Surgery
1/126
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
127 Terms
A
C
D
What is a hernia? What are the three components of a hernia? (LA)
Protrusion of an organ or tissue through a natural or traumatic opening
Components of a hernia
Defect
Content
Sac
Internal vs external hernias? (LA)
Internal hernia
A hernia not involving the abdominal wall
Epiploic, mesenteric, diaphragmatic et al.
External hernia
The hernia content protrudes through a defect in the abdominal wall
Umbilical, scrotal, ventral, prepubic
True/false: a one finger hernia has a worse prognosis due to bowel moving in and secreting fluid (LA)
true
How should you treat an umbilical hernia? (LA)
Conservative Treatment
Manual reduction
Useful for small hernias (less than 2 fingers) with no infection
Owner is instructed to examine and reduce the hernia at once or twice daily
Hernia ring may close spontaneously
Corset
Work well in calves but not in foals
Small hernias can be the most dangerous
Ring scarification
Injection or topical application of irritant drugs
Strangulation
Devices
Elastator bands
Strangulating sutures
Hernia clamps
ONLY tiny hernias, otherwise can cause infection!!
Induce necrosis and sloughing of the hernia sac
Reserved for hernias that are <5cm, reducible and non-infected
Surgical Treatment
Indications
Large reducible hernias
Small hernias which have not responded to conservative therapy
Mandatory for treatment of strangulated or irreducible umbilical hernias
The optimal age for repair is 3-4 months
Preferably after weaning
Umbilical herniorrhaphy (open vs closed)
Umbilical resection
Indications = Umbilical infection
Pain, swelling, heat, purulent drainage on physical examination
Thickened, enlarged vessels (often with a hypoechoic center) on ultrasound examination
Patent urachus
If unresponsive to conservative therapy
3 umbilical remnants in the horse (LA)
Umbilical vein
Round ligament of the liver
Umbilical arteries
Round ligaments of the bladder
Urachus

What is a ventral hernia and its etiology? (LA)
A hernia in the abdominal wall at a site other than a natural opening
Etiology
Blunt trauma (kicks, thrusts)
Iatrogenic (incisional hernia)
The size of the defect and content vary considerably
Strangulation of contents is unusual
Timing of repair for ventral hernia (LA)
Rarely do an immediate repair - unless strangulated
Traumatic hernias
Immediate repair (within 8-12hrs of injury)
Required for strangulated hernia
Tissue damage and severe inflammatory reaction are unfavorable for healing
Delayed repair (after 6-8 weeks)
Inflammatory reaction has subsided and fibrosis at the site gives better purchase for sutures
Postoperative hernias
Repair is delayed until inflammation subsides and any infection in the wound is brought under control
Method of repair for a ventral hernia (LA)
Depends on location and size of hernia
Re-closure of fascial and muscle layers
Mesh herniorrhaphy
Large defects
Hernias with a weak hernial ring.
Use of synthetic mesh to either bridge an abdominal wall defect or to reinforce closure of a defect with sutures
Mesh may be placed deep to the body wall, superficial to the body or both deep to and superficial to the body wall
Mesh should be used only under strict aseptic conditions. Infection of the implant and formation of draining tracts is a serious complication
What is a prepubic tendon rupture and how do you diagnose it? (LA)
Prepubic tendon rupture
Usually occurs late term mares. Particularly draft breeds
Occurs rarely in cattle
Rupture may be either unilateral or bilateral
Usually preceded by severe ventral edema (differentiate from physiological edema common in late term mares)
May be avulsion of ventral musculature
Prepubic tendon rupture - diagnosis
Imminent rupture
Caudoventral abdominal edema
Pain on palpation of the caudoventral abdomen
Reluctance to move the rear limbs
Following rupture
Sagging of the caudoventral abdomen
Disruption of the prepubic tendon on rectal palpation or ultrasound
Rear limb discomfort
How do you treat a prepubic tendon rupture? (LA)
Impending rupture
Strict rest
Control of edema
Consider induced parturition
Following rupture
Prognosis for salvage of the mare is grave
Strict rest
Induced, attending foaling
Or terminal c-section
Successful
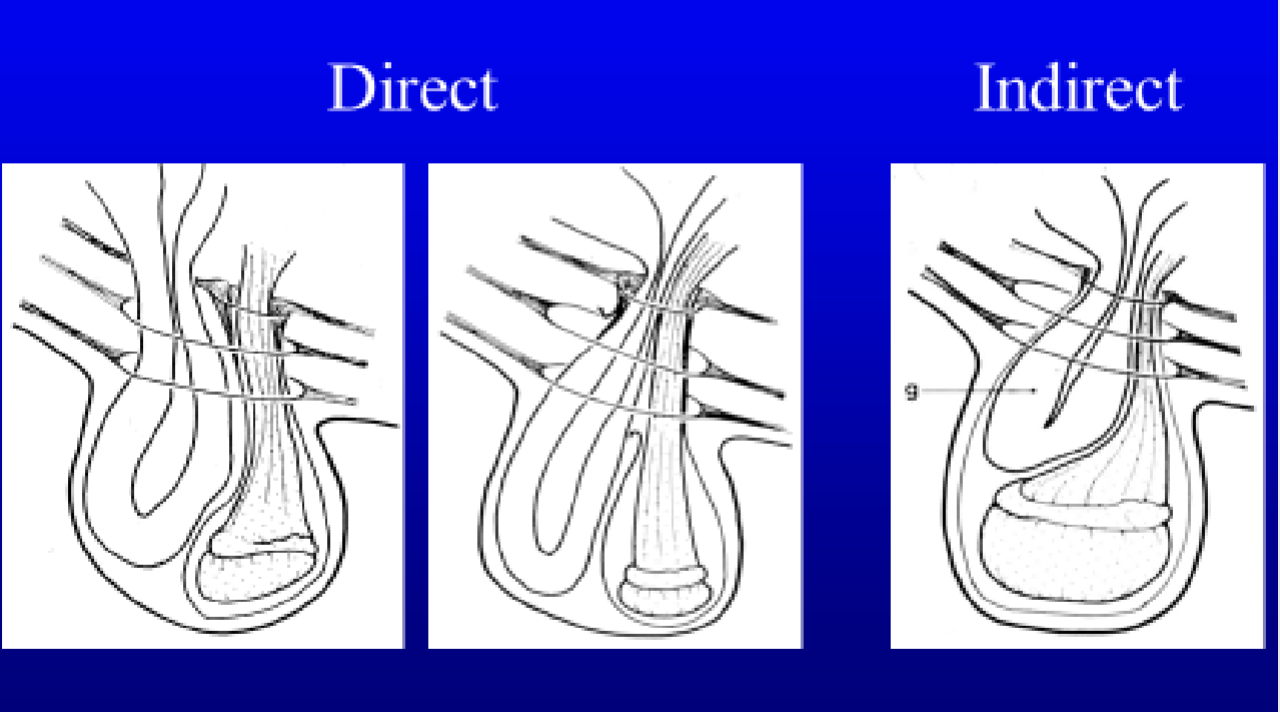
Describe a direct vs an indirect inguinal herniation. (LA)
Indirect = Intestine within vaginal tunic - adjacent to the testicle
Only so much intestine can fit in here
Vaginal tunic can rupture and become a direct hernia
Much more common
Content enters the inguinal canal via an abnormally large vaginal ring. The superficial and deep rings are normall.
Direct = direct defect in the peritoneum, intestine slipped down adjacent to the vaginal tunic = allows for more intestine to fit.
content passes through the body wall (internal oblique muscle) and into the inguinal canal
hernia content is outside the common tonic
Do umbilical hernias usually have signs in small animals?
No
True/false: umbilical hernias are not risky because there is no chance of bowel entrapment (small animals)
false!!!!!! bowel entrapment is a risk!!!!
If an umbilical hernia is soft, non-painful, and reducible, how should you approach treatment? What if it is firm, painful and associated with GI signs? (small animals)
Soft, non painful, reducible =
small ring - close at neutering if desired
large ring - have owner monitor - close at neutering.
Firm, painful, associated with GI signs = surgical emergency.
true/false: inguinal hernias are mostly seen in males (small animals)
false - 70-90% are females.
Estrus and pregnancy are risk factors
L > R
(LA) Congential inguinal hernias are almost always _______, however acquired hernias may be either indirect or direct
indirect
How do you treat a congenital scrotal hernia? (LA)
Congenital scrotal hernia - conservative treatment
Indicated for small reducible hernias in foals
Hernia is reduced at least twice daily. Close observation is mandatory to identify possible strangulation
Most congenital hernias in foals will respond to this therapy within several weeks
Heriation in newborn foals is associated with an abnormally large vaginal ring. Temporary herniation is relatively common since testicular descent is late (last trimester of gestation) and the testis is relatively large
Recommend primary closure castration when gelded
Congenital scrotal hernia - surgical treatment
Indications
Piglet and lambs
Foals
Colic due to the hernia
Exceptionally large hernias
Hernias that fail to respond to conservative therapy in timely fashion (3-4 months)
Technique = castration with a twist and tack (twist the spermatic cord about its long axis to obliterate the cavity of the vaginal tunics and anchored it to the superficial inguinal ring using a transfixing ligature)only works on indirect hernias
True/false: you diagnose a stallion with an acquired inguinal/scrotal hernia. Treatment is rest and monitor.
NOOOOOOOO!!! It is a surgical emergency!!!!!
Herniorrhaphy with castration
Resection of damaged intestine or
Laparoscopy (it may be possible to save the testicle if it is not compromised)
C
F
a 7/o male intact lab undergoes negative abdominal exploratory. Locoregional anesthesia not provided. Which opioid is best for pain management post op?
hydromorphone
buprenorphine
tramadol
butorphanol
hydromorphone
Function of the skin
Protection
Regulation
Sensation
Immunosurveillance
Scalpel vs electrocautery vs laser
Longer healing time using laser vs. scalpel
Reduced inflammation and bleeding when using electrocautery than with scalpel
Phases of Wound Healing
Inflammation
Tissue formation
Remodeling
Describe the inflammation phase of wound healing
Begins with platelets - activate and degranulate
Potent callout for neutrophils
Neutrophil migration into wound bed peak at ~48hrs
Clean up agent (using NETS)
Looking for bacteria
Looking for ROS
Releases cytokines to set up stage for next phase
Associated with swelling, redness, pain, heat
Calls in macrophages - inflammatory to regenerative
Describe the tissue formation phase of wound healing
Defined by macrophages (architects)
Tissue formation (beginning of granulation tissue) 3-5 days dog, 5-6 days cat
Angiogenesis
Fibroblasts
Clinical implication
Angiogenesis = immature leaky vessels (clear fluid in wound - normal)
Fresh granulation bed = exudative wound
Wound fluid rich in cytokines and MMPs - can inhibit healing = frequent dressing changes
Want fluid to leave (keep wound dry) = cytokine soup = inhibits regeneration
Good granulation tissue = healthy wound, OK to close
Absence of granulation tissue in an open wound by 3-5 days (dogs) or 5-6 days (cats) signals a problem
Excess necrotic tissue
Contamination
Poor perfusion
Infection
Poor patient health
Describe a clean wound
Surgical wound made under conditions of asepsis
ABX prophylaxis not required unless implants used/extended surgical time/break in asepsis
Describe a contaminated wound
Open traumatic wound
Wounds made with a major break in sterile technique eg spillage of GI contents
ABX prophylaxis required
Describe a dirty/infected wound
>10^5 bacteria per gram of tissue
Clinically exhibits heat, pain, swelling, redness, and discharge
Therapeutic abx required
Purulent necrotic wound
Established peritonitis
Descibe a clean contaminated wound
Surgical wound under conditions of asepsis but during which respiratory, urinary, or alimentary tract is entered (this is on purpose)
Abx prophylaxis required
How does wound classification dictate wound management
Heavy contamination/established infection/necrotic tissue = period of open wound management prior to closure
Minimally contaminated traumatic wound or clean surgical wound = can be closed immediately
Describe primary closure
One stage surgical closure
Success depends on
Good perfusion to wound bed and skin margins
Minimal exudate production
Ability to remove all foreign material from wound
Absence of any necrotic tissue
Minimal to no tension
Restricted to clean, clean-contaminated and contaminated wounds where contamination can be managed
If dehisces - you got it wrong
Describe delayed primary closure
Wound is managed open until a healthy granulation bed has formed, then close
Best method where
Wound viability is questionable
Limited tissue available if prematurely closed wound dehisces
Describe second intention healing
Wound managed open as it granulates, contracts, and epithelializes all the way to closure without surgical intervention
Patient factors that inhibit wound healing
Diabetes mellitus - impaired macrophage function
HAC
FIV
Steroids
Chemotherapy
Severe anemia
Poor nutritional status
Hypotension under GA
Hypothermia under GA
Length of time under GA
Species = cats
Wound factors that inhibit wound healing
Tension = poor found perfusion
High mobility area
Pressure points = point of elbow/hock
Radiation site
Highly productive wound
Excessive suture material in wound bed
Presence of foreign material or necrotic tissue
Active vs passive drains. Function? When to place? Complications?
Active
Jackson pratt
Active suction
Passive
Penrose
Relies on gravity
Functions
Eliminate dead space
Remove excess fluid-macrophages don't swim
When to place
At the time of surgical closure of healthy wounds where
Wound is exudative
When dead space can’t be effectively managed by other means (suture/bandages)
To manage a deep abscess (closed suction only)
Complications
Foreign material in wound increases risk of dehiscence
potential for ascending bacterial infection
Potential for drain material to be accidentally retained in wound
Drain principles
Drain should not exist through the primary incision
For passive drains, exit point must be gravitationally dependent and amenable to aseptic management with bandaging
In the case of the abdominal cavity, closed suction drains ONLY
Avoid in oncologic surgery - they expand the surgical margin
Use the smallest number of drains and size of drain possible
Use active closed suction drains instead of passive where possible
Remove the drain as soon as possible - typically 2-4 days
Penrose drains
Only exist through ONE hole
Don’t make exit point too tight
No sutures anchoring drain in wound bed
Don't - suture at both ends, fenestrate the drain, make the exit hole too small.
Basic wound management
wear gloves
apply sterile water/soluble gel to wound surface
clip local area generously
lavage
± debride
± forage exposed bony surfaces
wound ready for closure.
Difference between primary closure, delayed primary closure, and second intention healing
Primary closure - minimal contamination, no necrotic tissue remaining and little likelihood of late onset necrosis
Delayed primary closure - manage open until good granulation coverage signals a healthy wound - then close
Second intention healing - managed with bandaging until the wound contracts and epithelialized without surgical intervention - can be lengthy - typically reserved for small wounds or wounds with minimal available soft tissues to mobilize
Incidence of bandage injuries? Generally traced to what?
Bandage injuries
60% incidence - of which 40% mild, 10% moderate, 10% severe
Can generally be traced to:
Insufficient padding
Too long between bandage changes
Bandage allowed to become wet
Bandage too tight
Poor bandage technique
Toes left out
No allowance made for flexion of limb
Poor owner communication
Poor staff training or inappropriate task delegation
Ehmer sling - closed reduction of hip luxation. 50% incidence of soft tissue wounds, 18% severe
How to prevent bandage injuries
Written and verbal owner instructions
Written instructions signed by owner to acknowledge receipt
Restricted activity
Warning re potential for serious bandage injury
Instruct to re-present patient immediately if:
Bandage wet, soiled, or slipping
Patient chewing at bandage
Patient becomes lame or stops using limb
If can’t re-present immediately then remove bandage
Indications and goals of bandaging.
Indications to bandage
To support/protect a surgical incision
To manage a contaminated traumatic wound until wound is suitable for delayed primary closure
To manage a wound to closure by second intention
Goals
To maintain an optimal environment for wound healing
Mechanically stable
moist
Protected
What do bandages consist of?
Contact layer
Absorptive layer
(splint)
Outer layer
Bandages - Contact layer for minimal/moderately contaminated wound prior to granulation tissue formation
Alginate dressings
Soluble - forms a gel trapping contaminants and bacteria
Non-traumatic
Moist
Bandages - Contact layer for heavily contaminated/necrotic/infected wound prior to granulation tissue formation
Honey soaked sterile gauze
Saline soaked lap sponges - “wet to dry”
Sugar under lap sponges
But these dressings are traumatic and termed DEBRIDEMENT DRESSINGS
Bandages - contact layers for granulating wound
Post formation of granulation tissue
Non-debridement dressing
hydrocolloid/hydrogel under non-adherent semi-occlusive dressing
Foam dressings eg mepilex
NOT telfa alone on an open wound - trying to avoid any dessication
Only useful for healing surgical incisions in first 6-12hr window
No absorption, fall off easily
Bandage change frequency
Debridement dressing - Q6-24hrs depending on fluid production
Non-debridement dressing (alginate/foam type Q2-4days)
Change as soon as there is any strike through
Adjust frequency of changes to wound appearance and the state of the contact layer at each change
If $$$ is a problem - better to improvise with materials than compromise on frequency
How does honey work on wounds?
Hyperosmolarity results in bacterial kill
Antioxidants
Protects against free radicals
Chelates iron, preventing bacterial growth
Peroxidases contained in unpasteurized honey
Acidity
pH 3.6-5.0
Promotes healing
Antimicrobial
Viscous barrier to wound invasion
Cheap and readily available
No drug resistance recorded
local honey
Purpose of absorptive layer when bandaging
Absorbs exudate
Distributes bandage pressure
$$$
True/false: superficial wound cultures are usually helpful when determining wound management
False - All open wounds contain bacteria, often a mix of species
Superficial wound cultures are rarely indicated/helpful
Systemic abx for open chronic wound management are indicated when:
Acute traumatic wound
The patient has systemic signs of infection
There is evidence of
Abscess
Cellulitis >1cm beyond wound margin (get culture from here)
Osteomyelitis
Lymphangitis
Not needed if:
Mild, local inflammation
Healthy granulation tissue covering full wound bed
Common causes of delayed second intention healing
Excess bandage pressure-insufficient padding
Excess time between bandage changes
traumatic/desiccating contact layer
Excess tension - poor availability of surrounding tissues limits contraction
Poor wound vascularity - bony surfaces
Halsted’s principles
Strict aseptic technique
Gentle tissue handling
Meticulous hemostasis
Preservation of blood supply
Obliteration of dead space
Accurate apposition of tissue planes minimization of tension on tissues
True/false: Undermining and walking sutures will close 90% of wounds that are NOT on a distal extremity
true
Which part of the body would you use a free graft for? Describe the biology of a free graft.
Distal limb
How to close a wound under tension?
Walking sutures
Tension suture
Dermis to fascia
PDS
Do not compromise blood supply, however skin sutures under tension will compromise blood supply and cause necrosis
Multiple releasing incisions for distal extremity wounds
Single releasing incision allowing skin to be mobilized and re-positioned to close a non-healing wound over a pressure point
Local flaps rely on…
local perfusion - no specific arterial supply.
Used for head neck and trunk
A caudal epigastric flap is an example of an _________.
axial parttern flap - used for head neck and trunk
What is a hernia?
A condition in which a part of an organ is displaced and protrudes through the wall of the cavity containing it
Contains a ring, sac, and contents.
What does a false hernia lack?
no epithelial lined sac.
Pathophysiology of a hernia
Loss of domain
Incarceration
Adhesions
Normal function may be impeded
Strangulation
Blood supply compromised
Venous obstruction = congestion + transudate
Surgical emergency
Describe an umbilical hernia (SA)
Common
Congenital and heritable
May have concurrent
Cardiac defects
Incomplete caudal sternal fusion
Cryptorchid
PPDH
Clinical signs rare
May spontaneously resolve by 6 months of age
Risk of bowel entrapment - see less often b/c small, but is a big problem.
Elective umbilical hernia repair (SA)
Male - separate surgical incision
Female - incorporate into spay incision
Procedure
Careful skin incision over hernia
Dissect skin off of underlying tissue
Reduce or excise fat to expose ring
Close ring using PDS or similar.
When is an umbilical hernia an emergency in small animals?
Intestinal adhesions
Intestinal necrosis
Septic abdomen
The inguinal canal contains
Genital structures
Vaginal process
Spermatic cord (males), round ligament (females)
Genitofemoral artery, vein, nerve
External pudendal vessels
Describe inguinal hernias in SA (signalment, risk factors). How to diagnose?
70-90% female - often see the uterus. Problematic (strangulation, pyometra)
Estrus and pregnancy are risk factors
L>R
Diagnose - palpation, rads/ultrasound
Surgical approach for inguinal hernia
Multiple approaches
Over the hernia
Abdominal - easier to pull things back in through the abdomen. Helps if need to perform RNA
Inguinal hernia surgery
Caudal midline laparotomy
Identify and reduce herniated structures to abdominal cavity
Increase hernial ring size if necessary
Check viability of all reduced tissue
Close inguinal ring
Important points
When closing the inguinal ring be careful of normal structures
Males: spermatic cord (with the genital branch of the genitofemoral nerve), ilioinguinal nerve, external pudendal vessels (a and v)
Females: round ligament, genital branch of the genitofemoral nerve, and the ilioinguinal nerve, external pudendal vessels (a & v)
Always check the other side
If not reducible - dissect skin/mammary tissue laterally and caudally to expose hernia contents
What is a scrotal hernia?
Variant of an inguinal hernia
Viscera pass through internal inguinal ring. Inguinal canal, and external inguinal ring to end up in the scrotum
Rare
Often concurrent strangulation
Chondrodystrophoid and brachycephalics
How does surgery differ for a reducible vs non reducible scrotal hernia?
Reducible or non-reducible?
reducible
Prescrotal incision running parallel to midline
Reduce and close external inguinal ring-partially if remaining intact, fully if neutering.
Non-reducible
Caudal midline laparotomy +/- = approach internal and external inguinal rings
Reduce hernial contents and evaluate viability
Abdominal wall ruptures are often caused by ________ therefore you must rule out concurrent ___________.
Polytrauma
Rule out concurrent
Pneumothorax
Pulmonary contusions
V-tach
uroabdomen/hemoabdomen
Bile peritonitis
Describe the surgery for Abdominal wall ruptures, prepubic tendon avulsion/rupture and thoracic wall ruptures
Abdomen
Approach via midline laparotomy
Care re aorta/ureters for repair of dorsolateral ruptures
In general
Fascia
Multiple layer
Pre-place sutures
2/0 PDS
Prepubic tendon avulsion/rupture
Pubis periosteum
Pre-drill holes in pubic brim
Non-absorbable suture
Thoracic wall ruptures
May be no external punctures, but total loss/ separation of underlying thoracic wall musculature with rib separation/fracture and lung herniation
When exploring be prepared
Chest tube
PPV
Lung lobectomy.
Pathophysiology of diaphragm hernias
Pathophysiology Polytrauma
Thoracic and abdominal pressures equalise
Loss of domain
Reduced tidal volume
Atelectasis
VQ mismatch
Impaired venous return
During induction - place them head up! Uses gravity to make sure things go into the abdomen, or if they are there we want them to stay there
incarceration/strangulation
Stomach
Liver lobe
Intestine
true/false: a gastric hernia is a true surgical emergency
true - stomach fills with gas.
Intubation, positive pressure ventilation, orogastric decompression, surgery
Clinical signs of diaphragmatic hernias
dyspnea
Decreased lung sounds
Asynchronous respiratory pattern - on inspiration thoracic wall moves out and abdominal wall moves in
Surgery for diaphragmatic hernia
Immediate PPV
Head up position
Midline laparotomy
Gentle traction to reduce organs
Enlarge defect if necessary
Before closing defect place small bore chest tube under direct palpation
Seldinger technique
Post-op considerations and complications of diaphragmatic hernias
Post op
May remain O2 dependent for 24-48hrs
Aspirate chest tube Q4
IV fluid support
Opioid analgesia
Early feeding
Complications
Chronic
Intra-thoracic adhesions
Re-expansion pulmonary edema
Abdominal compartment syndrome = chronic ruptures - rare - bogota bag.
Peritoneopericardial diaphragmatic hernia (PPDH)
Congenital
Pericardial sac connects with abdominal cavity
Frequently asymptomatic until
GI obstruction
Cardiac tamponade.
Often concurrent with
Umbilical hernia
Caudal sternal defect-xiphoid absent
Identified at spay
Surgery
Evacuate pericardial sac
Liver lobe herniation and necrosis
Complex
Surgical asepsis
Complete absence of contamination by pathogenic organisms
Prevents wound contamination by pathogenic organisms
Patient
OR personnel
Environment
_% of small animal surgical patients develop post-op wound infection
5%
Progression of surgical wound to infection depends on:
Which is most important?
Microbial pathogens - most important
Local wound environment
Host defense mechanisms
Infection will develop if >___bacteria/gram of tissue
Dependent on
10^6
dependent on:
Duration
For every hour of surgical time, infection rate approximately doubles
Type of procedure (degree of operative contamination)
Clean: 2.5-6%
Clean-contaminated: 2.5-9%
Contaminated: 5.5-28%
Dirty: 18-25%
Clean orthopedic procedures have higher infection rates than clean soft tissue procedures
Sources of microbial pathogens
Endogenous
Within patient
Site-specific
Exogenous
Air, surgeons, instruments, etc
Generally implicated in surgical infections (along with transient patient flora)
Direct transfer
Blood, lymphatics, IV drugs, distant infection.
What is generalized pyoderma?
Elective procedures should not be performed if multiple skin lesions present: lesions likely contain bacteria that could contaminate the surgery site and/or incision = generalized pyoderma
Presurgical skin prep
Humans - presurgical bathing conflicting results
Highest reduction of microbial counts when performed several times prior to surgery and with 4% chlorhexidine gluconate instead of other medicated soaps
Veterinary - data not available
Prewash surgical site with a neutral, non-medicated soap is advised to start surgical antisepsis of the area
Veterinary patients do not dry - so don’t wash unless farm animals etc.
Purpose: remove transient microorganisms and reduce resident flora for duration of surgery
Clipping: within 4 hours of surgery = associated with lower incidence of surgical site infection
Preservation of the integrity of the natural skin barrier is key to reducing surgical site infection
Use least traumatic method (no razors): rashes and skin abrasions induced by shaving and clipping can provide a portal or entry for microorganisms
It is better to leave some hair than to give an animal clipper burn
Antiseptic application
Scrub, paint, or spray equally control bacterial growth
Povidone Iodine
More skin reactions including acute contact dermatitis (eye, prepuce)
4% chlorhexidine rinsed with saline or 70% isopropyl alcohol
Combination with 70% isopropyl alcohol may result in higher residual antimicrobial activity7
CHXD 1% and 4% are effective
CONTACT TIME!!!
Single step process - faster and has been found to be equally effective sa the use of multiple soaps
Alcohol based iodophor and chlorhexidine products seem to exhibit greater efficacy compared to the aqueous solutions
Describe how to drape your surgical patient
Blood and fluid resistant
Lint free, antistatic, able to maintain isothermic environment relative to patient
Single-use disposable drapes: low cost and benefit in preventing SSI outweigh the use of reusable drapes
Steps
Quarter drapes
Ideally disposable
Penetrating towel clamps
Second drapes
Should extend onto instrument table (which is first covered with its own drape
Clamps should not penetrate to deeper layers
Ioban 2 self adhesive drapes
Sterile, waterproof, transparent and available with infused antimicrobial agents, typically an iodophor
Use of these with abbreviated skin preparation techniques is not superior to use of nonadhesive drapes
Nonmedicated adhesive incise drapes should not be used because of their association with increased risk for surgical site infection
What is the primary source of surgical contamination
Shedding OR personnel is primary sources of contamination = perineal area
Closely weaved fabric decreases degree of bacterial dissemination, but overall effect of scrub suits on the environment is questionable - scrub suit with elastic cuffs or other occlusive seals better
Routine laundering does little to decrease pathogenic bacteria on scrub suits
Just a barrier
Tuck top into pants
No undershirts showing
Tuck pants into socks
Purpose of pre surgical hand prep
Hand hygiene is major deterrent for hospital acquired infections
Purpose - remove and/or kill transient skin organisms and reduce resident microbiota for duration of the surgical procedure
Transient microbiota: colonize the superficial layers of the skin, easier to remove with hand washing, most common cause of surgical site infection
Resident microbiota: reside in the deeper layers of the skin, are more difficult to remove, considered to be less pathogenic on intact skin
Ultimate goal: risk reduction for surgical site infections
Methods of hand prep
Waterless
Hand washing increases prep time, cost, carbon footprint, water usage
Faucets common sources of pseudomonas spp and other gram negative bacteria
Alcohol based hand rub is superior
The initial reduction of the resident skin flora (microbiota) is rapid and effective with alcohol-based hand rubs (bacterial regrowth to baseline values on the gloved hand takes more than 6 hours)
Sublingual area is reported to have highest bacterial load despite hand scrubbing
true/false: Gown contamination in both open and closed technique 100% of the time, particularly around the cuff site, whereas no contamination patches were found when the assisted gloving technique was used.
true
which side is easier to ligate the vascular pedicle?
left - more caudal
leaves of the suspensory ligament
Medial leaf = ipsilateral kidney
Lateral leaf = bodywall at last rib
Describe feline spay flank approach
Occasionally performed in a flank approach
Landmarks - position in lateral with hindlimbs pulled caudally. The point of incision is the third point of an equilateral triangle created by the femoral head and the iliac crest
Flank approach vs midline - more painful at 1 hour post op and discharge and less painful at 3d and 10d post op
See notes in powerpoint
Presentation and pathophysiology of pyometra
Presentation
4-10weeks post estrus (8yrs, nulliparous, large breed)
Depression, anorexia, vomiting, PU/PD
Purulent vaginal discharge in 75% = “open pyo”
Pathophysiology
Endometrial hyperplasia, secondary infection E. coli
“Stump” pyometra can occur in spayed females, but concurrent with an ovarian remnant/exogenous progestogens
Septicemia, ADH antagonism by endotoxin
Obligate polyuria, sepsis -> severe dehydration, pre-renal azotemia, shock
NOT kidney disease = kidney can’t concentrate due to endotoxin.
How does a spay differ if the animal has a pyometra?
Long midline incision
Fully exteriorise uterus
Gentle handling - can rupture
Three clamp ligation technique ovarian pedicles
Uterine vessels very prominent
Ligate each individually
Encircling ligature (Millers) below
Don't oversew uterine stump
Lavage abdomen with saline prior to closure
Same approach with spay during C section