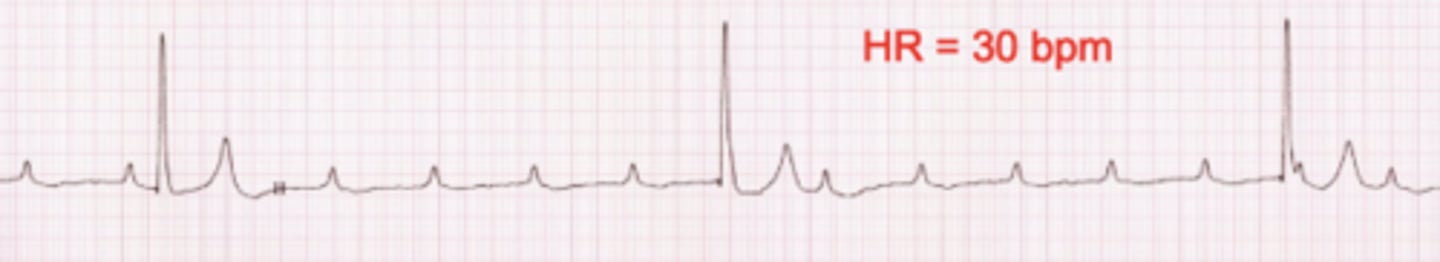
A bradyarrhythmia involves a greater than _____________ second pause in the heart's electrical activity.
- 2nd degree AV block
Name the arrhythmia.
- Hyperkalemia
- AV myopathy
What are causes of atrial standstill?
- If HR is >300 bpm for >10s
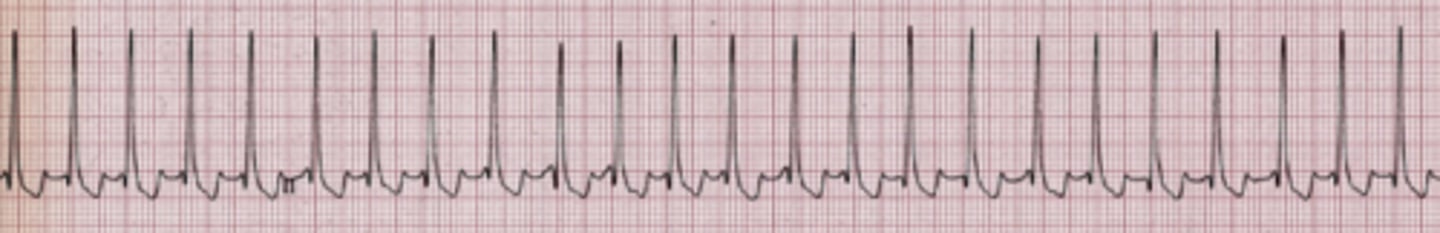
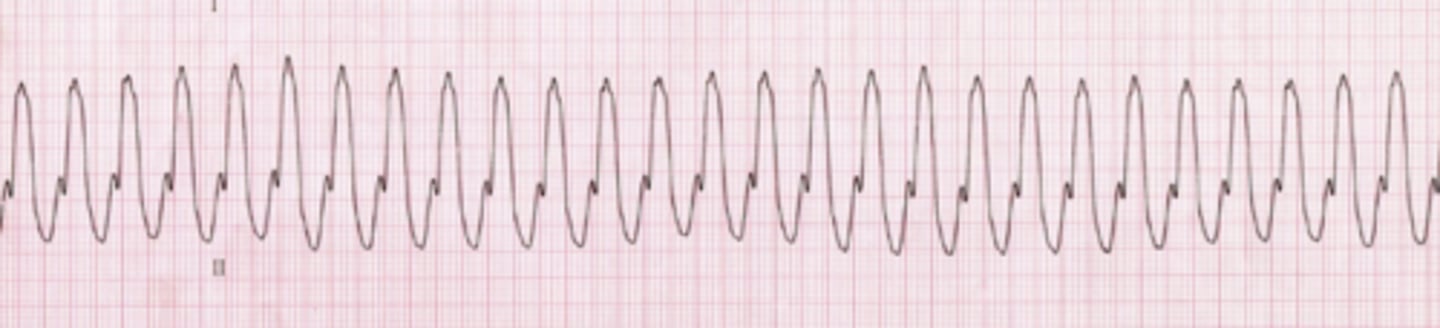
What defines a tachyarrhythmia?
- Supraventricular tachycardia (Narrow QRS complexes)
Identify the tachyarrhythmia.
- Ventricular tachycardia (Wide QRS complexes)
Identify the tachyarrhythmia.
- Exercise
- Fixed cardiac output in the face of exercise induced vasodilation leads to hypotension and syncope (inability to meet metabolic demands)
Syncope due to outflow obstructions commonly occur with ______________. Why?
- Pulmonic valve stenosis (relatively common congenital defect in dogs)
- Subaortic stenosis
- Pulmonary hypertension (normal MPA pressure is about 25 mm Hg for systole; can get as high as 80-100)
What are some causes of outflow obstruction?
- DCM (poor systolic function +/- arrhythmia)
- Severe mitral regurgitation
- Pericardial effusion and tamponade (reduced venous return and therefore reduced CO)
What are some causes of low CO?
- Tetralogy of Fallot
- R to L PDA
What are some causes of cyanotic heart disease?
- Shunting of deoxygenated blood into arterial system leading to reduced oxygenated blood flow to the brain and tissues
Why does cyanotic heart disease cause hypoxemia?
- Tussive or "cough drop syncope"' Coughing increases intra-thoracic pressure leading to decreased venous return. Coughing may trigger reflex bradycardia and vasodilation.
What is cough drop syndrome?
- Differentiating between seizures and syncope
What is the first step in working up a patient with potential syncope?
- What activities occurred leading up to the event?
- What was the duration of the episode?
- What activities were occurring during the episode? Was the patient responsive to touch/voice during that time?
- What occurred after the episode?
What are some focus questions to ask to help differentiate syncope and seizures?
- False; it is short and transient
True or false: By definition, syncope is long but transient.
- False; Both can occur with syncope
True or false: If a patient has an episode suspected of syncope, but was paddling and urinating during the episode, it was likely a seizure.
- DCM: Dobermans, giant breed dogs (adult)
- ARVC: Boxers (adult)
- Chronic degenerative valve disease: Older, small breed dogs
- Subaortic stenosis: Boxers, Goldens, GSDs (young)
- Sick sinus syndrome: Miniature Schnauzers, Dachshund
- AV block: Labradors, many breeds
- SVT: Labs
- Ventricular tachycardia: Doberman, boxers
What are some breed predispositions to cardiogenic syncope?
- Murmur
- Arrhythmias
- Altered pulse character or quality
- Cyanosis
What are some pieces of evidence of cardiac disease which can be noted on a physical exam?
- An artificial pacemaker
Bradyarrhythmias are most appropriately treated with what?
- Sympathomimetic drugs (Epinephrine, Dobutamine, Terbutaline, Theophyline)
- Vagolytic drugs (Atropine, Hyosycamine)
What medications can be used to treat bradyarrhythmias?
- Those that abolish the arrhythmia (Na+ channel blockers; Class 1a): Procainamide, Quinidine
- Those that slow the arrhythmia (slow AV nodal conduction): Digoxin, Ca channel blocks, beta blockers
What medications can be used to treat supraventricular tachycardias?
- Class 1b: Lidocaine, mexiletine
- Class III: Sotalol
What medications can be used to treat ventricular tachycardias?
- Balloon valvuloplasty
How is a pulmonic stenosis treated?
- No documented therapy benefit (can try beta blockers like atenolol)
How is a subaortic stenosis treated?
- Sildenafil
How is pulmonary hypertension treated?
- Positive inotrope (pimobendan)
How is severe mitral regurgitation treated?
- Hydrocodone
- Butorphanol
What are some antitussive medications which can be used for Tussive or "cough drop syncope"?
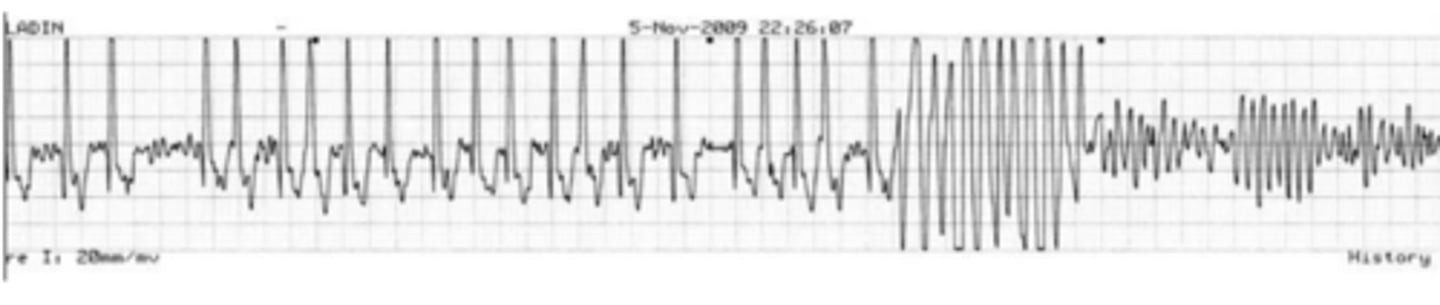
1. Monomorphic V-tach ➔V fib (42%)
2. Polymorphic V-tach ➔V fib (21%)
3. Malignant bradycardia or asystole (37%)
What are the most common arrhythmic causes of sudden cardiac death in dogs?
- DCM
- ARVC
- Subaortic stenosis
- Pulmonic stenosis
- Chronic degenerative valve disease
What are the most common disease conditions which lead to sudden cardiac death in dogs?
- Ventricular tachycardia with a run of ventricular fibrillation
Name the arrhythmia.
- HCM
- RCM
- Unclassified cardiomyopathy
What are the most common disease conditions which result in sudden cardiac death in cats?
- Ventricular tachycardia -> Ventricular fibrillation
In cats, it is suspected that sudden cardiac death is most commonly due to what arrhythmia?
- Corticospinal pathway (origin in the cerebral cortex, fine motor movements)
- Rubrospinal pathway (origin in the brainstem via the red nucleus, main motor pathway in non-humans/primates)
- Reticulo- and vestibulospinal pathway (mediates extensor and flexor tone)
What are the components of the motor system? Briefly describe them.
- Weakness with voluntary motor activity still intact
Define paresis.
- Complete loss of voluntary motor function
Define paralysis.
- Spasticity
- Hyperreflexia
- Hypertonia
- Positive Babinski sign
What are some UMN signs?
- These pathways are inhibitor -> Disinhibition leads to increased extensor tone
Why does damage to UMNs lead to increased extensor tone?
- True
True or false: Damage to UMN system can lead to increased extensor tone and paraplegia at the same time
- Flaccidity
- Hyporeflexia
- Hypotonia
- Atrophy
What are some LMN signs?
- Cell bodies of motor neurons (in cranial nerve motor nuclei or ventral horn of spinal cord)
- Axons in nerves to the muscle ("final common pathway")
Where are LMNs found?
- Contralateral hemiparesis/plegia or quadriparesis/plegia
- Contralateral partial cranial nerve deficits (UMN)
What signs can lesions in the forebrain lead to?
- Ipsilateral hemiparesis, hemiplegia or quadriparesis/plegia
- Ipsilateral complete cranial nerve deficits (LMN) CNN III-XII
What signs can lesions in the brainstem lead to?
1. Olfactory 2. Optic 3. Oculomotor 4. Trochlear 5. Trigeminal 6. Abducens 7. Facial 8. Vestibulocochlear 9. Glossopharyngeal 10. Vagus 11. Accessory 12. Hypoglossal (Ooh ooh ooh to touch and feel very good v*****, ah heaven)
What are the 12 cranial nerves?
- Quadriparesis
- UMN reflexes fore and rear
What signs will damage to C1-C5 lead to?
- Quadriparesis
- LMN reflexes fore
- UMN reflexes rear
What signs will damage to C6-T2 lead to?
- Paraparesis
- UMN reflexes rear
What signs will damage to T3-L3 lead to?
- Paraparesis
- LMN reflexes to rear
What signs will damage to L4-S2 lead to?
- Normal limbs
- LMN signs in anus, bladder and tail
What signs will damage to S2-Coccygeal lead to?
- + / - tetraparesis / plegia (severe cases)
Hyperpathia (pain)
- Conscious proprioceptive (CP) deficits ipsilateral or bilateral fore / hind
- + / - ipsilateral hemiparesis / plegia
UMN fore / hind limb reflexes
- + / - intact pain perception (severe cases)
- + / - diaphragmatic paralysis due to phrenic nerve involvement (C4, 5, 6)
- Abnormal head carriage
- Root signature
What are signs associated with C1-C5 myelopathies?

- Normal withdrawal reflexes all four limbs
Describe the withdrawal reflexes seen in all four limbs with C1-C5 myelopathy.
- Lameness associated with some sort of nerve root pathology (inflammation, infiltration, lateralizing disc, etc.)
What is a root signature?
- Ipsilateral hemiparesis / plegia (if severe)
- Ipsilateral CP deficits fore / hind
- LMN signs (hyporeflexia) fore limb(s)
- UMN signs (hyperreflexia) hind limb(s)
- + / - Horner's Syndrome (T1 - T3)
- Abnormal head carriage + / - cervical pain
- + / - loss of conscious pain perception
What are signs associated with C6-T2 myelopathies?
- Bone associated Wobblers
What is another name for caudal cervical spondylomyelopathy?
- Short/choppy stride in the front and loping wide stride in the hind
- Progressive improvement with time post-operatively (patience is a virtue)
What type of gait is borderline pathognomonic for caudal cervical spondylomyelopathy? Post-operatively, what is the prognosis?
- Ipsilateral or bilateral paraparesis / plegia
- CP deficits one or both hind limbs
- UMN reflexes hind, normal fore limbs
- + / - UMN tone fore limbs if T13 - L2 lesion severe (Border cells)
- Spinal hyperpathia (thoracolumbar area or referred)
- +/- panniculus loss
- +/- loss of CP in the hind
What are signs associated with T3-T3 myelopathies?
+/- painful at site (G) -> Loss of CP (A) -> Weakness/ataxia (H) -> Cannot stand unassisted (F) -> loss of motor function (paralyzed) (B) -> decreased superficial sensation (E) -> Urine retention/UMN bladder (C) -> Loss of deep pain sensation (D)
Place the following items in the order with which they occur with increasing lesion severity/cord compression.
A. Loss of CP
B. Loss of motor function (paralyzed)
C. Urine retention/UMN bladder
D. Loss of deep pain sensation
E. Decreases superficial sensation
F. Cannot stand unassisted
G. Painful at site (+/-)
H. Weakness/ataxia
- True
True or false: It is possible to have a normal reflex without complete consciousness of the senses.
- Ipsi or bilateral paraparesis / plegia
- Normal fore limb myotatic reflexes, strength
- Hind limb LMN reflexes and diminished withdrawal reflexes unilateral or bilateral (L4 -L6 vs. L7 - S2)
- CP deficits unilateral or bilateral hind limbs
- Urinary / fecal incontinence
- Decreased anal tone, perineal reflex
- Change in tail carriage
- L-S hyperpathia on palpation + / - rectal exam
What are signs associated with L4-S2 myelopathies?
- Spinal hyperpathia / hyperesthesia
- Root signature
- Generalized weakness / paralysis
- Voice change
- LMN signs to one limb / multiple limbs dependent on cause
- Normal mentation
- + / - Horner's Syndrome
- Muscle atrophy - focal or generalized
- + / - sensory loss
What are some signs associated with radiculopathy?
- Polyradiculoneuritis
- Brachial plexus avulsion
- Rabies
- Tick paralysis
What are some examples of radiculopathies?
- Flaccid paresis or paralysis of innervated structures (limb, facial muscles, esophagus, anus)
- Neurogenic muscle atrophy
- Reduced or absent reflexes and muscle tone
- Muscle fasciculations/voice change
What are some signs associated with motor neuropathies?
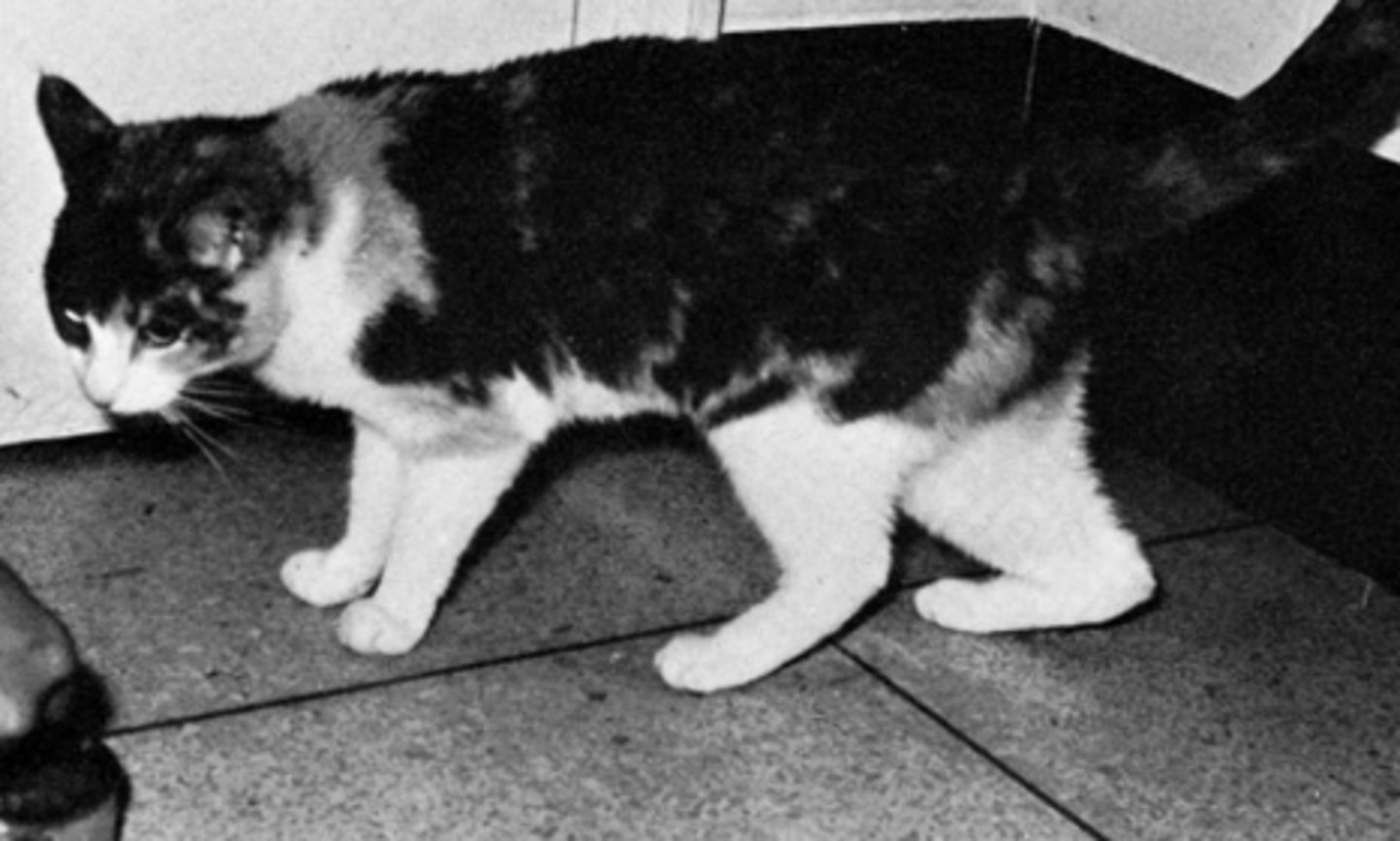
- Diabetes mellitus
What do you suspect this cat has?
- Decreased pain response or sensation
- Proprioceptive deficits
- Abnormal sensation or sensitivity (paresthesia) of face, trunk or limbs
- Self-mutilation
- Reduced or absent reflexes without muscle atrophy
Describe signs associated with sensory neuropathies?
- Long haired Dachshund
- GSPs
What breeds are pre-disposed to sensory neuropathies?
- Anisocoria or dilated pupils
- Decreased tear secretion
- Decreased salivation
- Bradycardia
Describe signs associated with autonomic neuropathies?
- Normal mentation
- + / - palpebral / menace deficits
- Generalized motor weakness or paralysis dependent upon the cause (Episodic or continual)
- Normal or hyporeflexic myotatic and withdrawal reflexes
- + / - voice change
- + / - muscle atrophy
- + / - respiratory difficulty
What are some signs of a junctionopathy (i.e. neuromuscular junction disease)?
- Myasthenia gravis
- Tick paralysis
- Botulism
What are some examples of junctionopathies?
- Tensilon
Myasthenia Gravis can be diagnosed with a response to _______________- test.
- Generalized weakness
- Exercise intolerance
- Stiff, stilted gait
- Localized or generalized muscle atrophy
- Generalized muscle hypertrophy
- Dimple contracture
- Muscle pain on palpation
- Limited joint movement (i.e., contracture)
- + / - voice change (if severe)
- + / - trismus (inability to open the mouth)
What are signs of a myopathy?
- Labrador myopathy
- Masticatory myositis
- Polymyositis
- Neospora of Toxoplasma myositis
What are some examples of myopathy?