Week 2: Collecting Data and Health Assessment Techniques
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
27 Terms
General Survey
Initial assessment of patient appearance and behavior.
Level of Consciousness (LOC)
Assessment of awareness using person, place, time.
Anthropometric Measurements
Height, weight, and BMI calculations for health assessment.
Vital Signs
Indicators of health status and body function.
Blood Pressure (BP)
Average 120/80; influenced by various factors.
Heart Rate
Normal range 60-100 beats per minute.
Respiratory Rate
Measured for ease or struggle in breathing.
Temperature
Normal range 35.9°C to 38.1°C.
Pediatric Assessment
Tracks development percentiles and health concerns.
Daily Weights
Monitored for changes in cardiac/renal patients.
BMI
Body Mass Index; weight relative to height.
Framingham Risk Score
Predicts cardiac event risk over 10 years.
Nutrition Status
Assessed through appetite, intake, and hydration.
Dehydration Signs
Cracked lips, no urine, vomiting bile.
Health Interview
Foundation for gathering patient care information.
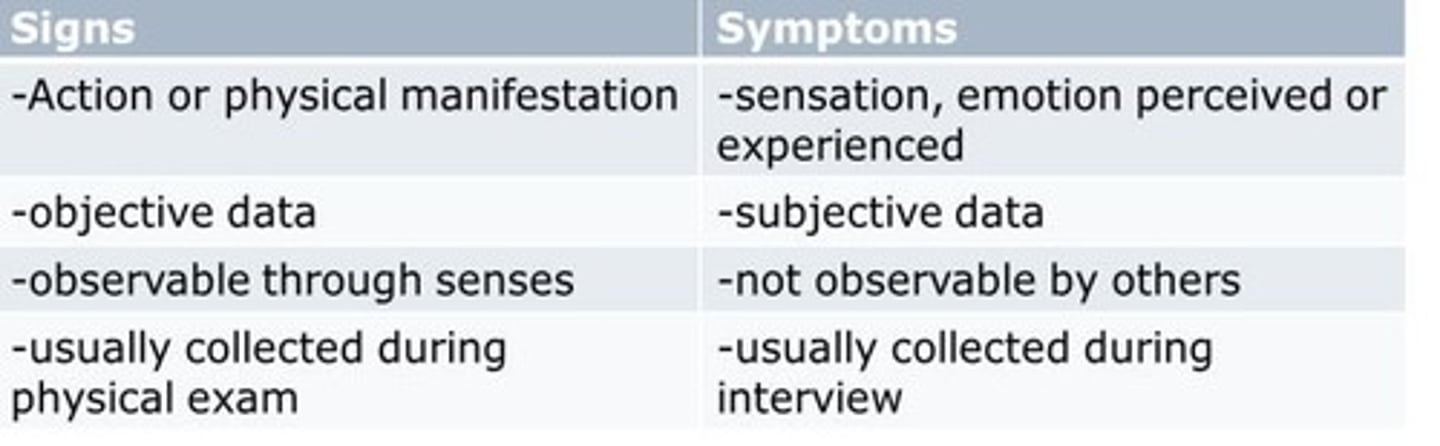
Subjective Data
Information reported by the patient.
Primary Data Source
Patient as the main source of information.
Secondary Data Sources
Family, charts, and other professionals' insights.
Health Interview Planning
Establish goals and prepare for patient interaction.
Demographic Data
Confirms patient identity and background.
History of Present Illness
Details symptoms using 10 attributes.
Sensitive Topics
Discuss alcohol, drugs, and mental health non-judgmentally.
Cultural Considerations
Cultural beliefs affecting health perceptions.
Environmental Considerations
Safety and exposure factors impacting health.
10 Attributes of Symptoms
Includes location, timing, severity, and patient perspective.

Review of Systems
Assessment of 14 different body systems.
Constitutional Symptoms
Overall presentation of the patient's health.