23. Surgical diseases of the trachea. Collapse of the trachea. Diagnosis and therapy
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
What are examples of surgical diseases of the trachea?
Tracheal collapse
Tracheal neoplasia
Foreign bodies
Tracheal rupture
What causes tracheal collapse?
Unknown: multifactorial (genetics, allergy, cartilage degeneration, nutrition, neurological)
Decreased glycosaminoglycan content of cartilage rings → weakening of tracheal cartilages → loss of support of dorsal tracheal membrane → collapse into the lumen
During inspiration due to low intrapleural pressure
During expiration due to high intrapleural pressure
Varying degrees of cough (goose-honking), waxing & waning dyspnoea, exercise intolerance & cyanosis. Syncopal episodes.
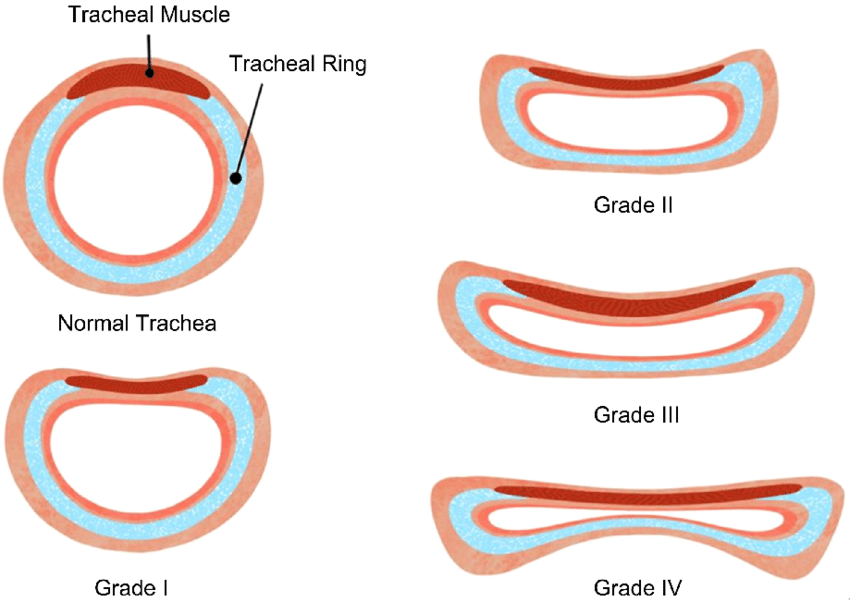
Grade 1: 25% reduction in lumen diameter, cartilage maintain normal C-shape, slightly pendulous membrane
Grade 2: 50% reduction in lumen diameter, cartilage partially flattened, widened & pendulous membrane
Grade 3: 75% reduction in lumen diameter, cartilage flat, membrane almost in contact w/ dorsal cartilage
Grade 4: 90-100% lumen is obliterated, cartilage flat & may invert dorsally, membrane in contact
Signalment, history, clinical signs
Palpation: may elicit coughing, but is not reliable for diagnosis
Radiographs: LL, DV
Fluoroscopy: direct visualisation of abnormal tracheal dynamics during all phases of respiration
Tracheoscopy: visualisation of collapse during inspiration and expiration
Sedatives, cough suppressants (butorphanol PO), short-acting corticosteroids, stabilise with O2
Similar drugs to acute treatment, environmental modification, nebulisation, bronchodilators (theophylline), diazepam, mucolytics, prednisone, weight reduction
What are some surgical treatments for tracheal collapse?
Grade 1 and 2: Dorsal tracheal plication with horizontal mattress sutures.
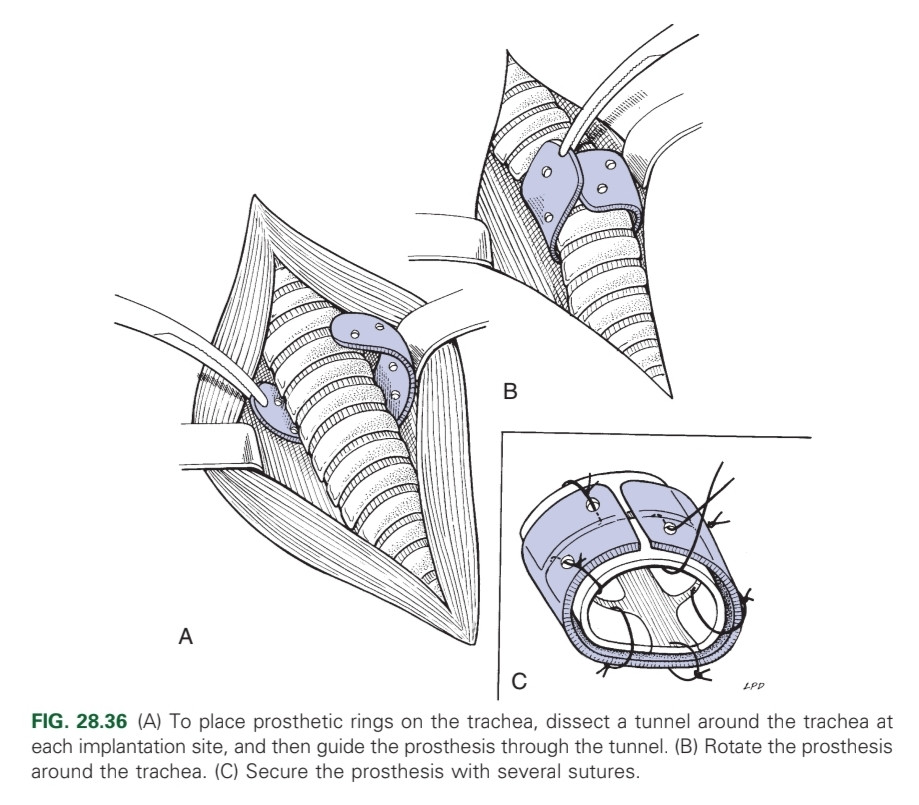
Grade 3 and 4: Extraluminal prosthetic tracheal rings, extraluminal spiral prosthesis, Intraluminal stents
Surgery (if small and benign), tracheal resection and anastomosis. Complete excision of malignant tumours is impossible
Manual removal: Endoscopy; Turn animal upside down; Insert foley catheter past foreign body, slightly inflate cuff and gently pull back
Surgical removal/tracheotomy: Thoracotomy or enter through the neck
Overinflation of tracheal cuff during intubation or trauma
Stridor, pneumothorax, coughing, subcutaneous emphysema, anorexia
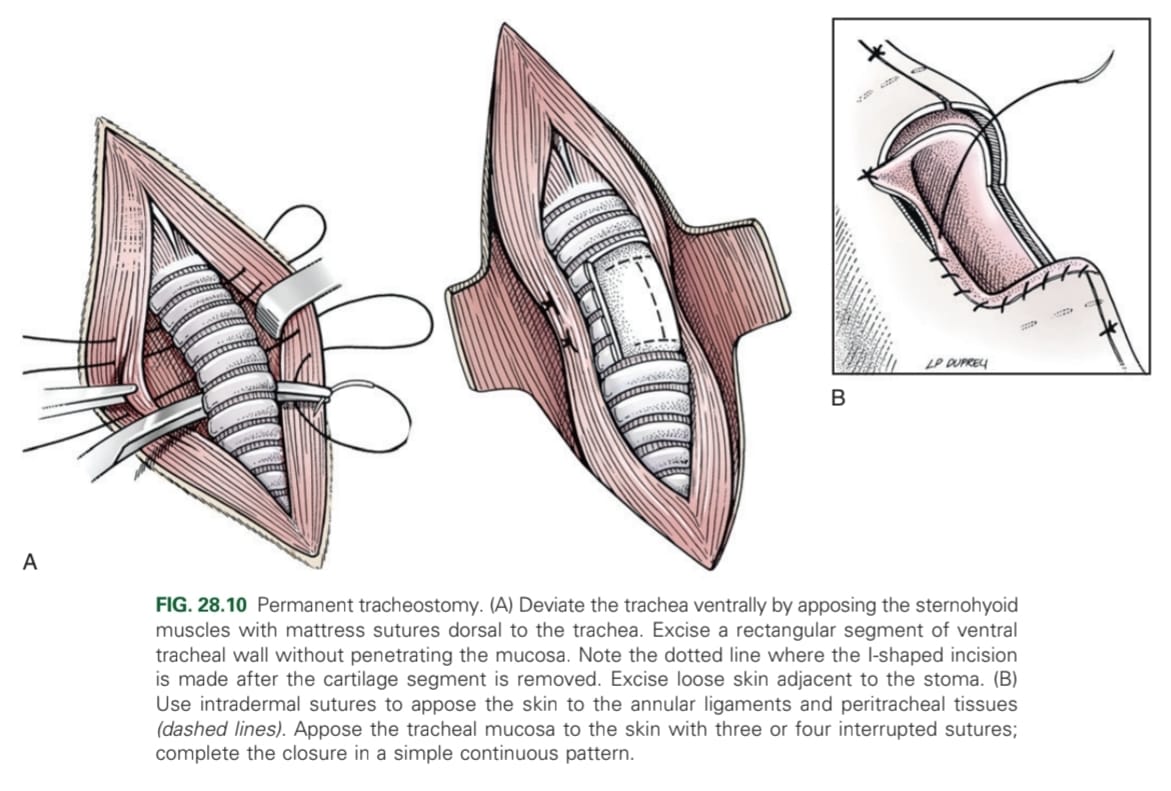
Surgically created opening into the trachea allowing air to bypass the nose, mouth, nasopharynx and larynx
Transverse flap, tracheal flap, vertical tracheostomy
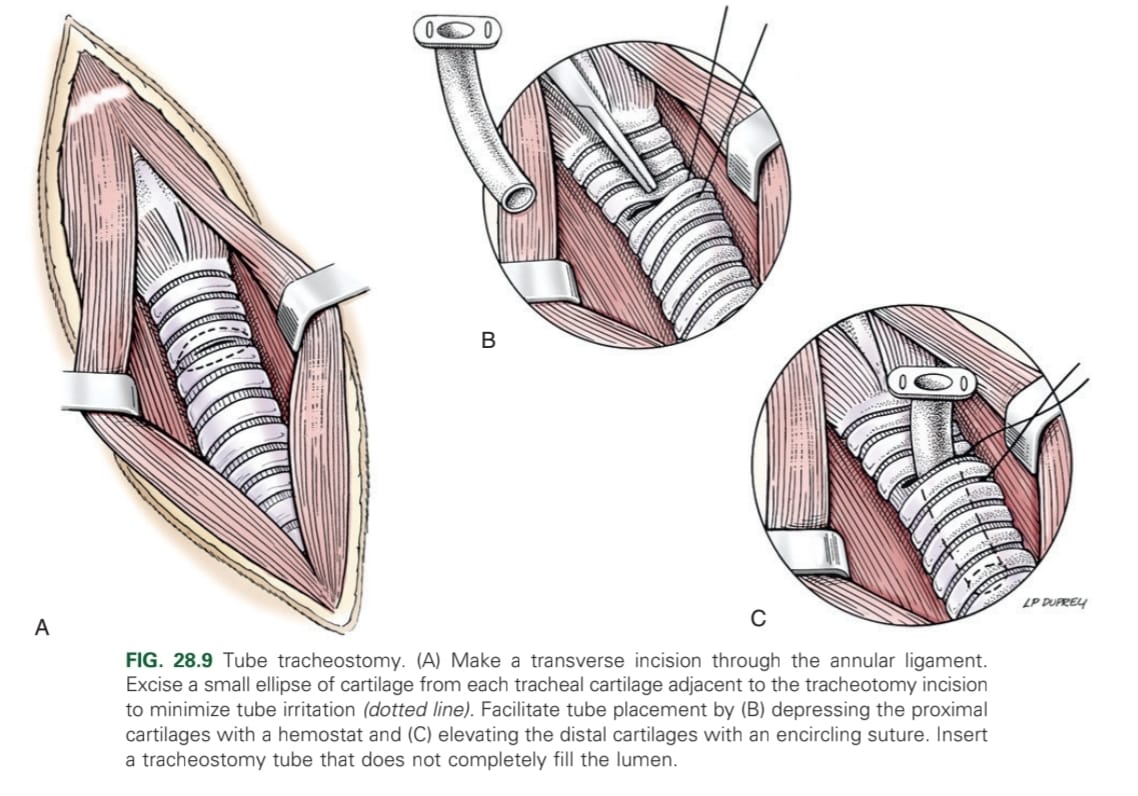
Cervical midline approach over 4-6th tracheal rings → separate sternohyoid muscles incise down to mucosa in a rectangle → make I- or H-shaped incision → intradermal & interrupted sutures at corners → close w/ simple continuous.
Antibiotics (5-7 days), avoiding water contact with the stoma