Sepsis, SIRS, MODS Papers
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
47 Terms
ARISE Investigators and ANZICS Clinical Trials Group, 2014
Goal-Directed Resuscitation for Patients with Early Septic Shock
Objective: To test the hypothesis that EGDT, as compared with usual care, would decrease 90-day-all-cause mortality among patients presenting to the emergency department with early septic shock in diverse health care settings
Results:
Of the 1600 enrolled patients, 796 were assigned to the EGDT group and 804 to the usual-care group
Primary outcome data were available for more than 99% of the patients
The lungs and urinary tract were th emost common locations of infection
Patients in the EGDT group received a larger mean volume of intravenous fluids in the first 6 hours after randomization than did those in the usual care group (1964 vs 1713 ml) and were more likely to receive vasopressor infusions (66.6% vs 57.8%), red cell transfusions (13.6% vs 7.0%) and dobutamine (15.4% vs 2.6%)
At the end of the 6 hour intervention period, the mean arterial pressure was higher in the EGDT group than in the usual-care group (76.5 mmHg vs 75.3 mmHg)
Other physiological and laboratory values were similar
At 90 days after randomization, 147 deaths had occurred in the EGDT group and 150 had occurred in the usual-care group for rates of death of 18.6% and 18.8%, respectively
There was no significant difference in survival time, in hospital mortality, duration of organ support, or length of hospital stay
Conclusion: In critically ill patients presenting to the emergency department with early septic shock, EGDT did not reduce all-cause mortality at 90 days
Khanna et al, 2017
Angiotensin II for the Treatment of Vasodilatory Shock
Objective: To determine whether the addition of angiotensin II to background vasopressors would improve blood pressure in patients with catecholamine-resistant vasodilatory shock
Results:
A total of 344 patients were assigned to one of the two regiments; 321 received a study intervention (163 received angiotensin II and 158 received placebo) and were included in the analysis
The primary end point was reached by more patients in the angiotensin II group (69.9%) than in the placebo group (23.4%)
Most common reason in both groups for lack of response was failure to achieve a mean arterial pressure of at least 75 mmHg or an increase of at least 10 mmHg (the other reason was an increase in the dose of background vasopressors)
During the first 48 hours, mean doses of background vasopressors were consistently less in the angiotensin II group than in the placebo group
At 48 hours, the mean improvement in the cardiovascular Sequential Organ Failure Assessment (SOFA) score (scores range from 0-4, with higher scores indicating more severe dysfunction) was greater in the angiotensin II group than in the placebo group
In multivariate analysis, treatment assignment (angiotensin II vs placebo) was the most significant positive predictor of a response with respect to mean arterial pressure
Significant negative predictors were hypoalbuminemia and elevated vasopressor dose
Serious adverse events were reported in 60.7% of the patients in the angiotensin II group and 67.1% in the placebo group
The most common adverse events leading to discontinuation were similar in the two treatment groups and included septic shock, multiorgan failure, cardiogenic shock, and cardiac arrest
Death by day 28 occurred in 75 of 163 patients (46%) in the angiotensin II group and in 85 of 158 patients (54%) in the placebo group
Conclusion: Angiotensin II effectively increased blood pressure in patients with vasodilatory shock that did not respond to high doses of conventional vasopressors
Seymour et al, 2017
Time to Treatment and Mortality during Mandated Emergency Care for Sepsis
Objective: Using data from New York, where hospitals are required to implement protocols and report on the treatment of sepsis, examined the association between the timing of treatment and risk-adjusted mortality
Results:
Among 49,331 patients at 149 hospitals, 40,696 (82.5%) had the 3 hour bundle completed within 3 hours
The median time to complete of the 3 hour bundle was 1.30 hours, the median time to the administration of antibiotics was 0.95 hours, and the median time to complete of the fluid bolus was 2.56 hours
Among patients who had the 3 hour bundle completed within 12 hours, a longer time to the completion of the bundle was associated with high risk-adjusted in-hospital mortality as was a longer time to the administration of antibiotics, but not a longer time to the completion of a bolus of intravenous fluids
In a multivariable model, each hour of time to the completion of the 3 hour bundle was associated with higher mortality (odds ratio of death until completion of 3 hour bundle, 1.04 per hour)
Patients who had the bundle completed during hours 3 through 12 had 14% higher odds of in-hospital death than patients in whom all three items in the 3 hour bundle were completed in 3 hours
Patients who received antibiotics in hours 3 through 12 had 14% higher odds of in-hospital death than those who received antibiotics within 3 hours
Associations appeared to be stronger among patients receiving vasopressors than among those who were not receiving vasopressors
On average, the completion of the 3 hour bundle at 6 hours was associated with mortality that was approximately 3 percentage points higher than the mortality associated with completion of the bundle within the first hour
Conclusion: More rapid completion of a 3 hour bundle of sepsis care and rapid administration of antibiotics, but not rapid completion of an initial bolus of intravenous fluids, were associated with lower risk-adjusted in-hospital mortality
Whiles et al, 2017
Increased Time to Initial Antimicrobial Administration is Associated with Progression to Septic Shock in Severe Sepsis Patients
Objective: To determine if time to initial antimicrobial is associated with progression of severe sepsis to septic shock
Results:
Identified 3,929 severe sepsis patients with overall mortality 12.8%
984 patients (25%) progressed to septic shock
The median time to antimicrobial was 3.77 hours in those who progressed versus 2.76 hours in those who did not
Multivariate logistic regression demonstrated that male sex, Charlson Comorbidity Index, number of infections, and time to first antimicrobial were associated with progression
Each hour until antimicrobial administration was associated with a 8.0% increase in progression to septic shock
Additionally time to broad-spectrum antimicrobial was associated with progression
Time to initial antimicrobial was also associated with in-hospital mortality
Conclusion: This study emphasizes the importance of early, spectrum antimicrobial administration in severe sepsis patients admitted through the emergency department, as longer time to initial antimicrobial administration is associated with increased progression of severe sepsis to septic shock and increased mortality
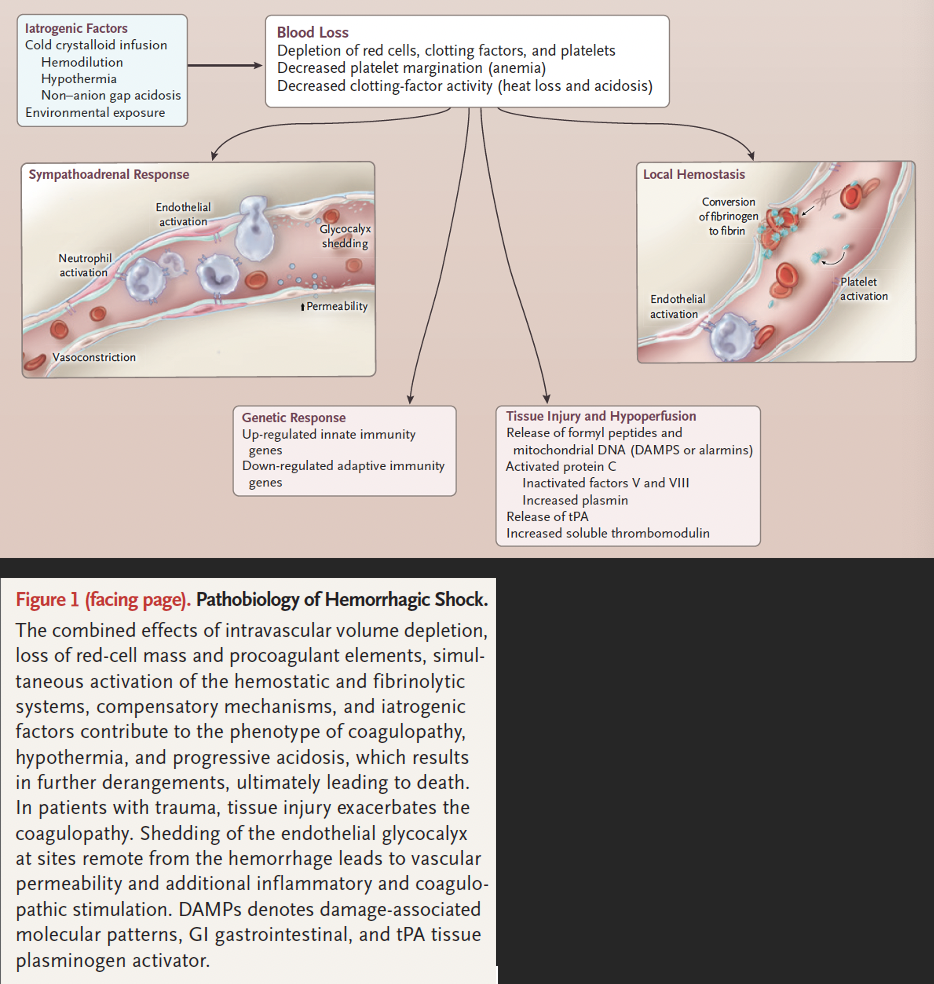
Hemorrhagic Shock
A form of hypovolemic shock in which severe blood loss leads to inadequate oxygen delivery at the cellular level
Pathobiology of Hemorrhagic Shock - Cellular Level
At the cellular level, hemorrhagic shock results when oxygen delivery is insufficient to meet oxygen demand for aerobic metabolism
Delivery-dependent state → cells transition to anaerobic metabolism
Lactic acid, inorganic phosphates, and oxygen radicals start to accumulate
Release of DAMPs incites a systemic inflammatory response
As ATP supplies dwindle, cellular homeostasis fails → necrosis, apoptosis, necroptosis
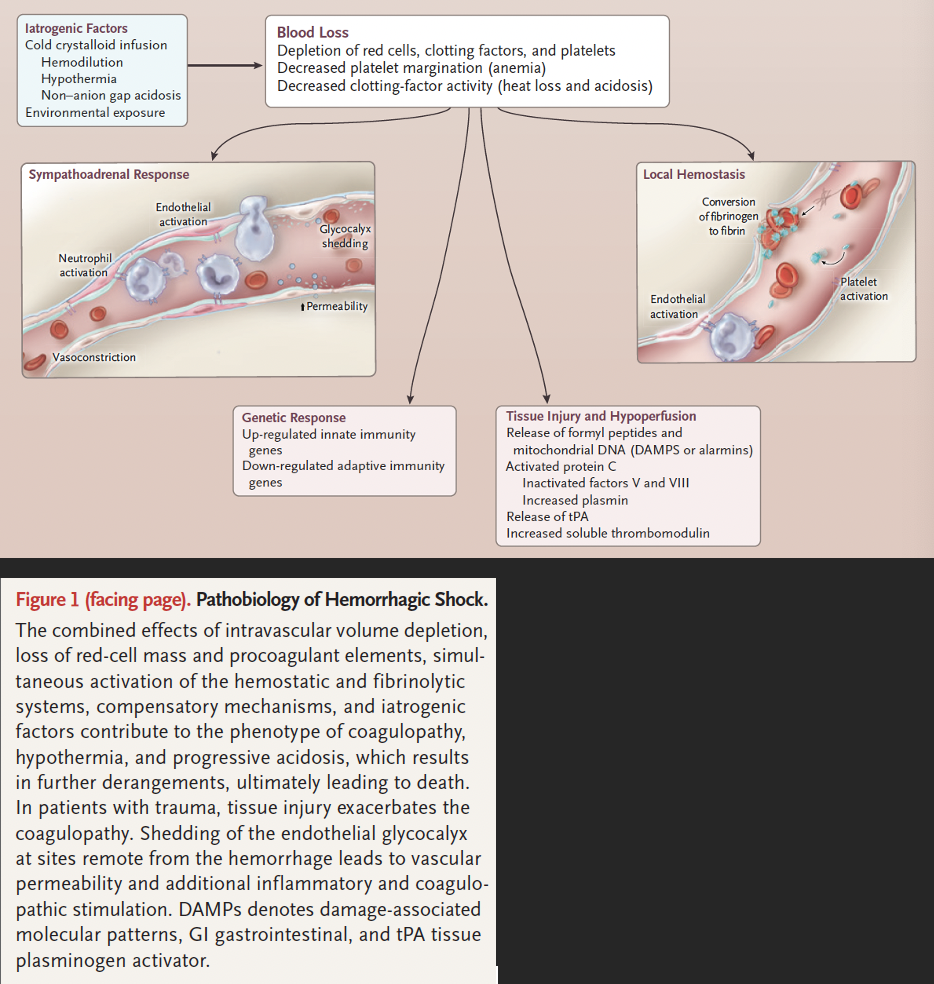
Pathobiology of Hemorrhagic Shock - Tissue Level
Hypovolemia and vasoconstriction cause hypoperfusion and end-organ damage in the kidneys, liver, intestine, and skeletal muscle, which can lead to multiorgan failure
In extreme hemorrhage with exsanginuation, pulselessness results in hypoperfusion of the brain and myocardium, leading to cerebral anoxia and fatal arrhythmias within minutes
At the site of hemorrhage, the endothelium and blood act synergystically to form a thrombus
Oxygen debt and catecholamine surge eventually induce an endotheliopathy through shedding of the glycocalyx
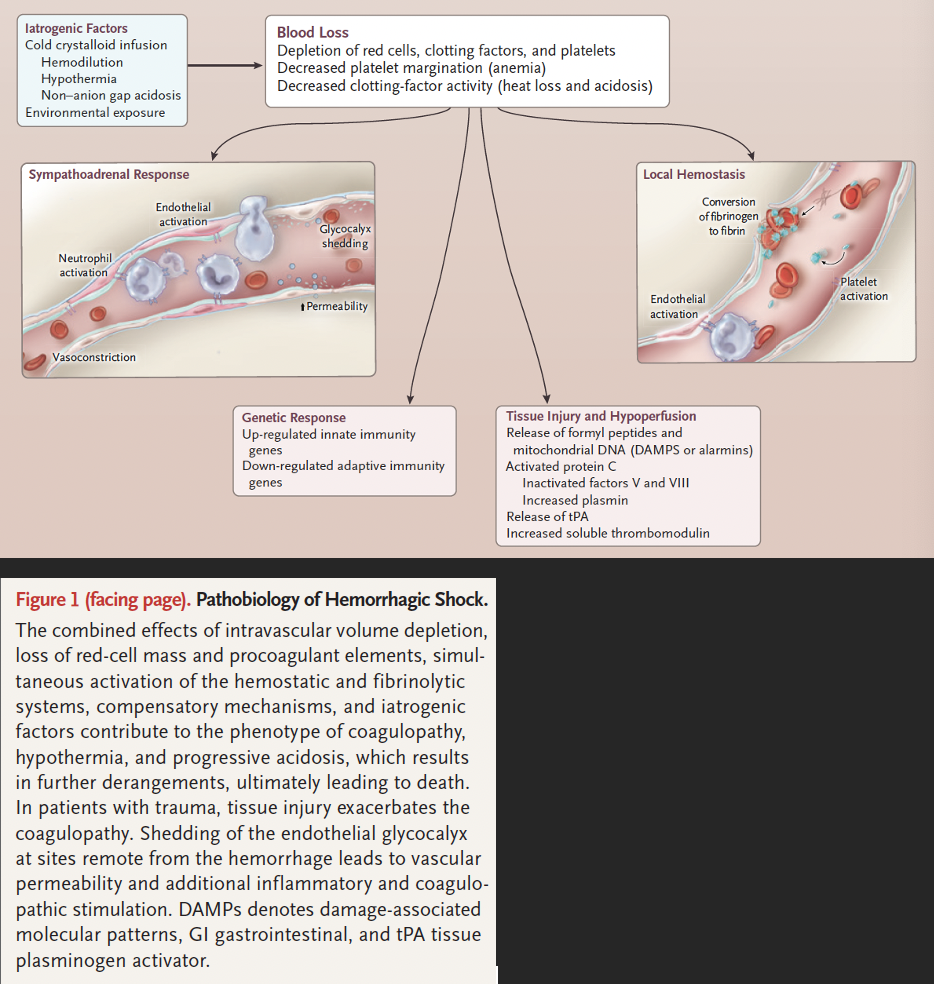
Pathobiology of Hemorrhagic Shock - Level of the Blood
At the site of hemorrhage, the clotting cascade and platelets are activated, forming a hemostatic plug
Remote from the site of hemorrhage, fibrinolytic activity increases
Excess plasmin activity and autoheparinization from glycocalyx shedding can result in pathologic hyperfibrinolysis and diffuse coagulopathy
Depleted platelets, decreased platelet margination due to anemia, and reduced platelet activity also contribute to coagulopathy and increased mortality
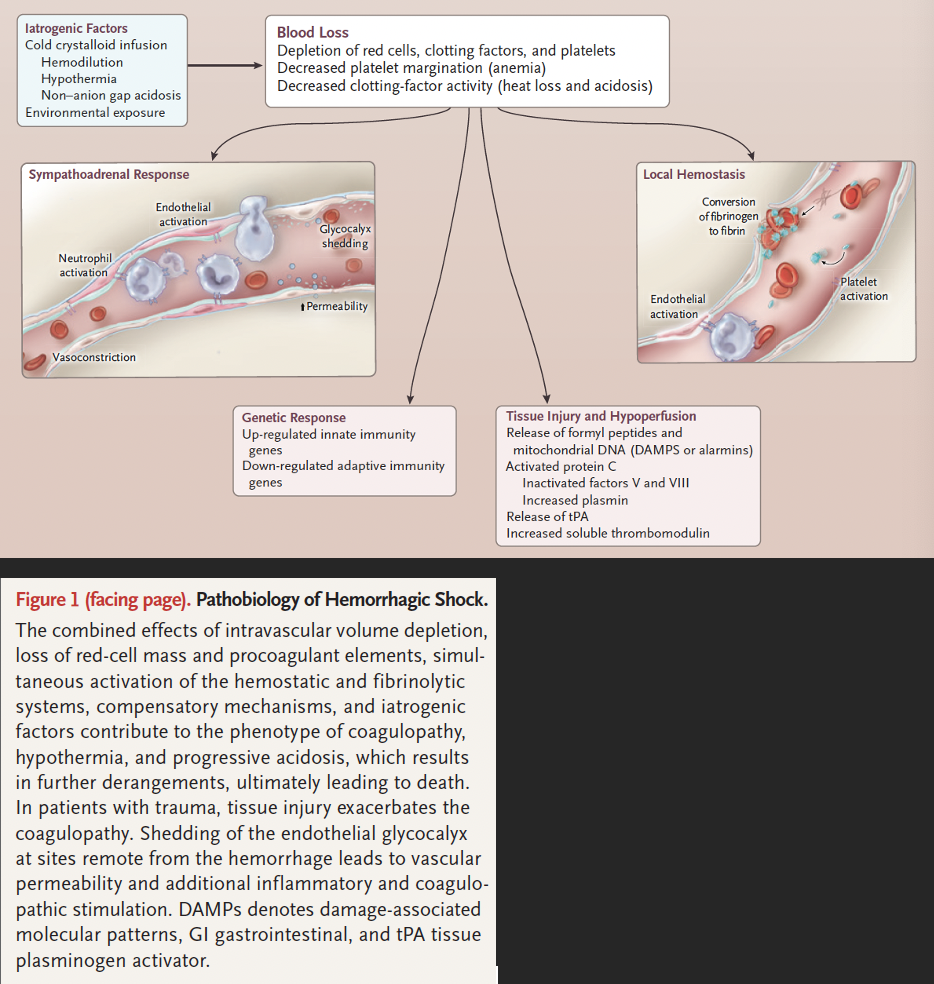
Iatrogenic Factors that can Exacerbate Coagulopathy in Patients with Active Bleeding
Overzealous resuscitation with crystalloids dilutes the oxygen carrying capacity and clotting factor concentration
Cold fluids exacerbates heat loss from hemorrhage, depleted energy stores, and environmental exposure and leads to decreased function of the enzymes in the clotting cascade
Overadministration of acidic crystalloids worsens the acidosis caused by hypoperfusion and further impairs the function of clotting factors
Prehospital Care for Hemorrhage
Minimize further blood loss
Tourniquet application proximal to sites of hemorrhage in the extremities if the patient is rapidly transported
For bleeding wounds in junctional areas where a tourniquet can’t be applied, apply a hemostatic dressing
Provide limited fluid resuscitation
Rapidly transport to a facility that can provide definitive care
Principles of Damage Control Resuscitation in People
Avoid or correct hypothermia
Apply direct pressure or a tourniquet proximal to sites of hemorrhage in the extremities; pack junctional wounds with hemostatic dressings
Delay fluid administration until the time of definitive hemostasis in selected patients (those with penetrating trauma to the torso and short prehospital transport times)
Minimize crystalloid infusions (<3 L in the first 6 hours)
Use a massive-transfusion protocol to ensure that sufficient blood products are rapidly available
Avoid delays in definitive surgical, endoscopic, or angiographic hemostasis
Obtain functional laboratory measures of coagulation (e.g. by means of thromboelastography or rotational thromboelastometry) to guide the transfusion from empirical transfusions to targeted therapy
Drewry et al, 2017
Antipyretic Therapy in Critically Ill Septic Patients: A Systematic Review and Meta-Analysis
Objective: To examine the impact of antipyretic therapy on mortality in critically ill septic adults
Results:
Antipyretic therapy did not reduce 28 day/hospital mortality in the randomized studies or observational studies
Early mortality was significantly lower in patients treated with antipyretic therapy in randomized studies
Fever treatment blunts the immunologic benefit of hyperthermia leading to increased nosocomial infections later in the hospital course
Shock reversal and acquisition of nosocomial infections were also unchanged
Antipyretic therapy decreased body temperature, but not heart rate or minute ventilation
Conclusion: Antipyretic treatment does not significantly improve 28 day/hospital mortality in adult patients with sepsis
Putzu et al, 2019
The Effect of Vitamin C on Clinical Outcome in Critically Ill Patients: A Systematic Review With Meta-Analysis of Randomized Controlled Trials
Objective: To assess the effect of vitamin C administration on major clinical outcome in ICU or cardiac surgery patients
Results:
In ICU patients, vitamin C administration was not associated with a difference in mortality, acute kidney injury, ICU or hospital length of stay compared with control
In cardiac surgery, vitamin C was associated to a reduction in postoperative atrial fibrillation, ICU stay, and hospital stay
No differences in postoperative mortality, acute kidney injury, stroke, and ventricular arrhythmias were found
Conclusion: In a mixed population of ICU patients, vitamin C administration is associated with no significant effect on survival, length of ICU or hospital stay. In cardiac surgery, beneficial effects on postoperative atrial fibrillation, ICU or hospital length of stay remain unclear. The quality and quantity of evidence is still insufficient to draw firm conclusions, not supporting nor discouraging the systematic administration of vitamin C in these populations. Vitamin C remains an attractive intervention for further investigations aimed to improve clinical outcome
Effects of alpha Adrenergic Agonists
Commonly employed to increase vascular tone, but may decrease cardiac output and regional blood flow, especially in cutaneous, splanchnic, and renal capillary beds
Effects of Beta-Adrenergic Agonists
Used to help maintain cardiac output via positive inotropic and chronotropic effects, as well as increased splanchnic perfusion, but can have deleterious effects such as increased cellular metabolism and immunosuppression
What determines the action of catecholamine vasopressor drugs?
Affinity for 3 major subclasses of adrenergic receptor subtypes
alpha-adrenergic (a1 and a2)
B-adrenergic (B1 and B2)
Dopaminergic (dopamine receptors 1-5)
Where are alpha-adrenergic receptors located?
Within pre- and postsynaptic regions of sympathetic nerve endings on smooth muscle cells and, in lesser number, on myocardial cells
What does stimulation of a-receptors result in?
Stimulation in the vascular muscle causes vasoconstriction and increases blood pressure
Myocardial a-receptor stimulation may have a slower onset and lead to a prolonged increase in the inotropic state of the heart
Where are Beta-adrenergic receptors located?
In the myocardium
B2 receptors are located in the peripheral vascular and bronchial smooth muscle
What does stimulation of B receptors result in?
Positive inotropic and chronotropic effects within the myocardium
Relaxation of smooth muscle in the bronchial tree and vascualture
Increases splanchnic and microcirculatory perfusion
Potential Adverse Effects of B-Adrenergic Agonists
Arrhythmias
Cellular modifications (e.g. insulin secretion, glycogenolysis, glucagon secretion, and lipolysis) that increase energy requirements
Lactate production
Immunosuppression
Where are dopamine receptors located?
Smooth muscle of renal, coronary, splanchnic, and cerebrovascular beds
What does stimulation of dopamine receptors result in?
Inhibition of norepinephrine release from the sympathetic nerve terminals, leading to vasodilation of the local vessels
Changes in the endocrine system, which may affect immunocompetency
Why do vasopressor agents commonly used to treat hypotension have some degree of B-adrenergic activity?
a-adrenergic effects lead to an increase in left ventricular afterload and may decrease cardiac output if used alone
Dopamine versus Norepinephrine
Studies suggest that norepinephrine might be preferable over dopamine
Epinephrine versus Norepinephrine
Only high doses of epinephrine are correlated with a higher cardiac index (and heart rate) compared with equivalent doses of norepinephrine
Epinephrine is associated with elevations in heart rate and serum lactate and a decrease in splanchnic perfusion for up to 48 hours in people with septic shock or circulatory failure from other causes
The B-adrenergic stimulation caused by epinephrine is more likely to cause tachyarrhythmias compared to norepinephrine
Vasopressin
Nonadrenergic vasopressor that potentiates the effects of a-adrenergic agonist drugs
Synthesized in the hypothalamus and transported to the pituitary gland for storage
What does vasopressin cause?
Constriction of vascular smooth muscle by directly activating the V1 receptors which leads to an increase in intracellular calcium via the phosphatidylinositol-bisphosphonate cascade
Inhibits IL-B induced production of NO and cGMP as well as inducible NO synthase mRNA expression via the V1 receptor
Blocks the K+ sensitive ATP channels in hte vascular endothelium, which are activated with endotoxemia, decreasing the amount of K+ flux and subsequently opening the voltage-dependent calcium channels, which further increases the intracellular calcium concentrations and promoted vasoconstriction
2012 Surviving Sepsis Guidelines for Vasopressors
Norepinephrine as the first-choice vasopressor to maintain a mean arterial pressure of 65 mmHg or greater
Epinephrine administration when an additional agent is required
Vasopressin can be added to norepinephrine to either raise the arterial blood pressure to the goal value or decrease the norepinephrine dose, but should not be used as the initial vasopressor
Dopamine is not recommended except in highly selected circumstances
Sepsis-3 Sepsis Definition
Life-threatening organ dysfunction caused by a dysregulated host response to infection
Sepsis-3 Organ Dysfunction Criteria
Represented by an increase in the Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score of 2 points or more, which is associated with an in-hospital mortality greater than 10%
Sepsis-3 Septic Shock Definition
Subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than sepsis alone
Sepsis-3 Septic Shock Criteria
A vasopressor requirement to maintain a mean arterial pressure of 65 mmHg or greater and serum lactate level greater than 2 mmol/L (>18 mg/dL) in the absence of hypovolemia
Mortality Rates Associated with Septic Shock
Associated with hospital mortality rates greater than 40%
quickSOFA (qSOFA) Criteria
In out of hospital, emergency department, or general hospital ward settings, adult patients with suspected infection can be rapidly identified as being more likely to have poor outcomes typical of sepsis if they have at least 2 of the following clinical critera that together constitute a new bedside clinical score termed quickSOFA (qSOFA): respiratory rate of 22/min or greater, altered mentation, or systolic blood pressure of 100 mmHg or less
2021 Surviving Sepsis Resuscitation Guidelines
For patients with sepsis induced hypoperfusion or septic shock, suggest that at least 30 ml/kg of IV crystalloid fluid should be given within the first 3 hours of resuscitation
For adults with sepsis or septic shock, suggest using balanced crystalloid instead of normal saline for resuscitation
Suggest resuscitation be guided by dynamic over static measures, target a decrease in serum lactate, and use capillary refill as an adjunct measure of perfusion
Recommend against qSOFA as a sole screening tool
Suggest that patients who are determined to need intensive care be admitted to an ICU within 6 hours
Albumin is suggested in patients who have received large volumes of cyrstalloid
2021 Surviving Sepsis Vasopressor Guidelines
For adults with septic shock, suggest starting vasopressors peripherally to restore mean arterial pressure rather than delaying initiation until a central venous access is secured
For patients with septic shock, recommend norepinephrine as the first line vasopressor
2021 Surviving Sepsis Vitamin C Recommendations
For adults with sepsis or septic shock, suggest against using IV vitamin C
2021 Surviving Sepsis Corticosteroids Guidelines
For adults with septic shock and an ongoing requirement for vasopressor therapy, suggest using IV corticosteroids
2021 Surviving Sepsis Follow-Up Guidelines
For adult survivors of sepsis or septic shock, recommend assessment and follow-up for physical, cognitive, and emotional problems after hospital discharge
2021 Surviving Sepsis Infection Recommendations
Recommend delivering antimicrobials as soon as possible, ideally within 1 hour of sepsis recognition
For patients with probable sepsis, recommend administering antimicrobials immediately, ideally within 1 hour of recognition
For patients with possible sepsis, but without shock, recommend rapid assessment of the likelihood of infection versus non-infectious illness
If concern for infection persists after a time-limited course of rapid investigation, then antimicrobials should be administered within 3 hours from when sepsis was first recognized
For patients with a low likelihood of infection and without shock, the guidelines suggest deferring antimicrobials while continuing to closely monitor the patient
Suggest use of empiric coverage for MRSA, empiric double-coverage for gram-negative pathogens, and empiric coverage for fungal pathogens be determined based on patient and contextual risk factors
2021 Surviving Sepsis Ventilation Recommendations
Recommend a low tidal volume ventilation strategy with limitation of plateau pressure for patients with sepsis-associated ARDS and the use of prone positioning in moderate-to-severe ARDS
Suggest a low tidal volume approach for all patients with sepsis induced respiratory failure
Suggest using traditional recruitment maneuvers but recommend against an incremental PEEP strategy
2021 Surviving Sepsis Goals of Care and Long-Term Outcomes Recommendations
Recommend screening for economic and social support for patient and families, involving patients and families in shared decision-making regarding discharge planning, reconciling medications at both ICU and hospital discharge, including information about sepsis and common impairment after sepsis in discharge summer, and assessing for physical, cognitive, and emotional problems after hospital discharge
Suggest having a critical care transitional program during ICU stay to floor transitions, using a handoff process during transitions of care, offering verbal and written sepsis education, and referring patients to peer support programs, post-critical illness follow-up programs (if available) and post-hospital rehabilitation programs (for selected survivators)
Wong et al, 2018
Evaluation of updated sepsis scoring systems and systemic inflammation response syndrome criteria and their association with sepsis in equine neonates
Objective: TO evaluate the sensitivity and specificity of 2 updated sepsis scores and the systemic inflammatory response syndrome (SIRS) criteria in regard to detecting sepsis in foals
Results:
126 foals were septic and 147 sick-nonseptic
The original and updated sepsis scores were significantly higher in septic foals as compared to sick non-septic and healthy foals
The sensitivity and specificity of the updated sepsis scores to predict sepsis were not significantly better than those of the original sepsis score
Evaluating Score 2 using a cut-off of 12, the sensitivity and specificity to predict sepsis were 60% and 61%, respectively, whereas using a cut-off of 10, the sensitivity and specificity were 73% and 40% respectively
Sensitivity and specificity of Score 2 were not significantly improved when compared with the sensitivity and specificity of Score 1, which was 62% and 64%, respectively, when using a cut-off of 8
A cut-off value of 11 for Score 3 maximized sensitivity (62%) and specificity (67%) to predict sepsis in hospitalized foals but was not significantly better in predicting sepsis when compared with Score 1
127 of 273 (46.5%) of foals met the original SIRS criteria and 88/273 (32%) foals met the equine neonatal SIRS criteria
The original SIRS criteria has similar sensitivity and specificity for predicting sepsis as did the 3 sepsis scores in the study
Notable differences in variables between sick and sick-nonseptic and healthy foals were a significantly lower WBC count in septic foals when compared with sick-nonseptic and healthy foals and a significantly lower rectal temperature and significantly higher lactate concentration in the septic and sick non-septic foals compared to healthy foals
Overall survival to discharge was 79.5% whereas survival to discharge of septic foals was 73%
Conclusion: The updated sepsis scores did not provide improved ability in predicting sepsis. Fulfilling the original SIRS criteria provided similar sensitivity and specificity in predicting sepsis as the modified sepsis score and might serve as a diagnostic aid in identifying foals at risk for sepsis
Hobbs et al, 2023
Plasma syndecan-1 concentration as a biomarker for endothelial glycocalyx degradation in septic adult horses
Objective: To determine whether plasma syndecan-1 levels are increased in adult horses affected with sepsis
Results:
191 horses were included and divided into three groups
Scores for SIRS were highest for Group 3 (septic) horses and lowest in Groups 1 (healthy, nonseptic) and 2 (sick, nonseptic)
Plasma syndecan-1 concentrations in Group 3 horses were greater than those for Group 1 and Group 1
There was no difference regarding syndecan concentrations between groups 1 and 2
Conclusion: Circulating plasma levels of syndecan-1, a biochemical marker of endothelial glycocalyx damage, are increased in septic adult horses
Anderon et al, 2020
Effects of administration of ascorbic acid and low-dose hydrocortisone after infusion of sublethal doses of lipopolysaccharide to horses
Objective: Hypothesized that intravenous infusion of LPS would a) decrease endogenous AA concentrations, b) induce CIRCI, and c) administration of a combination of AA and hydrocortisone (HC) would have decreased indices of inflammation compared to either drug alone
Results:
There was no effect of drug on clinical signs or pro-inflammatory cytokine gene expression or production compared to controls at any time point
Administration of AA was associated with higher blood neutrophil counts 6 hours after LPS infusion compared to other groups
Administration of HC was associated with higher blood neutrophil counts 12 hours after LPS infusion compared to other groups
Serum cortisol increased from 5.11 before LPS administration to 9.59 1 hour after completion of LPS infusion (T1) without an effect of treatment
Conclusion: Ascorbic acid and HC appeared to protect against LPS-induced neutrophil depletion and could be considered as adjunctive therapy in horses with endotoxemia
Bauquier et al, 2020
Effect of the p38 MAPK inhibitor doramapimod on the systemic inflammatory response to intravenous lipoposlysaccharide in horses
Objective: To determine whether doramapimod is well tolerated when administered IV to horses and whether it has anti-inflammatory effects in horses in a low-dose endotoxemia model
Results:
No adverse effects of clinicopathological changes were seen in the safety study
When treated with doramapidmod as compared to placebo, horses had significantly lower heart rates, rectal temperatures, and cytokine concentrations, and a significantly higher white blood cell count after LPS infusion
Conclusion: Doramapimod has clinically relevant anti-inflammatory effects in horses, likely mediated by a decrease in leukocyte activation and decrease in the release of pro-inflammatory cytokines. To evaluate its potential as a novel treatment for systemic inflammatory response syndrome in horses, clinical trials will be necessary to determine its efficacy in naturally occurring disease