Mood Disorders and Suicide
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
25 Terms
mood disorders
characterized by severe disturbances in mood and emotions; most often depression, but also mania and elation
These people also experience mood fluctuations, but their fluctuations are extreme, distort their outlook on life, and impair their ability to function
Symptoms can range from the extreme sadness and hopelessness of depression to the extreme elation and irritability of mania
differ from normal mood states in duration and severity
lasts for several weeks or more
causes extreme distress or impairment in functioning
specifiers: course, severity, features, onset
depressive disorders (also called unipolar disorders)
a group of disorders in which depression (intense and persistent sadness) is the main feature
Depressed people feel sad, discouraged, and hopeless; they lose interest in activities once enjoyed, experience a decrease in drives (ex: hunger), and frequently doubt personal worth
major depressive disorder and persistent depressive disorder (dysthymia)
bipolar and related disorders
group of disorders in which mania (a state of extreme elation and agitation) is the defining feature
When people experience mania, they may become extremely talkative, behave recklessly, or attempt to take on many tasks simultaneously
bipolar disorder type I, bipolar disorder type II, Cyclothymia
types of episodes: manic, hypomanic, and mixed
major depressive disorder diagnostic criteria
Presence of a single major depressive episode and no history of a
manic episodeMDE – Five or more of the following, within a two week period.
Depressed mood, almost every day
Markedly diminished interest or pleasure
Change in weight (when not dieting) or appetite
Insomnia or hypersomnia
Psychomotor agitation or retardation
Fatigue or loss of energy
Feelings of worthlessness, or excessive or inappropriate guilt
Diminished ability to think, concentrate, make decisions
Recurrent thoughts of death, suicidal ideation (with or without
specific plan), or suicide attempt
major depressive disorder
Characterized by a depressed mood most of the day, nearly every day (sad, empty, hopeless), and loss of interest and pleasure in usual/gratifying activities
Extremely heterogeneous symptom presentation! Considering all the different combinations of symptoms, there are over 16,000 different possible profiles!
Lifetime prevalence is 10-25% for women and 5-12% for men
First episode often occurs following a severe psychosocial stressor, but this is less common for subsequent episodes
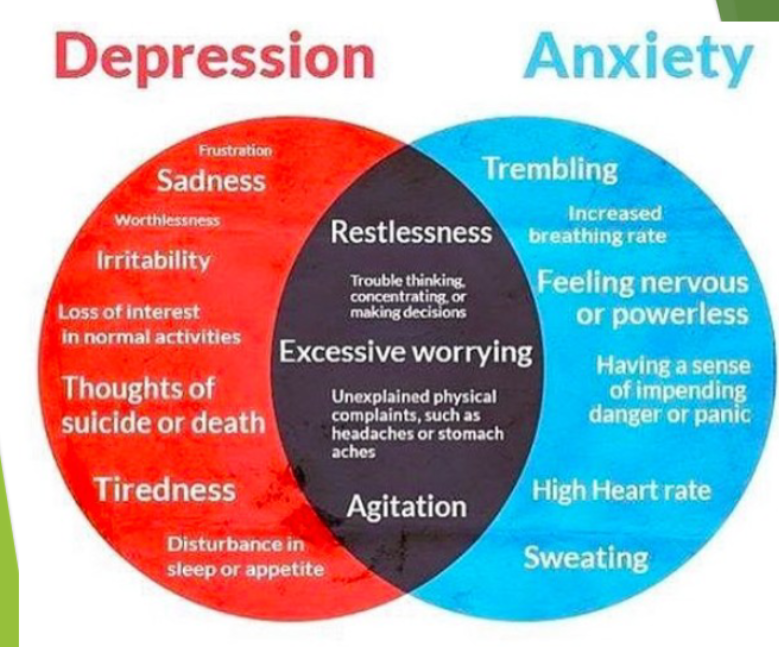
50% have a comorbid anxiety disorder
Average age of onset is mid-20s, but this appears to be getting younger
60% of people who experience a MDE will experience a second, 70% with two with experience a third, and 90% with three will
experience a fourth1 year after diagnosis, 40% will still meet criteria for MDD, 20% have symptoms that do not meet criteria, and 40% have no mood
disorderOne of the most controversial changes in DSM5 was the removal of the “bereavement exception” for MDD which was in DSM-IV
That means that clinicians can now diagnose depression shortly after the death of a loved one, though there are guidelines about when this should be done
persistent depressive disorder (Dysthymia)
Depressed mood most of the day for at least two years (one year in children), with no more than two months at a time in which criteria are not met
Two or more of the following when depressed:
Poor appetite or overeating
Insomnia or hypersomnia
Low energy or fatigue
Low self-esteem
Poor concentration or difficulty making decisions
Feelings of hopelessness
Female : male ratio is about 1:1 in children and adolescents, but 2-3x more common in women than men in adulthood
Onset is often early and insidious
Differentiating between dysthymia and MDE is difficult, as they share many symptoms
DD is more chronic and has less severe symptoms

premenstrual dysphoric disorder
During most menstrual cycles, in the week before onset of menses, a total of five of:
One of: mood lability, irritability, depressed mood, or anxiety
One of: Decreased interests, problems concentrating, lack of energy, changes in appetite/cravings, changes in sleep, feeling of being overwhelmed, physical symptoms (breast tenderness, joint pain, bloating)
1-year prevalence of around 1-2%
Heritability of about 50%
manic/hypomanic episode
Period of abnormally and persistently elevated, expansive, or
irritable mood lasting at least 4 (hypomanic) or 7 (manic)
daysAt least three or more, unless mood is irritable (4)
Inflated self-esteem or grandiosity
Decreased need for sleep
More talkative
Flight of ideas or racing thoughts
Distractibility
Increased goal-direct activity or psychomotor agitation
Excessive pleasurable activities that have high potential for
painful consequences (financial, s*xual, etc)
Hypomanic episode does not cause marked impairment in
social or occupational functioning, does not require
hospitalization, and does not have psychotic features
mixed episode
Period of time lasting at least four days where criteria for Manic episode and Major Depressive episode are both met
Very rapid cycling of moods, or a mix of extremely high and low emotions
Sometimes occurs following somatic treatment for unipolar depression (antidepressant medication, phototherapy, ECT), and may make patients more vulnerable to future manic episodes
bipolar disorders
Bipolar Type I
At least one manic or mixed episode
Major depressive episode is not required for diagnosis, but most patient have one
Bipolar Type II
Recurrent major depressive episodes with hypomanic episodes
Cyclothymia
Hypomanic episodes with depressive episodes that do not meet criteria for MDE
Two year duration
Prevalence of BD Type 1 is 0.6-0.1%, Type II is 1.1%, cyclothymia is 0.5-2.5%
Childhood bipolar is a controversial topic!
40% increase in Dx of BP in children between 1994 and 2003
Differential diagnoses include severe ADHD, oppositional-defiant disorder, and disruptive mood dysregulation disorder (severe and developmentally inappropriate temper outbursts, and irritability)
specifiers for bipolar and depressive disorders (but mostly depressive)
With anxious distress
Symptoms of general anxiety co-occur with mood symptoms
Melancholic features
Extreme anhedonia (lack of interest to things that typically bring joy) or lack of mood reactivity
Despondency, despair
Mood worse in the early morning
Early awakening
Marked psychomotor retardation or agitation
Significant weight loss
Excessive guilt
Melancholic depression is associated with a different set of biomarkers compared to other types of depression, involving altered reward processing (limbic-cortical pathways)
With seasonal pattern (depressive disorders only)
Regular temporal relationship between onset of mood symptoms and particular time of the year
Not surprisingly, more common at higher latitudes (2-3%
prevalence in Canada)
Postpartum onset (depressive disorders only)
Onset of episode within 4 weeks postpartum
Distinguish from baby-blues (70% of women) which does not
impair functioning10-20% of mothers and 10% of fathers
specifiers for bipolar disorders (and also depressive)
Atypical features (though actually common)
Mood reactivity, increased appetite or weight, and hypersomnia
Pattern of rejection sensitivity
Psychotic features
Delusions or hallucinations (usually mood congruent, often persecutory)
Catatonia
Motor immobility, excessive pointless motor activity, extreme negativism, posturing, echolalia (repetition of words/phrases spoken by someone else) or echopraxia (imitation of someone’s physical movements or facial expressions)
Four or more distinct mood episodes in a 12 month period
Episodes separated by either full remission or switch to
opposite pole (MDE to manic)
specifiers for depressive and bipolar disorders: severity
Mild – only minimally meets criteria
Moderate – between mild and severe
Severe – needs near constant supervision to avoid threat of harm to self or others, or has psychotic features
etiology of depressive and bipolar disorders
Genetics
Heritability of MDD estimated at 0.36, while heritability of bipolar disorder estimated at 0.8 or higher
The famous (but very incomplete) monoamine hypothesis
Insufficient serotonin and other monoamines in the brain, BUT, reductions in serotonin, dopamine, and
norepinephrine are not always associated with depressionSSRIs immediately increase serotonin levels, but depression symptoms take weeks to change
stress and deregulation of the HPA axis
overlap with marijuana induce amotivational syndrome
several brain areas with abnormal activation in major depression:
amygdala (abnormal activation)
prefrontal cortex (less activation)
anterior cingulate (less activation)
insula (greater activation)
hypothalamus (greater activation)
childhood and adult attachments - mood disorders more common individuals with insecure and anxious/avoidant attachment styles than those with secure attachment
cognitive theories
maladaptive thoughts (cognitive distortions)
schemas may represent a diathesis
behavioral theories
emphasize maintenance of the mood disorder
avoidance of pleasurable activities, lacks of assertiveness, habits around sleep/eating/social activity
treatment for depressive and bipolar disorders
Psychotherapy
CBT, interpersonal, and brief psychodynamic therapy are all empirically validated treatments for major depressive disorder
Some evidence that CBT and mindfulness-based CBT are more effective at preventing relapse than other treatments
Changing automatic thoughts, behaviours, and schemas that maintain and exacerbate depression
Medication for unipolar depression (efficacy is equivalent, effectiveness depends on the person)
Tricyclic antidepressants (TCAs)
Monoamine oxidase inhibitors (MAOIs)
Selective serotonin re-uptake inhibitors (SSRIs)
Serotonin-norepinephrine re-uptake inhibitors
(SNRIs)
Combination of medication and psychotherapy
In adolescents, chronic depression, or severe depression, a combination of treatments appears to be superior to either treatment alone
Medications for Bipolar mood disorders
Lithium
Anticonvulsants
Antipsychotics
Antidepressants (carefully)
Other therapies
Phototherapy for seasonal mood disorders
Electroconvulsive therapy (ECT)
Transcranial magnetic stimulation (TMS)
Deep brain stimulation (DBS)
suicide
Worldwide, about one million people die by suicide per year, 10- 20 million attempts
11.3 per 100,000 people in Canada
17.8 in males, 5.1 in females
Second highest cause of death in people aged 10-24
Highest single cause of death in boys 15-19
In North America, suicide is considerably more common in rural than urban environments
Availability of methods, geographical barriers to help seeking, culture of independence, stigma, privacy concerns, economic changes
Suicide clusters and suicide pacts
SAD PERSONS (sex, age, depression, previous attempt, excess alcohol or substance, rational thinking lost, social supports lacking, organized plan, no spouse, sickness)
<5 is low risk, >6 is high risk
suicide - definitions
Suicidal ideation: thoughts of death and/or plans for suicide
Suicidal gestures: behaviours that look like suicide attempts, but are not life-threatening
Suicide attempt: carrying out a plan to actually die by suicide, that does not result in death
Completed suicide: carrying out a suicidal plan that results in death
Suicide survivors: family, friends, co-workers, professionals involved in care, of someone who completes suicide
suicide and psychological disorders
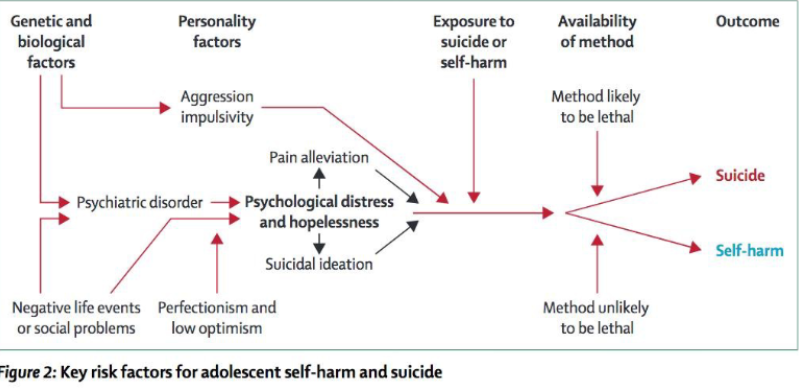
Up to 90% of people who die by suicide have a mental illness (70% have MDD; 46% have substance abuse disorders)
Up to 10% of people with schizophrenia will complete suicide
Social factors
Loss of cultural and social identity in First Nations, intergenerational transmission of trauma
Massive social changes in rapidly industrializing countries (China)
Relative acceptability of suicide in some cultures (comparing North Americans of European to African ancestry); Indigenous people have higher suicide rates
suicide prevention
High risk groups
Screening, observation and removal of means, specific treatments and interventions (DBT), aggressive treatment or hospitalization?
Suicide contracts – safety plans
patient safety plan template
1. Warning signs (thoughts, images, mood, situation, behavior) that a crisis may be developing
2. Internal coping strategies – Things I can do to take my mind off my problems without contacting another person (relaxation technique, physical activity)
3. People and social settings that provide distraction
Step 4: People whom I can ask for help. Names and phones. Doctors, emergencies, hospitals, support lines.
Step 5: Professionals or agencies I can contact during a crisis.
Step 6: Making the environment safe
Population based
Educational programs and awareness campaigns, encourage appropriate communication/media approaches,
especially around the deaths of celebrities, restrict means or make means more difficult to use, telephone hotlines
depression attributional scale
a cognitive-behavioral theory that explains how individuals' attributions about the causes of negative events can influence their mood and behavior
It posits that people who attribute negative events to internal, stable, and global causes are more likely to develop depression
Internality: This dimension determines whether the cause of an event is attributed to factors within oneself (internal) or external factors (external).
Stability: This dimension concerns whether the cause is viewed as permanent and enduring (stable) or temporary and changeable (unstable).
Globality: This dimension determines if the cause is limited to a specific domain (specific) or influences all aspects of life (global).
A person's consistent placement along these three dimensions forms their unique explanatory style, which has profound implications for their motivation, resilience, and susceptibility to psychological distress
biological basis of mood disorders
Genetic factors play a stronger role in bipolar disorder than in MDD
People with mood disorders often have imbalances in certain neurotransmitters, particularly norepinephrine and serotonin
These neurotransmitters are important regulators of the bodily functions that are disrupted in mood disorders, including appetite, sex drive, sleep, arousal, and mood
Medications that are used to treat MDD typically boost serotonin and norepinephrine activity, whereas lithium, which is used in the treatment of bipolar disorder, blocks norepinephrine activity at the synapses
Depression is linked to abnormal activity in several regions of the brain, including those important in assessing the emotional significance of stimuli and experiencing emotions (amygdala), and in regulating and controlling emotions (like the prefrontal cortex)
Depressed people show elevated amygdala activity, especially when presented with negative emotional stimuli
Depressed people exhibit less activation in the prefrontal, particularly on the left side
Because the prefrontal cortex can dampen amygdala activation, thereby enabling one to suppress negative emotions, decreased activation in certain regions of the PFC may inhibit its ability to override negative emotions that might then lead to more negative mood states
Abnormal elevated levels of cortisol, which is a stress hormone released into the blood by the neuroendocrine system during times of stress
High levels of cortisol are a risk factor for future depression, and cortisol activates activity in the amygdala while deactivating activity in the prefrontal cortex
diathesis-stress model and major depressive disorders
proposes that depression is triggered by a cognitive vulnerability (negative and maladaptive thinking) and by precipitating stressful life events
Stressful life events can trigger depression, especially exit events (instances in which an important person departs, such as death, divorce, etc.)
Exit events are especially likely to trigger depression if these happenings occur in a way that humiliates or devalues the individual
People who are exposed to traumatic stress during childhood are at a heightened risk of developing depression at any point in their lives
Which predispositions could cause depression?
An alteration in a specific gene that regulates serotonin (5-HTTLPR gene) might be one culprit
If a person experienced a stressful life event and carried one or two short versions of this gene, instead of the two long versions, then they were more likely to be depressed
However, if the person didn't experience a stressful life event, and had one or two short versions of the gene, then they were unlikely to experience episodes of depression
People experiencing chronic depression in adulthood suggests a much higher incidence in individuals with a short version of the gene in combination with childhood maltreatment
Aaron Beck’s cognitive theory
depression-prone people possess depressive schemas, or mental predispositions, to think about most things in a negative way
This dysfunctional style of thinking is maintained by cognitive biases, or error in how we process information about ourselves, which lead us to focus on negative aspects of experiences, interpret things negatively, and block positive memories
Ex: a person whose depressive schema consists of a time of rejection might be overly attentive to social cues of rejection and he might interpret this cue as a sign of rejection and automatically remember past incidents of rejection
hopelessness theory
postulates that a particular style of negative thinking leads to a sense of hopelessness, which then leads to depression
Hopelessness stems from a tendency to perceive negative life events as having stable ("it's never going to change") and global ("It's going to affect my whole life") causes, in contrast to unstable ("it's fixable") and specific ("It applies only to this particular situation") causes, especially if these negative life events occur in important life realms, such as relationships, academic achievement, and the like
People who exhibit this cognitive style in response to undesirable life events will view such events as having negative implications for their future and self-worth, thereby increasing the likelihood of hopelessness – the primary cause of depression
other cognitive theory
focuses on how people's thoughts about their distressed moods – depressed symptoms in particular – can increase the risk and duration of depression
This theory focuses on rumination, which is the repetitive and passive focus on the fact that one is depressed and dwelling on depressed symptoms, rather than distracting one's self from the symptoms or attempting to address them in an active, problem-solving manner
This theory is used to explain the higher rates of depression in women than in men because women are more likely to ruminate