The Nephron-Structural & Functional Considerations
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
The number of nephrons varies from ______ to _____ but there is NO ____-______ variation in numbers.
species, species, intra-species
Where are the renal corpuscles located in the kidney?
Cortex of the kidney
Although there is no intra-species variation in the number of nephrons, there may be differences in the _____ _____ which may be _____ in larger breeds.
renal corpuscles, larger
The outer surface of the kidney is covered by a fibrous capsule which can prevent…
Swelling, any swelling can damage the renal corpuscles and cause necrosis
Can additional nephrons develop once the kidney is full developed?
Can damaged nephrons regenerate?
NO
Yes, a degree of regeneration may be possible but will never fully replace the damaged nephrons
What is the functional unit of the kidney and what is it responsible for?
Nephron - responsible for filtering blood through microcirculation
What does the renal corpuscle contain?
The glomerulus and Bowman’s capsule
Where is the bowman’s capsule located?
Closely surrounds the first capillary bed, which originates from the afferent arteriole of the interlobular artery.
Forms a specialised relationship with the glomerulus, where blood filtration occurs.
Essentially a blind ending initial part of nephron.
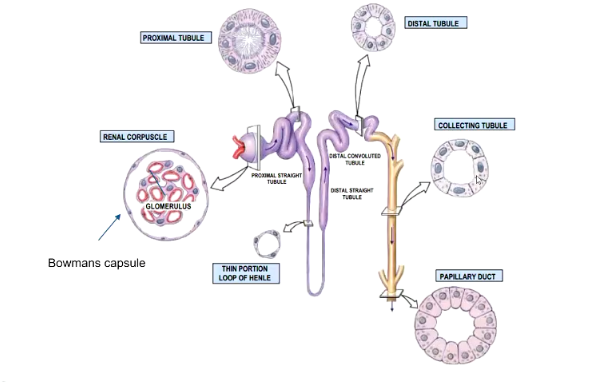
Describe the filtrate pathway.
Filtrate passes from Bowman's capsule into proximal convoluted tubule.
Immediate modifications of the filtrate occurs here, filtering out valuable substances.
Filtrate then passes into the loop of Henle, which ascends towards the corticomedullary junction (where the arcuate blood vessels are located). The loop continues as the distal convoluted tubule, where further modification of the filtrate occurs.
The remaining filtrate passes into the collecting duct for final modification, mainly concentrating the urine.
Outline the location of the nephron within the kidney.
- Cortex: Most of the microcirculation (Glomerulus) and a large component of the nephron are located in the cortical region around the CM junction.
- Medulla: Contains the loop of Henle, associated blood vessels (vasa recta)
Is the collecting duct considered part of the nephron?
Not necessarily, but is closely associated
Due to different embryological orgin
Describe…
Location
Features
Function
Blood Flow
Of cortical nephrons.
Location:
Located primarily in the outer cortex of the kidney
Features:
Have a shorter loop of Henle that extends only into the outer region of the medulla (in humans they are completely contained within the cortex)
Function:
Responsible for bulk of filtration and reabsorption processes, playing a major role in excretion and regulation
Blood Flow:
Peritubular capillary network surround PCT and DCT (in the cortex) role in tubular reabsorption and secretion
Describe…
Location
Features
Function
Blood Flow
Of juxtamedullary nephrons.
Location:
Located near CM junction
Function:
Longer loop of Henle extends deep into the inner medulla
Feature:
Crucial for concentrating urine, essential for water conservation
Blood Flow:
Vasa recta: A peritubular network running parallel to loop of Henle, helping maintain concentration gradient in medulla.
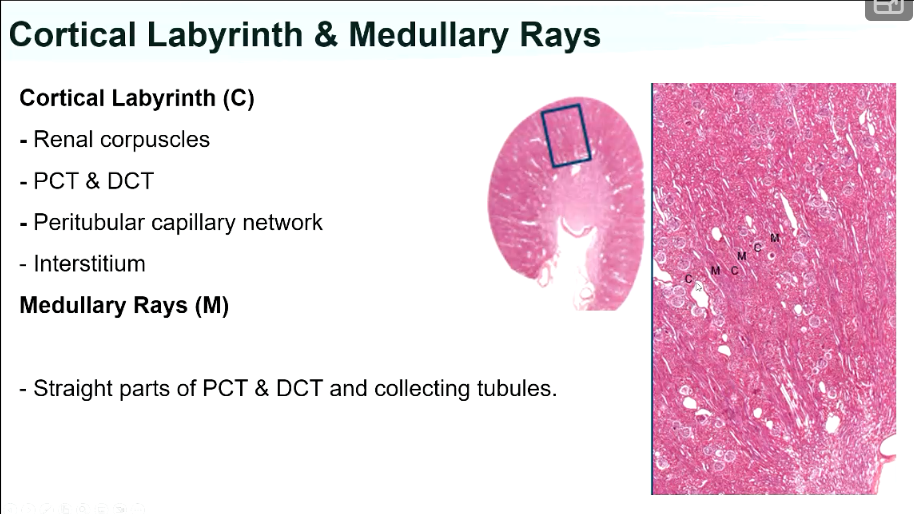
Describe what components of the nephron are located within the Cortex.
Cortex:
Presence of renal corpuscles and the cortical labyrinth surrounding them
The cortical labyrinth includes sections of the proximal and distal tubule, evidence of blood vascular system, and peritubular network surrounding some tubular structures of the nephron.
Also contains the interstitium corresponds to the connective tissue surrounding these structures, providing a supportive framework.
Describe what components of the nephron is associated with the Medullary Ray.
Despite its name, it is associated with the cortex.
Refers to the arrangement of structures (corpuscles, PCT & DCT and blood vessels) in recognisable blocks within the cortical area
Describe what components of the nephron are associated with the medulla.
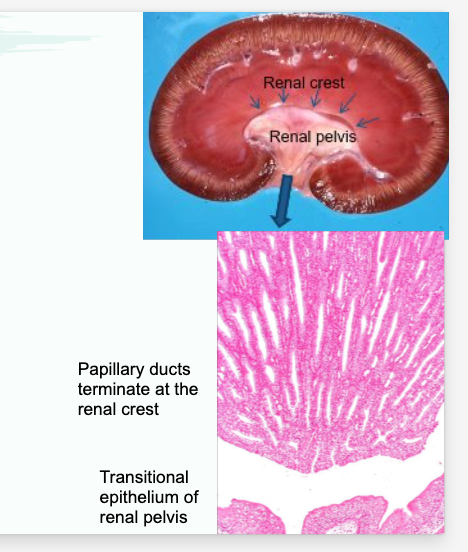
- Contains the loop of Henle, vasa recta and collecting ducts.
Papillary duct: Refers to the larger parts of the collecting duct system. These ducts start as small structures that unite from different areas of cortex, then extend into the medulla and become larger.
Where does the urine collect from the bottom of the medulla?
At the bottom edge of the medulla, urine drips out of this tissue and is collected by the origins of the ureter. This part of the collecting ducts is sometimes referred to as the papillary ducts or ducts of Bellini.
Describe the following structures:
(C)
(M)
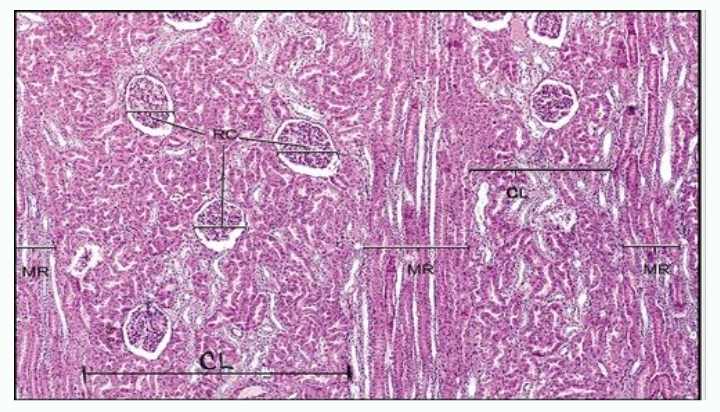
(C)
The structures labelled C (though difficult to see) are part of the cortical labyrinth. The cauliflower-like clusters in this area are the renal corpuscles.
(M)
The structures labelled M are the medullary rays which consist of straight parts of the PCT and DCT and origins of the collecting ducts.
Identify the following features in the image.
CL
MR
RC
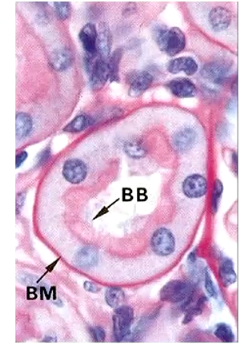
Describe the epithelium of bowman’s capsule.
Bowman’s capsule lined with simple squamous epithelium
Neck of balloon (PCT) is lined with cuboidal epithelium, as shown in diagram. This distinction is important for understanding the function of these structures.
Describe the two poles of the renal corpuscle.
Vascular pole: The origin of the glomerulus where blood vascular system is located. (Afferent + Efferent arterioles)
Urinary pole: The area where the filtrate flows out. (Neck of renal corpuscle)
What makes up the filtration barrier of the renal corpuscle?
Filtration barrier:
Components involved are the capillary wall surface and the visceral layer of Bowman’s capsule, which are tightly apposed.
Visceral layer of the BC, then there is a space (urinary space) where filtrate will start to fill. The outer surface of balloon (BC) would be the parietal layer.
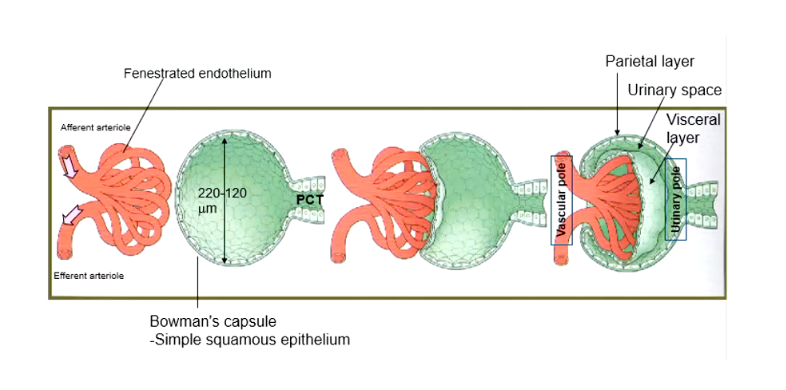
Describe the parietal layer of Bowman’s capsule.
The outermost part of the Bowman’s capsule is composed of simple squamous epithelium. This layer transitions to cover the glomerular capillaries, forming the visceral layer.
Describe the visceral layer of Bowman’s capsule.
Layer of capsule in direct contact with walls of glomerulus
Made up of specialised cells called podocytes (yellow structure).
Podocytes extend tentacle-like arms, known as pedicels or foot processes, which cover the glomerular capillaries.
These projections interdigitate, forming filtration slits with small gaps, creating a sieve-like structure
The thin membrane covering these spaces is called the slit diaphragm.
Describe how plasma filters through the bowman’s capsule, specifically the visceral layer of the capsule.
Also note the function of the glomerular basement membrane in the filtration process.
Around 20% of plasma filters through these sieve-like tentacles into the urinary space of Bowman’s capsule and is funnelled to the PCT.
The fenestrations (small holes) in the endothelium of the glomerular capillaries (shown in left image – layer with red dots) align with the spaces between the podocyte pedicels, allowing small molecules to pass through.
The shared basement membrane (pink sponge-like structure) separates the capillary lumen from the lumen of Bowman’s capsule and is referred to as the glomerular basement membrane. It has been modified to facilitate filtration of certain substances.
What layers compose the filtration barrier?
Endothelial cells of the capillary, glomerular basement membrane and podocyte of the visceral layer of bowman’s capsule
Describe the filtration pathway through bowman’s capsule and the glomerulus.
Filtration Pathway:
Filtration slits between the pedicles allow for faster filtration than if substances had to pass through entire cells. Most substances will pass through these slits.
For substances to filter from inside to outside, they must:
Either pass through endothelial holes or through the cells.
Traverse the glomerular basement membrane.
Finally, they can either pass through the podocyte cell wall or slip between the podocytes and through the thin membrane where the podocyte is not in direct contact. (Slit diaphragm)
How much blood plasma filters through the BC over 24 hours?
100-200L
Describe the cell types in the following diagram.
Yellow Wall
Blue Cells
Pink Line
Orange Cells
Light Green
Yellow wall: Outer wall of Bowman’s capsule (parietal epithelium)
Blue cells: Podocytes of the visceral layer of Bowman’s capsule
Pink line: Glomerular basement membrane (GBM)
Orange cells: Endothelial cells lining the capillary, with a RBC visible inside (showing the capillary walls with fenestrations)
Light Green: Between capillaries, mesangial cells
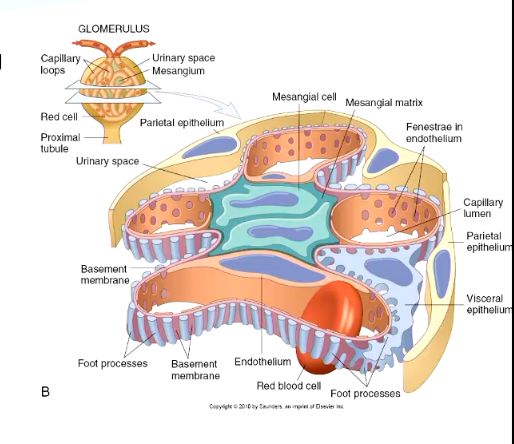
What do the mesangial cells do?
Where are they found?
These cells produce a gel-like matrix that integrates into the glomerular basement membrane, helping to maintain and cleanse the GBM, as it undergoes constant turnover.
Found between the capillaries in BC.
Any debris retained by the filtration barrier is effectively phagocytosed by mesangial cells.
If substances, like large molecules (e.g. proteins) manage to pass through part of the filtration barrier, they can get stuck in the GBM. The mesangial cells help dispose of these substances to keep the barrier clean and functioning properly.
What factors determine whether a substance can pass through the filtration barrier?
- Particle size: Large particles won’t pass through
- Charge: Negatively charged particles tend to be repelled and generally don’t make it into the filtrate.
Filtration results in a removal of ______ waste.
Absorption of up to ___ of glomerular filtrate.
nitrogenous
70%
What are the specialisations of the PCT epithelium intended for reabsorption?
Leaky intercellular junctions
Interdigitations in the cell wall
Lateral interdigitations
Basal interdigitations
Microvillous surface
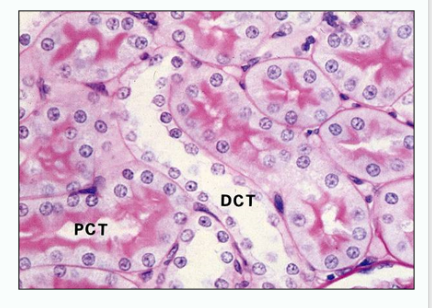
Describe the cell structure of the PCT epithelial layer.
PCT epithelium consists of a single layer of cuboidal epithelium.
These cells contain numerous mitochondria, indicating active transport processes.
Their surface is highly specialised for absorption, with microvilli and interdigitations that significantly increase surface area.
Describe features of the cell junctions and permeability in the PCT.
The cell junctions appear “wobbly”, meaning they are leaky.
This allows substances to pass between cells (paracellular transport), as well as through cells (transcellular transport).
Describe the reabsorption pathway in the PCT.
Once substances pass through or between cells, they move across the basement membrane into the interstitium (light orange area at bottom of image).
The PCT is closely associated with peritubular capillaries, ensuring that reabsorbed substances quickly enter the bloodstream.
This setup allows for efficient and rapid reabsorption of essential nutrients, water and ions back into circulation.
Note some of the notable features in PCT histological sections.
The PCT is lined by cuboidal epithelial cells, but individual cell boundaries are not clearly visible due to the leaky junctions between cells.
The nuclei of these cells are typically basally located (toward the base of the cell)
Microvilli on the luminal surface appear pink and fluffy under PAS staining.
In H&E staining, the lumen of the PCT appears fuzzy and indistinct, making the microvilli harder to distinguish.
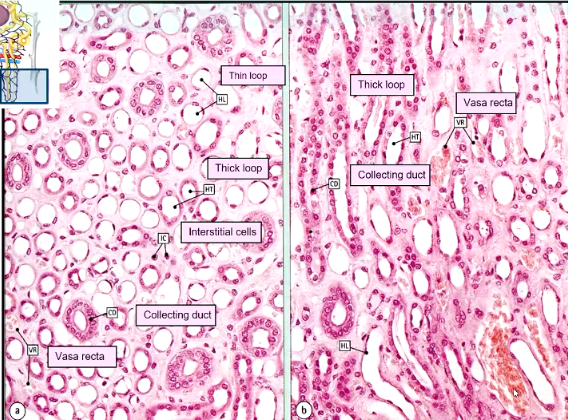
What are the general features and functions of the renal medulla?
Features of renal medulla: Nephron loop & vasa recta
Function: Give rise to counter current multiplier system (creates concentration gradient required for urine concentration).
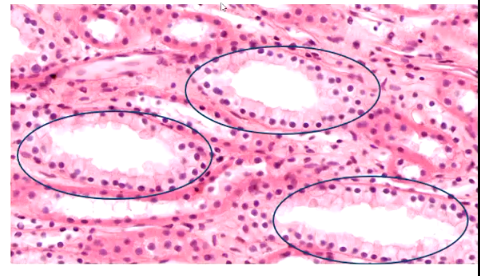
Describe how to identify collecting ducts, loops of henle, blood vessels and thick segments of loop of henle in histology.
Collecting ducts are the easiest to identify, as they have well-defined thickened walls.
Thin loops of Henle appear as small tubules with very thin walls and bulging nuclei.
Thick segments of the loop of Henle serve as an intermediate between these two structures.
Blood vessels can be difficult to distinguish, as they often lack visible blood cells.
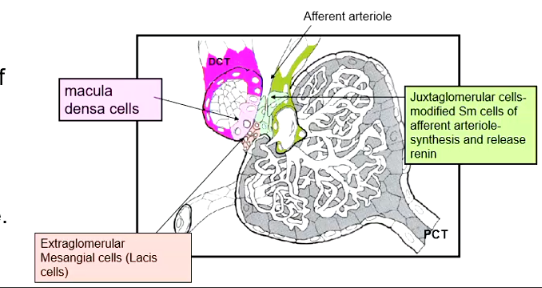
What is the key role of the DCT?
The DCT is primarily involved in secretory processes, but it also plays a crucial role in the regulation of renin production.
The straight part of the DCT loops close to the renal corpuscle and forms…
juxtaglomerular apparatus.
Describe the cell types composing the Juxtaglomerular Apparatus.
Cell Types in this region:
1) Macula Densa Cells (lighter pink cells)
- Found in this specialised area of the DCT.
- Act as osmoregulatory sensors, detecting sodium concentration in the tubule lumen.
- When sodium levels are low, they stimulate juxtaglomerular cells to synthesise and release renin.
2) Extraglomerular Mesangial Cells (Lacis cells – orange coloured).
- Located between the macula densa cells
- Plays a supporting role in the renin release mechanism but do not produce renin themselves.
3) Juxtaglomerular (JG) cells (Green cells)
- Modified smooth muscle cells found in the afferent arteriole.
- Responsible for synthesising, storing, and releasing renin in response to signals from macula densa cells.
Summarize the main function and factors affecting the role of the JGA.
Also summarize the cell roles.
The JGA is a specialised structure that regulates glomerular blood flow based on factors such as:
Hydration status
Blood volume
Ion concentration
It consists of:
Macula densa cells (sodium sensors)
Extraglomerular cells (supporting role)
Juxtaglomerular cells (renin producers)
Describe the histological features of the macula denas.
In histological sections, the macula densa cells can be identified within the DCT, particularly near the vascular pole, where the afferent arteriole enters to form the glomerulus.
Function: Blood pressure regulation via renin-angiotensin aldosterone mechanism
The DCT appears within the yellow-circled area, which has a more open lumen compared to surrounding structures.
A distinct row of tightly packed cells along one side of the DCT represents the macula densa cells.
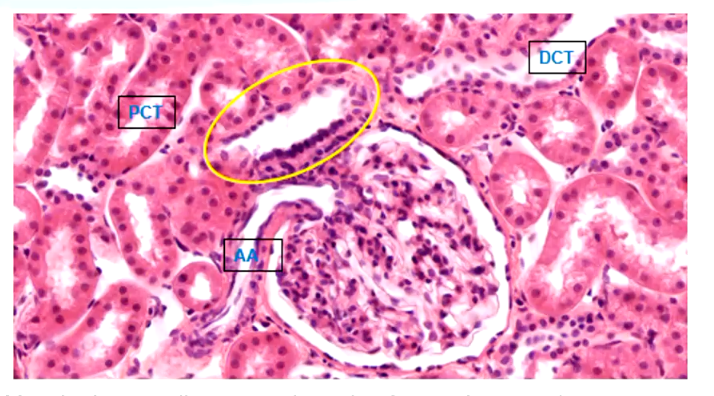
Describe the key differences between the PCT and DCT, regarding key histological features.
The PCT has a fuzzy appearance due to its microvilli, which are easily seen in sections.
The DCT lacks these microvilli, making its lumen appear clearer and more defined.
The DCT has fewer convolutions than the PCT, so fewer DCT sections are visible in a given histological slide.
Key features of DCT:
Cuboidal epithelium appears paler when stained
Lacks brush border, making its lumen sharper and more defined compared to the PCT
Cells are shorter in height, giving the DCT a more open appearance.
Nuclei more apical
Fewer DCT sections are typically seen in histological slides compared to the PCT, due to its less convoluted structure.
Overall, what is the function of the DCT?
- Reabsorption of sodium, chloride, calcium & magnesium (actively)
- Tubular secretion (H+, K+ (aldosterone))
What are the main histological features of the collecting tubules?
- Cells become more columnar, with distinct boundaries between individual cells.
- They appear paler when stained with H&E compared to other structures.
Describe how collecting ducts release urine.
Collecting ducts fuse into papillary ducts, terminating on the renal crest, and release urine into the renal pelvis to be collected and transferred away
Summarize the histological features of the nephron.