Chapter 13: Control of Body Movement単語カード | Quizlet
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
56 Terms
Voluntary Movements
Conscious awareness of movement
- Physical awareness
- Purposeful movement
Involuntary movements
No conscious awareness
- unconscious
- automatic
Combination of voluntary and involuntary
- learned actions that become automatic
- reflexes that can be consciously blocked or augmented
- muscle memory
Neural Reflexes: Afferent information
INPUT:
Sensory input
- collect info for a desired movement
- proprioception
INTEGRATION
Processing
- assess input or develop a specific intended movement
- determine necessary action
- motor program
*formulate the neural activity required for the action
Neural Reflexes: Efferent Information
OUTPUT:
Descending pathways
- motor output
- send appropriate signals to appropriate areas
ACTION:
Desired action
- motor neuron pool and associated muscle activation
*motor units
1. Type of efferent control
(autonomic vs. somatic)
2. Location of integration
(spinal vs. cranial)
3. Development of reflex
(innate vs. learned or conditioned)
4. # of neurons in the pathway
(monosynaptic vs. polysynaptic)
How can neural/motor reflexes be categorized?
autonomic controlled reflexes
Visceral reflexes
- occur in organs
- most are unconscious, some are conscious (ex. urination)
- most have tonic activity
Location of integration
- Spinal (can also be influenced by brain)
- Cranial (can modify relfex)
Polysynaptic
monosynaptic
-single synapse between sensory neuron that received and motor neuron responds
-e.g. knee jerk
polysynaptic
-at least 1 interneuron between sensory and motor neuron
-e.g. withdrawl reflex
somatic controlled reflexes
Skeletal muscles - voluntary (doesn't rely solely on sensory coming in)
Location of Integration:
- Cranial
(integration or inhibition - primary motor cortex with influence of other areas)
- Spinal
"reflex action"
(May be influenced by the brain)
- moderate a reflex action
- block a reflex action
Monosynaptic or Polysynaptic
Stimulation vs. Inhibition
- activity at the neuromuscular junction is ALWAYS excitatory
- stimulate myofiber: get a twitch
- stop stimulating myofiber: relax myofiber
- inhibition must occur at the somatic motor neuron
- block development of AP in somatic motor neuron
Muscle receptors
Golgi tendon organs
Joint receptors
What are the three types of proprioceptors (sensory receptors) that are found in skeletal muscle reflex control?
upper motor neurons
motor neurons in the CNS (brain and spinal cord) that control the lower motor neurons in the peripheral nervous system
lower motor neurons
somatic motor neurons that are in the PNS
categorized into:
Alpha motor neurons
Gamma motor neurons
alpha motor neurons
type of lower motor neuron
innervates extrafusal fibers
generates tension/force
gamma motor neurons
type of lower motor neuron
innervates intrafusal fibers
detects muscle stretch
Extrafusal fibers
contractile myofibers
innervated by alpha motor neuron
- flaccid paralysis
- polio
covered by muscle spindles
function: to develop force/contraction
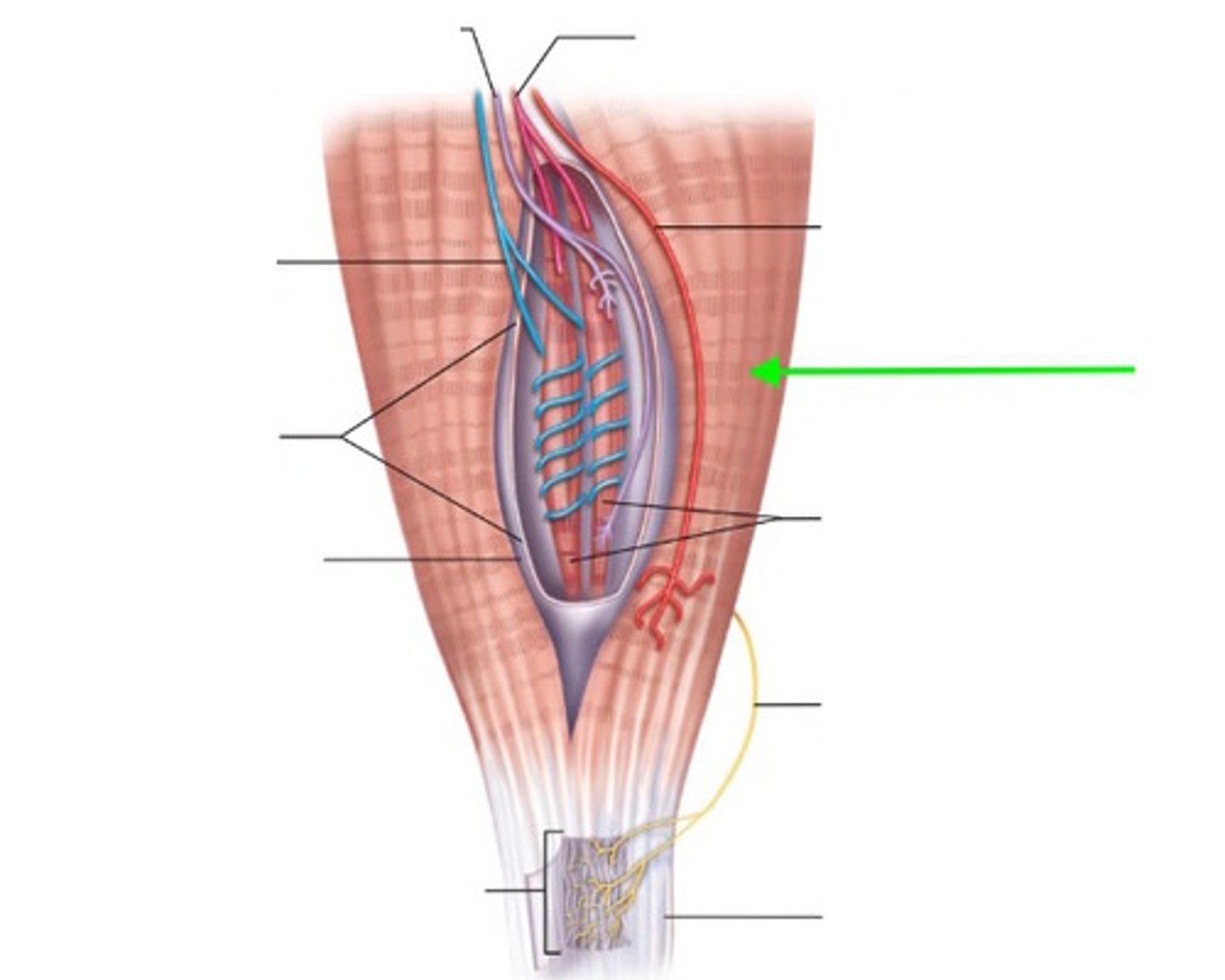
muscle spindles
buried among the extrafusal fibers of the muscles
1. connective tissue capsule
2. intrafusal fibers
- contractile myofiber ends (gamma motor neurons)
3. non-contractile center
- sensory stretch receptors
Intrafusal fibers
contractile myofiber ends
innervated by gamma motor neurons
function: to maintain shape of receptive area in the center
tonic activity at rest
Muscle spindles have what kind of activity? Meaning they are firing even when relaxed.
monosynaptic spinal reflex
Are muscle stretch (muscle-spindle reflexes) a monosynaptic or polysynaptic spinal stretch relfex?
When muscles stretch and strengthen, muscle spindle sensory afferent neurons fire more.
The reflex response is muscle contraction to prevent damage from over-stretching.
Why does a muscle stretch trigger a stretch reflex?
Negative feedback control:
1. stretch signal
(activates alpha motor neuron)
2. Contract extrafusal fibers
(compress receptive area)
3. No more stretch
(return to tonic signal rate)
- turn system off
in more detail:
1. muscle stretch
-> increased afferent signals to spinal cord
-> spinal cord
-> increased efferent signals through alpha motor neurons
2. muscle contracts
How does a muscle stretch trigger a stretch reflex?
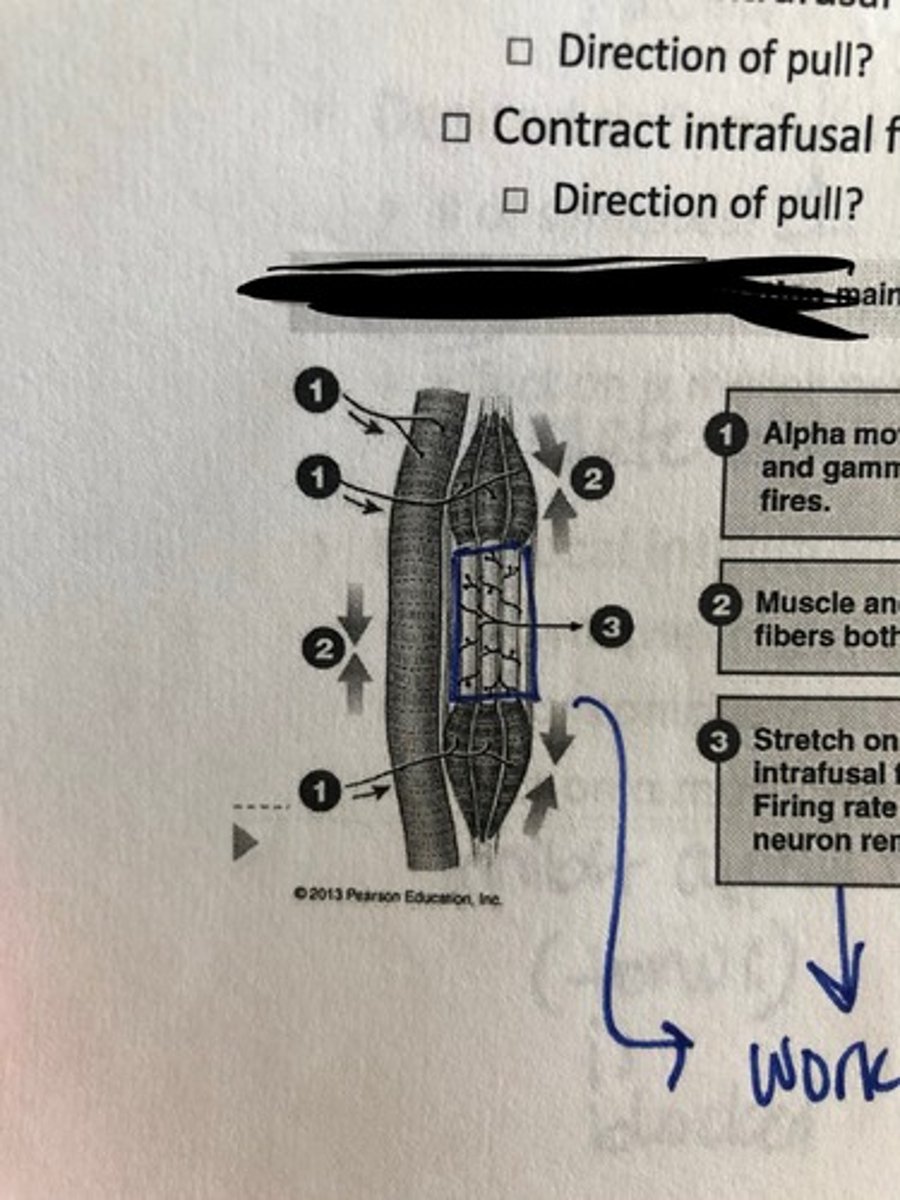
***Without gamma motor neurons, muscle contraction causes the spindle firing rate to decrease.
Alpha motor neuron stimulation w/o stretch receptor activation causes a problem:
- it compresses the stretch receptor area and you lose the ability to detect stretch. (you end up dropping the weight)
Why does the shortening of extrafusal fibers in a muscle stretch become a problem?
(in terms of not having the gamma motor neurons (intrafusal fibers))
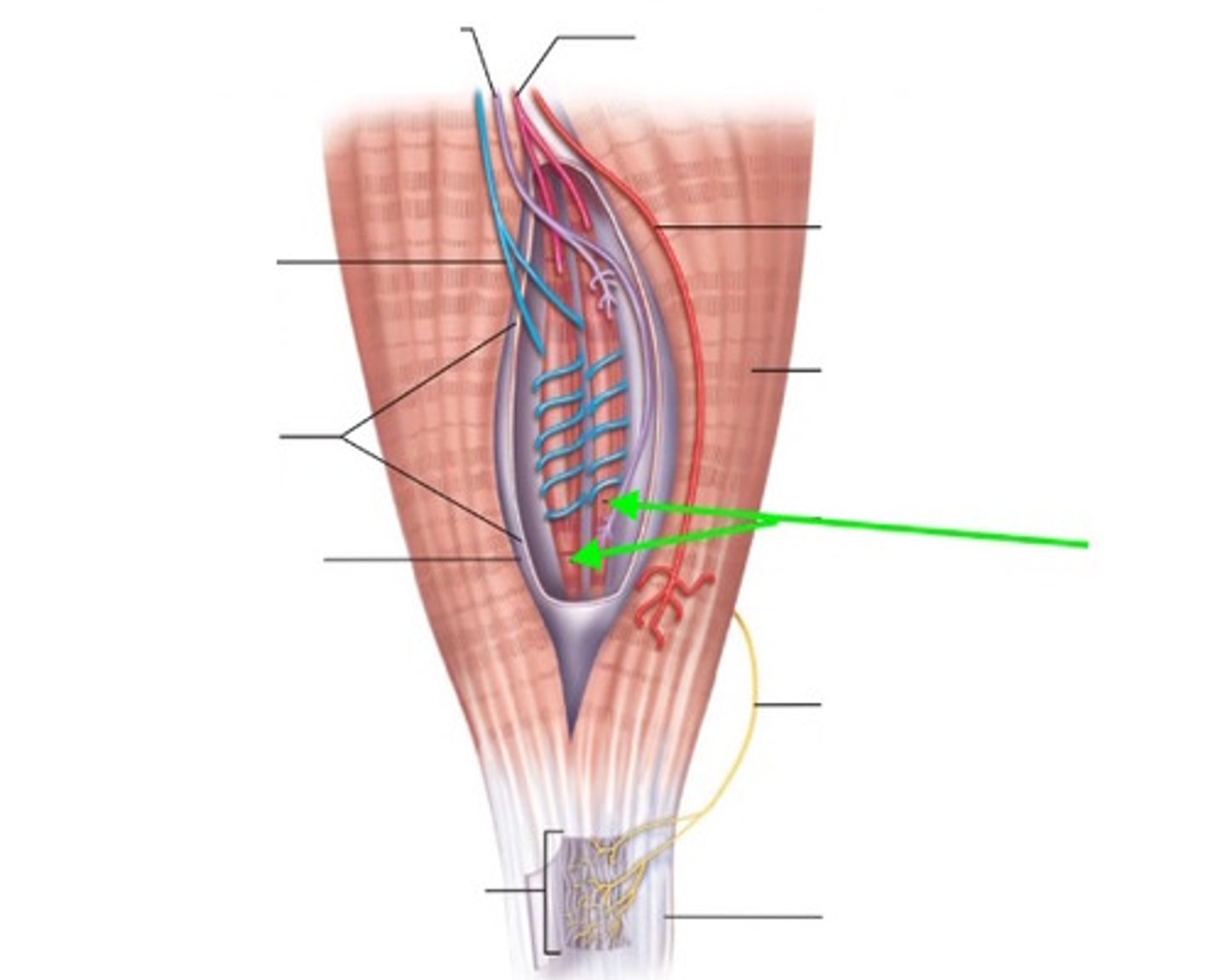
alpha-gamma coactivation
Alpha and Gamma motor neurons both activated
- contraction of extrafusal fibers is to develop force
Direction of pull: towards center
- contraction of intrafusal fibers is to maintain shape of receptive area
Direction of pull: each end of the muscle spindle (the intrafusal fibers are also pulling towards its center.
* works together to keep muscle contracting
Golgi tendon organs
receptors sensitive to tension in tendons
free nerve endings in tendons
***Isometric phase of voluntary muscle contraction
- stretch elastic components of muscle
- increase tension on tendons
- increase firing of golgi tendon receptors to keep muscles from shortening - keep same length. STILL AT REST
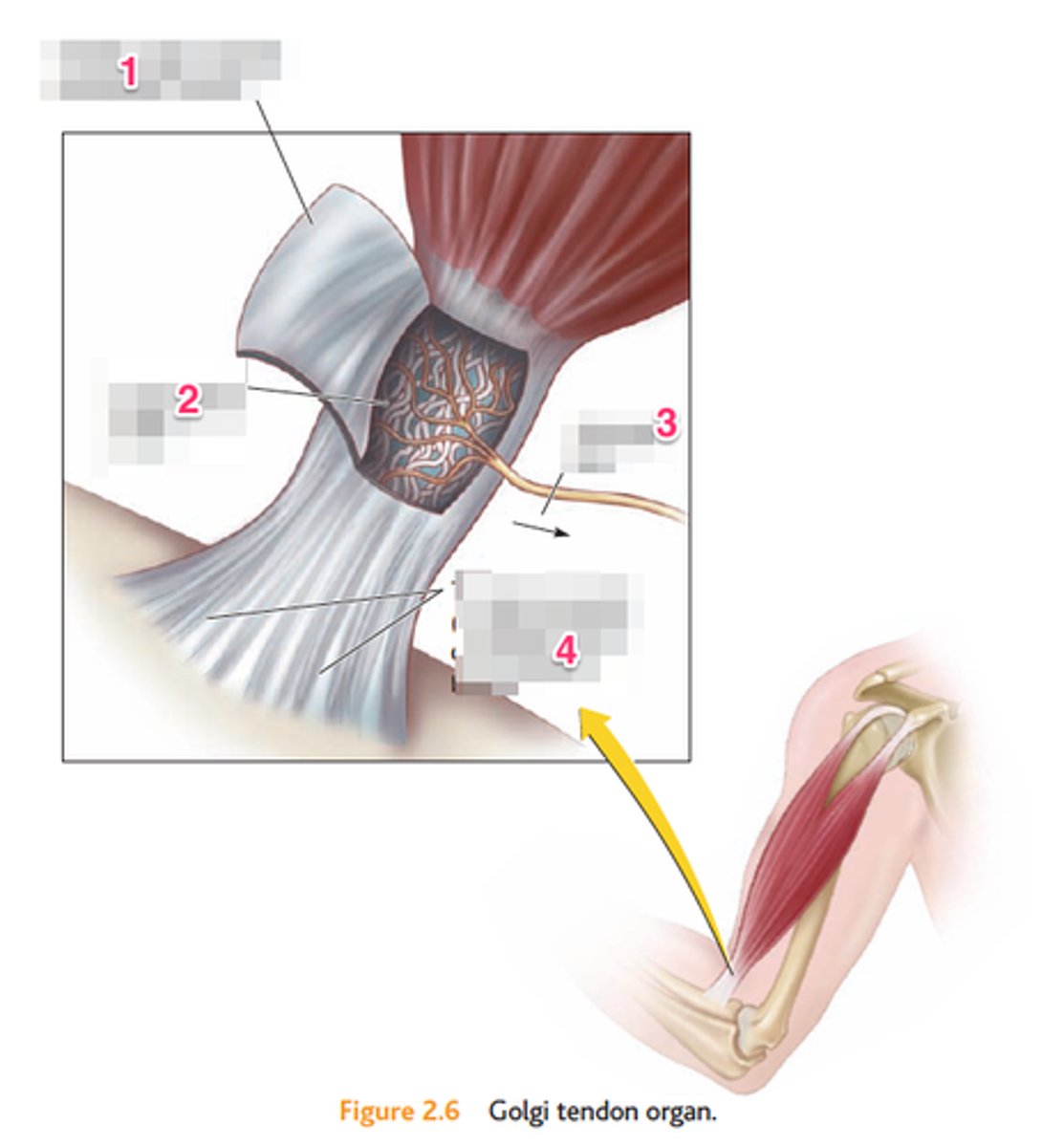
alpha-gamma coactivation:
- maintain appropriate tension
golgi tendon organ:
- increase sensory information to CNS allowing for
*better motor control: posture and movement
Muscle spindles and Golgi tendon organs: why have both?
joint reflexes
Myotatic units
All pathways involved in control of a joint movement:
- reflex components
- agonist & synergists & antagonists
Integration of multiple individual reflexes into a functional response
- desired reflex
- reciprocal inhibition
Monosynaptic vs. poly- or multisynaptic
Ipsilateral vs. contralateral
Patellar tendon or knee jerk (stretch reflex)
Stimulus: tap to tendon - detects stretch in muscle
Receptor: muscle spindle stretch receptors
Desired Action:
- # synapses: monosynaptic
- Ipsi-contra?: ipsilateral
- Effect on alpha motor neuron: excitation, causes it to contract and swing forward
Reciprocal inhibition: antagonist flexor must relax
- # synapses: poly (2)
- Ipsi-contra?:
ipsilateral
- effect on alpha motor neuron: relax hamstring
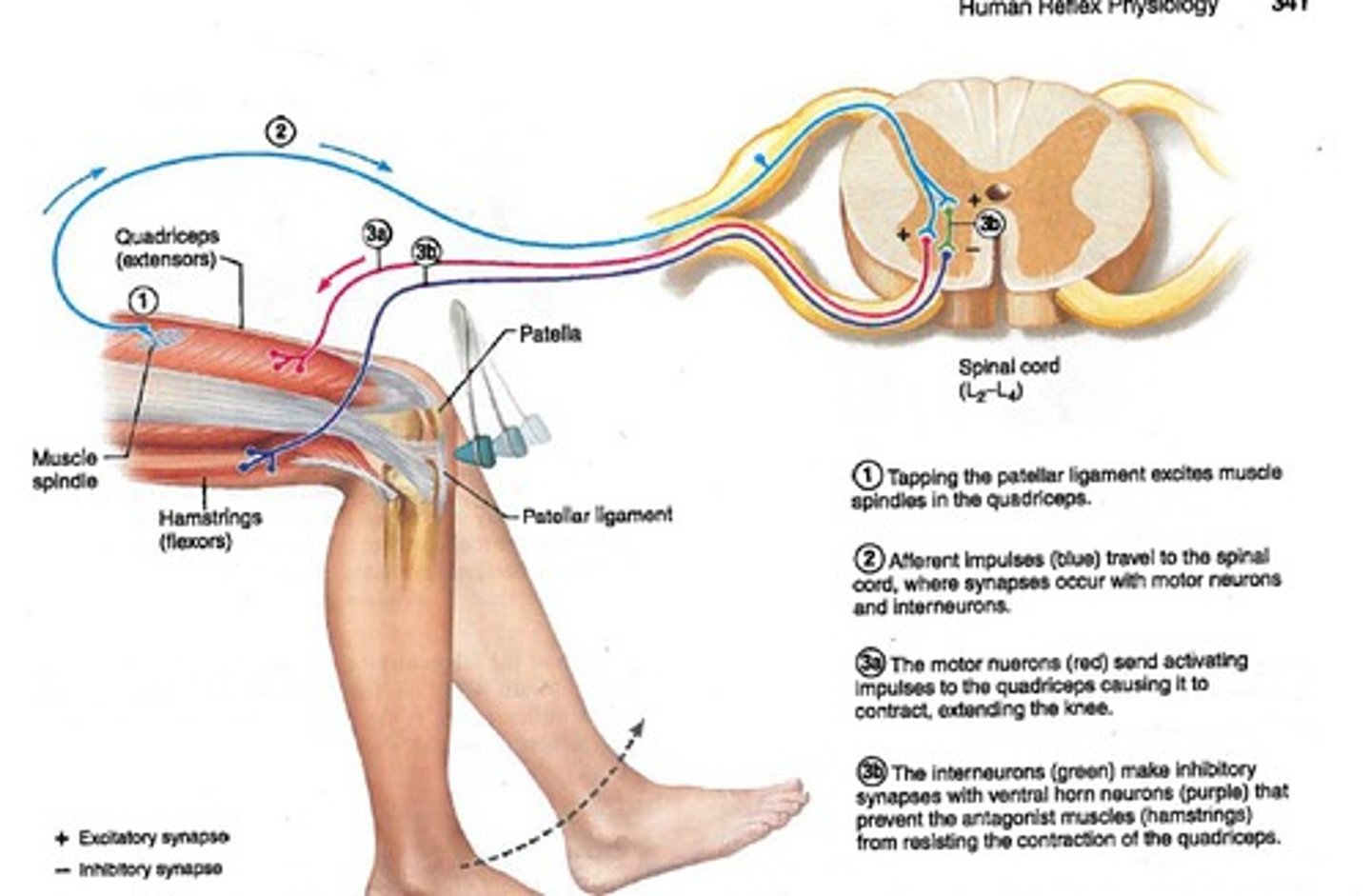
agonist pathway (monosynaptic)
antagonist pathway
(polysynaptic)
works together because you have anterior muscles that contract and posterior muscles that need to relax in order to kick
In a patellar tendon or knee jerk reflex (stretch reflex)
there are two efferent pathways why?
withdrawal or flexion reflex
Stimulus: pain (stepping on something sharp)
Receptor: nociceptors
Desired Action: pull foot away (flex)
- # synapses: multisynaptic
- Ipsi-contra?: ipsilateral
- effect on alpha motor neuron: excite (stimulate)
Reciprocal inhibition:
- # synapses: multisynaptic
- Ipsi-contra?: ipsilateral
- effect on alpha motor neuron: relax
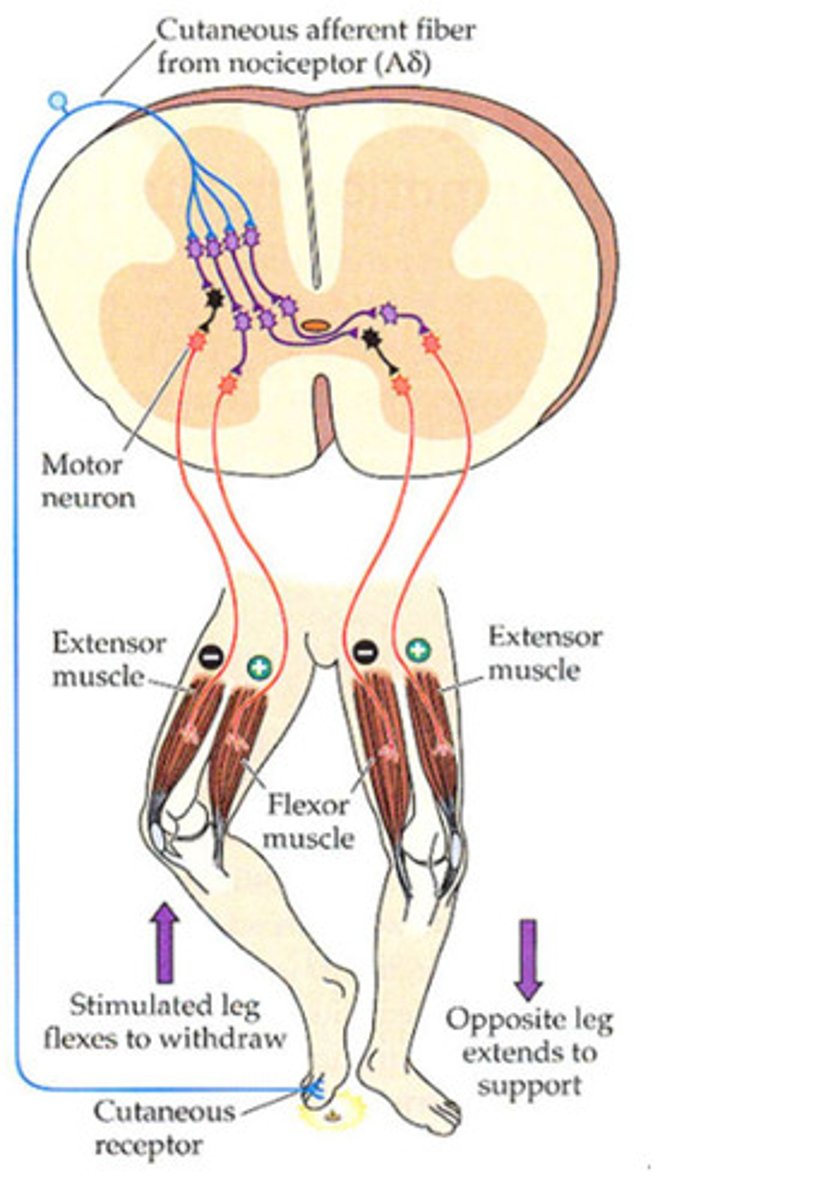
Crossed extensor reflex
Stimulus: pain (stepping on something sharp)
Receptor: nociceptors
Desired Action:
- # synapses: multisynaptic
- Ipsi-contra?: contralateral
- effect on alpha motor neuron: excite (stimulate)
Reciprocal inhibition:
- # synapses:
multisynaptic
- Ipsi-contra: contralateral
- effect on alpha motor neuron: relax

1. spinal cord
(spinal cord reflexes & some central pattern generators)
2. cerebellum & brainstem
(postural reflexes & hand and eye movement)
3. Cerebral cortex & basal ganglia
(true voluntary movements)
Where are the places CNS integration can occur?
CNS Control of Movement:
Reflex Movements
Simple movements & postural reflexes
Most are spinal or brainstem reflexes:
1. no input from cerebral cortex is needed
2. info also goes to other parts of the brain to be assessed
- response can be modulated:
enhanced or inhibited
Sensory info:
- proprioceptors, golgi tendon organs, muscle stretch receptors
- may also be used for following voluntary or postural reflexes
postural reflexes
maintenance of body position
most are integrated in the brainstem
sensory info: proprioceptors, vestibular apparatus, vision, tactile receptors
CNS Control of Movement:
Voluntary Movements
Desired movement
- often learned movement
May become involuntary
- automatic movements
- muscle memory
Integrated in the cerebral cortex
- but coordinated with input from other parts of the brain
- basal ganglia
- cerebellum
Sensory info:
- may be developed without external sensory input
- proprioceptors, vestibular apparatus, vision, tactile receptors
Rhythmic movements
- initiated by cerebral cortex
- maintained by central pattern generators: CPGs
- interneuron networks in brain and spinal cord
- some rhythmic movements maintained by spinal cord only
- variation of the pattern requires new cerebral cortex input
voluntary
but they can become involuntary
Are rhythmic movements voluntary or involuntary?
feedforward reflexes
preps body for movement
sensory feedback
allows continuous, smooth movement
coordination of movement
integration of multiple parts of the brain
1. Planning
2. Initiating
3. Executing
What are the 3 components of voluntary movements?
Planning the movement
"Higher Centers": integration from multiple areas
- Sensory cortex: current position info
- Prefrontal cortex & motor association areas: determines appropriate movement and the results
- Basal ganglia & thalamus: refinement of movement
Initiating the movement
Motor cortex to brain stem: starting action of specific motor units
- cortex area & # motor units
- Basal ganglia & cerebellum: modication of the movement
- humunculus
Executing the movement
local level of control: CNS to PNS
- brain stem to spinal cord:
direct motor cortex influence
- Basal ganglia & cerebellum: modifcation of movement
- Spinal cord to motor unit
- Continuous sensory feedback
Corticospinal pathway (cortex to spine)
(pyramidal or direct tracts)
- lateral, anterioral, corticobulbar tracts
- start at cerebral cortex and then work your way down: Descending pathway
What is the Voluntary Movement Pathway?
What are the different tracts?
Where does it start?
Lateral corticospinal tracts
(think Lateral = meduLLa = Low part of Limbs -> L!!!!!)
80-90% of pyramidal fibers
decussation in medulla
distal limbs, hands, feet
Anterior corticospinal tracts
(think Anterior = Axial)
10-20% of pyramidal fibers
decussation at level of synapse in spinal cord
axial trunk skeleton muscles
- hoola hooping
- also some proximal parts of limbs
Corticobulbar tracts
motor cortex to brainstem and cranial nerves
cortex -> bulb
decussation is variable
skeletal muscles in the head
- eyes, tongue, chewing, face, speech, neck
Brainstem pathway
May be a component of the extrapyramidal tracts
muscles of the trunk
- balance, posture, walking
most do NOT decussate
- which side of the brain controls movement in your right in external oblique muscle? idk...if they don't decussate, then it must be the right side??
involuntary - bc it begins in the brainstem
Pathway overlap and complement
corticospinal and brainstem pathways overlap in function
- corticospinal: most fine or detailed movement; most voluntary movement
- brainstem: most gross movements of balance, posture, and orienting the body relative to a stimulus; most involuntary movements of tonus, posture and balance
spastic paralysis
upper motor neurons are affected
reflexes still occur
flaccid paralysis
alpha lower motor neurons affected
muscles go limp and atrophy
hypertonia
increased muscle tone causes rigidity, spasms, cramps, spasticity after stretching
increase alpha motor neuron activity
decreased descending pathway inhibition
- C. tetani: block NT release to inhibitory interneurons
hypotonia
decreased muscle tone causes flaccid muscles
decrease alpha motor neuron activity
neuromuscular junction disorders
disorders of the muscle itself
Parkinson's
Symptoms:
- akinesis and bradykinesis in voluntary movements
- shuffling and unsteady gate
- lack of blinking
- tremors at rest
Malfunction of basal nuclei(ganglia) and activation of motor cortex
- degeneration of substantia nigra
--- decreased dopamine release to basal ganglia
--- decreased excitatory input to motor cortex
imbalance between excitatory and inhibitory input to basal nuclei and cortex
Treatments:
- L-dopa: dopamine receptor agonists, MAO and other dopamine enzyme inhibitor, electrical stimulation of underactive area, destruction of overactive areas
- undifferentiated embryonic stem cells
Cerebellar disease (intension tremor)
Symptoms: gate ataxia, tremors when moving, lack of coordination of movements, difficulty learning new movements and modification of movements
cerebellar damage: trauma and chemicals