Lec 21 Ion and Water Balance 2
1/89
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
90 Terms
Vasopressin/Antidiuretic Hormone (ADH)
The concentration of the urine depends on the amount of ______ in the blood stream.
enhanced
H2O reabsorption is _______ by Antidiuretic Hormone (ADH), also called vasopressin
late distal tubule/collecting ducts
ADH acts on epithelial cells of the _________ and the _________ to increase the number of aquaporin channels on the apical membrane.
aquaporin channels/apical
ADH acts to increase the number of _______ on the ______ membrane.
ADH/impermeable
In the absence of ___, these tubules are almost completely ______ to water
bloodstream
The concentration of the urine depends on the amount of Vasopressin/Antidiuretic Hormone (ADH) in the ________
Plasma osmolarity
the concentration of solutes in the blood
receptors/hypothalamus
Plasma osmolarity is monitored by _______ in the _______
dehydration/hypothalamus
If the plasma osmolarity increases, which can occur due to _______, the ________ detects the higher concentration of solutes (such as sodium).
thirst
Hypothalamus also has an area responsible for generating sensation of ______
blood pressure/plasma osmolarity
Both low ______ and high _______ lets the hypothalamic neurosecretory cells to start pathway to release ADH
Carotid/aortic/stretch/medulla
_______ and _____ baroreceptors respond to ______ (blood pressure): axons go to cardiovascular center in _______, which has neurons projecting to the hypothalamus.
pituitary gland
ADH is released by the posterior ______
Aldosterone
Hormone secreted by the adrenal cortex that increases number of Na+/K+ ATPase pumps on basolateral membrane
Adrenal cortex
Adolsterone is released by the _____
collecting ducts/Na+/K+ ATPase pumps
Adolsterone acts on the epithelial cells of the ________ to increase the number of _________ on the basolateral membrane
K+/Na+
Adolsterone causes more ___ to be secreted into urine and more ____ to be reabsorbed
K+ channels/apical
Not only does adolsterone increase Na+/K+ ATPase pumps on the basolateral membrane, but also _____ on the ______ membrane.
Parathyroid hormone
Hormone secreted by parathyroid glands
distal tubule/Ca2+
Parathyroid hormone acts on the epithelial cells of the ______ to increase ____ reabsorption
Bone
To remedy decreasing blood Ca2+, parathyroid hormone can increase blood Ca2+ via the kidneys, but also by the dissolution of CaPO4 crystals in _____
deamination/ammonia
The amino group (NH₂) is removed from the amino acid during ______. The amino group is converted to _______, which is toxic at high levels, so it needs to be excreted or converted into less toxic forms.
Fish
_____ can excrete ammonia directly into the surrounding water
Mammals
_______ excrete ammonia by converting it into urea in the liver and then excreting urine
Birds
____ convert ammonia and excrete it as uric acid
H+ ions
Metabolic processes lead to the production of _____
HCO3-
_____ in the blood buffers acid load so blood pH doesn’t drop
kidney/HCO3-
The ____ makes _____ to replace that which is lost buffering the H+ ions
buffering
If bicarbonate (HCO3-) was not replaced continuously, the ______ capacity of the blood would be lost.
Phosphate buffer
______ prevents urine from becoming acidic
proximal/distal/carbonic anhydrase
In the _____ and _____ tubules, H2O and CO2 are being converted into H+ and bicarbonate by _______.
HCO3-/Cl-/HCO3- exchanger/Cl-
After carbonic anhydrase converts in the tubular epithelial cells, the _____ is moved into circulation (blood) via ___________ (uses concentration gradient of ____).
H+/H+ ATPase
After carbonic anhydrase converts in the tubular epithelial cells, the ___ is secreted into the urine by active transport (_______)
metabolic
The bicarbonate ion in blood used to mop up free H+ produced by ______ processes throughout body
collecting duct
In addition to the proximal and distal tubules, additional reabsorption of HCO3 - occurs in the _______
juxtaglomerular apparatus
Specialized structure in the kidney, made up of cells that surround the afferent arteriole and secrete renin when blood pressure decreases
Renin
Cells in the juxtaglomerular apparatus secrete ______ when BP is low
Renin-Angiotensin System
Hormonal system that regulates long-term blood pressure and body fluid volume by involving the kidneys, liver, lungs, and adrenal glands
Juxtaglomerular cells/stretch receptors
________ in the walls of the afferent arterioles receive information about blood pressure from __________
angiotensinogen
Inactive precursor protein produced by the liver waiting to be activated by renin
Angiotensin I
Renin converts Angiotensinogen to _______
Angiotensin-converting enzyme
Enzyme that converts Angiotensin I to Angiotensin II
Angiotensin II
Hormone that causes vasoconstriction and aldosterone release from the adrenal gland
vasoconstriction/aldosterone
Angiotensin II (hormone) causes ________ and _________ release from the adrenal gland
salt/water/blood pressure
In the angiotensin system, once aldosterone is released, it leads to _____ and ____ retention, which also increases _______
Starling Equation for Net Glomerular Filtration Pressure
PGC - PBS - piGC = Net glomerular filtration pressure
P gc
Glomerular capillary blood pressure, favors filtration
P bs
Fluid pressure in Bowman’s space, opposes filtration
pi gc
Osmotic force due to protein in plasma, opposes filtration
0
The osmotic force of the Bowman’s capsule (π BS) is typically __
Glomerular Filtration Rate
Volume of fluid that enters Bowman’s capsule per unit time
GFR formula
GFR = Rate of urine (ml/min) x (Urine concentration of solute (mol/ml))/(Plasma concentration of solute (mol/ml))
Rate of urine
The volume of urine produced by the kidneys per minute. (for GFR calculations)
Urine concentration of solute
The concentration of a specific solute in the urine. (for GFR calculations)
Plasma concentration of solute
The concentration of the same solute in the blood plasma. (for GFR calculations)
filtered/reabsorbed/secreted
When calculating GFR, the solute needs to be something that is ______ but then neither ______ nor _______, otherwise will not get accurate measure of GFR
Inulin
A substance that is freely filtered but neither reabsorbed nor secreted. It requires constant intravenous infusion into the patient over several hours. This is an invasive procedure but gives a very accurate measurement of GFR.
creatinine
A metabolite of creatine (found in muscle cells). It is a commonly used solute to estimate GFR because it is filtered by the kidneys, but only a small amount is secreted into the urine.
Experimental/metabolic
Unulin is a ______ solute while creatinine is a _____ solute
secreted/urine
Creatinine has no reabsorption but a small amount is ______ into the _______
invasive
Creatinine is less ______ than metabolic but slightly less accurate than inulin
afferent arteriole/efferent arteriole
If GFR is low, _____ constricts and _____ dilates
efferent arteriole/afferent arteriole
If GFR is high, ______ constricts and _____ dilates
Landd
The ability to control internal osmolarity independent of external conditions was essential for the success of the animal lineages that invaded ____
Kidney/malpighian tubules/gills/salt glands
Osmoregulatory Organs:
______
______
______
______
length/kidney medulla/urine
The ______ of the loops of henle correspond to the thickness of the _______ and the ability to concentrate _______
concentration gradient/water
The longer the LOH the larger the _________ in the medulla and the more _____ can be reabsorbed
Long/concentration/Kangaroo Rat
_____ Loops of Henle allow the extreme _________ of urine in the Desert ________
Malpighian Tubule
Site of urine formation in insects
secretion
Most ______ occurs in the Malpighian tubules, producing the primary urine
reabsorption/rectum
Unlike vertebrates, most water and ion _______ occurs in the ______ for insects
midgut/hindgut
The malpighian tubules can be used as a landmark to distinguish between the _____ and ______
Principal/stellate
The malpighian tubules is made up of ______ cells and _____ cells
Principal cells
Cells found in the malpighian tubules that have microvilli, many mitochondria to power active transport of positively charged ions into the lumen of the tubule
Stellate cells
Cells found in the malpighian tubules that mainly function in secreting Cl-
microvilli/mitochondria/positive ions
Principal cells have ______ and many ______ to power active transport of ______ into the lumen of the tubule
Aquaporins
Both principal and stellate cells have ________
water/salts
Freshwater fish are in constant danger of taking on too much ______ and diluting necessary body ______
permeability/water
To combat taking on too much water, freshwater fish have low ________ of skin to ________
drink
To combat taking on too much water, freshwater fish don’t _____ water
dilute
To combat taking on too much water, freshwater fish produce a _____ urine
reabsorb
To combat taking on too much water, freshwater fish actively _____ salts
salty
To combat taking on too much water, freshwater fish ingest ______ foods
Na+/gills
To combat taking on too much water, freshwater fish actively pump ___ from water into cells in ______
permeability
Similar to freshwater fish, marine fish have a low ______ of skin to water
seawater/salts/gills
Marine fish drink lots of _______ and then activelly secrete ____ through ____ into water
losing/excess
Air Breathing Marine Animals are in constant danger of ______ water to the environment and taking _____ salt
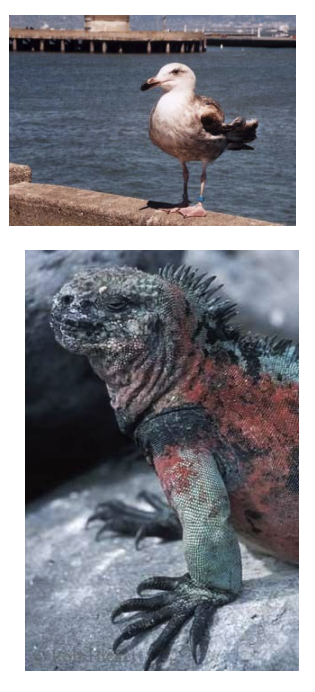
Marine fish/salt/salt glands
Air breathing marine animals have similar adaptations to _______. For example, air breathing marine animals actively secrete ___ with _______
hyperosmotic
Salt glands produce _________ secretions
high salt
Salt glands allow survival in ______ environments