BRS- Glucose Homeostatis
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
23 Terms
What type of structure is the pancreas gland?
retroperitoneal structure(if they have peritoneum on their anterior side only)
Function of exocrine acinar cells
release enzymes for digestion of food
What is the key hormone involved in the Incretin effect?
Glucagon like peptide-1 (GLP-1)
What is the insulin receptor made?
-2 alpha subunits-interact with the insulin molecules
-2 beta subunits-membrane bound
-joined together by disulphide bonds
How does the insulin receptor work?
1.insulin released by the beta cells
2.binds to the extracellular domain of the insulin receptor-A chains
3.change in formation of tyrosine kinase domains within the beta subunits.
-allows insulin to mediate its effects.
-Autophosphorylation occurs, activates the receptor to phosphorylate intracellular target proteins.
Why does insulin have to bind to the extracellular domain?
-insulin is a very large polypeptide.
-so does not have the ability to cross cell membrane.
Importance of glucose
-energy substrate
-for CNS
-prevent unconsciousness and coma
How is glucose regulated?
-insulin: to decrease the glucose levels
-glucagon, Cortisol, GH and Catecholamines- to increase glucose levels
Hypoglycemia
-<4-5mmol/L, cerebral function is increasingly impaired.
-Blood glucose concentrations <2mmol/L results in unconsciousness, coma and ultimately death can result.
Function of islets of langarhans
involved in glucose homeostasis
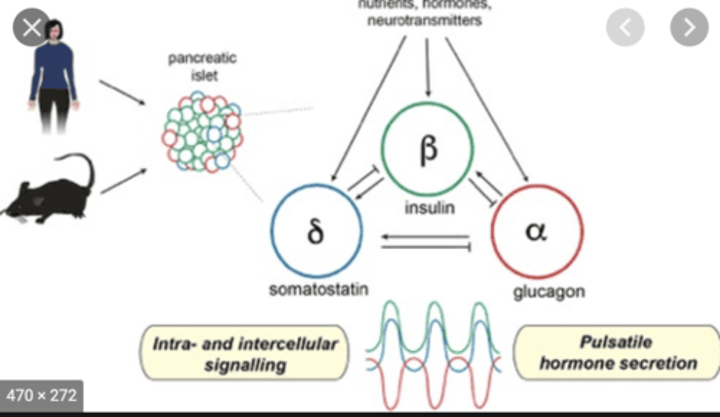
Describe the islets of Langerhans
-made of:
1. alpha cells-glucagon
2.beta cells-insulin
3.gamma cells-somatostatin
-have paracrine effects- allow communication between cells
Describe the type of junctions between the different cells of the I of L
1.gap junctions- allow small molecules to pass directly between cells
2.tight junctions- create small intercellular spaces
Functions of the different hormones
-insulin- decreases blood glucose and stimulates growth and development.
-glucagon-increases blood glucose
-somatostatin-inhibits insulin and glucagon production
Reaction to increased blood glucose
1.stimulation of beta cells by glucose, certain amino acids and certain GI hormones
2.they produce insulin
3.this leads to decrease in blood glucose levels
4.also inhibition of alpha cells to produce glucagon and stimulation of gamma cells to produce somatostatin
Functions of Insulin
1.build up of glycogen stores(glycogenesis)
2.breakdown of glucose(glycolysis)
3.uptake of glucose via GLUT4
4.increases protein synthesis
5.reduces fat breakdown and increases fat build up.
Reaction to decreased blood glucose
1.stimulation of alpha cells by decrease in blood glucose, certain amino acids, some GI hormones, SNS and PNS activity.
2.leads to the release of glucagon
3.this leads to an increase in blood glucose concentration.
4.also inhibition of beta cells to produce insulin and stimulation of gamma cells to produce somatostatin.
Functions of Glucagon
1.increases blood glucose concentration(bcg)
2.increases breakdown of fat therefore increase bcg.
3.increases amino acid uptake into liver which helps with the breakdown of glycogen reserves.
4.breakdown glycogen stores in the liver- clinical application:
-used for patients with T1 diabetes with severe hypoglycaemic episode.
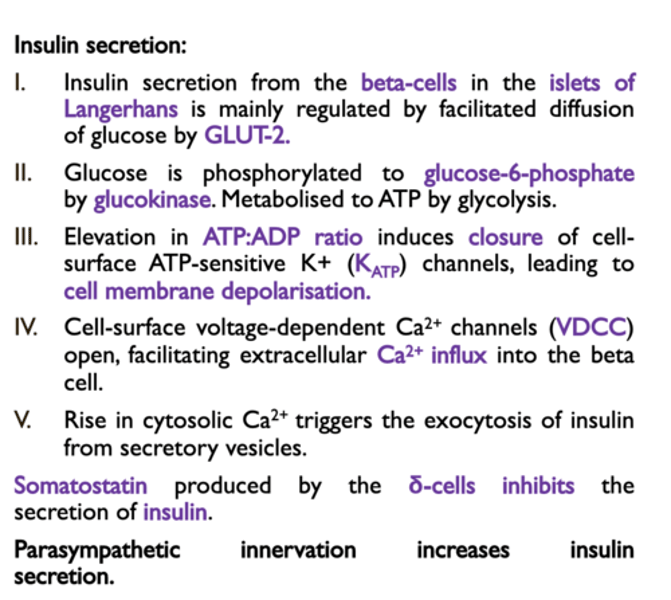
Mechanism of insulin secretion in Beta cells
1.glucose enters beta cells by GLUT2 transporters(these are not insulin dependent unlike GLUT4)
2.glucose is metabolised into glucose-6-p by glucokinase(hexakinase 4)
3.this is a rate limiting step; main glucose sensor
4.glucose-6-p converted into ATP
5.ATP blocks channels at the cell surface membrane
6.this leads to secretion of potassium
7.this stimulates calcium ion voltage gated channels
8.calcium enters cells
9.leading to release of stored insulin and synthesis of new insulin.
How is insulin stored in the cell?
1.stored as proinsulin
2.which is a polypeptide(53 amino acids)
3.when it is released, it undergoes proteolytic cleavage
4.which produces C-peptide and 2 chains of insulin which are bound together by disulphide bonds.
Advantage of the release of C-peptide
-acts as a surrogate marker for insulin assessment as they are released in equimolar amounts
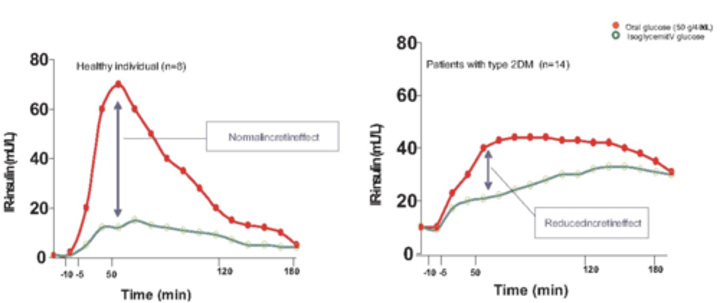
What is the incretin effect?
-Defined as the increased stimulation of insulin secretion elicited by oral as compared with intravenous administration of glucose under similar plasma glucose levels.
-Patients with type 2 diabetes have been demonstrated to exhibit a total loss of incretin effect.
Mechanism of GLP-1
1.gut hormones
2.secreted in response to nutrients in the gut
3.secreted from L-cells in stomach
4.stimulates insulin release from Beta cells.
5.inhibits the glucagon release from Alpha cells.
6.effect on appetite- promotes satiety(fullness)
7.short half life- DPPG-4(dipeptidyl peptidase-4) degrades the hormone
8.this hormone is low in people with T2 diabetes
9.so this can be administered into those patients therefore benefits them as helps with satiety(help with weight loss)and increased insulin secretion.
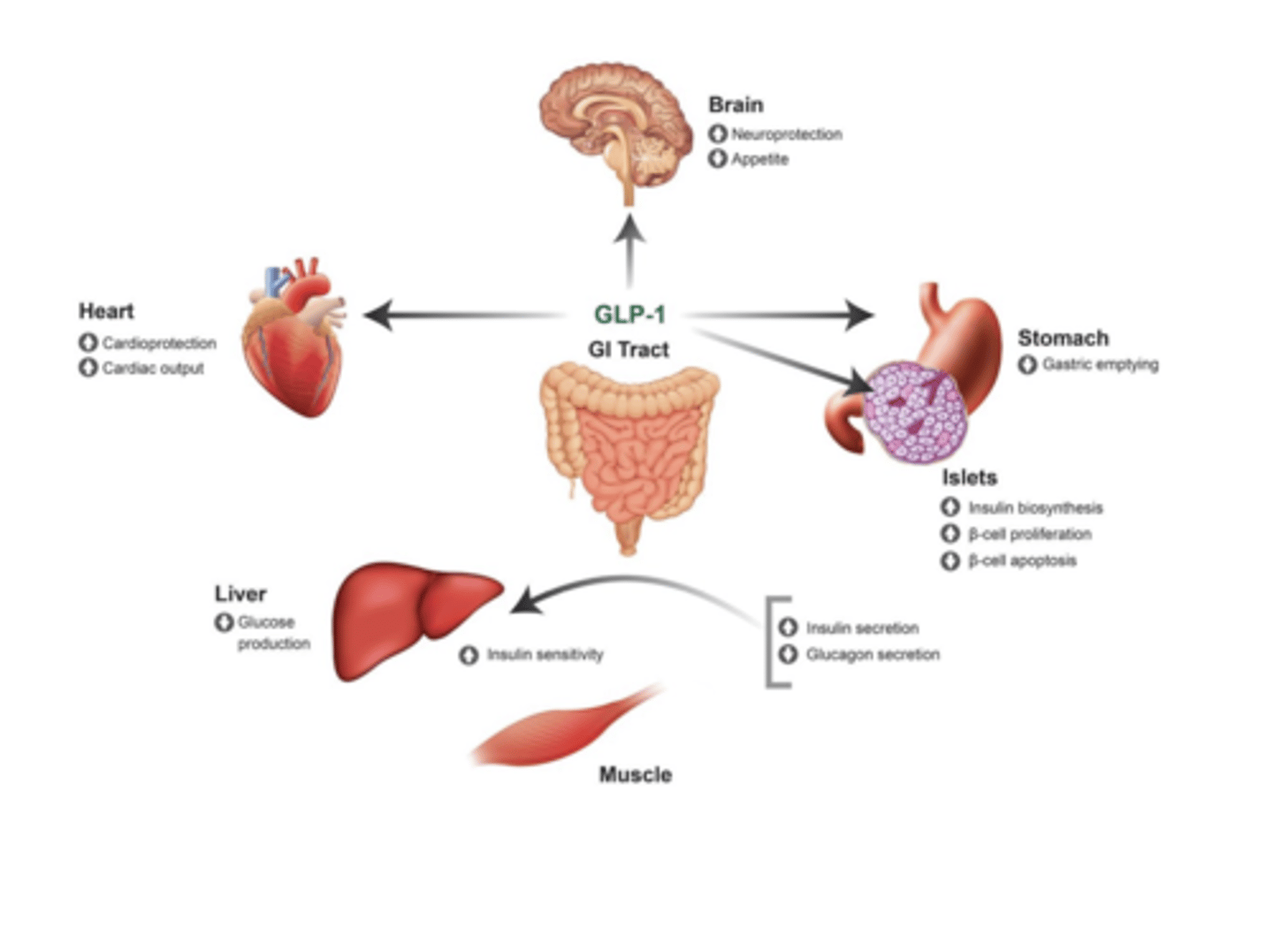
How can you treat Diabetes mellitus?
Administer injections of GLP-1 to individuals to promote insulin secretion, in addition to promote satiety, therefore regulating the control of glucose levels.