CH61: The Patient with a Cardiovascular Disease (LECTURE)
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
23 Terms
Learning objectives
• Identify the cardiovascular conditions that may be encountered in patients seeking oral health care
• Discuss the etiology, symptoms, and risk factors associated with cardiovascular conditions
• Discuss the impact of cardiovascular diseases on the oral cavity and their relationship to oral health
• Plan dental hygiene treatment modifications for the patient with cardiovascular disease
Why this matters
Cardiovascular disease = #1 cause of death in the U.S.
Oral inflammation ↔systemic inflammation
Dental hygienists often first to identify risk factors
Our goal: keep hearts safe during care + support prevention
Cardiovascular system review
Heart + vessels work with lungs to deliver oxygen
Pump deoxygenated blood →lungs; oxygenated →body
Both systems interdependent —disease in one affects the other
Modifiable risk factors
90 % of MI & stroke risk is preventable
Change be changed: tobacco use, hypertension, hyperlipidemia, diabetes, obesity, stress, inactivity, poor diet
Non-modifiable: age, sex, family history
Dental team role = identify and reinforce healthy behaviors
Prevention and lifestyle counseling
Encourage tobacco cessation, exercise, diet changes
Link oral and cardiovascular health
Refer to physician if risk signs appear
Infective endocarditis
Bacterial infection of endocardium or heart valves →vegetations
Caused by: Streptococcus viridans, Staphylococcus aureus
Risk ↑ with bacteremia during subgingival instrumentation
Prevention = excellent oral hygiene + appropriate antibiotic prophylaxis
Who Needs Premedication?
Only for patients at highest risk of adverse outcomes from this
◦ Prosthetic valves or material used for valve repair
◦ Previous infective endocarditis
◦ Certain congenital heart defects
◦ Unrepaired cyanotic CHD (shunts/conduits)
◦ Repaired CHD with residual defect near prosthetic patch/device
◦ Cardiac transplant recipients with abnormal valves
Clinical Management for at risk pts
Review medical history each visit –confirm cardiac status
Ask: “Has your cardiologist recommended antibiotic premed?”
Delay elective care if unclear or unstable
Reinforce biofilm control & document antibiotic use
Fetal circulation and development
Fetal heart is completely developed by week 9 of gestation
Ductus arteriosus connects pulmonary artery →aorta (bypasses fetal lungs)
Normally closes shortly after birth
If it stays open →patent ductus arteriosus (PDA)
Congenital heart defects and dental implications
Ventricular septal defect (VSD) = most common congenital heart defect
Other examples: atrial septal defect (ASD) and PDA
May occur with Trisomy 21 and other genetic syndromes
Surgically repaired early in life (may involve prosthetic device or patch)
Premedication indicated for 6 months post-repair or if residual defect remains
If unsure whether premed is still needed, always consult with the cardiologist!
Rheumatic heart disease
From Group A strep →rheumatic fever →valve damage
Preventable by early antibiotic therapy for strep throat
Usually no premed unless other AHA indications exist
Mitral valve prolapse
Valve between left atrium and left ventricle doesn’t close properly →slight backflow of blood
May produce a click or murmur, often benign
Most cases asymptomatic
No premedication needed unless other qualifying cardiac condition exists
If patient uncertain, verify with physician before treatment
Heart murmurs and valve disorders
Murmur = sound from turbulent valve flow (not disease itself)
May indicate MVP or rheumatic scarring
Requires medical evaluation if new or symptomatic
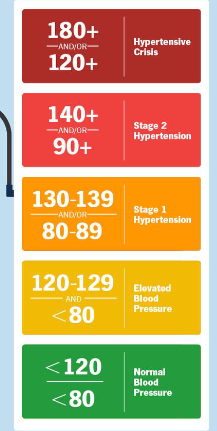
Hypertension
“Silent killer” → major MI/stroke risk
Risk factors: age, obesity, diet, stress
Proceed if controlled; stress reduction, epi ≤ 0.04 mg, monitor BP every visit
≥180/110 + symptoms (severe dyspnea, headache)→ activate EMS
Ischemic heart disease
Reduced blood flow → reduced oxygen to tissue → pain or tissue death
Includes angina, MI, and heart failure
Risk factors: atherosclerosis (*main cause), smoking, hypertension
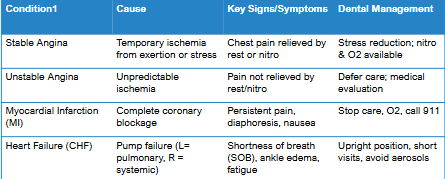
Angina pectoris
Chest pain due to temporary ischemia
Stable →predictable triggers (stress, exercise); relieved by rest/nitro
Unstable →unpredictable; may precede MI →urgent referral
Limit stress and chair time; always have nitro & oxygen accessible
Myocardial infarction
Complete coronary blockage → tissue death
Symptoms: chest pressure, nausea, sweating, shortness of breath, fatigue
Not relieved by rest or nitroglycerin
Emergency response: terminate treatment, sit upright, oxygen, call 911
Do not perform chest compressions unless unconscious & no pulse
Post Care:
Delay elective dental care 4-6 weeks, only after cardiology clearance
◦ Older “6 months” rule no longer currrent
Use stress-reduction techniques and monitor vitals
Keep oxygen and nitroglycerin available during appointments
Heart failure (CHF)
Heart can’t pump adequately
Left sided: pulmonary congestion →shortness of breath, fatigue
Right sided: systemic congestion →swelling in feet/ankles, distended neck veins
Both sides: fluid in lungs and legs
Semi-supine or upright; short appointments; limit aerosols
Ischemic and circulatory conditions at a glance
Cardiac arrhythmias and devices
Abnormal rhythm or rate →may have pacemaker or ICD
Can be symptomatic or asymptomatic
Most do not require treatment
If they do:
◦ Drug therapy
◦ Lifestyle modification
◦ Medical procedures
Cardiac surgery and devices
CABG: bypass surgery; no premed after healing (~6 weeks)
Coronary stent: on antiplatelets →mild bleeding; don’t stop without MD approval
Pacemaker/ICD: avoid electromagnetic interference (ultrasonic cords, magnets)
Document device type + placement date
Antithrombotic therapy
Warfarin, DOACs, Aspirin, Clopidogrel ↑bleeding risk
Do not discontinue without physician clearance
Use local hemostatic measures (pressure, sutures, hemostatic agents)
Appointment planning and instrumentation
Review history & BP each visit
Stress-reduction protocol (quiet room, short appointments)
Semi-supine if dyspneic
Use HVE; avoid ultrasonic if pacemaker unshielded or respiratory distress present
Patient education and collaboration
Emphasize daily biofilm control →↓bacteremia risk
Reinforce modifiable risk factors (quit smoking, diet, activity)
Encourage compliance with meds & follow-ups
Coordinate with medical providers as needed
Key takeaways
Identify cardiac risk →modify care appropriately
4–6 weeks post-MI before elective care (when cleared)
AHA premed = high-risk only
90 % of CVD risk modifiable —DH impact matters