Roles and Settings for Community Health Nursing Practice
1/15
Earn XP
Description and Tags
Chapter 2
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
16 Terms
Roles in Community Health Nursing
Clinician
Educator
Advocate
Manager
Collaborator
Leadership
Researcher
Role: Clinician
Care Provider:
Home health
Urgent care
Health department
And others
Focus on holism, health promotion, and prevention while using expanded skills.
The nurse ensures health services are provided not just to individuals and families but also to groups and populations.
Role: Educator
Health teacher
Plan for community-wide impact
Community clients are usually not acutely ill and can absorb and act on health information.
Example: a class of expectant parents, unhampered by significant health problems, can grasp the relationship of diet to fetal development
A wider audience can be reached with an emphasis on population and aggregates:
Instead of limiting teaching to one-on-one or small groups, the nurse has the
opportunity and mandate to develop educational programs based on community needs that seek a community-wide impact.
Role: Advocate
Pleader of the client’s cause or actor on behalf of the client.
Support the client’s self-determination and independence.
Make the system responsive and relevant to the client’s needs.
Advocates Must:
Be assertive
Take risks
Communicate and negotiate well
Identify and obtain resources for the client.
Role: Manager
Administrative direction of goals: plan, organize, lead, control, and evaluate.
The nurse helps achieve clients’ goals by assessing their needs, planning and organizing to meet those needs, directing and leading to achieve results, and controlling and evaluating the progress to ensure goals are met.
Participative approach with community.
The nurse serves as this role when overseeing client care as a case manager, supervising ancillary staff, managing caseloads, running clinics, or conducting community health needs assessment projects.
Role: Collaborator
Working jointly with others in a common endeavor, cooperating as partners.
Successful community/public health practice depends on this multidisciplinary collegiality and leadership.
Role: Leadership
Implement innovative change that transforms the lives of residents on a large scale.
Seek to initiate changes that positively affect people's health.
Seek to influence people to think and behave differently about their health and the factors contributing to it.
Role: Researcher
Systematic investigation, collection, and analysis of data for solving problems.
Evidence-based findings to community settings.
This role helps to determine needs, evaluate effectiveness of care, and develop a theoretic basis for community/public health nursing practice.
Settings of Community Health Nursing
Homes
Ambulatory service
Schools
Occupational health
Residential Institutions
Faith Communities
Community at large (domestic and international)
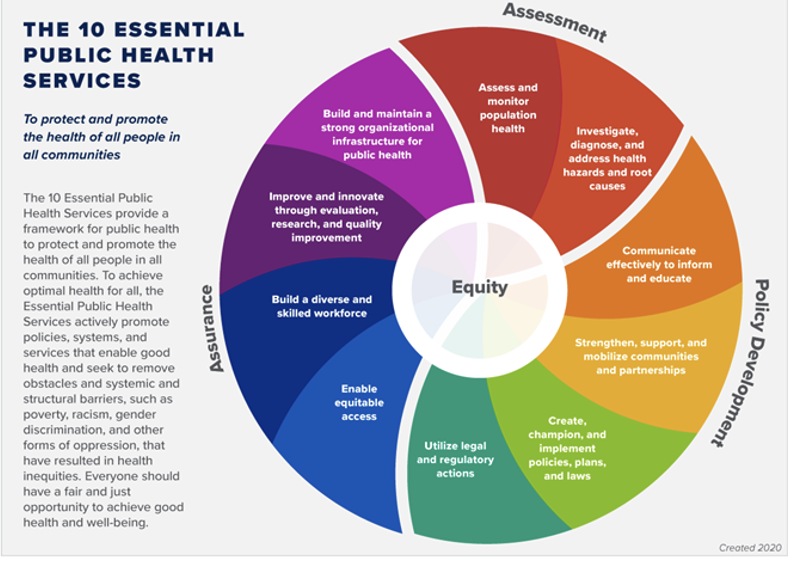
Public Health Core Functions (picture)
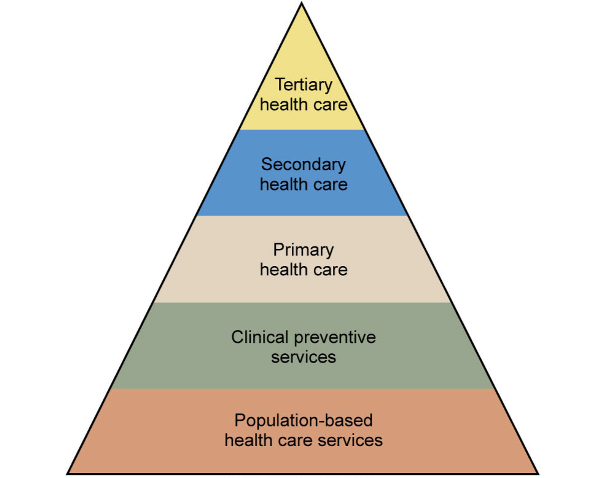
Core Public Health Functions—10 Essential Public Health Services
Assessment:
Regular collection, analysis, and sharing of information about health conditions, risks, and resources in a community.
Systematic collection, assembly, analysis, and dissemination of information about the health of a community.
Ex: Windshield surveys; assessment of communities and families
Assess and monitor population health.
Investigate, diagnose, and address health hazards, and root causes.
Policy Development:
Use of assessment data to develop policy and direct resources toward those policies.
Is enhanced by the synthesis and analysis of information obtained during assessment to create comprehensive public health policy.
Ex: Developing a clean air ordinance
Communicate effectively to informal and educate.
Strengthen, support, and mobilize communities and partnerships.
Create, champion, and implement policies, plans and laws.
Utilize legal and regulatory actions.
Assurance:
Availability of necessary services throughout the community.
Is the pledge to our constituents that services necessary to achieve agreed-upon goals are provided by encouraging the actions of others (public or private) or requiring action through regulation or provision of direct services.
Ex: Access to vaccines.
Build and maintain a strong organizational infrastructure of public health.
Improve and innovate through evaluation, research, and quality improvement.
Build a diverse and skilled workforce.
Enable equitable access.
Social Determinants of Health (SDOH)
Are the circumstances in which people are born, grow up, live, work, and age, as well as the systems, put in place to deal with illness.
These circumstances are shaped by a wider set of forces including economics, social policies, education, and politics.
Factors that influence an individuals’ health include safe housing; clean water, food, and air; safe work places, equitable social interactions; and adequate community resources.
Create social and physical environments that promote good health for all:
Economic Stability: Poverty, employment status, food security, housing.
Education: High school diploma, college, language and literacy, early childhood education.
Social and Community Context: Social cohesion, civic participation, perceptions of discrimination and equity, incarceration, institutionalization.
Health and Health Care: Access to health care, access to primary care, health literacy.
Neighborhood and Built Environment: Access to healthy foods, quality of housing crude and violence, environmental conditions.
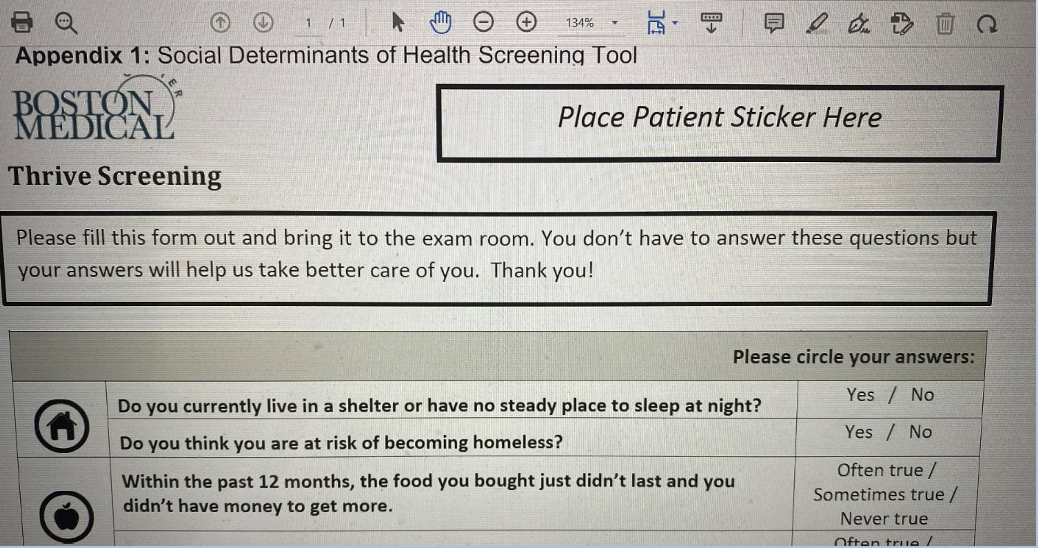
What screening tool is used for SDOH issues?
Boston THRIVE Tool
Health Disparities
Differences among populations as it relates to…
Quality of disease
Burden of disease
Age and rate of mortality due to disease
Health behaviors and outcomes
Other health disparities
Can be viewed as a disproportionate burden of morbidity, disability, and mortality found in specific portions of the population in contrast to another.
Example: Poor access to care, discrimination, language barriers, and non-confident providers.
Access to Healthcare—What can affect a client/community’s healthcare outcomes?
Lack of health insurance
Problem with transportation
No choices for healthcare close by
Lack of healthcare providers
Chapter 2 (book) Summary
The various roles and settings for practice hinge on the three primary functions of public health—assessment, policy development, and assurance—and are applied at three levels of service: individual, family, and community.
Assessment is the systematic collection, assembly, analysis, and dissemination of information about the health of a community.
Policy development involves convening and facilitating community groups to evaluate health concerns and develop a plan to address those concerns. This includes recommending new programs or expanded services based on identified needs, and developing standards for individual client care.
Assurance is the commitment to provide necessary services to clients in order to achieve agreed-upon goals. This is done by encouraging or requiring action—either through regulation or by providing direct services—by public or private entities.
The 10 essential public health services fall within these three core functions and represent the scope of work performed by community/public health nurses (C/PHNs) and other public health professionals.
Community/public health nursing (C/PHN) practice is defined by specific standards of practice developed by organizations such as the AACN, ANA, and the CPHNO (formerly the Quad Council of Public Health Nursing Organizations). These standards are outlined in publications related to ethics, scope of practice, and core competencies.
C/PHNs take on many roles, including:
Clinician
Educator
Advocate
Manager
Collaborator
Leader
Researcher
C/PHNs may work in a variety of settings, which can be grouped into seven major categories:
Homes
Ambulatory service settings
Occupational health settings
Residential institutions
Faith communities
Schools
The community at large
Community/public health nursing is not limited to a specific location. It is a specialty of nursing defined by the nature of its practice—population health—rather than the site of practice.