Female Reproductive System pt. 2
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
21 Terms
Luteinization + progesterone
The LH surge transforms the collapsed follicle into the corpus luteum (yellowish body). The luteinized granulosa and theca cells of the corpus luteum begin to produce large amounts of progesterone.
Progesterone triggers a negative feedback at the hypothalamus and pituitary, which keeps GnRH, LH, and FSH secretions low so no new dominant follicles develop.
Luteal phase meaning
The post-ovulatory phase of progesterone secretion.
What is corpus albicans and why does it form?
If pregnancy does not occur within 10 to 12 days of ovulation, the corpus luteum will stop secreting progesterone and degrade into corpus albicans, a nonfunctional whitish body that will disintegrate in the ovary over a few months.
Since progesterone secretion is reduced, FSH and LH are again stimulated and the follicular phase begins again.
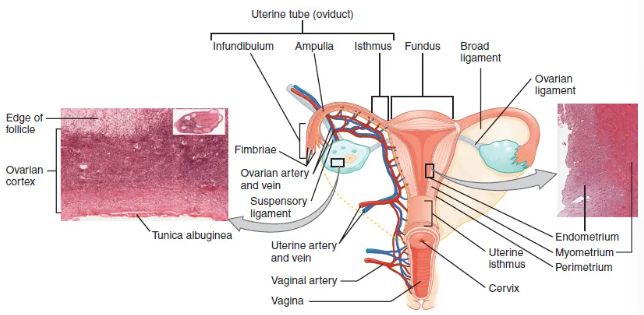
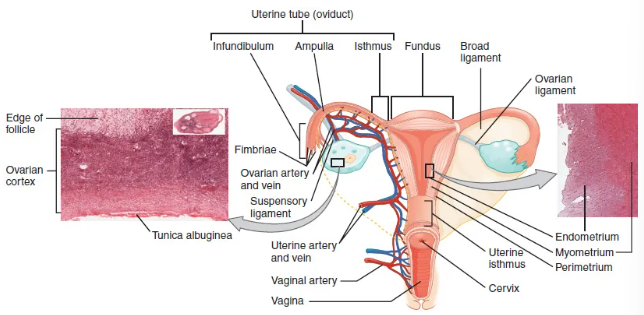
Uterine tube structure
Fallopian tubes. Serve as a conduit of the oocyte from the ovary to the uterus.
The isthmus is the narrow medial end of each uterine tube connected to the uterus.
The wide distal infundibulum flares out with slender, finger-like projections called fimbriae.
The middle region of the tube (ampulla) is where fertilization occurs.
Uterine tube layers
Outer serosa, a middle smooth muscle layer, and an inner mucosal layer. The inner mucosa contains ciliated cells that beat in the direct of the uterus, producing a current critical in moving the oocyte.

Travel of the secondary oocyte
High concentrations of estrogen occurring at the time of ovulation induce contractions of the smooth muscle along the length of the uterine tube. They occur every 4-8 seconds and the result is a coordinated movement that sweeps the surface of the ovary and pelvic cavity.
Once the oocyte-granulosa complex is pulled into the interior of the tube, muscular contractions and beating cilia move the oocyte toward the uterus. When fertilization occurs, the sperm meets the egg while it is still moving through the ampulla.
If successfully fertilized, zygote begins dividing and makes into the uterus. If not fertilized, the egg degrades.
Bacterial infections within the vagina
Sepsis is associated with STDs like gonorrhea and chlamydia.
These increase a woman’s risk for pelvic inflammatory disease (PID), infection of the uterine tubes, and other reproductive organs.
Even when resolves, PID can leave scar tissue in the tubes, leading to infertility.
Uterus definition
Muscular organ that nourishes and supports the growing embryo.
Uterus structure + cervix secretion
The portion of the uterus superior to the opening of the uterine tubes is called the fundus.
The middle section of the uterus is called the body of uterus (corpus)/
The cervix is the narrow inferior portion of the uterus that projects into the vagina.
The cervix secretes mucus that becomes thin and stringy under the influence of high plasma estrogen concentrations, which facilitate sperm movement through the productive tract.
Ligaments of the uterus
Ligaments maintain the position of the uterus within the abdominopelvic cavity.
The broad ligament is a fold of peritoneum that serves as the primary support for the uterus, extending laterally from both sides and attaching it to the pelvic wall.
The round ligament attaches to the uterine near the uterine tubes, and extends to the labia majora.
The uterosacral ligament stabilizes the uterus posteriorly by connection from cervix to pelvic wall.
Perimetrium
Perimetrium - most superficial layer (serous layer)
Consists of epithelial tissue that covers exterior portion of uterus.
Myometrium
Myometrium - middle layer, thick layer of smooth muscle responsible for uterine contractions. Most of the uterus is myometrial tissue. Has powerful contraction during labour and softer contractions to expel menstrual blood.
Endometrium + stratum functionalis function
Innermost layer of the uterus. Contains connective tissue lining (lamina propria), covered by epithelial tissue lining the lumen.
Has two layers - stratum basalis and stratum functionalis.
Stratum basalis is part of lamina propia and does not shed.
Stratum functionalis is thicker and contains glandular portion of the lamina propria and endothelial tissue lining uteral lumen.
Stratum functionalis grows and thickens in response to increased levels of estrogen and progesterone.
In the luteal phase, special branches of the uterine artery called spiral arteries supply thickened stratum functionalis. This layer provides site of implantation and is shed during menstruation.
Maintaining a thick stratum functionalis
Post-ovulatory increase in progesterone is key for maintaining a thick stratum functionalis.
If an embryo implants, signals are sent to corpus luteum to continue secreting progesterone to maintain endometrium.
If an embryo does not implant, no signals are sent to corpus luteum and it degrades, ceasing progesterone and ending luteal phase.
How does menstruation occur?
Without progesterone, the endometrium thins and because of prostaglandins, the spiral arteries of the endometrium constrict and rupture, preventing oxygenated blood from reaching the endometrial tissue.
Endometrial tissue dies and blood, pieces of endometrial tissue, and white blood cells are shed through the vagina during menstruation.
Menarche
The first menses after puberty.
The three phases of the menstrual cycle
Menses phase, proliferative phase, and secretory phase
How is cycle length determined?
Counting the days between the onset of bleeding in two subsequent cycles.
Menses phase
The phase during which the lining is shed. It averages ~5 days, it can last 2-7 days.
The menses phase occurs during the early days of the follicular phase of the ovarian cycle, when progesterone, FSH, and LH levels are low. (Basically when the corpus luteum begins to degrade).
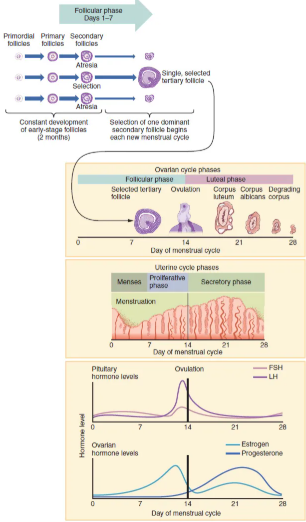
Proliferative Phase
Once menstrual flow ceases, the endometrium begins to proliferate again, marking the beginning of the proliferative phase of the menstrual cycle.
Occurs when the granulosa and theca cells of the tertiary follicles begin to produce increased amounts of estrogen.
These rising estrogen [ ] stimulate the endometrial lining to rebuild.
Ovulation occurs on day 14 (of the typical 28-day cycle). Ovulation marks the end of the proliferative phase as well as the end of the follicular phase.
Secretory phase
High estrogen levels prompt LH surge and increase uterine tube contractions to pick-up and transfer ovulated oocyte.
High estrogen levels also decrease acidity of vagina to make it more hospitable to sperm.
Luteinization of granulosa cells from collapsed follicle form corpus luteum.
Progesterone from the corpus luteum begins the secretory phase of the menstrual cycle, in which the endometrial lining prepares for implantation.
Over the next 10-12 days, the endometrial glands secrete a glycogen rich fluid. If fertilization occurs, the fluid nourish the ball of cells developing from the zygote. Spiral arteries continue to supply blood to the thickened stratum functionalis.
If no pregnancy occurs after 10-12 days, the corpus luteum degrades into corpus albicans.
Estrogen and progesterone levels fall, endometrium grows thinner, prostaglandins are secreted and constrict spiral arteries supplying blood
Endometrium dies and menses begins.