Fluid and Electrolyte Pathophysiology
1/210
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
211 Terms
Where do cells of the body contain fluid?
inside of them and are surrounded by fluid (outside)
Fluid in the body provides
the medium in which all of the biochemical reactions, necessary for life, can occur
The concentration of solutes, solvents, as well as the pH of body fluids are maintained within a __________ range in order to support life
narrow
Derangements in the body fluid composition can have
life threatening effects
The body fluid is distributed amongst
various compartments
The water within the body fluid can move ________ from compartment to compartment
freely
The solutes within the body fluid can only move based on
concentration gradients and the permeability of various compartments to those solutes
The two main compartments for body fluid are the
intracellular space
extracellular space
intracellular space, which contains
intracellular fluid
extracellular space, which contains
extracellular fluid
The extracellular space is further divided into the
interstitial and intravascular spaces
Intracellular fluid = _____ of body fluid
2/3
Extracellular fluid = _____ of body fluid
1/3
Intravascular ____% of body weight
5
Intravascular ____L
3
Should you add more of the blue chart??
Total Body Water (TBW) is maintained within a
narrow range despite any significant variations of water intake and/or elimination
What are the (3) primary sources of water intake
1. Drinking water
2. Ingestion of water contained within food
3. Byproduct of ATP production
What are (3) primary sources of water elimination
1. Renal excretion (greatest source of loss)
2. Stool
3. Evaporation from lungs, skin, sweat, etc. (insensible loss)
•Water moves freely between compartments based on:
• Concentration gradients
• Hydrostatic pressure gradients
What happens when you give a hypotonic fluids
cell swelling
Hydrostatic pressure gradients
Capillary hydrostatic pressure (blood pressure)
pushes water from blood stream (capillaries) to the interstitial space
Hydrostatic pressure gradients
Capillary oncotic pressure
sucks water into blood stream (capillaries)
Hydrostatic pressure gradients
Interstitial hydrostatic pressure
pushes water from interstitial space to blood stream (capillaries)
Hydrostatic pressure gradients
Interstitial oncotic pressure
sucks water from blood stream (capillaries) into the interstitial space
What is Hydrostatic pressure gradients
Basically 2 forces pushing water out of the blood stream and 2 forces pushes water into the blood stream
•Imbalance between any of the 4 forces (Hydrostatic pressure gradients) leads to altered water balance causing
1. Edema
2. Dehydration
Water movement picture?

What is edema
Excessive accumulation of fluid within the interstitial space
Edema is most often a problem of
How the fluid is distributed, not a water excess
Can edema cause dehydration and edematous at the same time?
What causes edema?
Capillary hydrostatic pressure (↑ or ↓)
(↑)
What causes edema?
Capillary oncotic pressure (↑ or ↓)
(↓)
What causes edema?
Interstitial hydrostatic pressure (↑ or ↓)
(↓)
What causes edema?
Interstitial oncotic pressure (↑ or ↓)
(↑)
What causes edema?
Capillary membrane permeability (↑ or ↓)
(↑)
What causes edema?
______ obstruction
Lymphatic
What are thing that are caused by edema via
Increased capillary hydrostatic pressure
• Venous obstruction
• Sodium/water retention
• Venous blood cots
• Tight clothing around extremities
• HTN
• Volume overload
What are thing that caused edema via
Increased capillary permeability
•Inflammation or immune response mediators released which increase capillary permeability
What are thing that cause edema via
Lymphatic obstruction
• Lymphatic vessels are blocked due to infection or tumor
• Lymphatic vessels damaged or removed intentionally during surgery
• Leads to lymphedema
Edema- Can be _____ or ______
localized or generalized
Edema can be ______
(fluid follows path based on gravitational pull)
dependent
Edema can be ______ if severe
pitting
Increased edema creates
________ against which __________ must try to overcome; in order to _______
resistance
arterial blood flow
perfuse tissues
Increased edema creates
can lead to _______ if severe
tissue ischemia
Kidneys and hormones are responsible for maintaining ___________ balance
sodium and water
______ follows _____, so changing _______ concentrations changes ______ concentrations
Water follows salt
sodium
water
•Sodium is regulated primarily by
aldosterone
Water is primarily regulated by
anti-diuretic hormone
Sodium accounts for _______ % of extracellular fluid cations
90
Since sodium is always associated with _______, it to is in very high concentrations in the ________ fluid
chloride
extracellular
Remember when ______ dissolves in fluid it floats around as ______ in water
salt (NaCl)
Na+ and Cl-
What are sodiums three main "roles" in the body?
• maintenance of conduction of nerve impulses
• Regulation of acid-base balance (sodium bicarbonate)
• Transport of substances across the cellular membrane (Sodium-Potassium-ATP pump)
Alterations in sodium and water balance are _______ related
closely
When sodium concentration is altered, changes in
water volume occur
Alterations in the concentration of sodium in water are generally referred to in terms of
tonicity
(which is the change in electrolyte concentrations in relation to water)
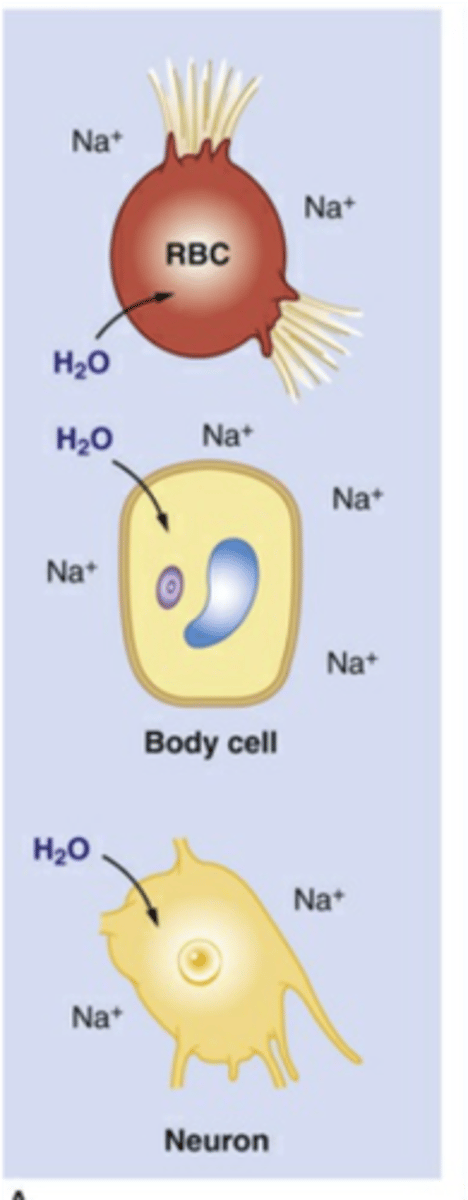
Hypotonic Alterations (picture)
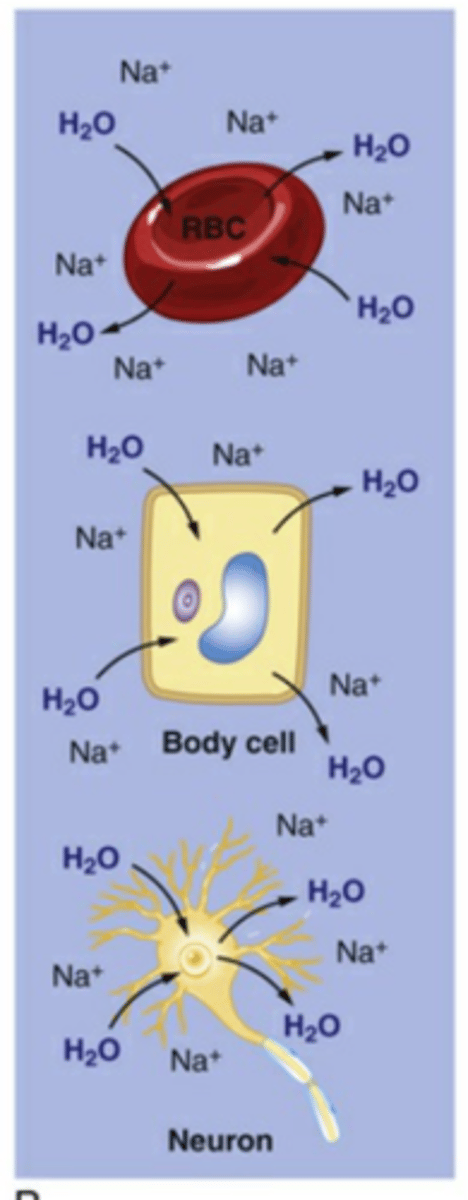
Isotonic Alterations (picture)
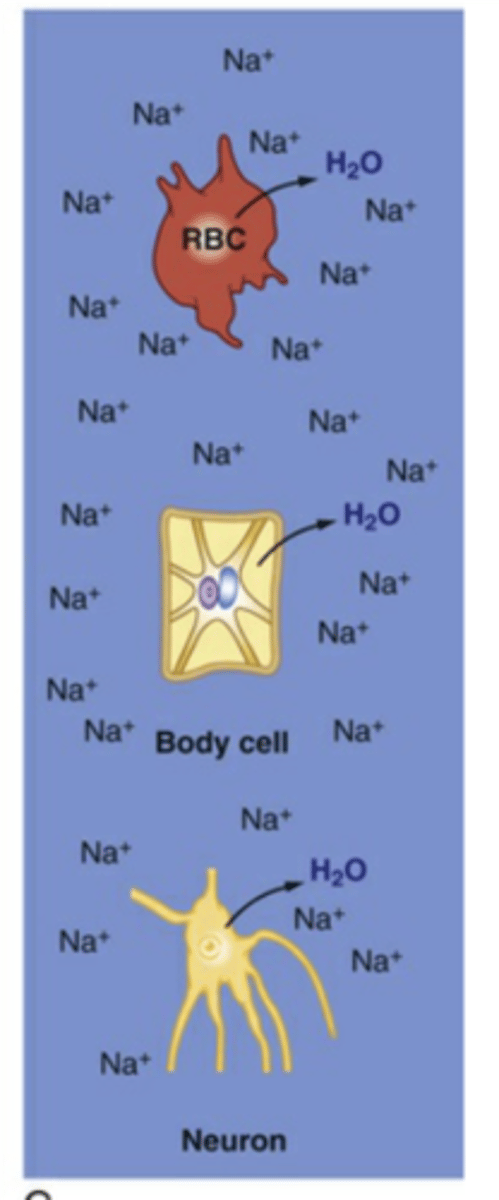
Hypertonic Alterations (picture)
What is the most common type of alteration between: Isotonic, Hypertonic, Hypotonic
Isotonic Alterations
Isotonic Alterations occur when there is a
proportional change in both the total body water (TBW) and the electrolytes
What are examples of Isotonic Alterations
• Hemorrhage (isotonic fluid loss)
• Sweating (isotonic fluid loss)
• Excessive IV fluid administration (isotonic fluid excess)
• Hypersecretion of aldosterone (isotonic fluid excess)
What are examples of Isotonic Alterations (isotonic fluid loss)
• Hemorrhage
• Sweating
What are examples of Isotonic Alterations (isotonic fluid excess)
• Excessive IV fluid administration
• Hypersecretion of aldosterone
Hypertonic Alterations - occur when
the electrolyte concentration is higher than normal in the extracellular fluid
(> 294 mOsm)
Hypernatremia
Amount of electrolytes increase in relation to water
Dehydration
Amount of water decreases in relation to electrolytes
Hypertonic Alterations
•Occurs when serum sodium levels
> 145 mEq/L
Hypernatremia can occur in
-
-
-
- hypovolemic
- euvolemic
- hypervolemic states
Risk factors for Hypertonic Alterations
1. Advanced age
2. Impaired mental state
3. Fever
4. Diarrhea
5. Vomiting
6. Use of diuretics
What is the MOST common and MOST severe sign of Hypertonic Alterations
•Central nervous system
What are Signs and symptoms of Hypertonic Alterations
1. Weakness
2. Lethargy
3. Muscle twitching
4. Hyperreflexia
5. Confusion
6. Coma
7. Seizures
Hypovolemic hypernatremia
• Loss of body sodium accompanied by a relative greater loss of body water
Hypovolemic hypernatremia
results from: (3 things)
loop diuretics
GI losses
failure of kidneys to concentrate urine
What is the MOST COMMON hypernatremia
Euvolemic
Euvolemic hypernatremia results from
loss of free water (water without sodium following it)
• Diabetes insipidus
• Water loss from burns
Hypervolemic Hypernatremia
• Rare
• Gain in in body water with a relatively larger increase in body sodium
• Infusion of hypertonic solutions
Hypotonic Alterations
• Occurs when the electrolyte concentration is lower than normal in the extracellular fluid
(< 280 mOsm)
Hypotonic Alterations
Leads to
intracellular overhydration (cell swelling)
Hypotonic Alterations
Is most pronounced in what two organs
the brain and lungs
What are the most common causes of
Hypotonic Alterations
• Sodium deficit (hyponatremia)
• Free water excess (water intoxication)
Hyponatremia
Develops when serum sodium concentration decreases to
< 135 mEq/L
What is the MOST COMMON electrolyte disorder
Hyponatremia
•Hyponatremia can have ..... varieties
-
-
-
- hypovolemic
- euvolemic
- hypervolemic varieties
Most individuals with Hyponatremia are
asymptomatic
Hyponatremia
can have issues with
edema and nervous cells depolarizing and repolarizing normally
Hyponatremia
Signs and symptoms
What is the sodium levels when symptoms are
Nausea and vomiting
125-130 mEq/L
Hyponatremia
Signs and symptoms
What is the sodium levels when symptoms are
lethargy, headache, confusion, apprehension, seizures, coma
Na+ < 125 mEq/L
hypovolemic hyponatremia
•Occurs with
loss of total body fluid and relatively larger loss of body sodium
hypovolemic hyponatremia
• Caused by
prolonged vomiting, severe diarrhea, inadequate aldosterone (adrenal insufficiency)
Euvolemic hyponatremia
Loss of
sodium without significant loss of body water
Euvolemic hyponatremia
Caused by
SIADH, inadequate dietary sodium intake, and glucocorticoid deficiency
Dilutional hyponatremia
Caused by
excessive intake of free water (drinking too much or D5W IV fluids)
Hypervolemia hyponatremia
Occurs when
there is an increase in sodium but a relatively larger increase in body water
Hypervolemia hyponatremia
Caused by
congestive heart failure or cirrhosis of the liver
Hypochloremia (lab value)
Serum chloride level < 97 mEq/L
Hypochloremia occurs with
hyponatremia
cystic fibrosis
elevated bicarbonate concentration
What is the major intracellular electrolyte
Potassium
Potassium intracellular concentration is
150 to 160 mEq/L,
Potassium extracellular concentration
3.5 to 5.0 mEq/L