Pulmonology Combined- Week 1
lung anatomy
pleural anatomy
-a serous membrane lining the lung, mediastinum, diaphragm, and inner chest wall
-visceral and parietal pleura
1/205
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
206 Terms
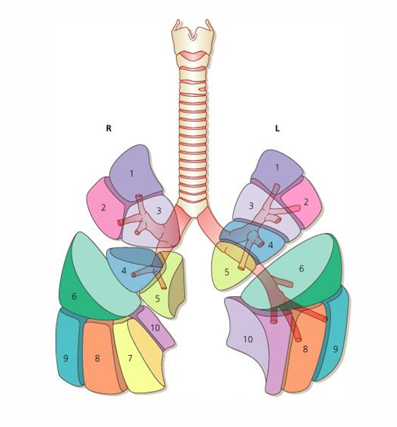
lung anatomy
pleural anatomy
-a serous membrane lining the lung, mediastinum, diaphragm, and inner chest wall
-visceral and parietal pleura
airway anatomy
ventilation and gas exchange
-ventilation: movement of air/gas between the atmosphere and the alveoli
-gas exchange: transfer of O2 into the pulmonary circulation and CO2 out of the pulmonary circulation

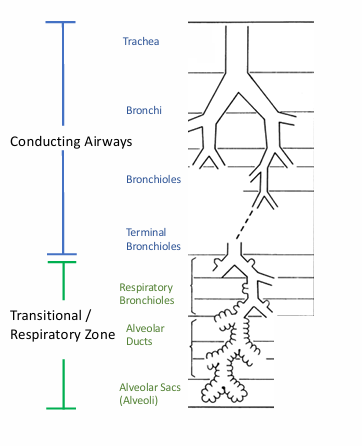
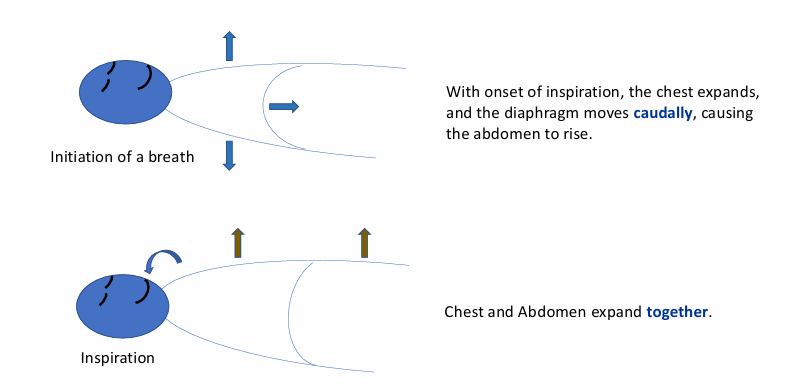
process of breathing
normal respiratory cycle
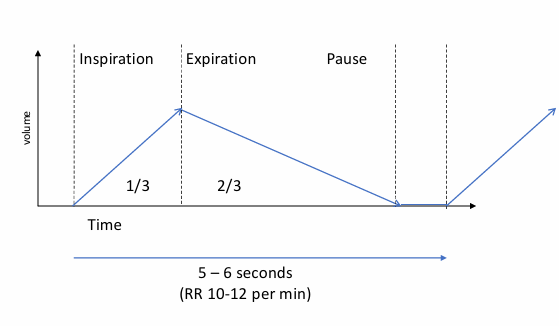
breathing and pulmonary muscle anatomy
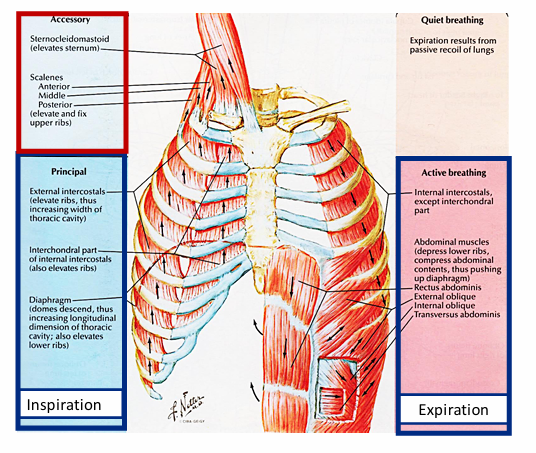
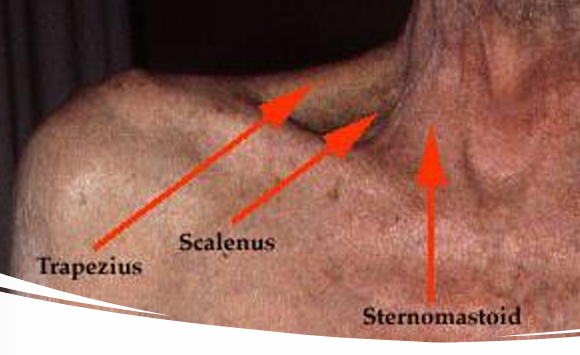
accessory muscles- abnormal inspiration
-a person’s demand exceeds their ability to breath with the normal muscles of respiration alone, or
-a person’s normal muscles of respiration are dysfunctional (weak, fatigued, non-functional)
mechanisms of disease
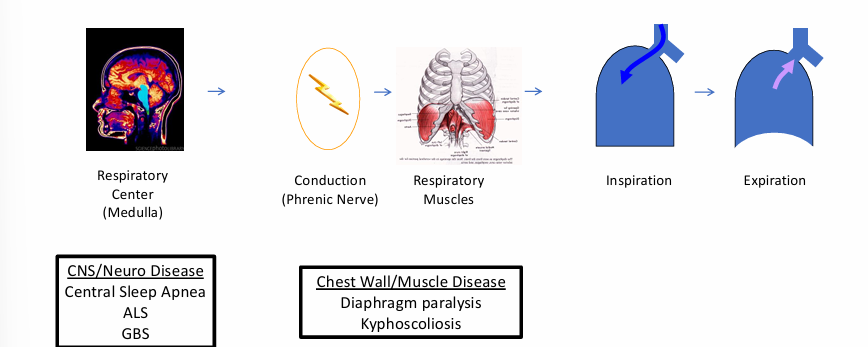
normal respiration
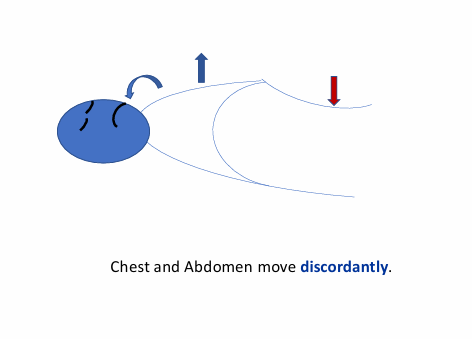
abnormal respiration- paradoxical breathing
-tells that something is wrong with the mechanics of the respiratory system
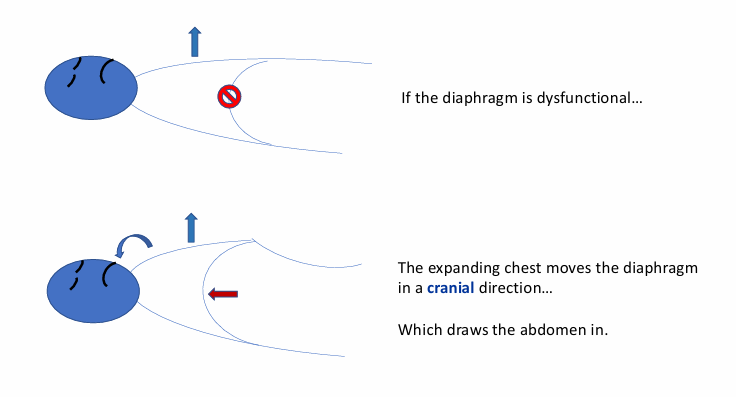
abnormal respiration- diaphragmatic paralysis
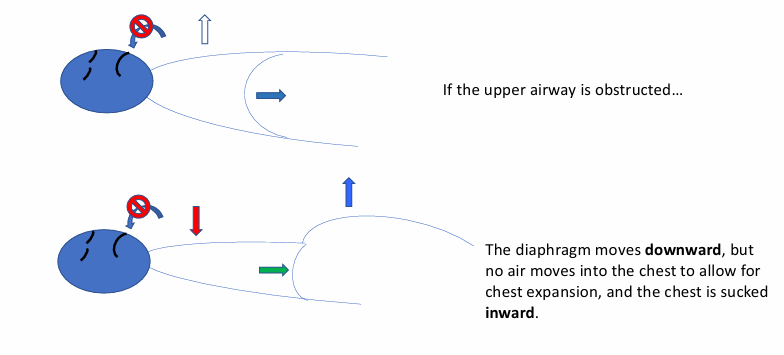
abnormal respiration- upper airway obstruction
mechanisms of disease

different disease states
-obstructive lung diseases
-restrictive lung diseases
obstructive lung diseases
-asthma
-COPD: chronic bronchitis, emphysema
-bronchiectasis: cystic fibrosis
restrictive lung diseases
-interstitial lung disease
-sarcoidosis
-asbestosis
-pneumoconiosis
-systemic sclerosis
-chest wall diseases: kyphoscoliosis, obesity
-neuromuscular weakness
respiratory failure
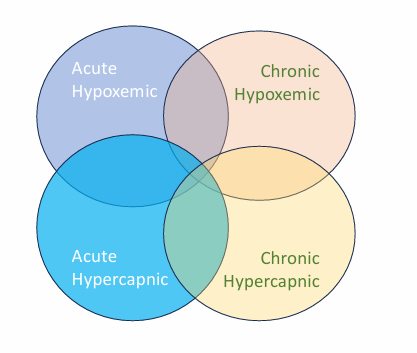
acute & chronic respiratory failure examples
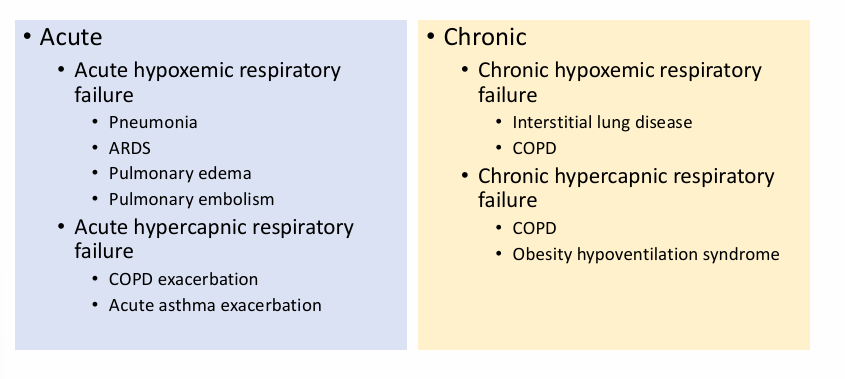
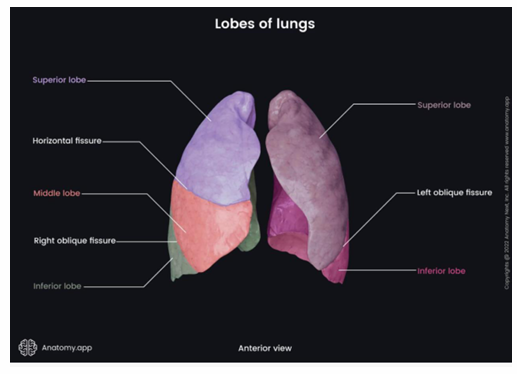
lung gross anatomy- lobes
-right: 3 lobes- upper, middle, lower
-left: 2 lobes- upper (+lingula), lower
gross anatomy- fissures, pleura, pleural cavity
-fissures: separate lobes, horizontal (right) and oblique (right and left)
-pleura (2 layers): visceral pleura (each lobe has separate pleural investment), parietal pleura (lines the thoracic wall)
-pleural cavity: space between visceral and parietal pleura
gross anatomy- pleura
-pleural fluid (secreted by mesothelial cells): lubrication between layers (reduces friction), surface tension (maintain position of lungs against thoracic wall)
-create division between organs

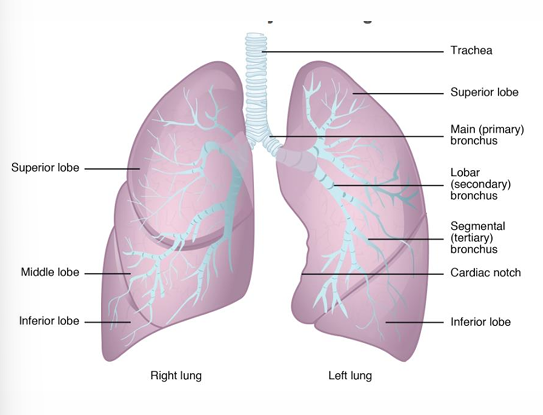
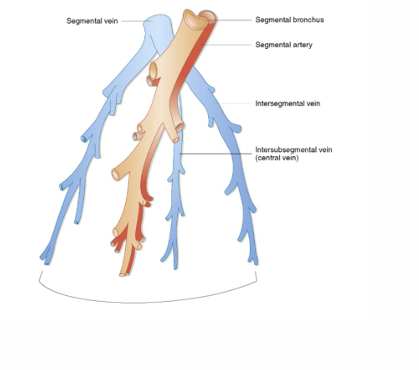
gross anatomy- bronchopulmonary segments
-each lobe divided into bronchopulmonary segments: right = 10 segments, left = 8-10 segments
-each segment receives air and blood from its own tertiary bronchus and segmental artery (of the pulmonary artery)
-in some cases, a disease may be localized to a bronchopulmonary segment(s), which can be resected with little impact on adjacent segments
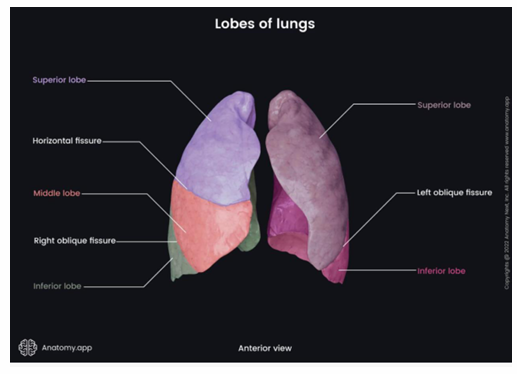
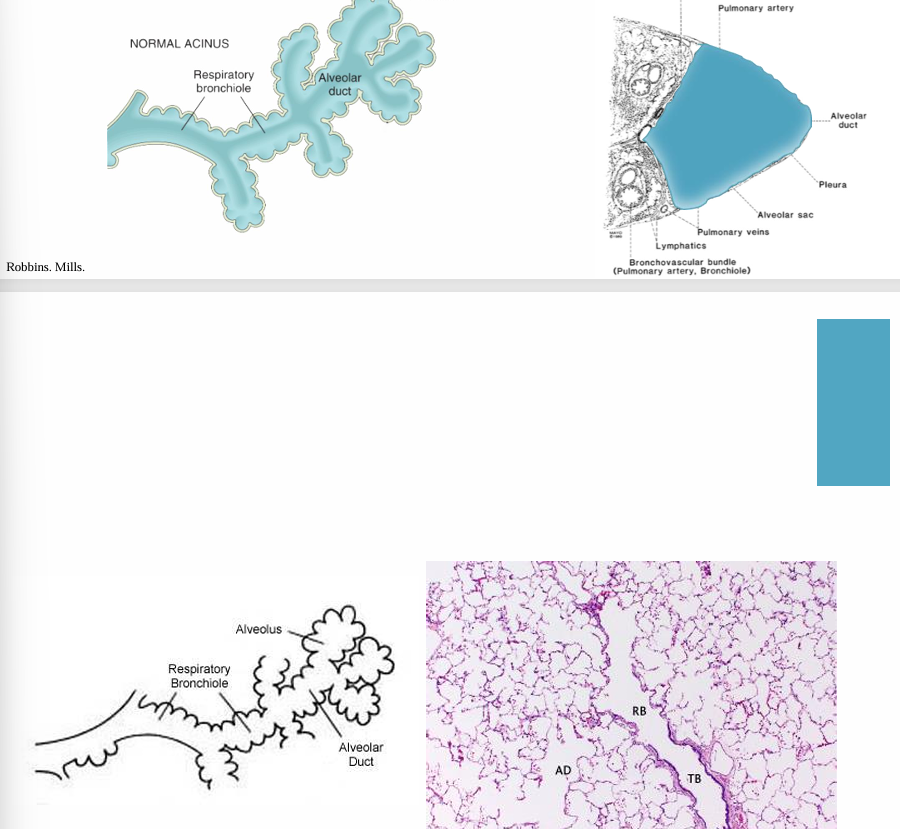
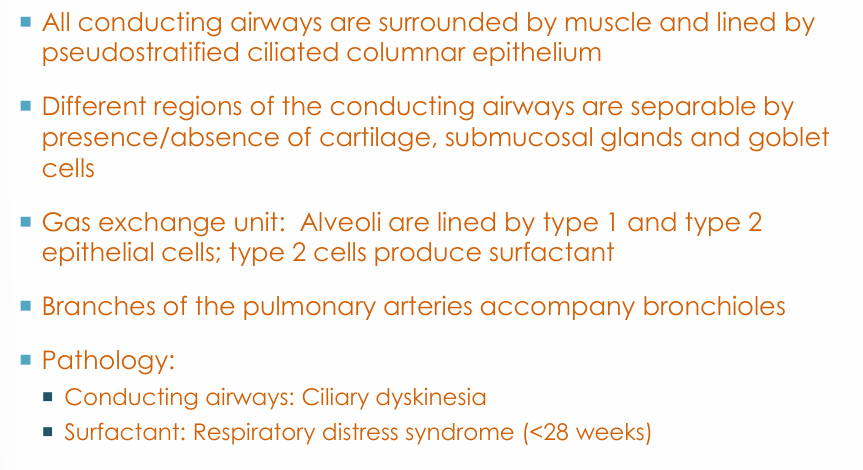
anatomy- airways
-branching from trachea to alveolar sacs: ~23 divisions
-conducting airways: carina → non-cartilaginous bronchioles
-gas exchange unit: acinus
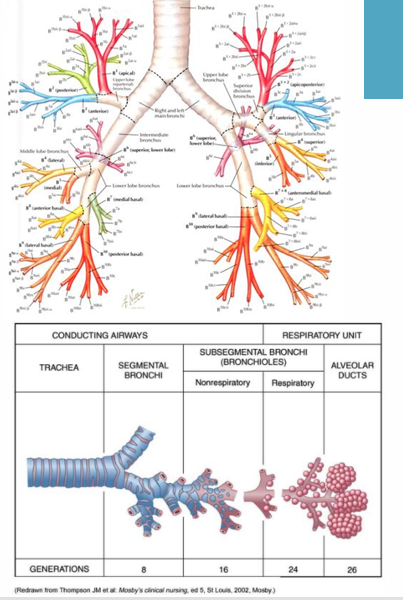
airway pathway
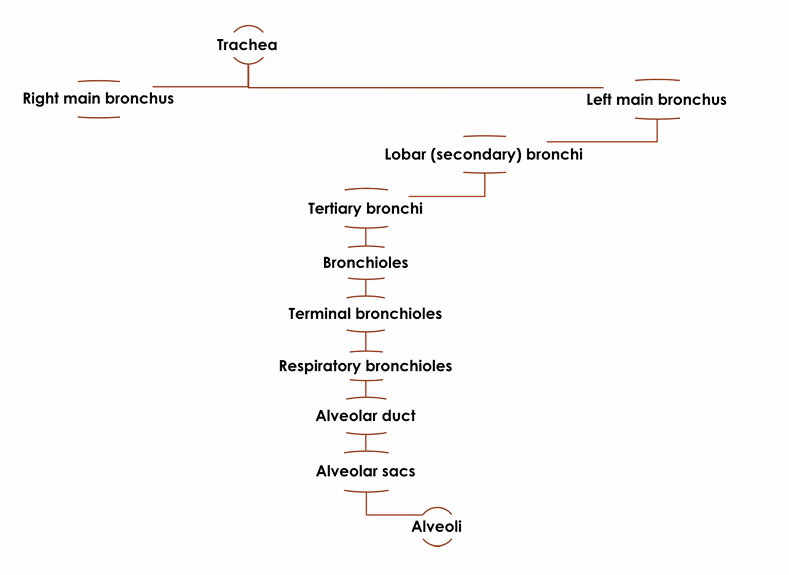
conducting airways
-trachea
-bronchi
-bronchioles + terminal bronchioles
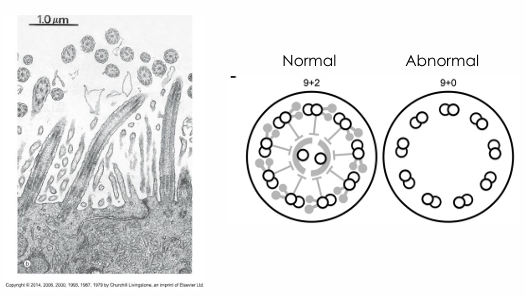
conducting airways details/functions
-conduits for air transfer
-cartilage: prevent airway collapse
-trapping/evacuation of material (mucociliary elevator): cilia, mucus (goblet cells and submucosal glands)
-air warming and moisture
-impaired function of cilia
-reduced/absent mucus clearance
-chronic respiratory infections
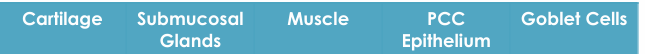
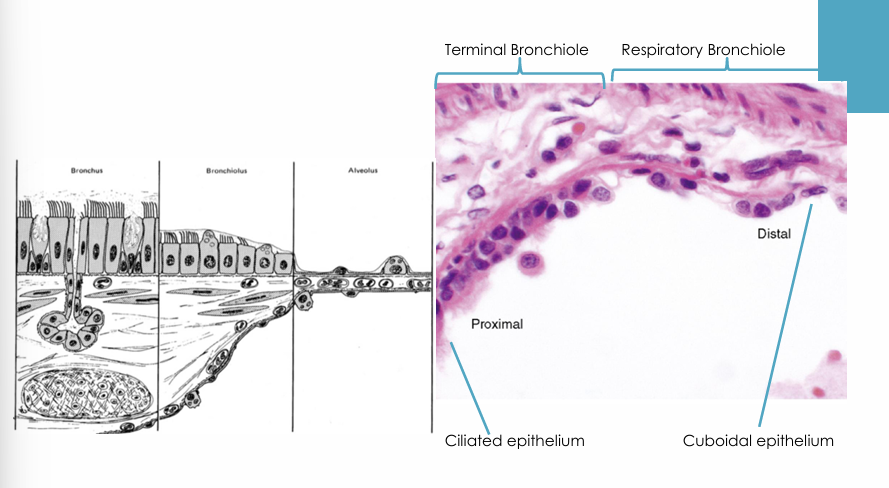
trachea, bronchi, bronchioles
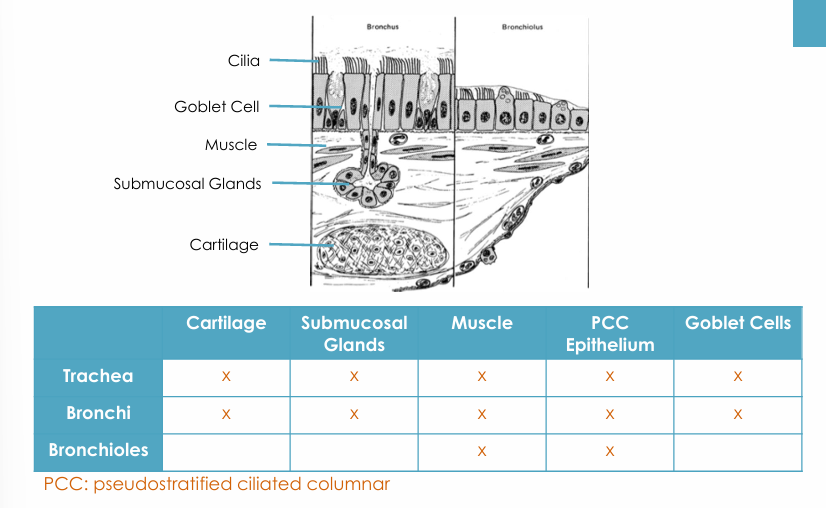
trachea
-smooth muscle
-cartilage: C-shaped
-submucosal glands
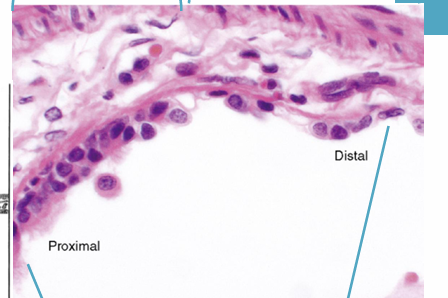
-respiratory epithelium: pseudostratified, ciliated, columnar
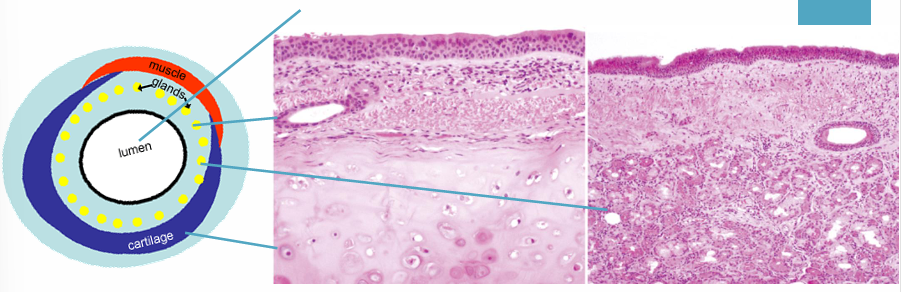
-submucosal glands
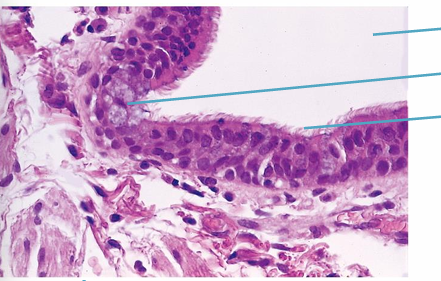
-pseudostratified ciliated columnar epithelium
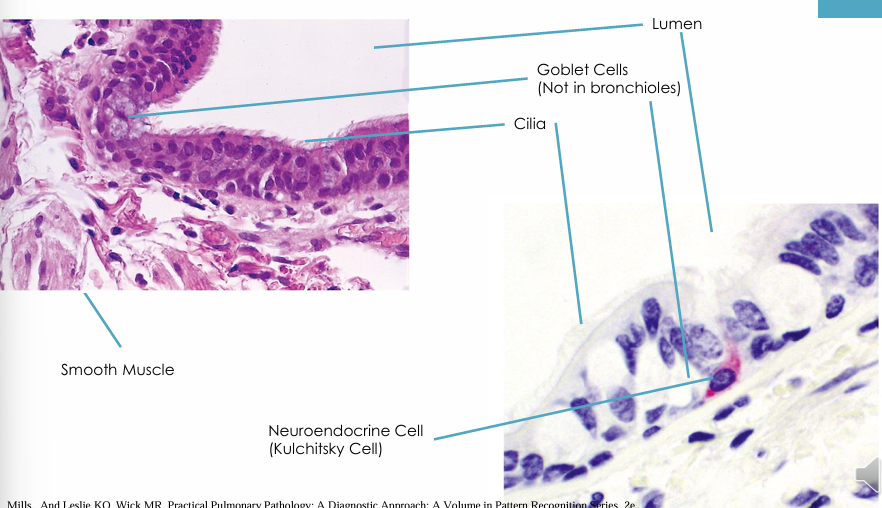
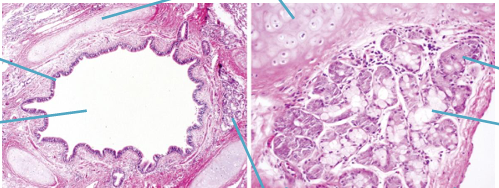
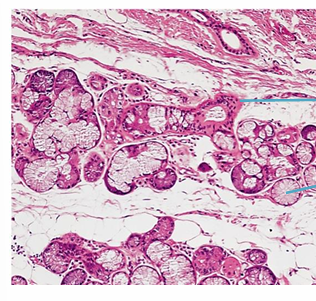
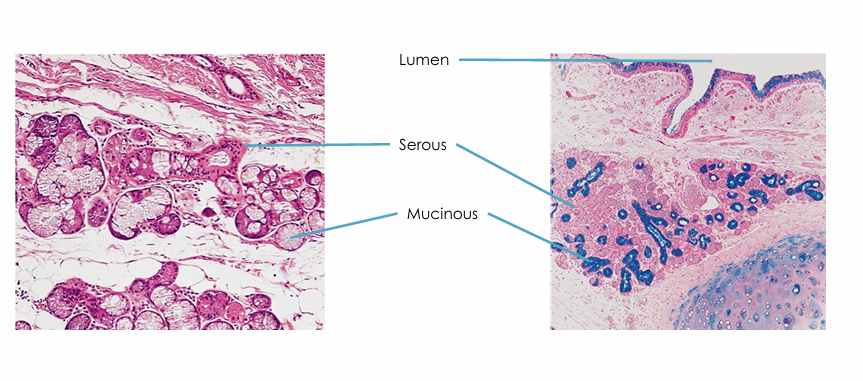
-bronchi begin at carina
-smooth muscle
-cartilage: decreases in density, change in arrangement (C-shaped to puzzle-like pieces)
-submucosal glands: serous, mucinous
-respiratory epithelium: pseudostratified, ciliated, columnar
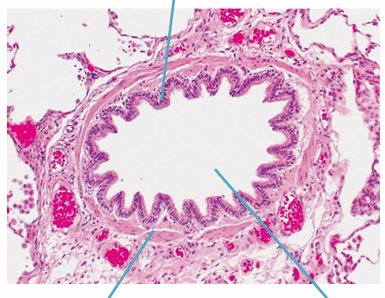
-bronchioles
-final air conductors: smallest- terminal bronchioles (<1mm diameter)
-smooth muscle
-respiratory epithelium: pseudostratified, ciliated, columnar
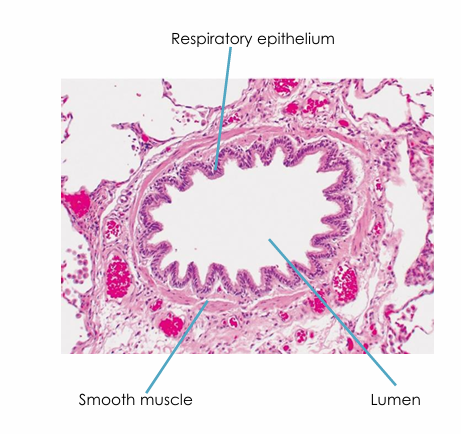
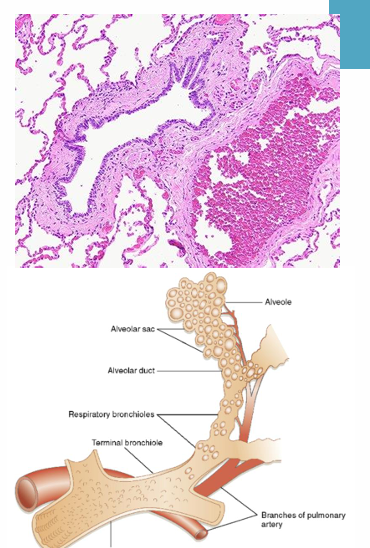
gas exchange unit (acinus)
-acinus: respiratory bronchioles (1st airways that have alveoli budding from their walls), alveolar ducts, alveolar sacs (aggregation of alveoli)
-lobule
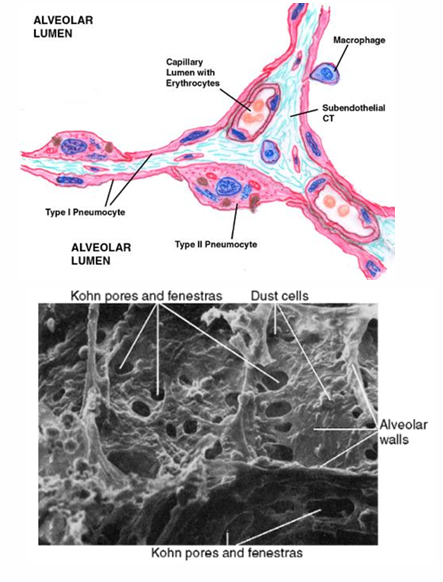
alveoli- type I epithelial cells
->90% alveolar wall surface
-thin and flat cells
-suited for gas exchange
alveoli- type II epithelial cells
-cuboidal cells
-decreased surface area compared to type I
-increased number compared to type I
-produce and secrete surfactant- lowers surface tension, prevents alveolar collapse at low pressures
-progenitor cells for type I and type II cells
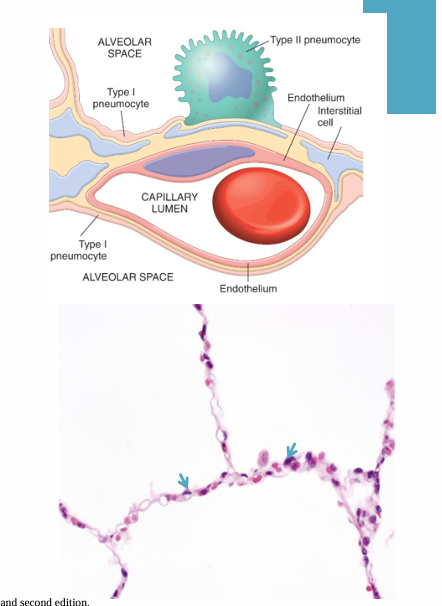
alveolar walls
-components: capillaries, connective tissue (elastic fibers), cells (sparse)- smooth muscle cells, fibroblast-like cells, lymphocytes
-epithelial cells and capillary basement membranes fused
-pores of Kohn: facilitate communication between alveolar sacs
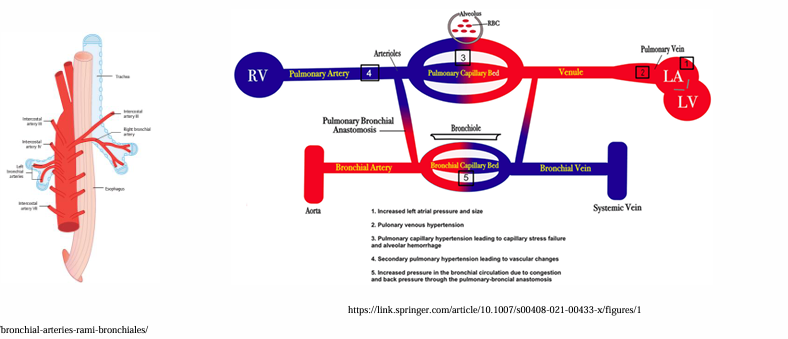
vessels
-pulmonary circulation: pulmonary artery and vein
-systemic (bronchial) circulation: bronchial artery and vein
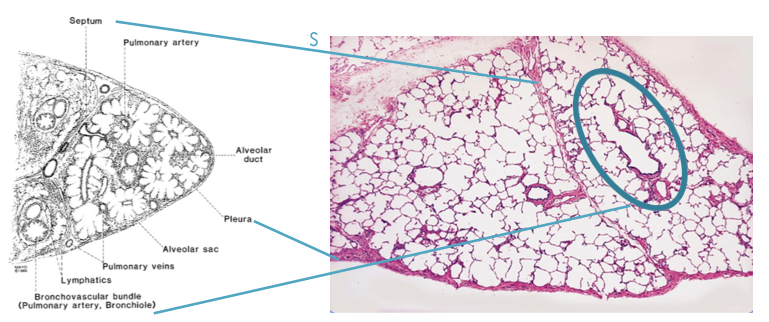
pulmonary arteries
-carry venous blood to the lung for gas exchange with inspired air
-run parallel with the airways
-diameter of airway and artery is similar
-comprised of 3 layers: intima, media, adventitia
pulmonary veins
-carry oxygenated blood to the heart
-travel separate form the arteries (except large veins at hilum): venous side of alveolar capillary bed, interlobular septa, larger pulmonary veins run in the interlobular septa
lymphatics
-bronchovascular sheath
-interlobular septa
-pleura

bronchial arteries and veins
-artery: arise from the aorta, supply arterial blood to the lung
-vein
lung development
-week 28
-sufficient respiratory development
-type I and type II cells- surfactant to reduce surface tension and allow expansion
-premature baby can usually breathe on its own
respiratory distress syndrome (RDS)
-infants born prematurely (mostly <28 weeks)
-insufficient surfactant production: prevents proper inflation of lungs, dyspnea and gas exchange is compromised
-treatment (supportive): surfactant therapy, supplemental oxygen, steroids
sequestration (extralobar)
-lung tissue that does not communicate with the tracheobronchial tree
-occur outside visceral pleura of adjacent lobe
-systemic (rather than pulmonary) arterial supply
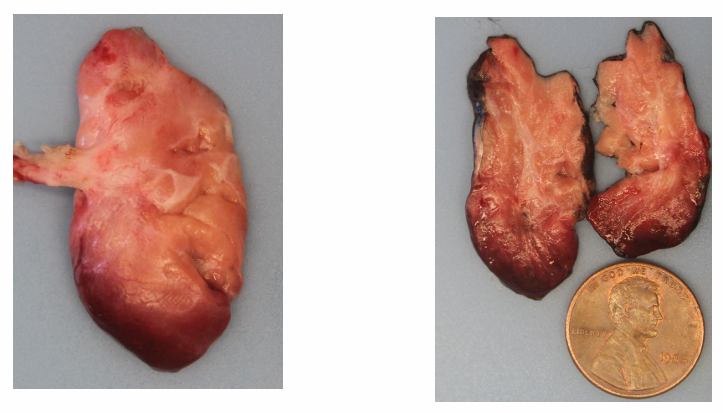
sequestration (intralobar)
-lung tissue that usually does not communicate with the tracheobronchial tree (but may and get infected)
-lacks its own visceral pleura
-systemic (rather than pulmonary arterial supply)
key learning points
ventilation and oxygenation
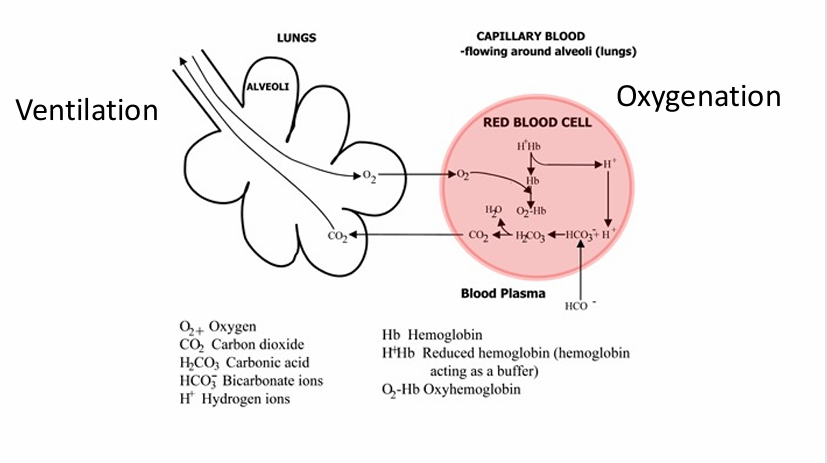
ventilation
-movement of gases between the atmosphere and the alveoli
-functions: provide atmospheric O2, remove CO2, maintain acid-base homeostasis
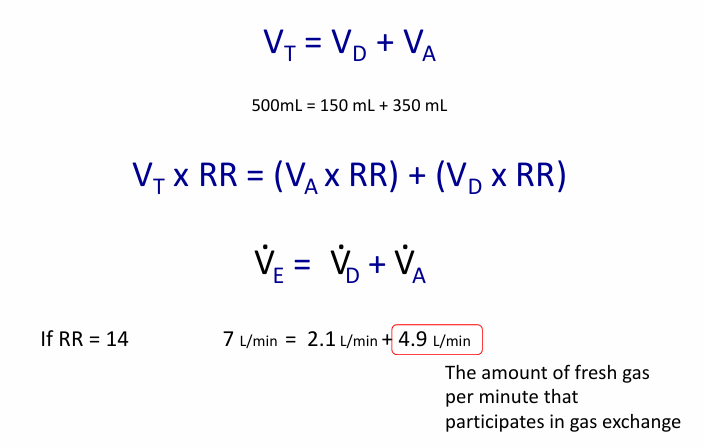
terms- tidal volume, minute ventilation, dead space, dead space ventilation, alveolar ventilation
-tidal volume: volume of a single breath
-minute ventilation: volume of gas moved in 1 min (tidal volume x breaths per minute)
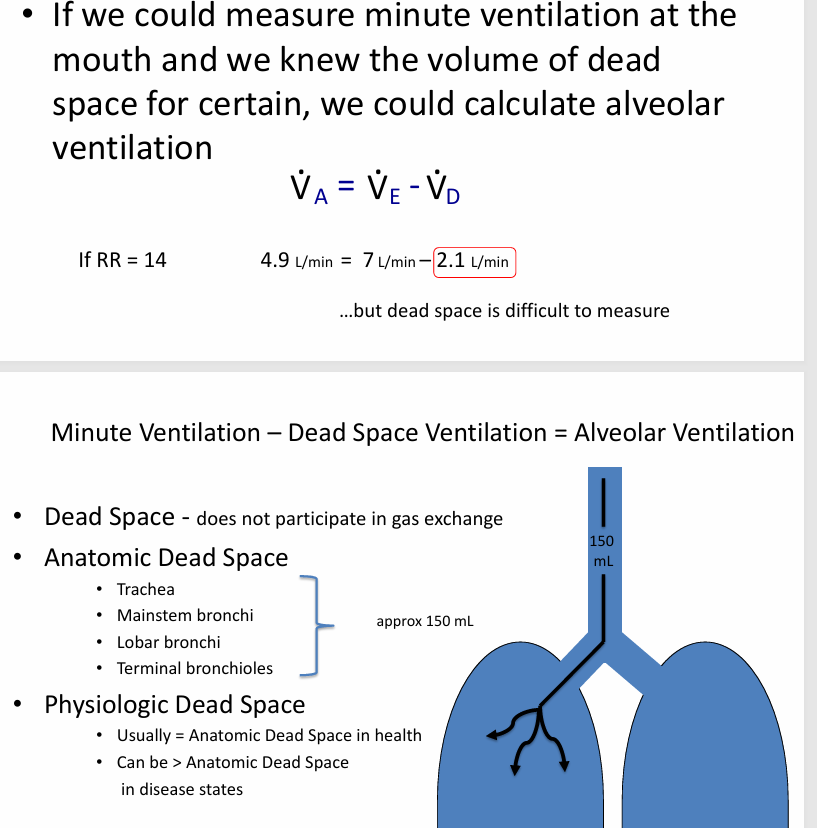
-dead space: parts of the respiratory system that do not participate in O2 and CO2 exchange (trachea, mainstem bronchi, lobar and segmental bronchi, terminal bronchioles)
-dead space ventilation: amount of ventilation “wasted” on the dead space volume
-alveolar ventilation: volume of gas seen by the alveoli (minute ventilation - dead space ventilation = alveolar ventilation)
delivery of O2 to the alveoli
-atmospheric O2 is source of fresh O2 for cellular metabolism
-hypoxemia: insufficient O2 in the blood
-hypoxia: insufficient O2 in an organ/tissue
-hypoxemia → tissue hypoxia → death
removal of CO2 from the blood
-hypercapnia: too much CO2 in the blood
-hypercapnia leads to: increased cerebral blood flow, intracranial pressure, tremor, confusion, respiratory depression, coma, death
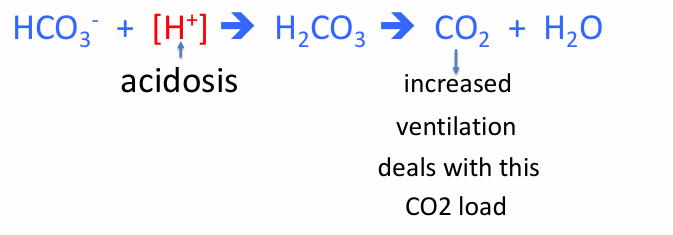
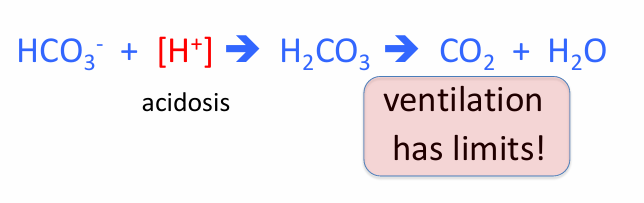
acid-base homeostasis
-ventilation helps to maintain
-CO2 is an acid
-body can increase or decrease ventilation to adjust CO2 levels in lungs, which in turn adjusts CO2 levels in the blood, in order to maintain a suitable pH in the setting of metabolic changes
-similarly, any change in ventilation for another reason will change CO2 levels in lungs, which in turn changes CO2 levels in the blood, leading to changes in blood pH
-an increase in blood CO2 levels causes acidemia (decreased pH)
-a decrease in blood CO2 levels causes alkalemia (increased pH)
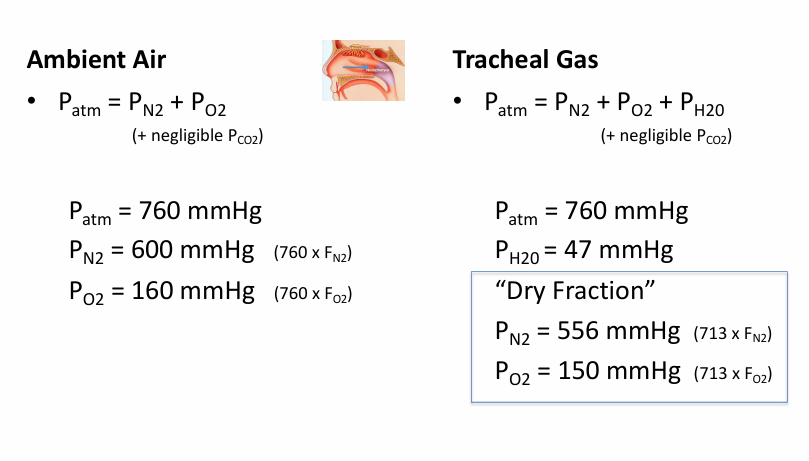
room air
-78% nitrogen
-21% oxygen
-1% other
fractional concentration of a gas
-relative concentration of a gas in a mixture
-presented as a % or decimal
-abbreviated “F”
-for air, this relationship is consistent regardless of air pressure: FN2 = 0.78 or 78%, FO2 = 0.21 or 21%
gas pressure
-used as surrogate for the amount of a particular gas in a mixture of gases
-proportional to the fractional concentration of the gas in the mixture
partial pressures of gases
-in a mixture of gases at any given pressure, each of the gases exerts a pressure that is proportional to the fractional concentration of that gas in the mixture
-Pgas = Fgas x Ptotal
-used as a measure of the amount of that gas in the mixture
-abbreviated “P”, measured in mmHg
-if the pressure of a gas mixture is 100 mmHg and Helium makes up ¼ of the mixture (FHe = 0.25) then the partial pressure of Helium is 25 mmHg (PHe = 25 mmHg)
atmospheric pressure
-depends on altitude
gasses dissolved in a liquid come to an equilibrium at
-the gas-liquid interface
-if the pressure of a gas mixture is 100 mmHg and Helium makes up ¼ of the mixture (FHe = 0.25) then the partial pressure of Helium is 25 mmHg (PHe = 25 mmHg)
inspired gas v room air
-inspired air: both warmed and humidified by the mucous membranes of the nasopharynx
-by the time inspired air reaches the trachea, it is fully saturated with water vapor, which displaces some of the gases so that the total gas pressure within the lung remains equal to the air pressure outside (760mmHg)
-water vapor exerts a partial pressure of 47mmHg at the body temperature
-760-47 = 713mmHg available for fractions of other gases
ambient air, tracheal gas- “dry fraction”
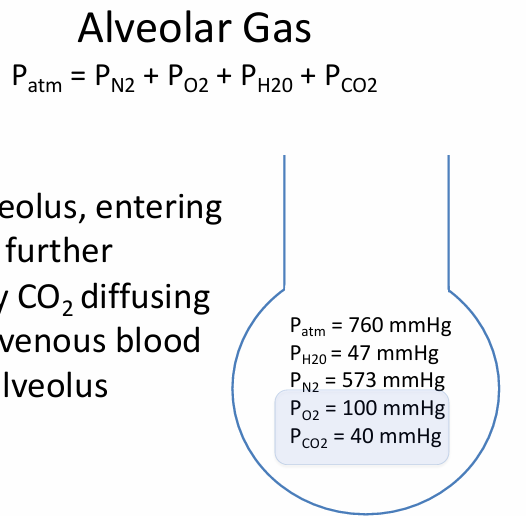
alveolar gas
-in alveolus, entering gases are further diluted by CO2 diffusing from the venous blood into the alveolus
alveolar/capillary gas relationship
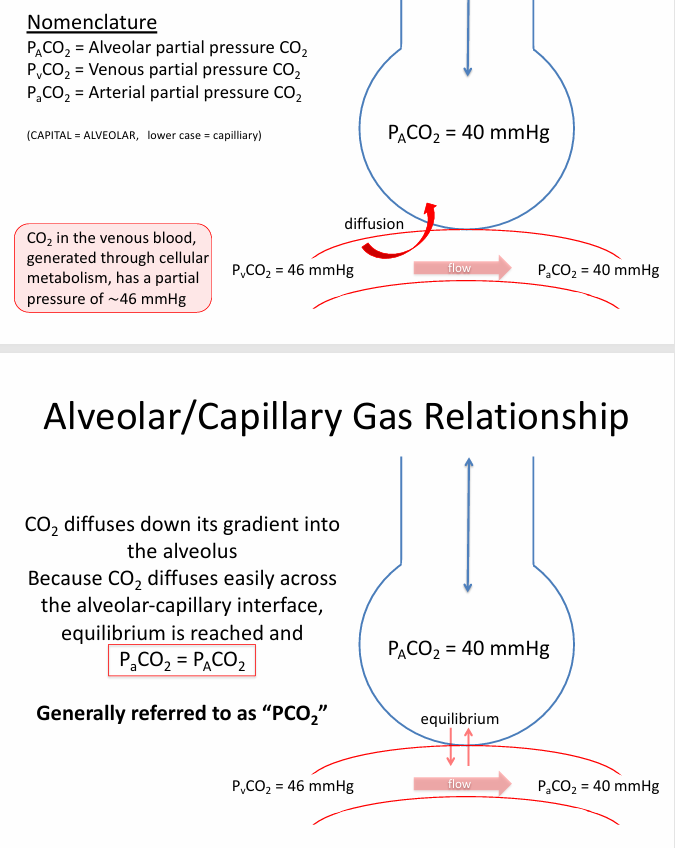
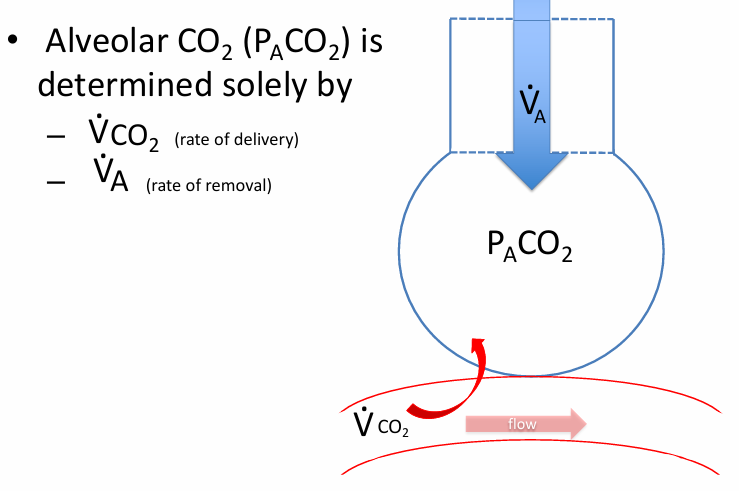
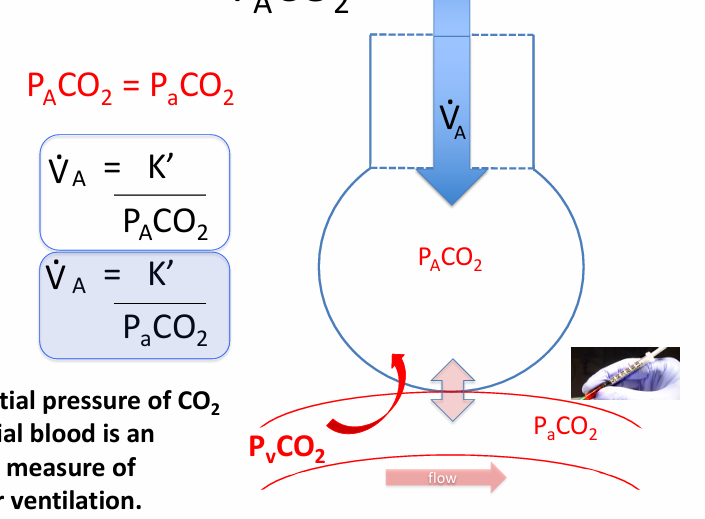
CO2 & the alveoli
-CO2 is continuously diffusing into the alveoli from the capillary blood
-CO2 is continuously being removed from the alveoli by alveolar ventilation
-end capillary blood is in equilibrium with the CO2 in the alveoli
-PaCO2 = PACO2
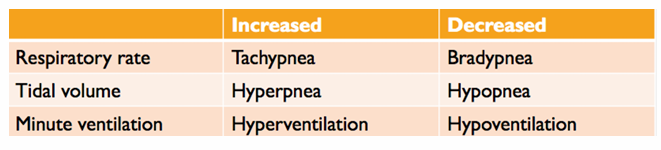
normal breathing
-respiratory rate (rr) = 10-16 breaths per minute
-tidal volume (Vt) = approximately 0.5L
-minute ventilation (Ve) = 5-8 L/min
pathologic breathing
-alveolar hypoventilation: alveolar ventilation insufficient for the body’s needs
-alveolar hyperventilation: alveolar ventilation in excess of what is needed
nomenclature (with symbols)
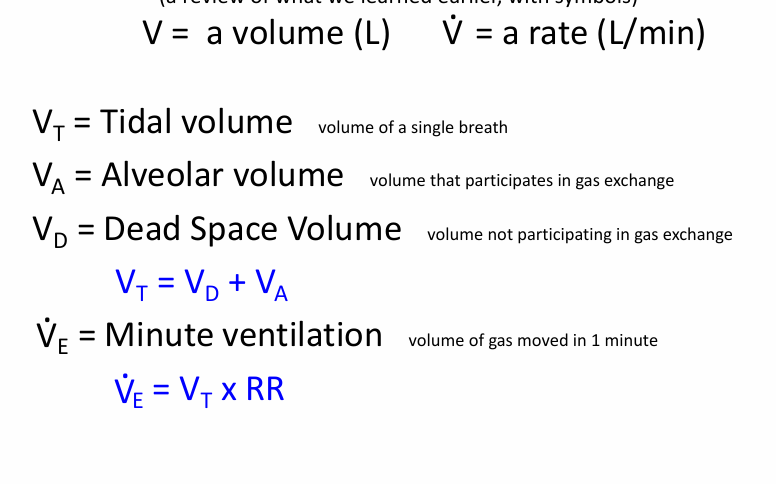
alveolar ventilation per minute
alveolar ventilation measurement
could measure alveolar ventilation by measuring
-the gas composition (Pgas) in the alveolus
what effects alveolar gas composition (Pgas)?
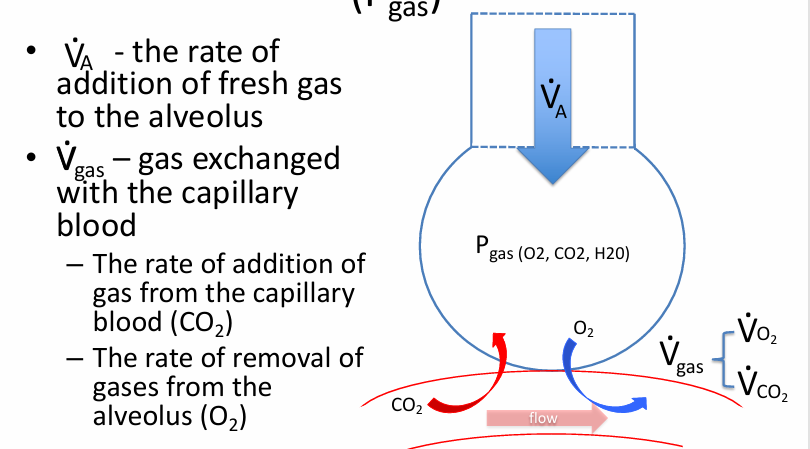
components of Pgas- PAO2 + PACO2
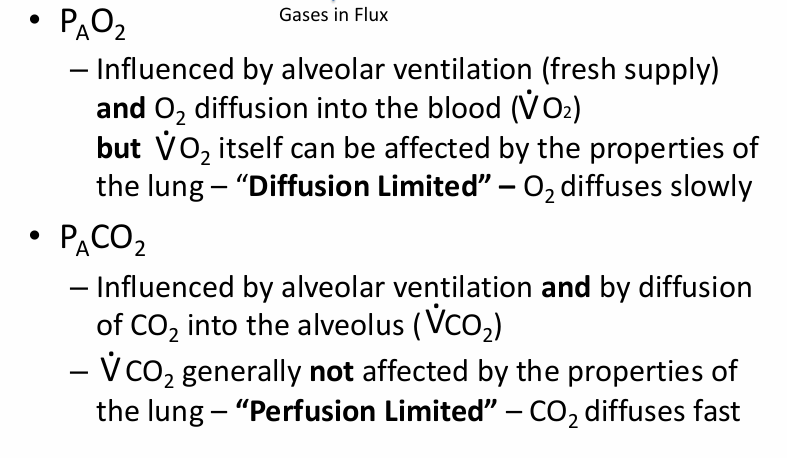
PACO2
VCO2
-CO2 highly soluble in tissues
-CO2 diffuses readily and quickly across the alveolar/capillary interface and into the alveolus
-CO2 transfer not limited by the properties of the lungs
-CO2 transfer dependent on amount of CO2 delivered to the alveolus: CO2 production in the tissues, cardiac output, “perfusion limited” (less readily diffusible gases are said to be “diffusion limited”)
PACO2 is a balance of
-how fast it is delivered to the alveolus and how fast it is removed (a balance of inflow and outflow)
-PatmCO2 = 0 (negligible)
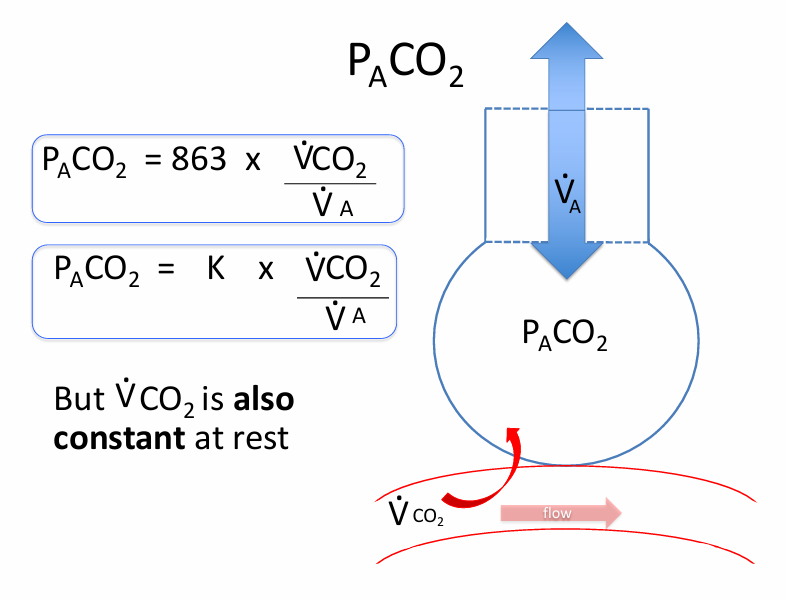
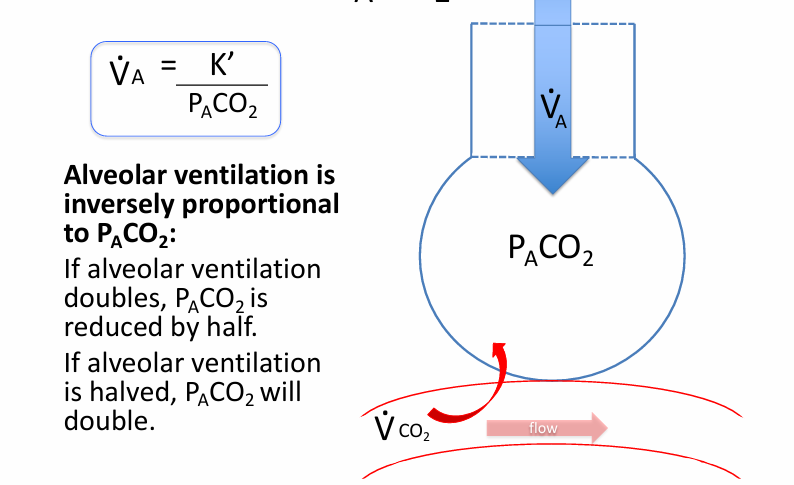
alveolar ventilation and PACO2
PaCO2
-CO2 diffuses readily and rapidly down its diffusion gradient
-equilibrium is rapidly reached between the alveolar CO2 and capillary blood
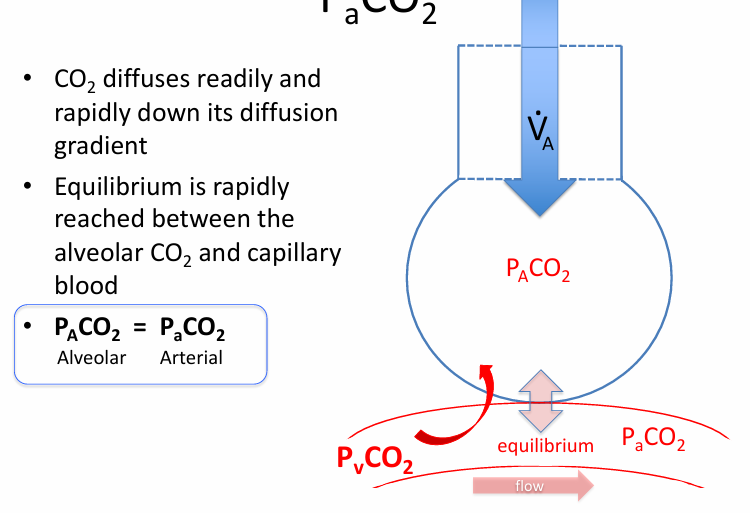
partial pressure of CO2 in arterial blood is an indirect measure of
-alveolar ventilation
arterial blood gases
-direct measures of pH, PaCO2, and PaO2
-calculates a saturation (SaO2)
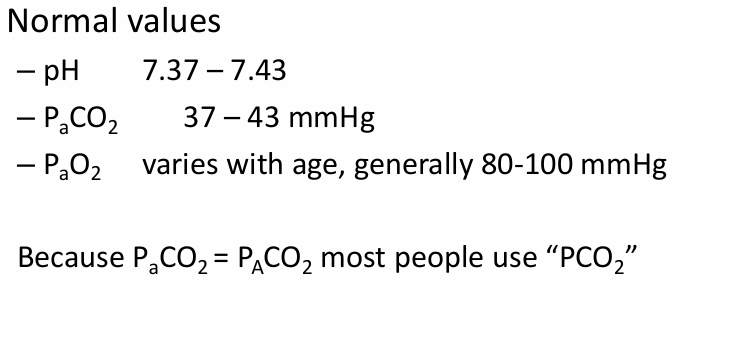
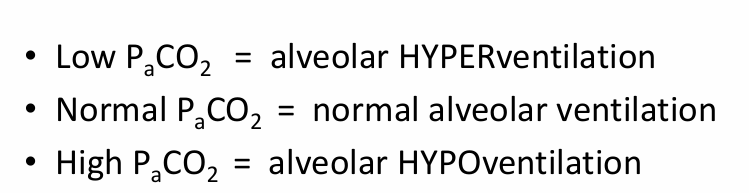
alveolar hyperventilation
-an increase in alveolar ventilation
-defined by a PaCO2 < 37 mmHg
-hyperventilation leads to hypocapnia (hybocarbia)
alveolar hypoventilation
-a decrease in alveolar ventilation
-defined by a PaCO2 > 43 mmHg
-hypoventilation leads to hypercapnia (hypercarbia)
terms for low, normal, and high PaCO2
causes of hyperventilation
-cause increased respiratory drive:
-exercise
-pain
-hypoxemia
-high altitude
-acidemia (low blood pH)
-pregnancy
-lung diseases
-head injury
-heart failure (Cheyne Stokes respirations)
causes of hypoventilation
-decreased respiratory drive: examples- opioids, benzodiazepines, alcohol
-neuromuscular impairment: examples- muscular dystrophy, spinal cord injury, peripheral neuropathy
-chest wall or spinal deformity: examples- severe scoliosis, pectus excavatum, morbid obesity
-muscular fatigue: example- a person with severe acute hypoxemia hyperventilating for hours develops respiratory muscle fatigue and exhaustion, leading to hypoventilation
hypoventilation due to fatigue
-increased work of breathing due to altered respiratory mechanics- severe asthma attack with increased airway resistance
-increased ventilatory demand- acidemia, sepsis
-increased physiologic dead space- PE, emphysema
increased physiologic dead space in pulmonary embolism
-dead space = ventilation to areas that do not participate in gas exchange
-blood clot occluding a pulmonary artery leads to areas of lung that receive ventilation but no perfusion
-if the patient can increase MV (Vt x RR) to compensate, PaCO2 may be normal, but this increases the work of breathing, which may lead to respiratory muscle fatigue
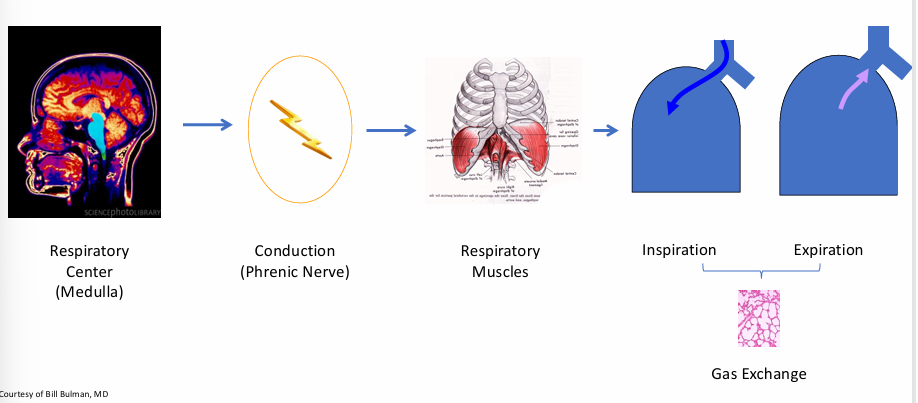
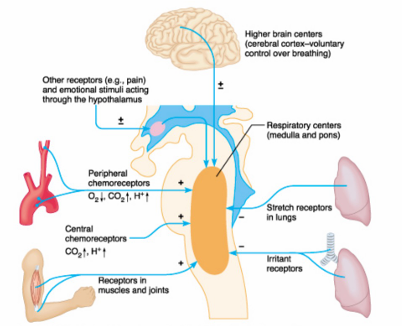
control of ventilation
-central controller
-sensors
-effectors
central control
-significant voluntary control of breathing, within limits
-cortex can temporarily override the brainstem: voluntary hyperventilation, breath holding
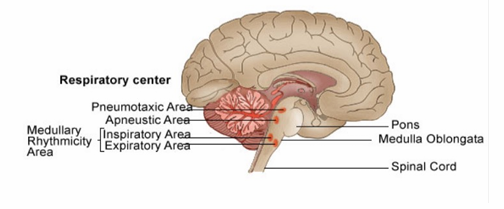
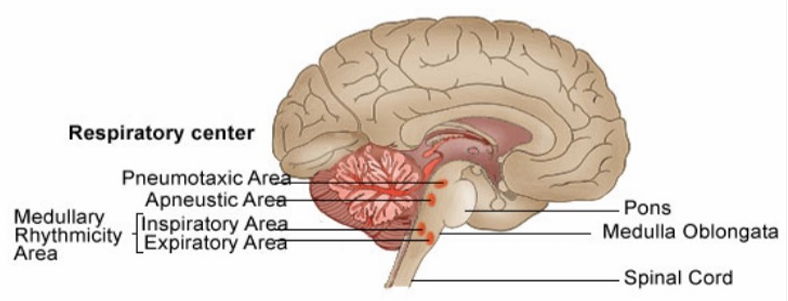
central control includes
-medulla: medullary rhythmicity area- inspiratory = dorsal respiratory group (sets and maintains the RR); expiratory = ventral respiratory group (inactive during resting breathing)
-pons: pneumotaxic center- inspiratory “off switch” (regulates the amount of air taken in each breath)
sensors
-central chemoreceptors
-peripheral chemoreceptors
-lung receptors
central chemoreceptors
-surrounded by the brain’s extracellular fluid (ECF)
-respond to changes in [H+] concentration: increased [H+]- stimulates ventilation, decreased [H+]- inhibits ventilation
-composition of the brain ECF (and [H+]) concentration determined by: CSF, local CNS metabolism, local blood flow
PaCO2 levels regulate ventilation by
-altering the pH of the CSF
-CSF is separated from the blood by the blood-brain barrier (BBB)
-CO2 diffuses readily across the BBB
-when PaCO2 rises, CO2 diffuses from the cerebral vessels into the CSF and liberates [H+]
-CO2 + H2O → H2CO3 → HCO3- + [H+]
-if PaCO2 rises, central chemoreceptors are stimulated, inducing hyperventilation which lowers PaCO2
![<p>-altering the pH of the CSF</p><p>-CSF is separated from the blood by the blood-brain barrier (BBB)</p><p>-CO2 diffuses readily across the BBB</p><p>-when P<sub>a</sub>CO2 rises, CO2 diffuses from the cerebral vessels into the CSF and liberates [H+]</p><p>-CO2 + H2O → H2CO3 → HCO3- + [H+]</p><p>-if P<sub>a</sub>CO2 rises, central chemoreceptors are stimulated, inducing hyperventilation which lowers P<sub>a</sub>CO2</p>](https://knowt-user-attachments.s3.amazonaws.com/c5746b12-f944-4b08-9281-bc237c2936e3.png)
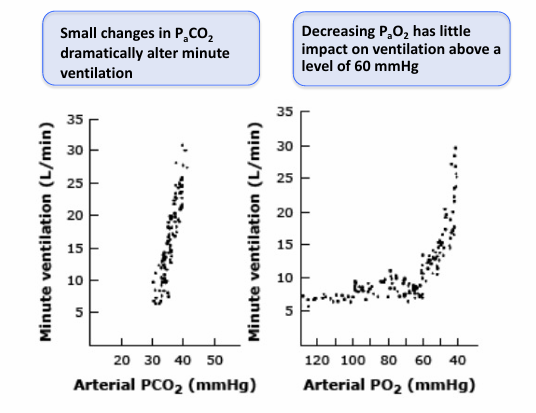
_____ is the most important factor in regulating ventilation under normal conditions
-PaCO2
-PaCO2 = PACO2 = PCO2
central receptors respond to changes in
-PaCO2
other important inputs
-peripheral chemoreceptors
-lung receptors: stretch receptors, irritant receptors, juxtacapillary receptors (J receptors) in alveolar walls, bronchial c fibers (respond to changes in the bronchial circulation)
-musculoskeletal receptors
-cortical input
ventilation in health and disease
-ventilation is very tightly regulated around a PCO2 = 40 mmHg
-as CO2 production increases in exercise, ventilation increases to meet this demand and maintain a normal PCO2 and pH
-H+ production can increase in disease (sepsis, lactic acidosis, ketoacidosis); ventilation increases to meet this demand and maintain a normal PCO2 and pH
ventilation in disease
-acid production can exceed ventilatory capacity
-ventilatory capacity can be limited by disease
-respiratory muscles can fatigue
“CO2 narcosis”
-a rise in PaCO2 will stimulate the central chemoreceptors, which in turn drive the effectors (respiratory muscles) to increase ventilation to bring PaCO2 back down
-when PaCO2 is very high, it acts as a CNS depressant, causing diminished mental status and a reduction in TV, RR, and MV, which worsens alveolar hypoventilation and worsens hypercapnia
how to assess pathology?
-airways
-parenchyma: alveolar spaces, alveolar walls (cellular, fibrotic), nodules
-vessels