Ventilation
1/39
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
40 Terms
where does gas exchange happen
alveoli
where does CO2 in alveoli come from
waste product from cells breaking down CHOs and fats
where does oxygen go from the alveoli
goes into blood to the tissues for oxidative phosphorylation
role of O2 in ETC? then what happens to it?
final electron acceptor in ETC, then is converted to H2O → why expired O2 is less than inspired O2
how does the body move air in and out of the lungs?
respiratory and accessory muscles contract to expand the ribs and increase the pressure gradient between the lungs and the atmosphere
(negative pressure within the lungs to pull air in, positive pressure in the lungs to push air out)
how to the ATP demands of breathing change with exercise
breathing more forcefully and at a higher rate requires more ATP to accommodate the increased work load of the respiratory muscles
how do increased ATP demands in the muscle affect breathing?
high ATP demands mean high energy transfer rates, which means a high production of CO2 needing to be expired and more O2 needing to be consumed in order to generate energy
does breathing impact exercise performance
yes, because there is an ATP cost to breathing and because ventilation is highly linked to metabolism
how to calculate how much air one breathes in one minute
VE =fb x VT
Volume expired = breathing frequency x tidal volume
average tidal volume (VT)
500mL
Average breaths per minute (fb)
12bpm
Concentration of oxygen in atmosphere
20.93%
concentration of carbon dioxide in the atmosphere
0.03%
how to calculate partial pressure
concentration of gas (%) x total pressure
pressure of 1 standard atmosphere (1 atm)
760mmHg
consequences to ventilation at high altitude
altitude means atmospheric pressure has dropped to about 220mmHg
therefore, even though the concentration of O2 is still the same as it was at sea level, its partial pressure (PO2) is very low
this means we inhale much less O2 and need to work harder to get the same amount of air and oxygen in, but its super easy to push CO2 out
have to create super negative pressure in lungs to create a gradient high enough to inhale
what does RER stand for
respiratory exchange ratio
how to calculate RER
VO2/VCO2
open-circuit spirometry
measures oxygen uptake and CO2 production to infer energy expenditure
subject inhales ambient (room) air
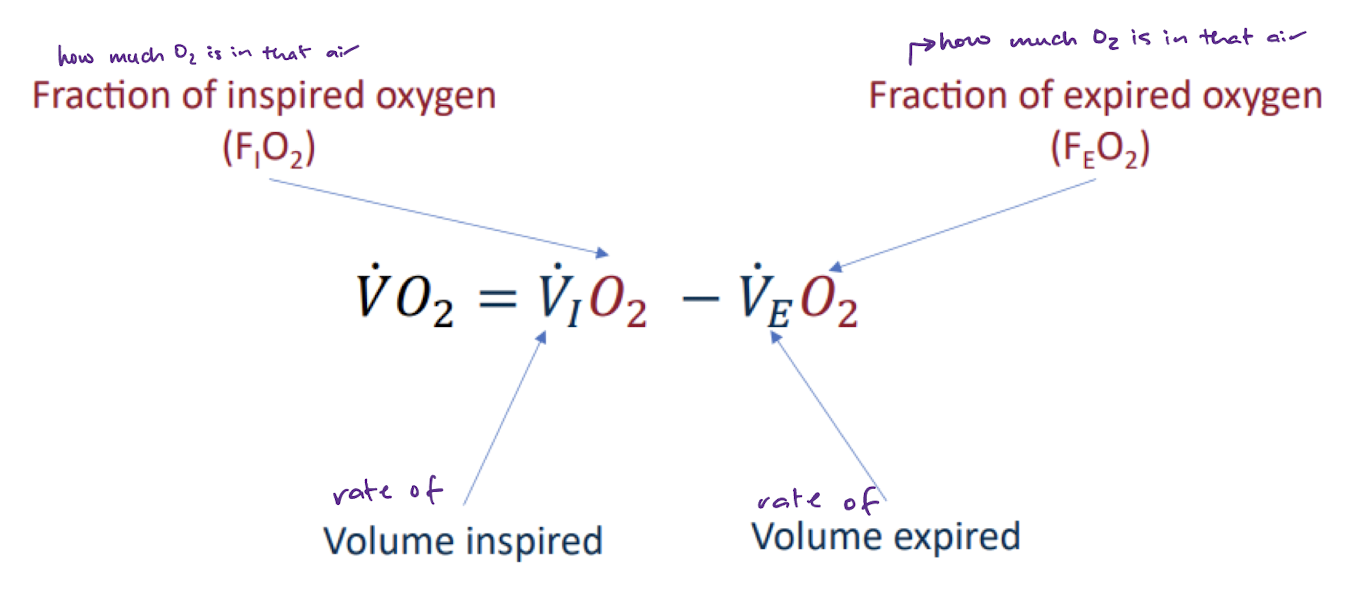
equation used in open-circuit spirometry
hyperventilation
increase in ventilation that is more than what is needed by metabolism to get the O2 in and the CO2 out
dyspnea
subjective SOB, seen with asthma, COPD
at a high pressure differential between two places, how does gas move
via diffusion, gas moves very quickly from high pressure to low pressure
at a halfway point to reaching equilibrium, how does gas move between two places
via diffusion, high rate of gas moving from high to low pressure, with some gas moving slowly from low to high pressure
gas movement at equilibrium between two places
via diffusion, gas moves equally in and out of each place
which is able to diffuse faster, O2 or CO2
CO2 because it is more soluble
how long does blood spend in the pulmonary capillary at rest?
about 0.75s
how long does blood spend in the pulmonary capillary at maximal exercise?
about 0.4s
factors that impair fas transfer capacity at the alveolar-capillary membrane
what impact do these have on gas equilibrium?
buildup of a pollutant layer that thickens the alveolar membrane → slows diffusion
reduction in alveolar surface area
these factors make it take longer to reach alveolar-capillary gas equilibrium
why does the blood spend less time in the pulmonary capillaries when exercising compared to at rest?
is this a problem?
because of the increased speed of blood flow
in a healthy person, there is still enough time for gas exchange to occur. but if they have a compromising condition, this will not be enough time and ventilation will be limited
how does increased oxidative phosphorylation alter the partial pressures of O2 and CO2 at different locations in the body
Venous blood leaving muscle
High oxidative metabolic demands mean higher O2 consumption. This results in more O2 turning into H2O, and a lower PO2. PCO2 goes up as the production rate is higher.
Arterial blood
Partial pressures here remain the same because we are able to increase RR to accommodate the higher O2 needs and higher CO2 levels that need to be expired
How does the body maintain homeostasis by minimizing changes in gas partial pressures
The body increases respiratory rate to better inspire O2 and expire CO2. This maintains the partial pressure of arterial blood
What ventilation changes can we measure in the lab with increased exercise intensity
oxygen expired
carbon dioxide expired
VO2
VCO2
RER
substrates being used
when might lungs limit exercise performance
mostly only when the lungs are compromised. otherwise, we are very good at breathing
Hb in blood
15g per 100mL of blood
150g per 1L of blood
amount of O2 in blood
20mL per 100mL of blood
200mL per 1L of blood
why do men have more RBC and Hb than women
testoterone
equation for blood O2 capacity
Hb x HbO2 capacity
how much O2 carried by Hb at full saturation with normal Hb levels
20mL O2 with each 100mL blood
200mL O2 with each L of blood