Peri-anesthesia Monitoring and Complications 2
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
59 Terms
The most ideal heart rate is a ____?
Resting heart rate
Large dogs have what resting HR?
35-100 Bpm
Medium dogs have what resting HR?
50-120bpm
Small dogs have what resting HR?
80-150bpm
Cats have what Resting HR?
90-160bpm
Horses have what resting HR?
25-45
If a patient has an arrhythmia or severe bradycardia how to should you measure HR?
Count over 20-30 and multiply by 3 or 2
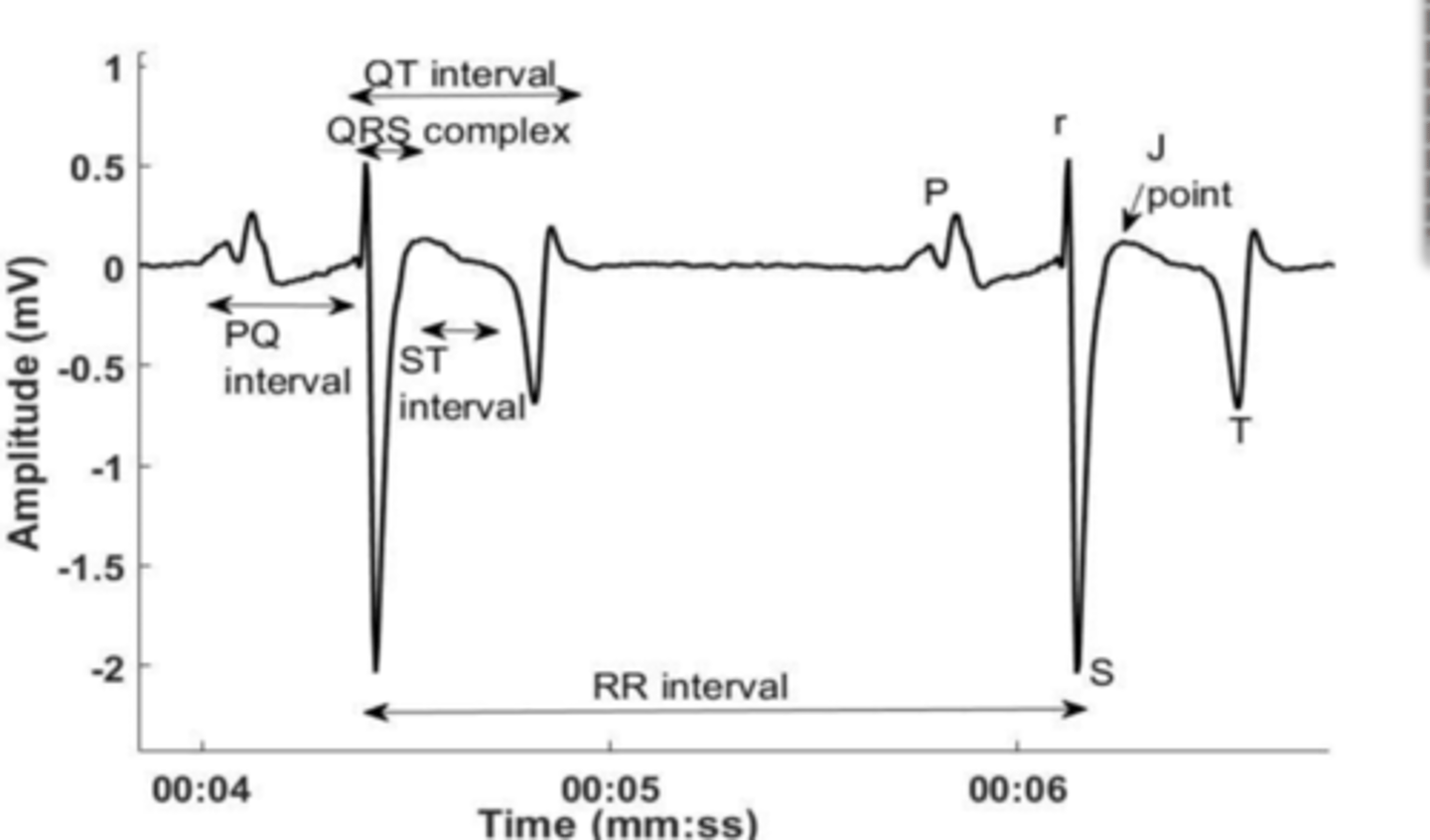
What will an ECG tell you?
Only electrical signal
Should you place ECG first?
No - always place capnograph and pulseox first
Small animals will use what leads?
Lead 2
Horses and cattle will use what kind of leads?
Base-apex lead (Lead 1)
Where is the proper placement of the lead on large animals?
White -on neck
Red - FR
Black - FL
What is the purpose of ECG?
Find obvious arrhythmias and major changes
You can use the ___ if forelimbs aren't accessible?
Ears
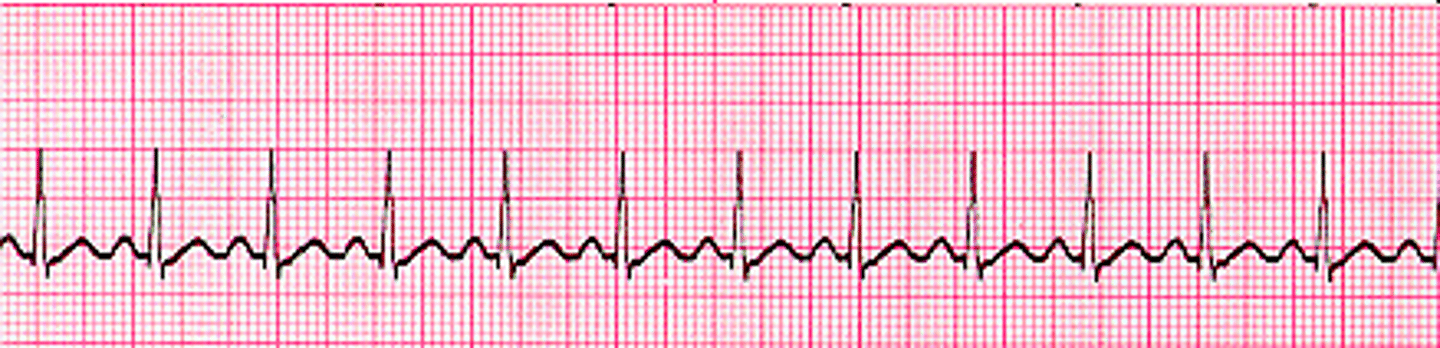
Is this a a normal ECG?
Yes for large animals and birds
What breed naturally gets sinus bradycardia under anesthesia?
Miniature dachshunds

What will sinus bradicardia going to look like on ECG?
Longer R-R
What is going to cause vagal sinus bradycardia?
-Anesthesia
-Opioids
-Sedatives
-Hypothermia
-Neck/abdomen/ manipulation
What is going to cause non-vagal sinus bradycardia?
Cardiac dz
Endocrine dz
Electrolyte abnormality
Beta blockers
Ca2+ channel blockers
When do we tx sinus bradycardia?
Hypotension
What animals is sinus bradycardia dangerous?
Young - neonates esp if hypotensive
-fixed sv so HR dependent CO
How can tx vagal bradycardia?
Anticolenergis
- Atropine (less potent, most efficacious 60min)
- Glycopyrrolate (Less efficacious but more potent 90min)
Which drug used to tx sinus bradycardia will be more likely to cause tachycardia and should be used in emergency situations?
Atropine,
(glycopyrrolate might not work and need multi-doses)
What interactions will anticholinergics have w/ A2 agonists?
Increased work load due to A2 causing vasoconstriction and Anticolinergic causing increased HR
You should avoid using an anticholinergic for ____ after use of dexmedetomine?
60mins
What is paradoxical bradycardia caused by anticholinergics?
A decrease in HR or AV block that will resolve w/ time
How do you tx non-vagal bradycardia?
Stop the cause
Isoproterenol - Nonselective B agonist
Pacemaker
What will we see on the ECG if we have sinus Tachycardia?
RR interval will be shorter
What will happen physiologically w/ sinus tachycardia?
Shorter diastolic period - less filling time
Less coronary perfusion
Decrease CO b/c smaller SV
What are causes of sinus tachycardia?
High Sympathetic tone - less depth, pain
Compensatory response (baro/ hypovolemia/ hypotension)
High sympathetic tone will have __ in BP and HR, Compensatory response will have ____ in BP and HR?
Increased
Separation
How do you tx High sympathetic tone sinus tachycardia?
More analgesics
Increase vaporizer
How do you tx compensatory response sinus tachycardia? ?
Decrease vaporizer
Volume replacement (5ml/kg fluid bolus)
Colloid
Tx hypotension
If the tachycardia is persistent in Hight SNS tone sinus tachycardia what drugs can we use to tx?
Esmolol -Beta antagonist (give loading dose and CRI)
Diltiazem - ca2+ channel blocker (refrigerated)
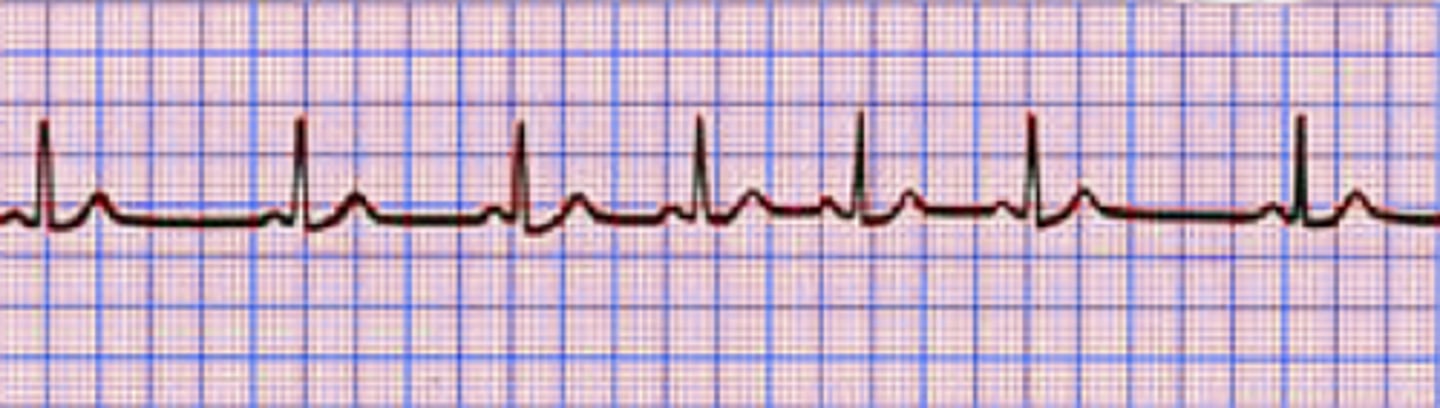
What is a respiratory sinus arrhythmia?
Benign arrhythmia due to decrease in pleural pressure during inspiration - increase in venous return, volume in R atria and stimulating stretch receptor while increasing HR. Will stop w/ cessation
How do you tx respiratory sinus arrhythmia?
No tx necessary
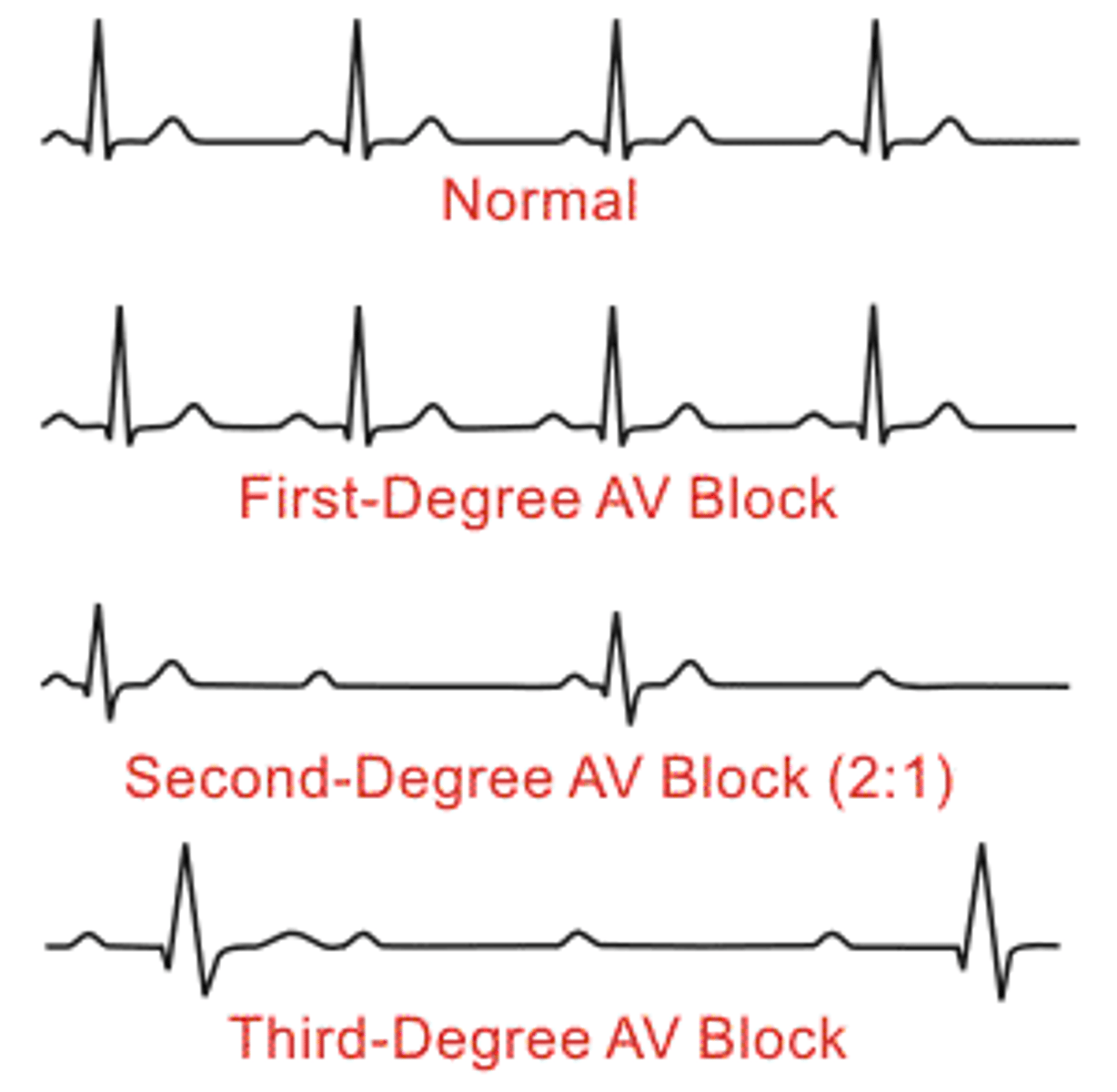
What an AV block 1ST degree?
Delay in transmission, PR interval is prolonged but every P wave has a QRS complex
What causes AV block 1ST degree?
Vagal tone
Drugs - beta blockers, Ca2+ channel blockers
Electrolyte abnormalities
Heart dz
Should you tx AV block 1ST degree?
No tx needed - very minor
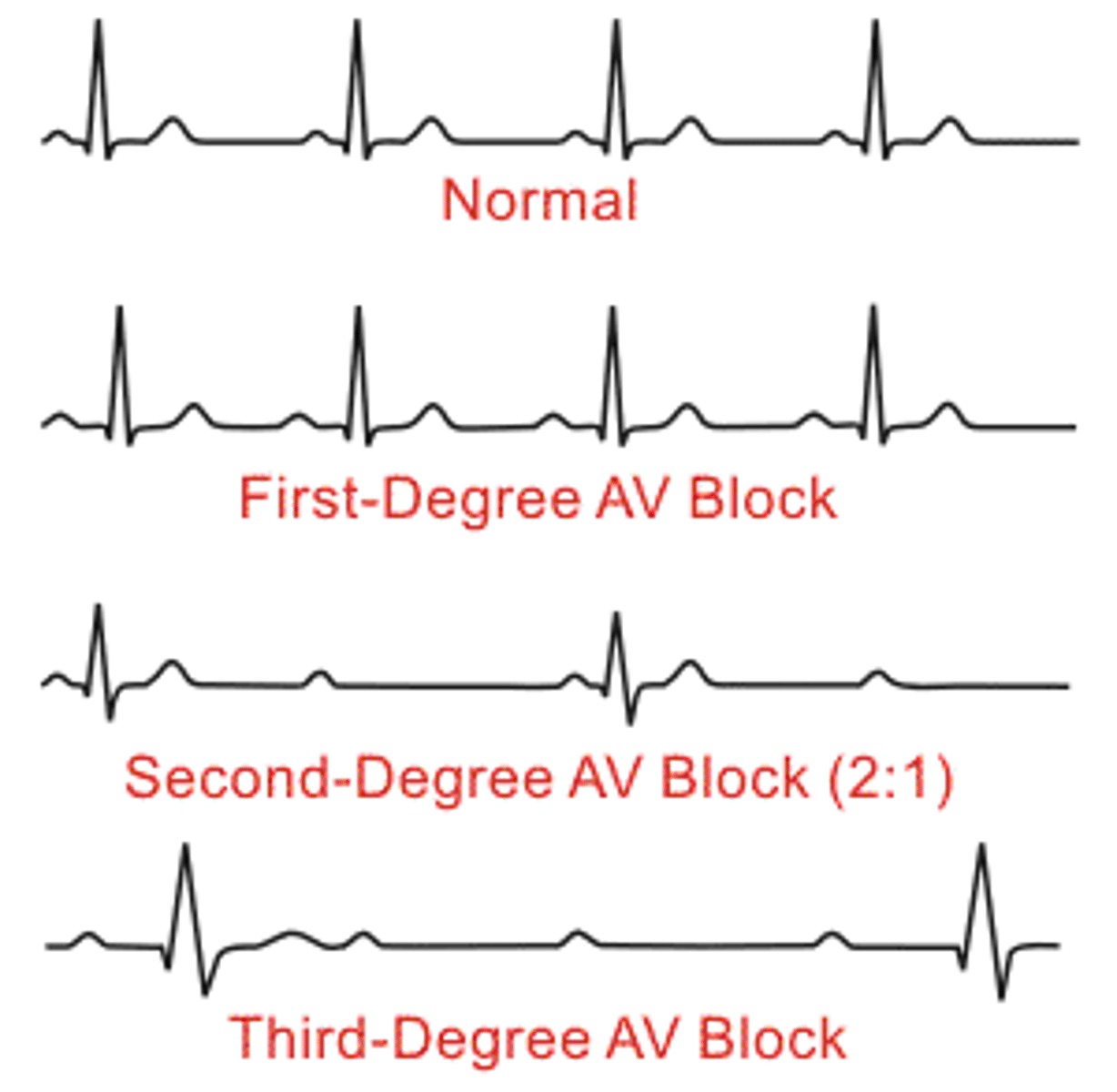
What is a AV 2nd degree block?
Intermediate failure of AV conduction - not all P waves have a QRS complex - occasional drops
What is mobitz type 1 AV 2nd degree block?
Vagal - prolonged P-R intervals before beat drops
What is Morbitz type 2 AV 2nd degree block?
A pathological condition in which there is no prolongation of P-R interval before dropped beat - sudden drops
When do you tx AV 2nd degree block?
If hypotensive or progressing severely w/ time
Type 1 AV 2nd degree block is treated w/ _____ and type 2 is treated w/ ___?
Anticholinergics - type 1
Pacemaker - type 2
What is a 3rd degree AV block?
Complete AV dissociation - no relation between P and QRS complex - PP and RR are constant
What are most common cause of 3rd degree AV block?
Pathological
-heart dz
-hyperkalemia
-digoxin tox
What is the severity of a 3rd degree AV block dependent on?
Ectopic pacemaker location (junctional better. ventricle can have problems)
What animals will have asymptomatic 3rd degree AV block?
Cats - adequate ectopic pacemaker rates
What is tx of 3rd degree AV block?
Pacemaker
Stop procedure if possible
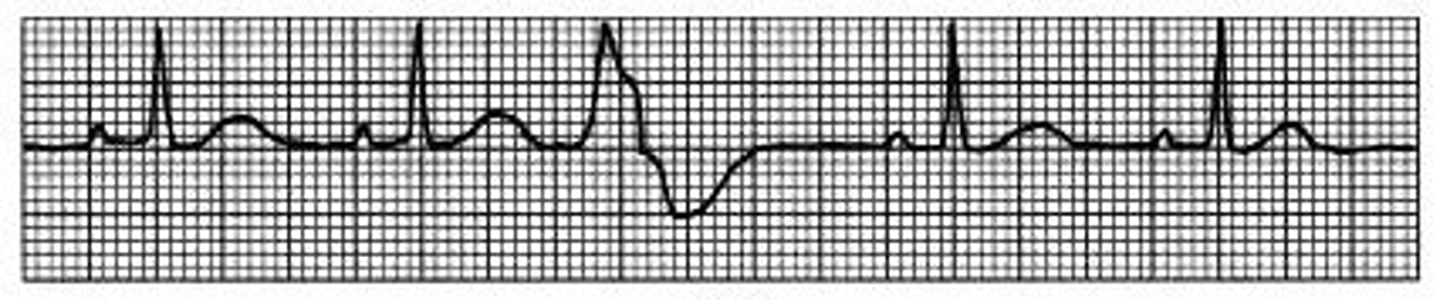
What is a ventricular premature complex (VPC)?
Depolarization of ectopic area in ventricle that is more rapid and premature than signal at SA node
-missing P wave,
-shorter RR interval,
-wide bizarre QRS complex
What are common causes of ventricular premature complex (VPC)?
Reentery - (something wrong with the heart)
High SNS tone - GDV, pain, high stress
How can you tell if ventricular premature complex (VPC) is clinical needing tx?
Pay attention to pulseox wave and if AUC of each triangle is large enough you still have an adequate stroke volume
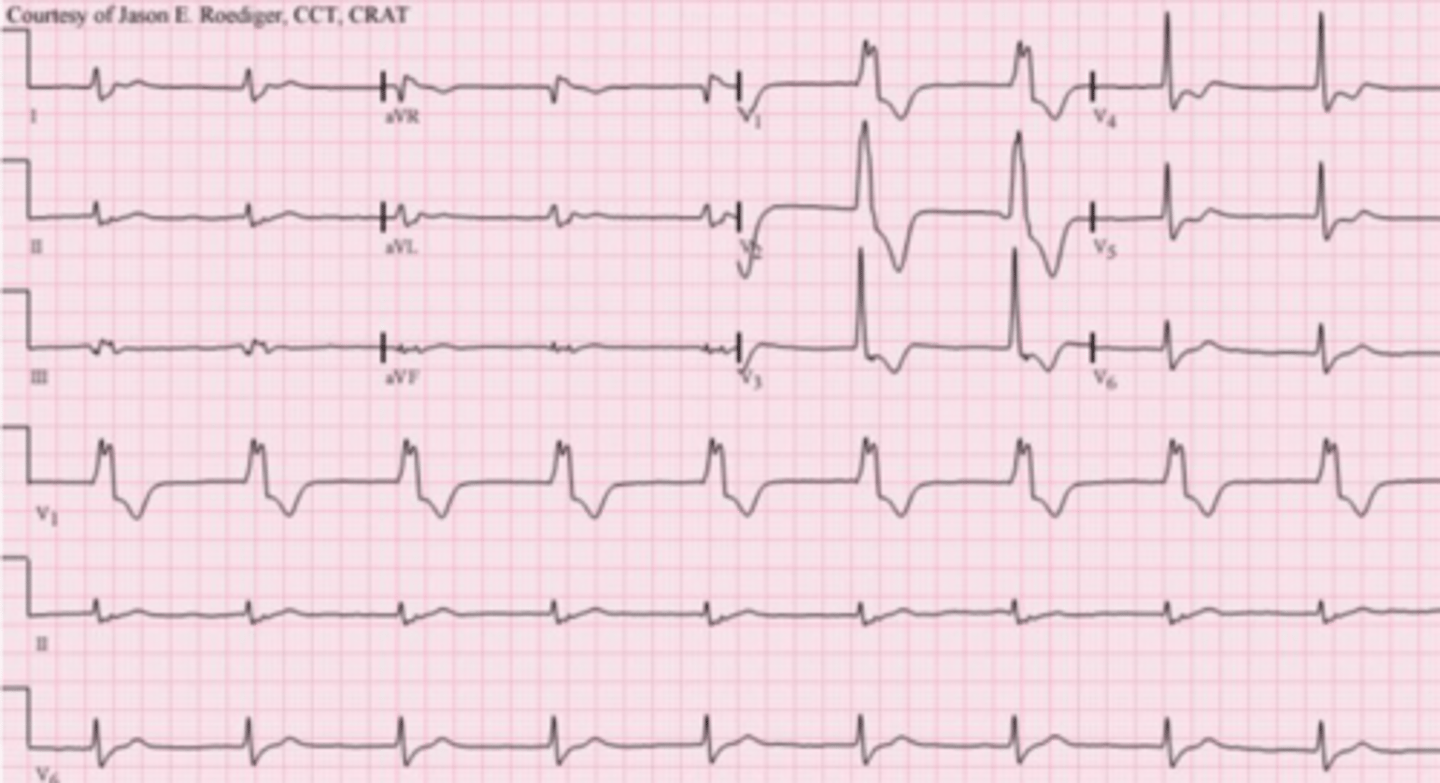
When do you have V-tach?
4 or more VPC in succession at more than 160 BPM
What do you do if the pet is in V-tach?
Check for pulse
-no pulse - CPR - Cardiac arrest
-Pulse - correct hypotension
What is tx for VPC/ V-tach?
Lidocaine -Na+ channel blocker B1 antiarrythmics
Procainamide - class A1
What is an accelerated idioventricular rhythm
slow V-tach - alternating between 2 sites - no tx nessasary
When are accelerated idioventricular rhythm most common?
GDV,
splenic dz
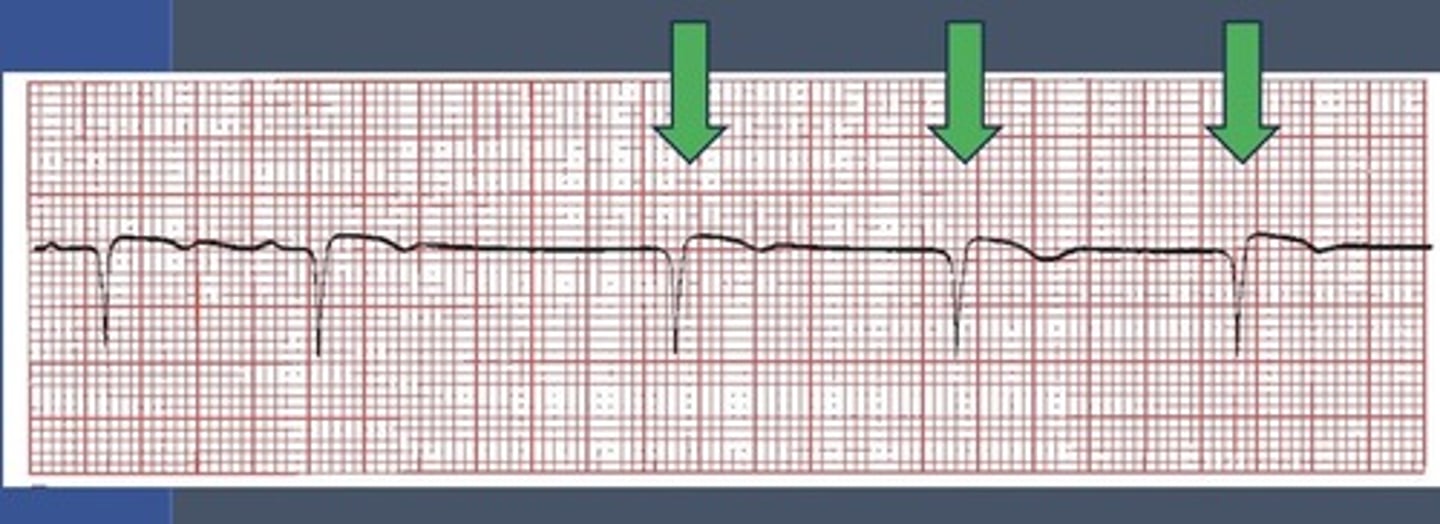
What is an escape beat?
Normal spontaneous depolarization of junctional or ventricular pacemakers - safety system in cases of conduction failure
Escape beats will alway follow a ___ and should ___ be treated?
Pause
Not be treated as VPC (can use anticholinergics