OFFICIAL CRAM TIME
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
100 Terms
What are the characteristics of delayed haemolytic transfusion reactions?
more common
haemolysis occuring > 24hours after transfusion
extravascular haemolysis in RE(reticular endothelial) system
after secondary exposure to antigen
What are the causative antibodies of delayed haemolytic transfusion reactions?
Anti-Jka, Rh, Kell, Duffy antibodies
What are the laboratory investigations of delayed haemolytic transfusion reactions?
DAT +
positive antibody ID
elution studies
spherocytes
decreased haptoglobulin
increased serum bilirubin
Describe the charactertics and cause TRALI.
Transfusion-related Acute Lung Injury
symptoms within 2-6 hours of transfusion completion
fever, chills, respiratory problems, hypotension, hypoxemia > respiratory failure
What is the pathophysiolgy of TRALI?
PATHOPHYSIOLOGY:
aby in donor plasma biind to HLA/HNA on recipients granulocytes > granulocyte activation
basement membrane destruction
increased permeability of pulmonary circulation
leakage of high-protein fluid into the lungs
> pulmonary oedema
Describe the characteristics of TACO?
Transfusion-Associated Circulatory Overload
withint 1-2 hours of transfusion
symptoms: dyspnoea, orthopnea, cyanosis, tachycardia, pulmonary oedema, hypertension
elderly, paediatric and anaemic patients
treatment: O2, diuretics
prevention: transfuse slowly
How is TRALI prevented?
Anti-HNA/HLA more common in women who have been pregnant
= only male plasma is collected
if woman has been previously pregnant > plasma but be tested neg
Compare and contrast TRALI and TACO
TACO: 1-2 hours of transfusion
TRALI: 2-6 hours of transfusion
Discuss the causes and prevention of transfusion-transmitted infections.
Causes: Donor, contamination
Treatment/further testing: antibiotics, culture and Gram stain
What is FNHTR?
Febrile Non-Haemolytic Transfusion Reactions
symptoms: increase temp after transfusion, chills, increase respiration headache
Treatment: Acetominophen
Prevention: Leukodepletion
What is the pathophysiology of FNHTR?
cytokine released from dono leukocytes
Anti-HLA/HNA abys in recipient bind and activate leukocytes in donor units
What is TA-GvHD?
Transfusion-Associated Graft vs Host Disease
VERY RARE
Symptoms: rash, fever, liver dysfunction > results in bone marrow aplasia
Diagnosis via HLA typing
What is the pathophysiology of TA-GvHD?
immunocompetent T-lymphocytes in donor are transfused into shared HLA or immunocompromised recipient
Donor lymphocytes engraft and proliferate in recipient BM
Recipient HLA class II and/or minor histocompatibility Ags are present to donor lymphocytes > activationcytokines release and cytolytic activity
Explain why platelet transfusion is the leading cause of transfusion-transmitted bacterial infections?
Platelets are stored at RT
Discuss the steps taken in the laboratory in the investigation of a transfusion reaction
stop transfusion immediately
monitor vitals
maintain IV access
bacterial/viral > contact ARCBS
SEND
transfusion reaction investigation request
post-transfusion blood sample
first post-transfusion urine sample
remainder of bag being transfused/anything that was used
What are some of the adverse donation effects?
Vasovagal
haematoma
allergy
Fe deficiency
apheresis (most common: Citrate toxicity)
What type of adverse tranfusion reactions are there?
Immune
acute
delayed
allergic
TRALI
FNHTR
TA-GvHD
Non Immune
TACO
infections
Define Acute haemolytic Transfusion reaction
complement-mediated intravascular haemolysis
complement activate > C3a and C5a release > mast cell activation > histamine and serotonin release
FactorXIII activation > bradykinin production > vasodilation and increase EC permeability > hypotension
EC activation and damage > TF exposure > DIC
Usually ABO incompatabilities
What tests are performed for adverse transfusion reactions?
IAT cross match
Gram stain and culture
ABO/Rh(D) group, aby screen DAT on pre and post transfusion samples
HLA/HPA/HNA antibody testing (TRALI suspecting)
Brain natriureic peptide (BNP)
decrease [TRALI] vs increase [TACO']
What are the characteristics of an infection via Hb transfusion?
bacterial, viral, parasitic
symptoms: fever, chills, vommiting
Bacteria sources: Donor or contamination
List the steps involved in pre-transfusion testing.
maximise the benefit to the recipient while minimising risk
performed before administration of a blood component that could result in the transformation of antigen-antibody complexes.
STEPS:
sample collection (request form, collection, appropriate sample)
ABO and Rh(D) grouping
Antibody Screen (ID if required too)
Selection of appropriate donor
Cross-match
Tranfsufino
Explain the importance of the date/time of collection and phlebotomist signature on the sample tube and request form for TS samples.
date/time > location
name/contact details of requestor > obstetric hx
test/blood product required > known abys
diagnosis/indications for blood > transfusion hx
date/time required
Explain the scenarios where samples for TS testing are valid for 72 hours, and 7 days.
patient not transfused or pregnant in the last 3 months > sample valid for 7 days from collection
patient has been transfused, is/has been pregnant in the past 3 months > sample valid for 72h from collection — due to anamnestic (secondary) IR
Why do we perform an antibody screen, and how one is performed?
performed to detect clinically significant antibodies that may be present in the patient plasma.
can cause haemolysis of corresponding antigen pos cells > HTR or HDNB
anti-a, anti-b and anti-ab is considered clinically significant
use antibody screening cell panel
2/3 cells from different donors that have known antigen expression
What are the characteristics of the cells used in an antibody screen?
come from different group O donors
combined must express:
C, c, D, E, e, M, N, S, s, K, k, Fya, Fyb, Jka, Jkb, Lea and Leb
one should be R1R1 and the other should be R2R2
homozygous pairing cells must be represented as those antigens demonstrate dosage
S, s, Fya, Fyb, Jka, Jkb
You perform an antibody screen there is no reaction with the three cells and the reactions are validated with AHG control cells. What is your interpretation of these results?
invalid test
check sample
check water bath is set @37°C
perhaps didn't follow steps properly
Explain donor RBC selection in individuals with and without antibodies.
should have same ABO and Rh(D) group as patient
if recipient has EVER produced a clinically significant antibody, RBCs that do not express corresponding antigen should not be chosen > aka “antigen negative cells”
if not clinically sig antibody is present - use IAT cross-match compatible cells
Explain when it is appropriate to perform cross-matches by IS and IAT
cross match is done to ensure donor RBCs will not be destroyed when transfused into patient(recipient)
IS: confirms ABO compatibility only
method used ONLY if recipient has NEVER had a clinically significant antibody detected in plasma
IAT: confirms ABO and other blood groups compat
method used if clinically significant antibody has EVER been detected in the recipient plasma
What is blood is given during a transfusion emergency? Explain the protocol
O Rh(D) neg blood is initially given
provide group specific blood asap
complete pre-transfusion testing asap
10min — ABO and Rh(D) group
30min — aby screen and cross-match
Define Group and Screen (Group and Hold)
ABO/RH(D) group and aby screen is performed prior to potential transfusion (i.e. elective surgery)
selection od unit and cross-match is performed when unit is requested
Why are donors in australia voluntary and unpaid?
maintain safe bloos supple and ensure donors have no ill effects from donation
What are the two types of donation and what can be produced from each?
Whole blood:
all blood components are collected via antecubital vein
separated to produce individual components
90 day cycle
Apheresis
blood collected into apheresis machine
blood is separated
plasma/platelets are collected and RBCs returned to donor
2-4 week cycle
Describe the processing of whole blood for transfusion component production?
whole blood
centrifugation
separated into RBCs, Plasma and Platelets > maco-press blood separator — separates blood components into different bags
RBCs
leukoreduced to minimise no of white cells present + decreases incidence of certain adverse transfusion reactions
additive solution added
plasma is separated into plasma and Cryoprecipitate
buffy coat in initial centrifuged bag adds platelet additive solution (PAS). washes with pas are added to another bag > centrifuge > maco-press
What is the benefit of apheresis donation for component production?
can be performed on a more regular basis
components don’t require further processing
In which circumstances are transfusions appropriate, and inapproriate?
appropriate:
blood loss
anaemia [Hb] < 70g/L
replacement of cells
replacement of specific factors
inappropriate:
undiagnosed or asymptomatic anaemia
post-op Hb > 80g/L
reversible short-term anaemia
anaemia responsive to therapy
improve general “well-being”
How much should 1 unit of RBCs increase an adult [Hb] by?
10g/L
How much should 1 unit of RBCs increase an adult [plt] by?
20-50 × 10^9/L
What is the shelf life of RBCs? Platelets? Fresh frozen plasma?Why is the platelet shelf life shorter?
RBCs: stored @2-6°C max 42 days.
must be transfused within 30min of removal from storage
Platelets: stored @20-24°C max 5 days
indications:
postop bleeding [plt] <50 × 10^9/L
thrombocytopenia if [plt] < 10 × 10^9/L
Fresh frozen plasma: stores @-25°C
thawed and transfused within 5 days
indications:
coagulopathies
bleeding patients who require factor replacement
warfarin OD
Cryoprecipitate: stored @-25°C
indications:
decreased plasma
dysfibrinogenaemia
disseminated intravascular coagulation
What are the indications for FFP and Cryprecipitate administration?
plasma exchange
prevent bleeding
stop bleeding
What is Apheresis
separation of cellular elements from plasma
can be used therapeutically
plasma exchange i.e. treatment of immune conditions
RBC exchange i.e sickle cell disease
What does ISBT128 labelling stand for
Information Standard for Blood and Transplant
What are the main 3 coagulation factor concentrates?
Biostate:
contains factor VIII and von Willebrand Factor
Treatment for von Willebrand disease
Prothrominex-HT
contains factors II, IX and X
Treatment for warfarin reversal
Monofix:
contains purified factor IX
Treatment for Haemophilia B
Describe the pathophysiology of HDN.
antigen neg mother carries antigen pos child (father is antigen pos)
mother is exposed to baby’s RBC's (during delivery)
mothers immune system stimulates IR against foreign antigen (baby’s) > IgG antibody
during pregnancy- IgG aby crosses placenta + enters foetal circulation
maternal IgG aby binds to foetal RBCs
foetal RBCs coated in Aby are destroyed via foetal reticuloendothelial system
Which antibodies commonly cause HDN?
most common: Anti-D, Anti-K
but any from:
Rhesus blood group
anti-c, C, e, E
Kell blood group
Anti-k
Duffy blood group
anti duffy a
Describe how an antibody titre is determined.
dilutions of plasma are reacted against cells with homozygous expression of antigen being tested
titre is clinically sig if ≥32 or rises by 2 dilutions
Summarise the serological testing required during the antenatal and post-natal periods.
Mother:
ABO/Rh(D) group, aby screen/ID (if not performed already)
determine degree of foetomaternal haemorrhage (FMH) if Rh(D)neg mother is delivering Rh(D)pos baby
Foetus:
if mother is Rh(D)neg or has a clinically significant antibody > ABO/Rh(D) group, elution studies, Hb, bilirubin
Explain how Rh(D)Ig is used in the prevention of HDN. Include the challenges faced in Rh(D)Ig administration.
Prophylactic Rh(D)Ig is isolated from plasma of Rh(D) neg individuals who produce anti-D. It can cross the placenta
given to Rh(D)neg mothers w/o immune production of anti-D
100IU of Rh(D)Ig protects against 1mL if foetal RBCs
given 625IU @ 28 weeks
note: administer Rh(D)Ig after collection of sample for baby screen
given 625IU @ 34 weeks
given 625IU @ delivery
if newborn is Rh(D)+ve
Challenges:
anti-D is highly immunogenic
may cause HTR/HDNB
What is HDN and its charcteristics?
Haemolytic Disease of the Newborn
HDNB, HDFNB (f=foetus)
characteristics:
jaundice
positive DAT
maternal antibody
leads to:
Kernicterus - bilirubin accumulation in the brain > brain damage
Hydrops fetalis - oedema in the foetus > death from heart failure
What does HDN lead to?
leads to:
Kernicterus - bilirubin accumulation in the brain > brain damage
Hydrops fetalis - oedema in the foetus > death from heart failure
What antenatal and postnatal practice is done for HDN recognition?
First-trimester visit
ABO/Rh(D) typing
re-rest at 28 weeks
Antibody screening
neg > re-test at 28 weeks
pos >
perform Aby ID,
determine its clinical significance
paternal/foetal genotype/phenotype
aby titration
What test is done for foetal anaemia?
Middle cerebral artery (MCA) Doppler ultrasound
non-invasive
measures velocity of blood flow in middle cerebral artery
increase blood flow > anaemia
How is foetomaternal haemorrhaging quantified?
Acid Elution Test (Kleihauer Test)
Flow cytometry
Explain Acid Elution Test.
Adult haemoglobin (HbA) is sensitive to acid, foetal haemoglobin (HbF) is resistant to acid
Expose blood film to acid
HbA denatures, HbF intact > stain w eosin/erythrosine
light pink/clear cells > HbA aka. ghost cells
How is the Kleihauer (Acid Elution Test) calculated?
Foetal RBCs(mL) = (HbF per FOV / HbA per FOV) x 2400
ensure there are 100 HbA in 40x FOV
based on the assumptions:
foetal RBCs are 22% larger than adult RBCs
only 92% of foetal RBCs are stained
maternal RBC volume is 1800mL
How to you calculate foetal RBCs via Flow cytometry
Foetal RBC(mL) + % foetal cells x 21.96
based on assumptions:
foetal RBCs are 22% larger than adult RBCs
maternal RBCs volume is 1800mL
more accurate, better reproducibility and less laborious than Kleihauer
What are the treatments for HDN?
Phototherapy: expose newborn to blue light (460nm)
breaks down bilirubin
Exchange Transfusion: exchange foetal blood to remove aby and reaplce RBCs
rarely performed as its performed in utero to allow foetal lungs to develop
What are the 2 methods of Rh(D)Ig administration?
Intramuscularyyly (IM)
Rh(D) Immunoglobulin-VF
250IU and 625IU are available
Intravenously (IV)
Rhophylac
1500IU
Explain the principle of the AHG test.
used to detect
IgG antibodies bound to RBCs that are not detectable by other methods
Complement proteins bound to RBS due to antibody binding
use anti-human IgG and/or anti-CD=3d antibodies to cross-link IgG or C3d already bound to RBCs > haemagglutination
Why is the wash step important when the AHG test is performed in tubes?
Removes IgG that is not bound to RBCs otherwise AHG reagent will bind to IgG that is free in the plasma > false negative result
When are AHG control cells added to the AHG test? Why?
add to every negative reaction
ensures that:
AHG reagent was added to tubes
make sure AHG reagent works
you have correctly performed your washes
Explain the difference between the DAT and IAT. When are each of the tests used?
Direct anti-human globulin test DAT
detects aby and/or c3d bound to patients RBCs in vivo
haemolytic transfusion reaction
haemolytic disease of the newborn
autoimmune haemolytic anaemia
Indirect anti-human globulin test (IAT)
detects aby bound to RBCs in vitro
antibody screening and identification
cross-matching
phenotyping
Why are potentiators used in the AHG test?
decrease RBC ζ-potential or surface charge to enhance IgG aby binding/agglutination + decrease distance between adjacent RBCs > Low ionic strength saline (LISS)
Explain the mechanism of action for each of the potentiators.
Low Ionic Strength Saline (LISS)
RBCs are diluted in 0.2% saline or Low ionic additive (LIA) is added
Glycine is present > maintain iso-osotic conditions > cells don’t burst
reduces ζ-potential by decreasing ionic strength
increases aby uptake during sensitisation
allows incubation time during AHG test shorter
Polyethylene glycol (PEG)
speeds aby binding to RBCs via steric exclusion of water molecules
conc aby around RBCs
allows shortened incubation time in AHG test
NB; addition of PEG > cannot centrifuge cells until addition of saline of wash
Albumin
increases dielectric constant of the medium > decrease in ζ-potential
used at 22-305
more expensive
Enzymes
modify antigens on RBC surface
decrease ζ-potential by removing sialic acid residues
enhance reactivity of some blood group antigens
decrease reactivity of others
performed in 2 stages:
Stage 1: incubate plasma, RBC and enzyme > centrifuge then read results
Stage 2: incubate RBCs and enzyme together > wash cells > incubate plasma with enzyme-treated cells > centrifuge and read results
Polybrene
cationic ammonium polymer that causes reversible aggregation of RBCs
added to aggregate cells > sodium citrate then added to neutralise polybrene
Aby present: agglutination
No Aby present: agglutination will disperse
When performing the AHG test using cards, why do the samples not require washing at any point of the test?
Buffer solution of high density is layed over the top of bead:
traps plasma proteins > no washing
Describe the three phased of the AHG test by tube method, including what is detected at each phase.
RT: agglutination @RT - IgM : not clinically significant
37°C: Some IgG antibodies (anti-Rh, anti-K)
IgM reactive @ 37°C
AHG: IgG antibody
What are the benefits of performing haemagglutination reactions in cards?
easy to use
require no washing
reagents already added
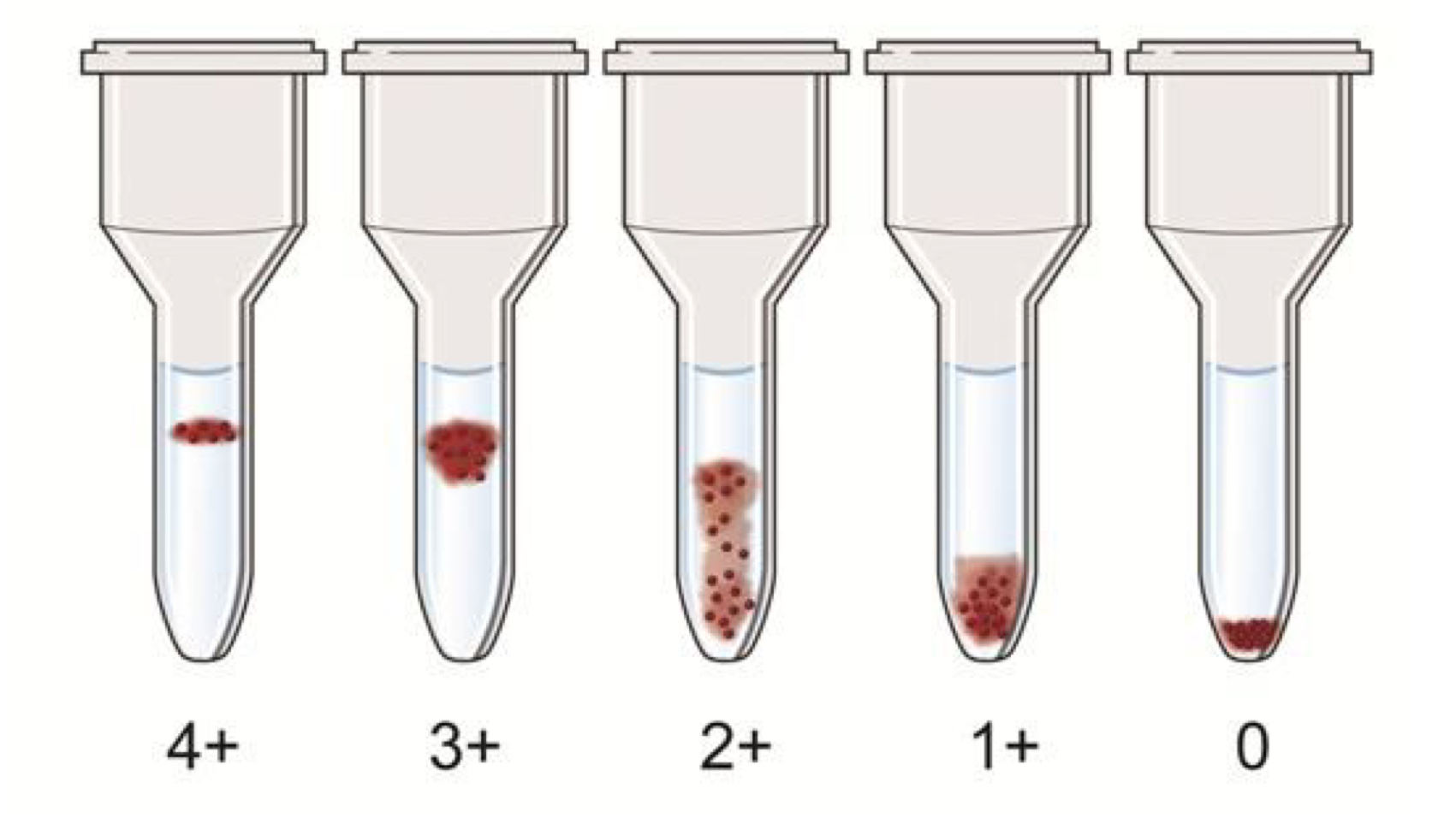
For haemagglutination reactions performed in cards, describe the appearance of each of the reaction grades when using the 0-4+ scale.
Describe how agglutination occurs.
Haemagglutination
Sensitisation: aby binds to antigen on the RBC surface
Agglutination: bound antibdy cross-links adjacent RBCs
What is meant by the term “dosage”?
how antibodies react to antigens which demonstrate dosage effect
i.e. Anti-Jka demonstrates dosage. It reacts stronger to cells which hall homozygous expression of Jka
Antigens of which blood groups are destroyed by enzyme treatment?
M, N, S, s, U (MNS blood group)
Fya and Fyb (Duffy blood group)
Antigens of which blood groups are enhanced by enzyme treatment?
C, c, D, E, e (Rh blood grouping)
Found on chromosome 1
RHD gene encodes D antigen
RHCE gene encodes C, c, E, e antigens
C and c differ by 6 nucleotides
E and e differ by 1 nucleotide
K, k (Kell blood grouping)
Jka, Jkb (Kidd blood grouping)
Why are Kidd antibodies so difficult to work with?
often weak, demonstrate dosage, found in combi with other aby’s
Anti-Jka, Anti-Jkb
IgG
best detected @37°C via IAT
unstable on storage
common cause of HTR, rarely HDNB
Why is there a racial difference in Duffy phenotype distribution?
absence of Duffy antigens on RBCs > RBCs more resistant to invasion by a malarial parasite
positive selection pressure
Explain the inheritance of Rh antigens.
inherited as a haplotype
one set of RHD and RHCE gene from one parent, second set from other
i.e. DCe/dce (Fisher-Race nomenclature)
Why is the D antigen so immunogenic?
contains at least 30 different epitopes
Explain the difference between the FIsher-Race and Weiner nomenclatrue.
Fisher-Race:
haplotype written as a triplet of letters
note - d isused to represent “absence of D”
DCe/dce
Genotype: DCe/dce
Phenotype: DCce
Weiner:
uses R/r and numbers/primes to represent haplotype/ genotype/phenotype
R = D antigen
r = absence of D antigen
Ce = R1 or r’
cE = R2 or r”
ce = R0 or r
What is the class of each of the antibodies in the MNS blood group?
anti-M/N: IgM or IgG;not clinically sig unless reactive @37°C
anti-S/s: IgG; clinically sig as react @37°C
What does RHD and RCHE gene encode?
417 aa transmembrane
non-glycosylated proteins
Describe the characteristics of Rh antibodies.
Immune
usually IgG
dont bind complement
react optimally @RT
Detect using IAT (“Weak D Test”
How should Partial D be expressed?
Recipient: Rh(D) neg
Donor: Rh(D) pos
Describe Kell blood group system antigens.
2 antigens(proteins) : K and k (cellano)
Antithetical pair expressed co-dominantly
well developed at birth
K is highly immunogenic
K-k+ most frequent
Antibodies
Anti-K
IgG
can cause HTR and HDNM
best detected @37°C via IAT
Anti-k
very rare > difficult to find compatible blood
IgG
best detected @37°C via IAT
Describe Kell blood groups antibodies.
Anti-K
IgG
can cause HTR and HDNM
best detected @37°C via IAT
Anti-k
very rare > difficult to find compatible blood
IgG
best detected @37°C via IAT
Describe Kidd blood groups antigens.
2 main antigens: Jka, Jkb
protein
antithetical pairs expressed c-dominantly
well developed at birth
poor immunogens
Describe MNS blood group antigens.
5 main antigens: M, N, S, s, U
protein
M/N expressed on glycophorin A (GPA)
furthest away from RBC membrane
S/s and U expressed on glycophorin B (GPB)
closest to RBC membrane
Describe Duffy blood group antigens.
2 main antigens: Fya and Fyb
antithetical pairs expressed co-dominantly
well developed at birth
What is a blood group, and what are the ISBT blood group requirements?
one or more RBC surface antigens controlled b an allelic gene.
ISTB requirements
antigen must be inherited
the gene encoding it must have been:
identified and sequenced,
chromosomal location must me known
gene is different from other gene encoding antigens of existing blood group systems
corresponding human alloantibody must be identified
What are the two main types of RBC antigen?
anti-a
anti-b
Explain the difference between an antigen and antibody
Antigen : produces and immune response (antibody) if recognised as foreign
Antibody : specific proteins produced in response to an antigen. only interact with specific part of the antigen before production
What are the two main subtypes of antibodies encountered in transfusion science? What are the kinetics of their production?
IgG & IgM
Kinetics :
Primary Challenge
long lag time (5-7days)
IgM predominant
some IgG
Memory B cell development
Secondary Challenge
Anamnestic Response
short lag time (2-3d)
IgG predominnat
some IgM
High Avidity
Define, and explain the characteristics of, naturally occurring and immune antibodies.
Present in plasma without any known immunisation
not present at birth
IgG : ~12nm, monomer, react @37°C, “incomplete”
e.g. Anti-Rh, Anti-Kell
IgM : ~30nm, penteramic, react @4°C, “complete”
e.g. anti-A, anti-B
What is in in vivo consequence of antigen-antibody binding in the transfusion science context?
RBC is damaged:
leads to complement activation > Antibody-dependent cell-mediated cytotoxicity (ADCC(lysis))
Haemolytic Transfusion Reaction (HTR)
Haemolytic Disease of the Newborn (MDNB)
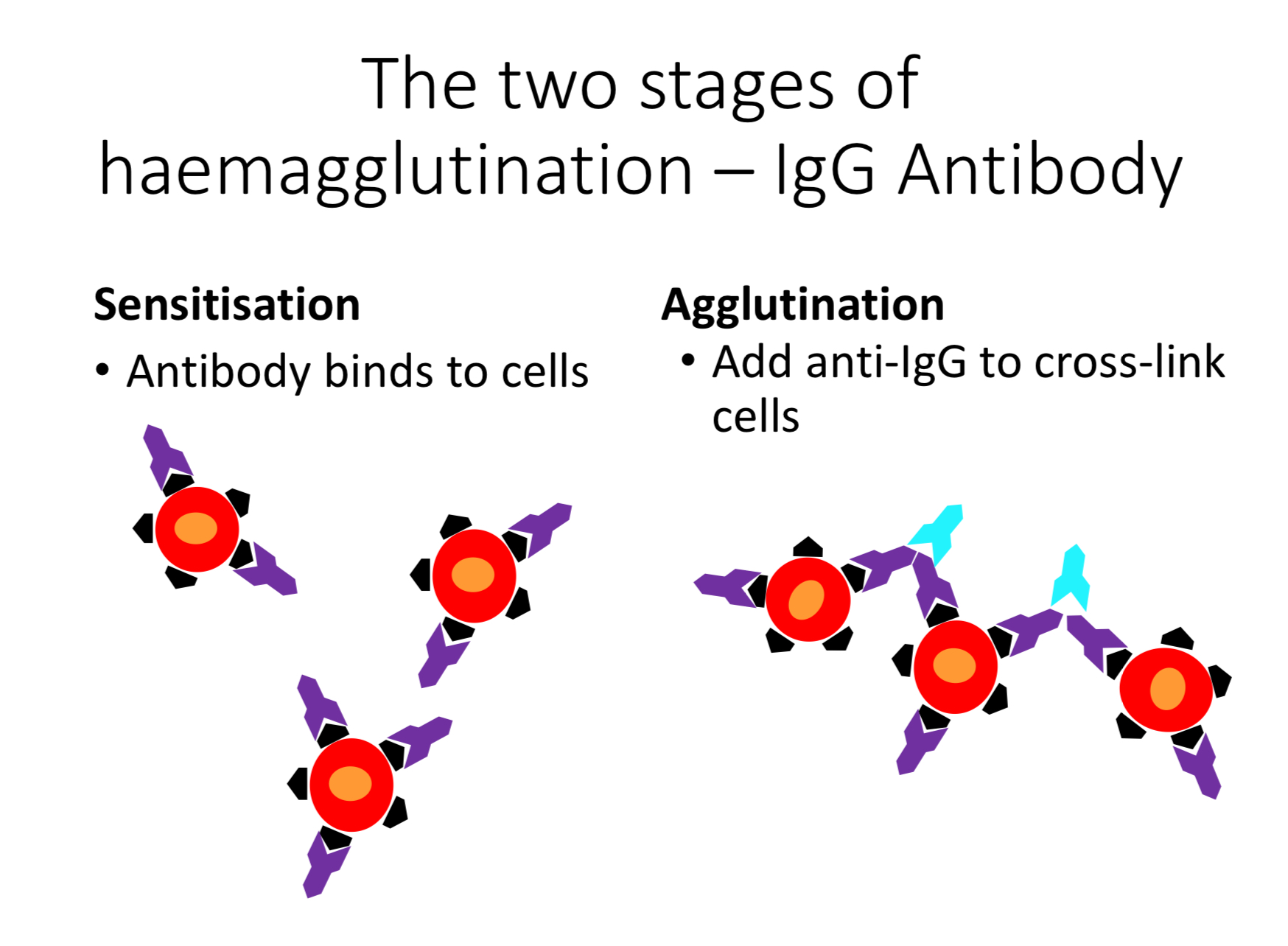
Describe the mechanism of haemagglutination for IgG and IgM antibodies.
Sensitisation
Agglutination
IgG
Sensitisation > Aby binds to cells
Agglutination > Add anti-IgG to cross-link cells
IgM
Sensitisation > Abyb binds to cells
Agglutination > Bound aby cross-link cells
Describe the appearance of each of the reaction grades used in the 0-4+ haemmagglutination grading scale.
0 — no agglutinates
1+ — small agglutinates w red background
2+ — many medium-sized agglutinates
3+ — one or two large agglutinates
4+ one large agglutinate
Explain how ADCC is stimulated.
Medianted by IgG
aby-coated RBC binds to macrophage via Fc receptor > extravascular haemolysis
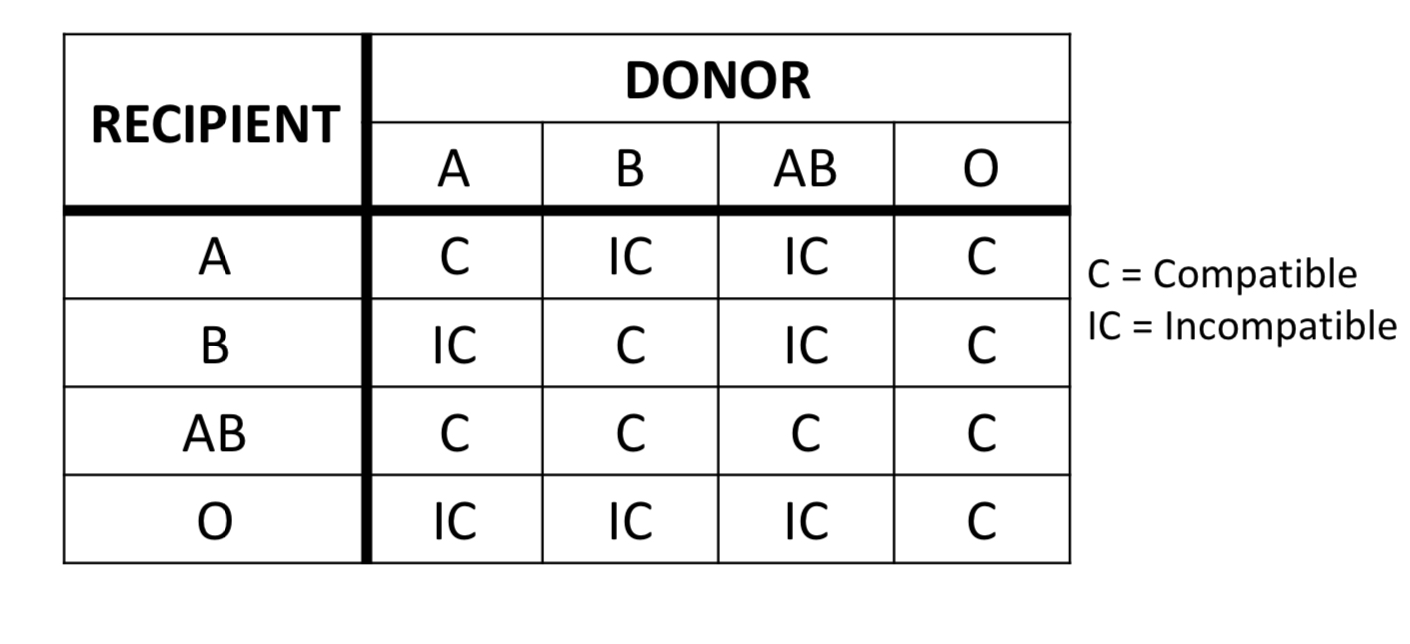
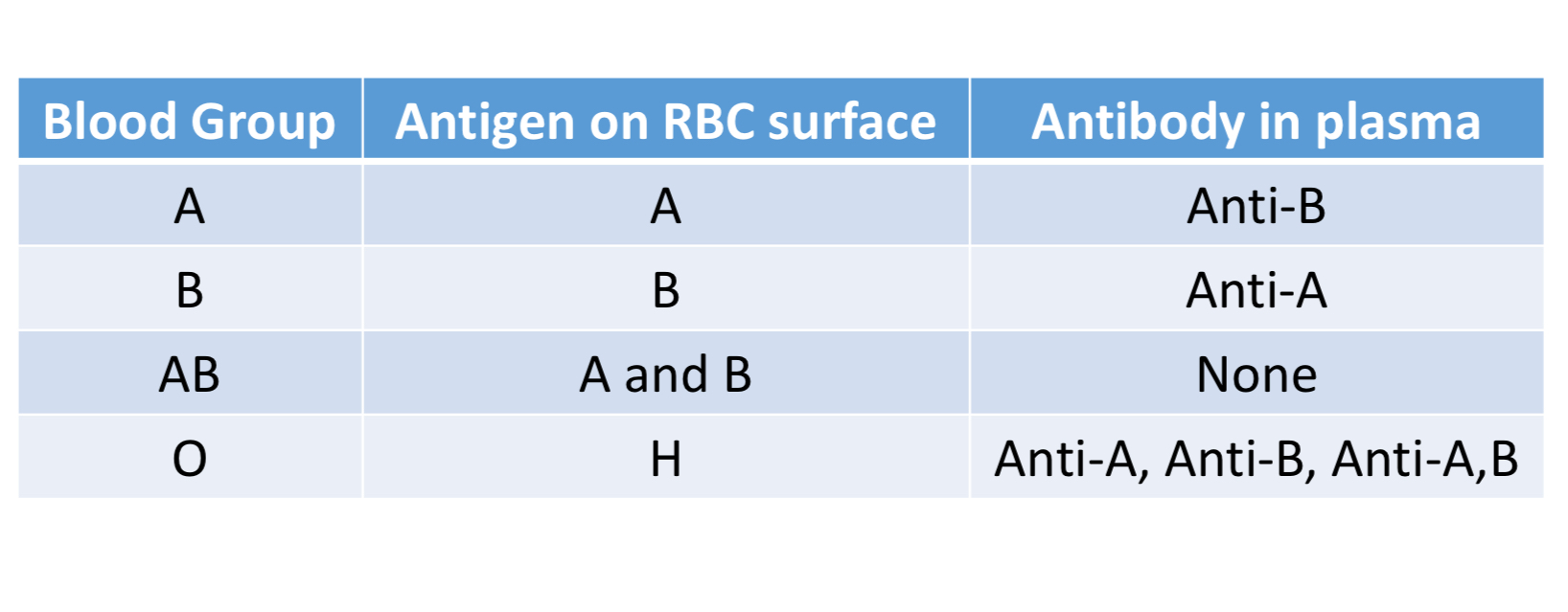
Which antigens and antibodies are produced on each of the ABO groups, and what is their distribution in the Australian population?
A : 39%
B : 11.5%
AB : 3.5%
O : 46%
Describe the production of the ABO antigens.
Type II precursor substance (CHO) + glycosyltransferase + —> H antigen
H antigen
A or B antigen
Describe the characteristics of ABO antibodies.
“Naturally occurring” - produced w/o priir exposure to antigen
Usually IgM but can be IgG (Anti-a,B in O people is IgG)
Bind complement
React optimally @ RT
Not detected until 3-6 months of age
Describe how an individual’s ABO group is determined
Forward Grouping
react patients RBCs with known antiserum (anti-a or anti-b)
identifies which antigens are present
Reverse Grouping
react patients plasma with cells of known phenotype (A cells or B cells)
identifies which antibodies are repesent in patient plasma
Draw a table describing which ABO groups are compatable