Silverstein and Hopper Chapter 81: Critical Illness-Related Corticosteroid Insufficiency
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
17 Terms
Critical Illness Related Corticosteroid Insufficiency (CIRCI)
Inadequate cellular corticosteroid activity for the severity of the patient's disease
Pressor-resistant hypotension is the most commonly reported clinical manifestation
Cortisol
Hormone released by the adrenal glands in small amounts in a circadian rhythm and in larger amounts during times of physiologic stress
Important Homeostatic Functions of Cortisol
Regulation of carbohydrate, lipid, and protein metabolism
Immune system modulation
Ensuring proper production of catecholamines and function of adrenergic receptors
Stabilizing cell membranes
Pathway of Cortisol Release
Hypothalamus produces corticotropin-releasing hormone (CRH) -> stimulates the anterior pituitary to release ACTH
Hypothalamus-derived arginine vasopressin works synergistically with CRH to enhance ACTH secretion
ACTH in circulation stimulates the zona fasciculata and zona reticularis of the adrenal gland to release cortisol
Negative Feedback of Cortisol
Cortisol has negative feedback action on the hypothalamic and pituitary release of these stimulatory hormones
When circulating cortisol concentration is low, CRH and ACTH increase, which stimulates cortisol production -> increased serum cortisol concentration inhibits the release of more CRH, arginine vasopressin, and ACTH
Cortisol in Circulation
Once in circulation, most cortisol is bound to corticosteroid binding globulin (CBG) and a small fraction is bound to albumin
Cortisol not protein-bound is free cortisol, the biologically active fraction
Action of Free Cortisol
Free cortisol enters target cells and binds the glucocorticoid receptor (GR) in the cytoplasm
GR-cortisol complex translocates to the nucleus where it affects the transcription of hundreds to thousands of genes which alters cell function
Cortisol exerts is nongenomic effects by intercalating into cell or mitochondrial membranes
What can decrease circulating cortisol?
Direct trauma, infarction or hemorrhage, or cytokine influence may impair the HPA axis function, decreasing circulating cortisol
Multiple medications are known to decrease cortisol production
Ketoconazole
Etomidate
Propofol
Opiates
Increased Cortisol in Critically Ill People
Critically ill people often have increased free and total cortisol concentrations in the face of low ACTH concentrations
Evidence that molecules other than ACTH, such as cytokines, lipopolysaccharide-bound toll-like receptors, and endothelin drive adrenal cortisol production and release independent of ACTH
The fraction of total cortisol that circulates as free (active) cortisol is increased in critical illness which may inhibit the hypothalamus and pituitary, leading to lower ACTH concentration
Free cortisol is increased because systemic inflammation decreases hepatic synthesis of cortisol's carrier proteins CBG and albumin
Acidemia, hyperthermia, and increased neutrophil activation lead to structural changes in CBG that lower its affinity for cortisol
There is also impaired cortisol metabolism by the kidney and liver
While circulating free cortisol concentration is often increased in critical illness, target tissues may be cortisol resistant
Glucocorticoid receptor structure and number are altered in sepsis
What is CIRCI likely due to?
The combination of altered production, plasma protein binding, metabolism, and target tissue effects of cortisol
Clinical Manifestations of CIRCI
Most common clinical abnormality is pressor-resistant hypotension
Logical since glucocorticoids influence adrenergic receptor function
Studies in people with septic shock have shown that low-dose corticosteroid administration leads to more rapid improvement in blood pressure than placebo
Critically ill dogs with poor response to exogenous ACTH may be more likely to be hypotensive than those with more robust response
People with altered cortisol response to ACTH may be more likely to die than those with similar illness severity and a normal HPA axis function
Complete adrenal failure is an uncommon manifestation of CIRCI
Diagnosing CIRCI in People
Unknown how to diagnose CIRCI
Current clinical guidelines recommend using either a resting cortisol or the 250 ug standard ACTH stimulation test to diagnose CIRCI in people in favor of using the patient's hemodynamic response to hydrocortisone
Two large clinical trials found no relationship between plasma cortisol testing and benefit from hydrocortisone therapy in pressor-resistant septic shock
Suggested that ACTH stimulating testing and resting cortisol measurements are unlikely to accurately diagnose the condition
The best way to identify critically ill patients that would benefit from corticosteroid therapy is unclear
Diagnosing CIRCI in Dogs and Cats
No recommendation can be made regarding how to make a diagnosis of CIRCI in dogs or cats
Treating CIRCI in Septic Shock in People
Current guidelines for CIRCI recommend the use of low-dose hydrocortisone (<400 mg/day/adult) for 3 or more days in people with septic shock that is not responsive to fluid and moderate to high-dose vasopressor therapy
The current Surviving Sepsis Campaign guidelines make the recommendation as a negative, suggesting against using hydrocortisone if fluid and vasopressor therapy are able to restore hemodynamic stability
If hydrocortisone is used, it should be 200 mg/day/adult
Both sets of guidelines recognize these recommendations as "conditional" or "weak", supported by low quality of evidence
In general hydrocortisone is given either as four divided doses daily (e.g. 50 mg every 6 hours, to total 200 mg/adult/day) or as a loading dose of 100 mg hydrocortisone followed by 10 mg/hr as a CRI (240 mg/adult/day) in people
Unclear whether tapering of hydrocortisone is required
Fludrocortisone is not recommended in any guidelines, likely because it was found not to improve survival when used in conjunction with hydrocortisone and because at relevant doses of hydrocortisone, all aldosterone receptors would be occupied
Corticosteroids are not recommended for people with sepsis that are not in septic shock
Treating CIRCI in Cardiopulmonary Arrest in People
Limited evidence for improved survival with good neurological function after administration of methylprednisolone during cardiopulmonary resuscitation in people
Limited evidence for improved survival with good neurological outcome after administration of hydrocortisone for people who are in shock after return of spontaneous circulation
Treating CIRCI in Dogs and Cats
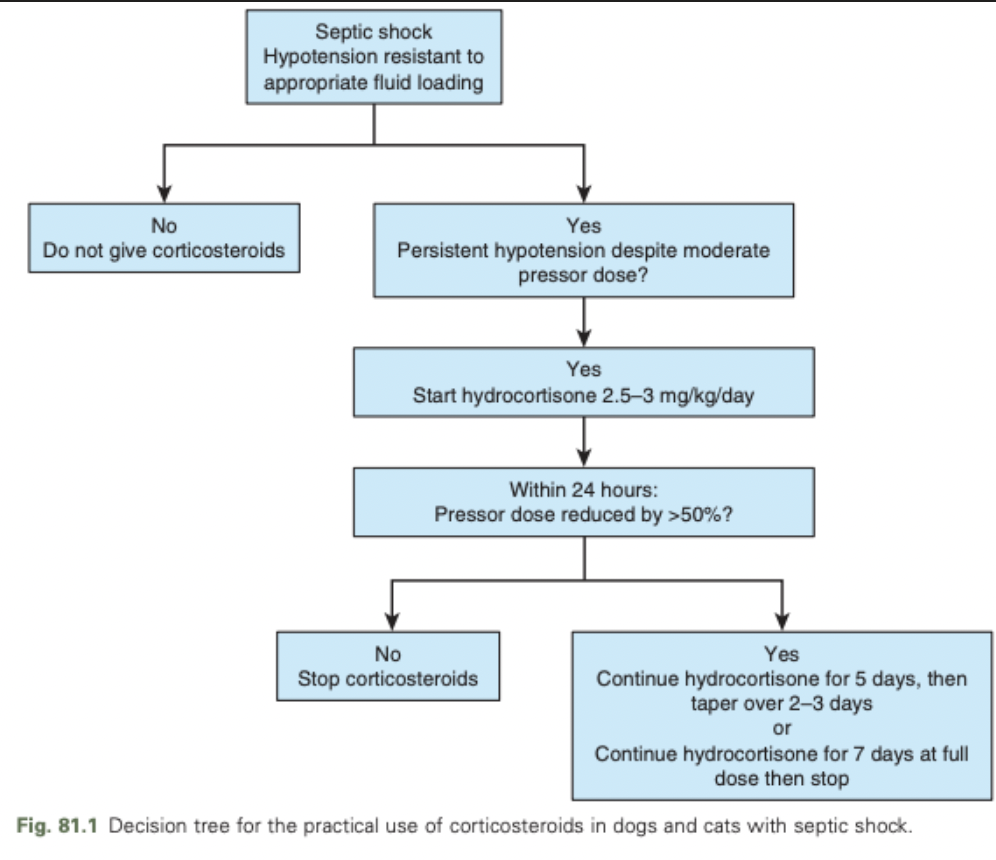
Dogs and cats with fluid-loaded, pressor-refractory septic shock can be treated with 2.5-3 mg/kg/day of hydrocortisone as a CRI
Reasonable to continue steroid therapy only in patients that show significant improvement in cardiovascular status within 24 hours of starting the drug
Prognosis for CIRCI
Within a week of ICU discharge, ACTH and cortisol increase to supra-normal levels in people
If the patient survives the primary underlying illness, prognosis for return of normal HPA axis function is good