5.2 Excretion
1/164
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
165 Terms
Excretion
The removal/processing of metabolic waste from the body
Metabolic Waste
Waste produced from metabolism (like CO₂, urea)
Egestion
The removal of undigested waste by defecation.
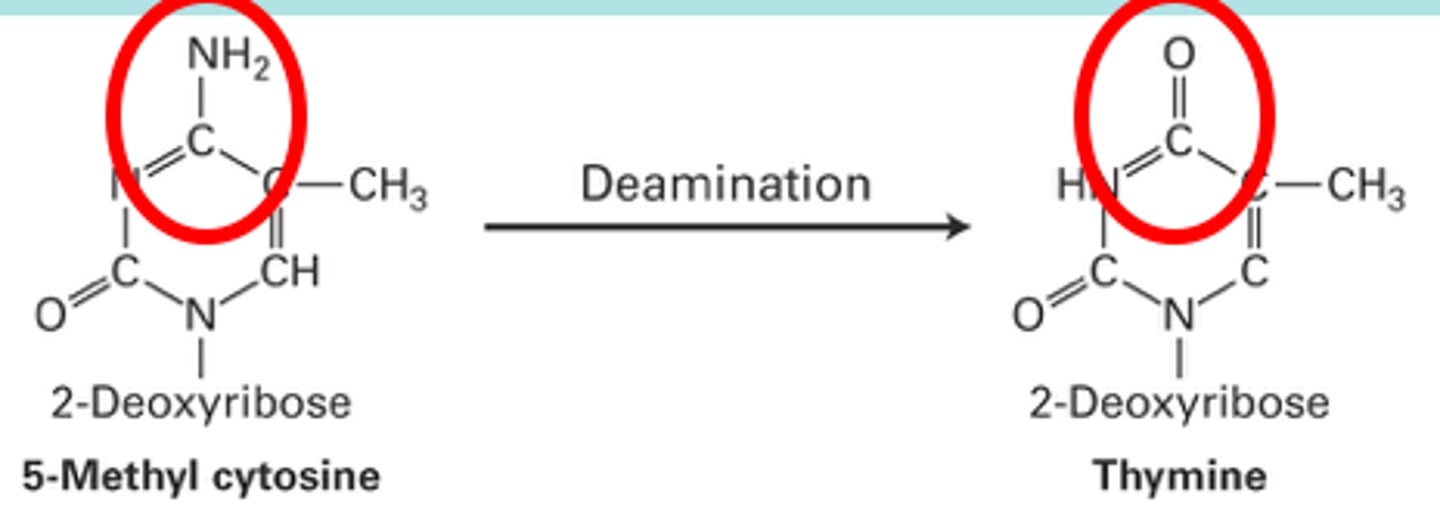
Deamination
The removal of ammonia from amino acids
Secretion
A process by which substances are produced and discharged from a cell, gland, or organ, for a particular function in the organism.
What are the main waste products?
CO₂
Nitrogenous waste in the form of urea
Why does CO₂ and urea need to be removed?
They are toxic and would cause damage if they were allowed to accumulate
What is excretion important in maintaining?
Excretion maintains normal metabolism and homeostasis by keeping levels of certain substances in the blood.
Which organs remove excretory products from the blood?
Lungs and kidney
How is CO₂ transported?
- 5% in solution in plasma as CO₂
- 10% combines with amino groups in Hb molecule (carbaminohaemoglobin)
- 85% hydrogen carbonate ions
85% hydrogen carbonate ions (HCO₃⁻)
Carbon dioxide combines with water to form carbonic acid (H₂CO₃)
Carbonic acid then dissociates into H⁺ and HCO₃⁻
HCO₃⁻ ions diffuse out of the RBCs and into the blood plasma, where they are transported in solution
What is an example of excretion?
A. the removal of undigested food through the anus
B. the release of saliva into the mouth
C. the removal of urea by the kidneys
D. the release of hormones from glands
C
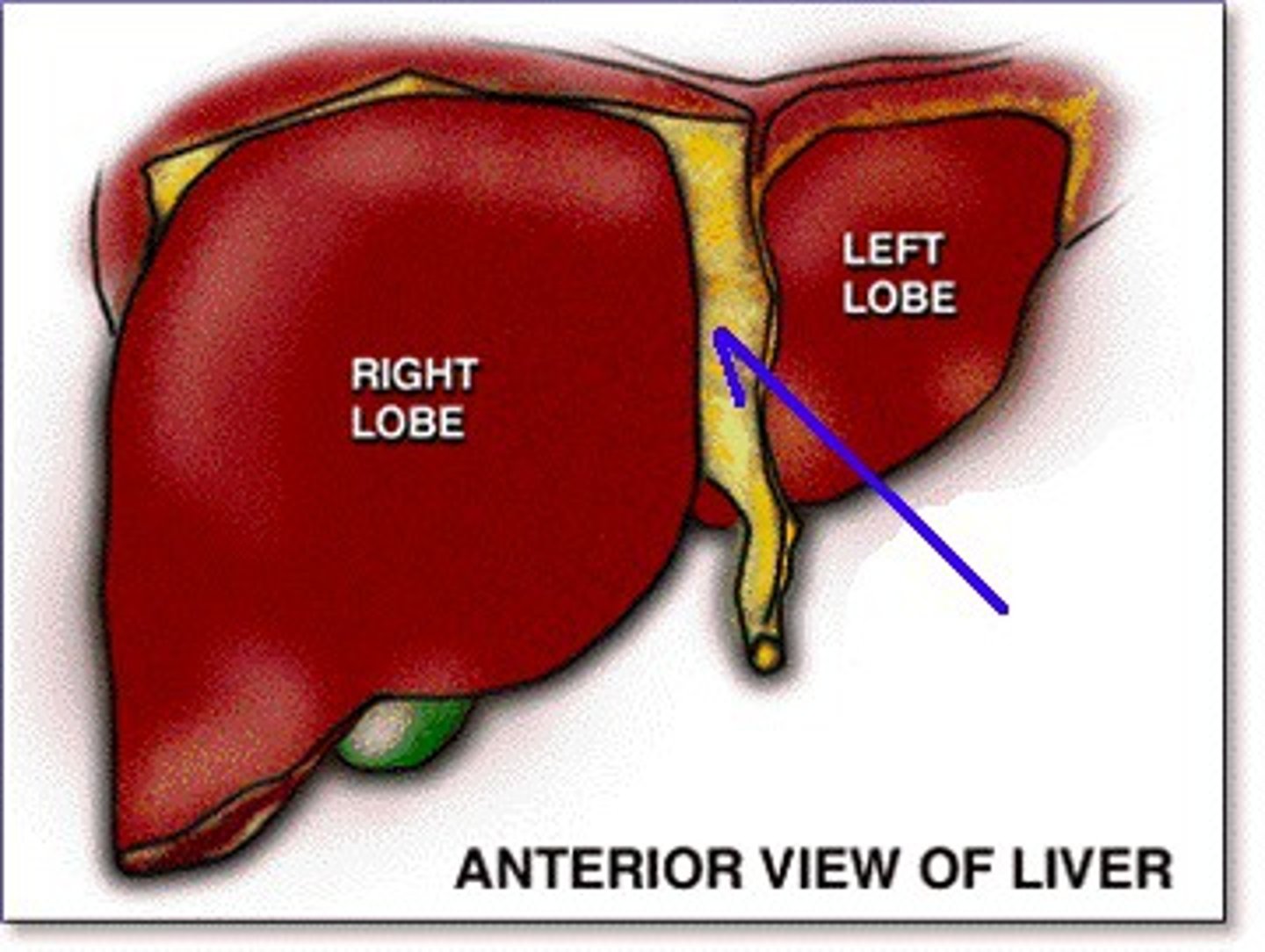
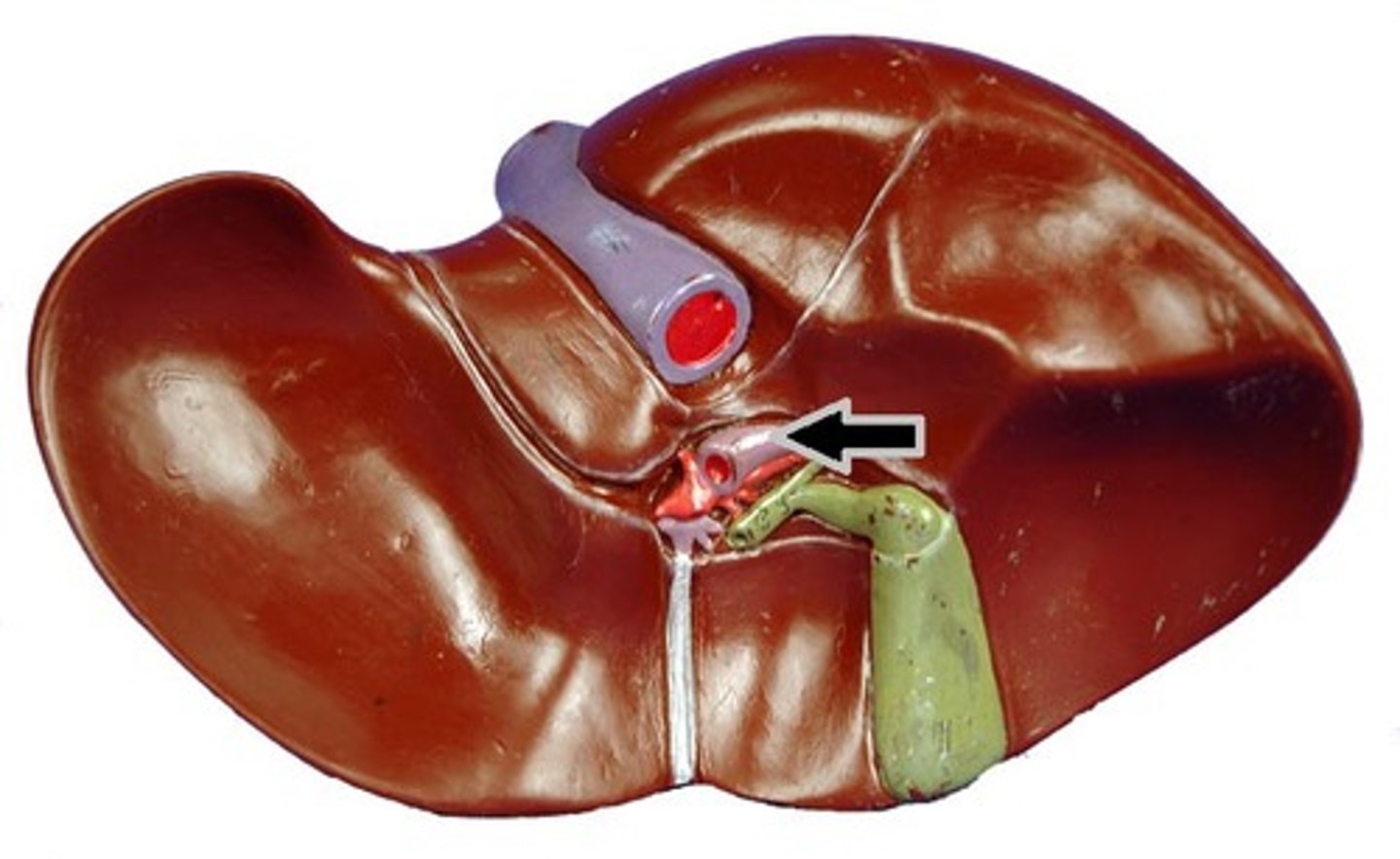
Where is the liver?
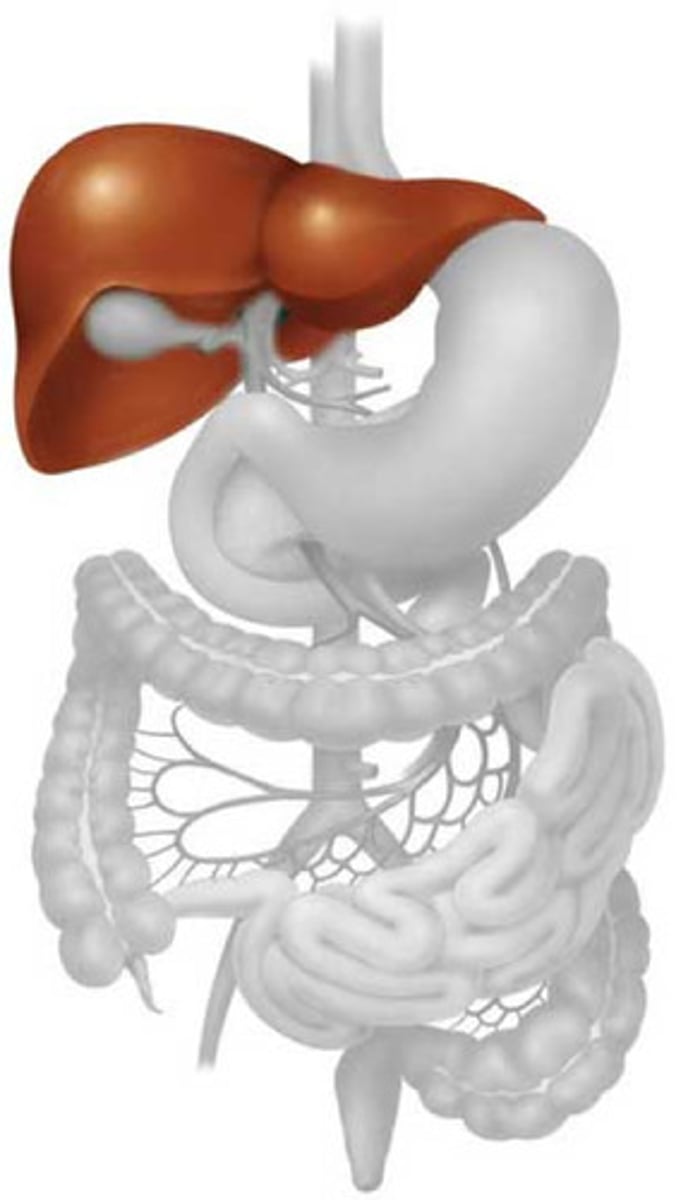
Blood supply
- Hepatic artery
- Hepatic portal vein
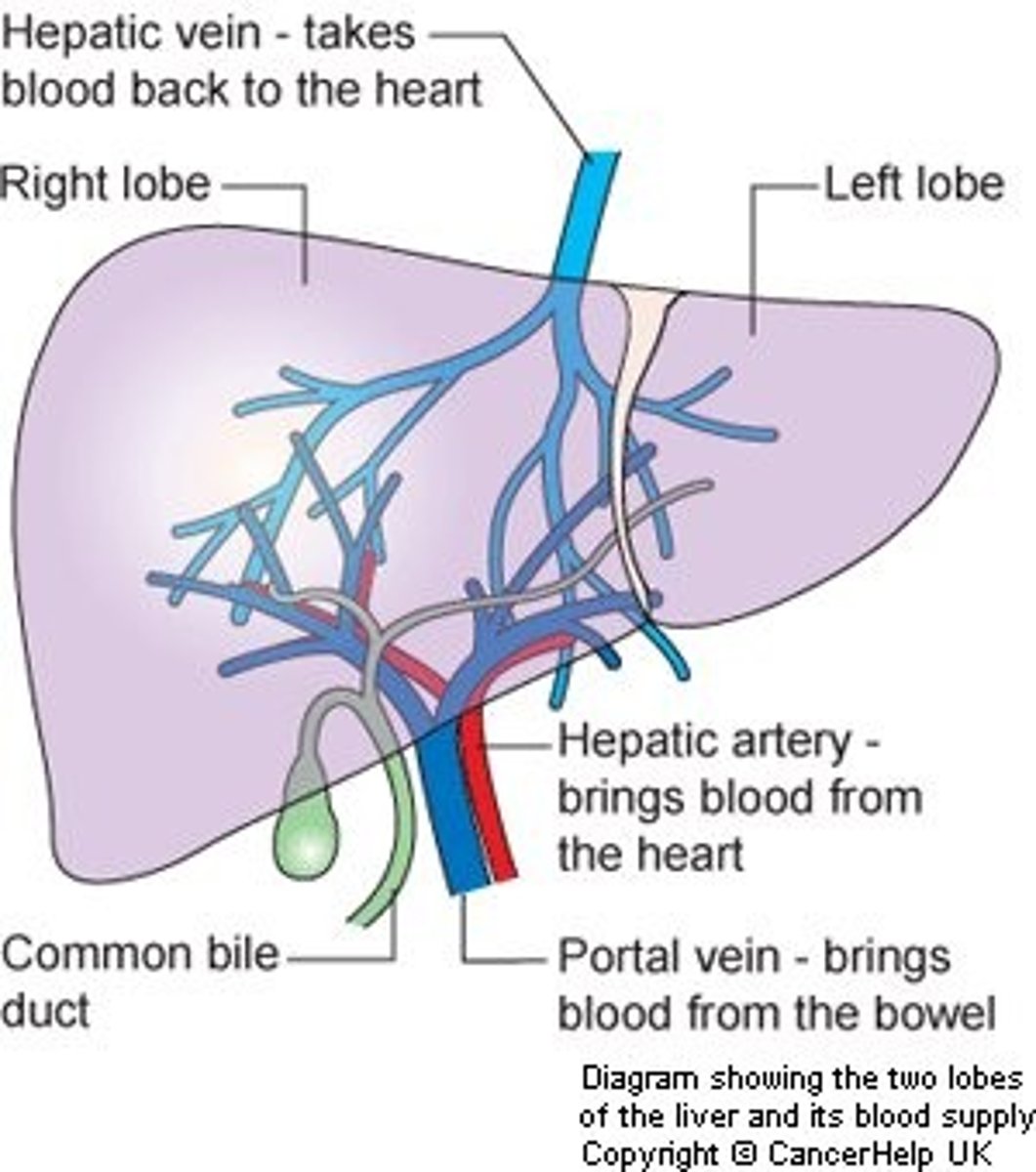
Hepatic artery
It brings oxygenated blood from the aorta to the liver through a narrow vessel
Hepatic portal vein
It delivers deoxygenated blood from the digestive tract with toxins and nutrients.
It is a branched vessel
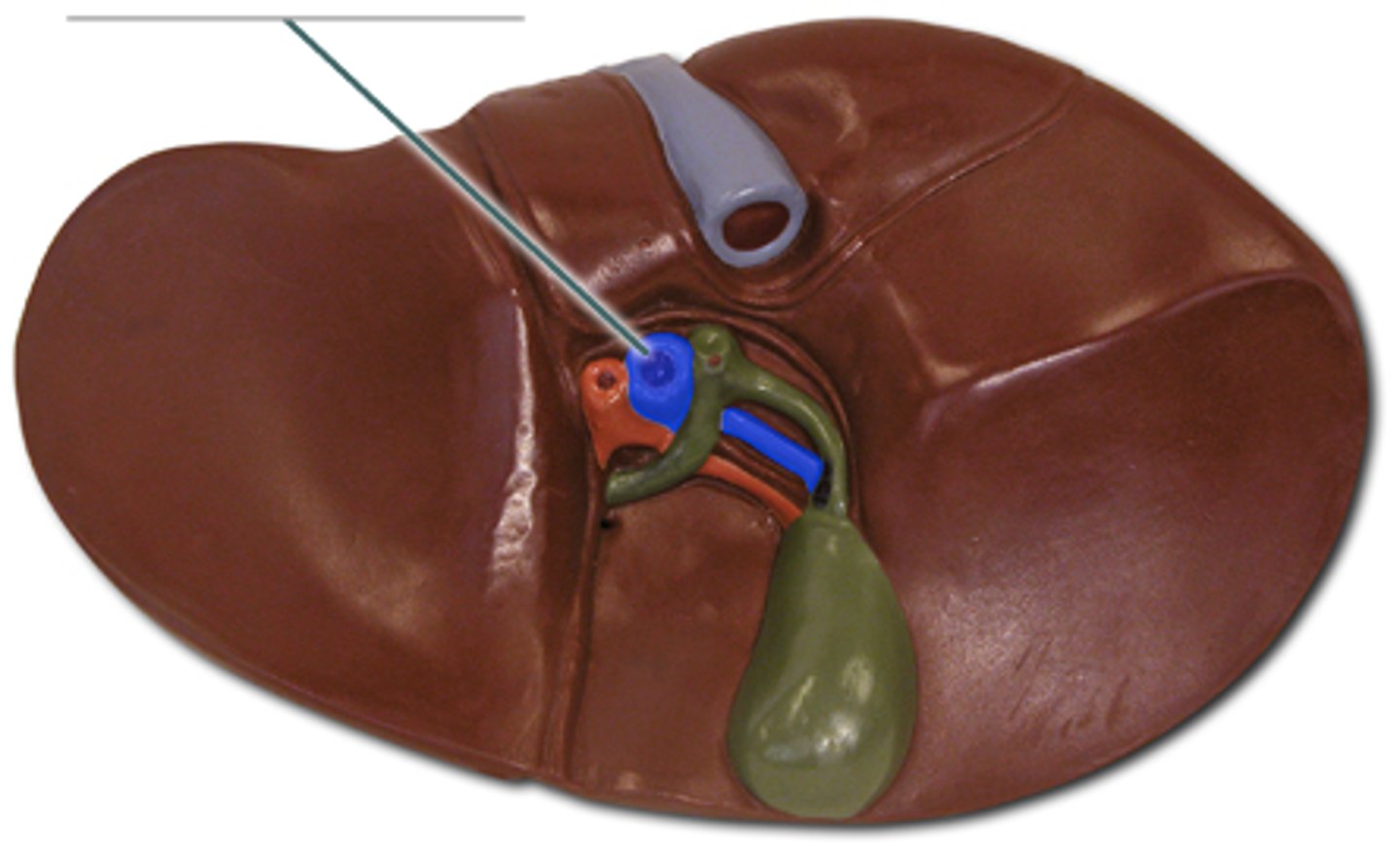
How much blood arriving to the liver is from the hepatic portal vein?
75%
The blood leaves at a very low pressure
How is blood removed?
Via hepatic vein
Hepatic vein
Blood is removed from the liver to the vena cava
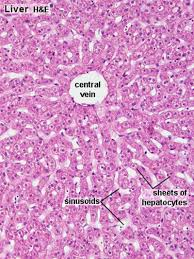
Hepatocytes
Liver cells
Features of hepatocytes
Large nuclei
Prominent Golgi apparatus
Lots of mitochondria
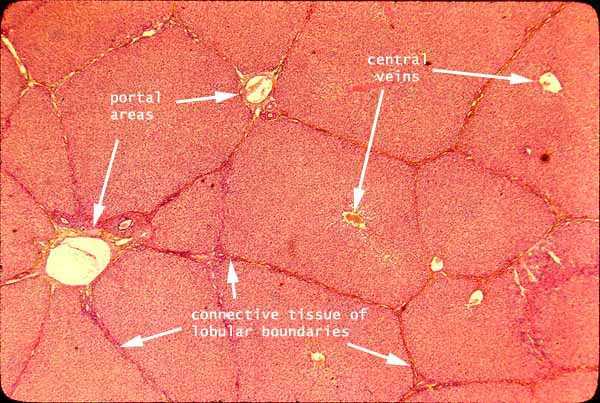
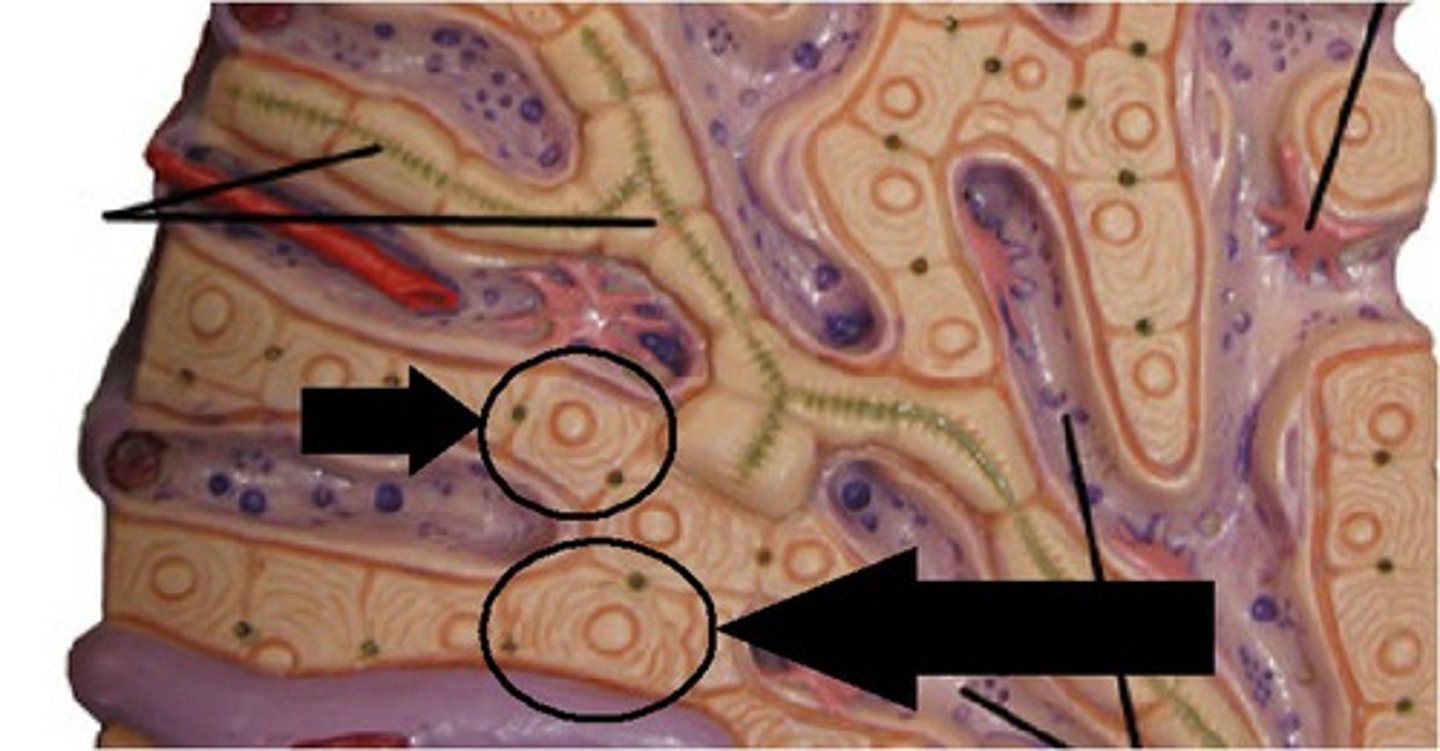
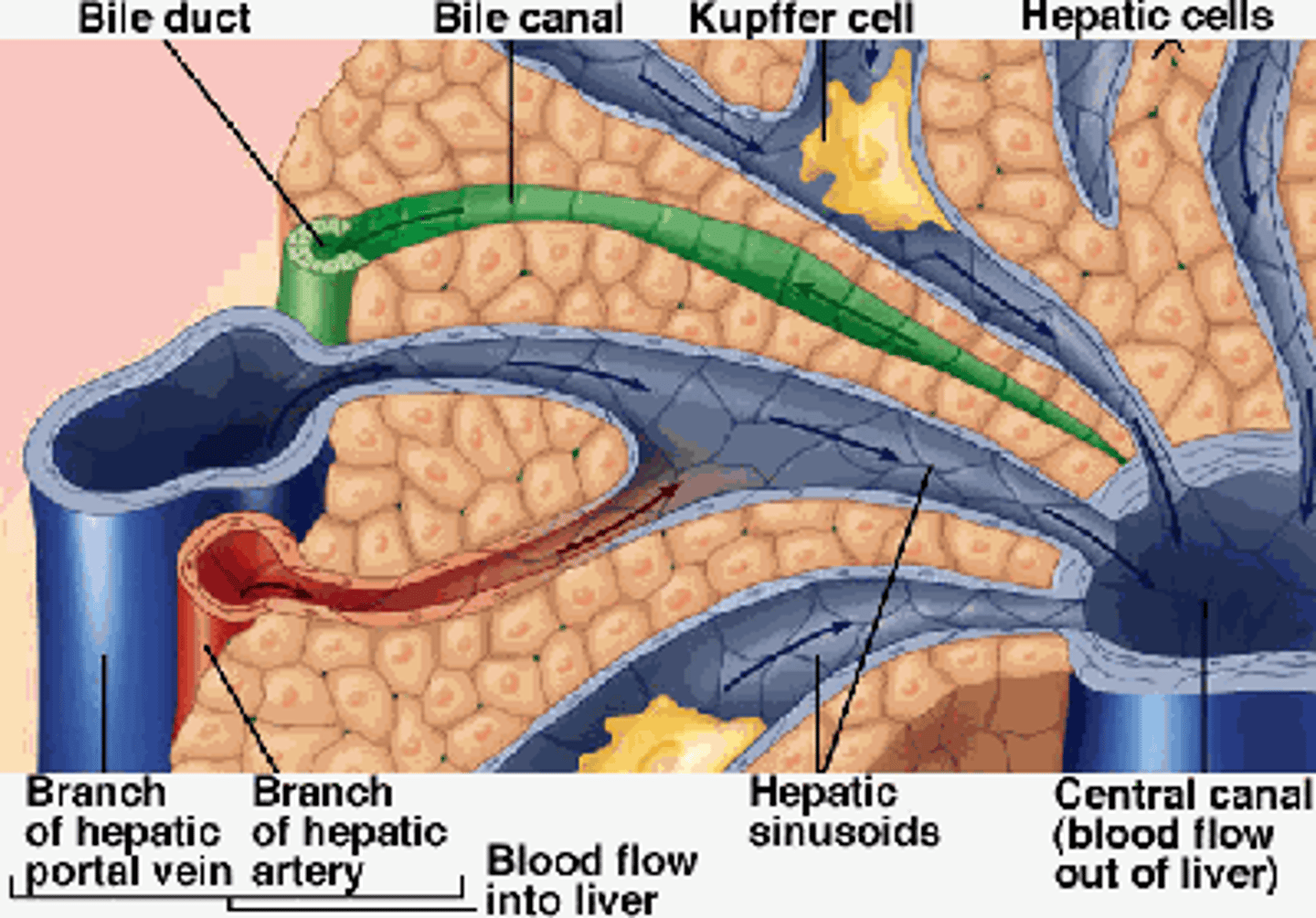
Histology of a Liver
Lobes & lobules
- The liver is divided into 2 principal lobes
- The lobes are subdivided into about 100,000 cylindrical lobules
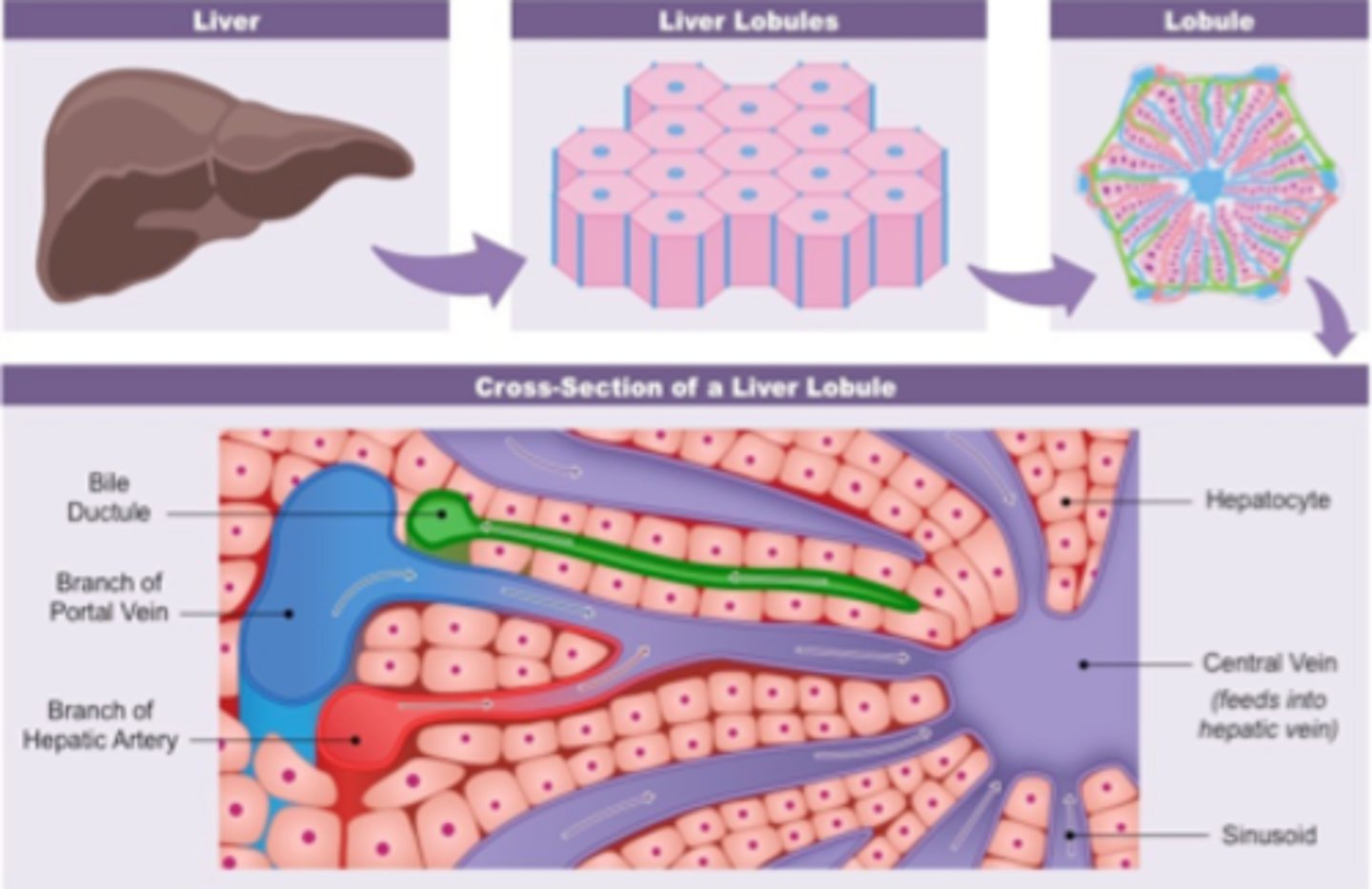
Cross section of a lobule
Branch of hepatic artery and hepatic portal vein both feed into the sinusoids which pass into the central canal, which lead to the hepatic vein
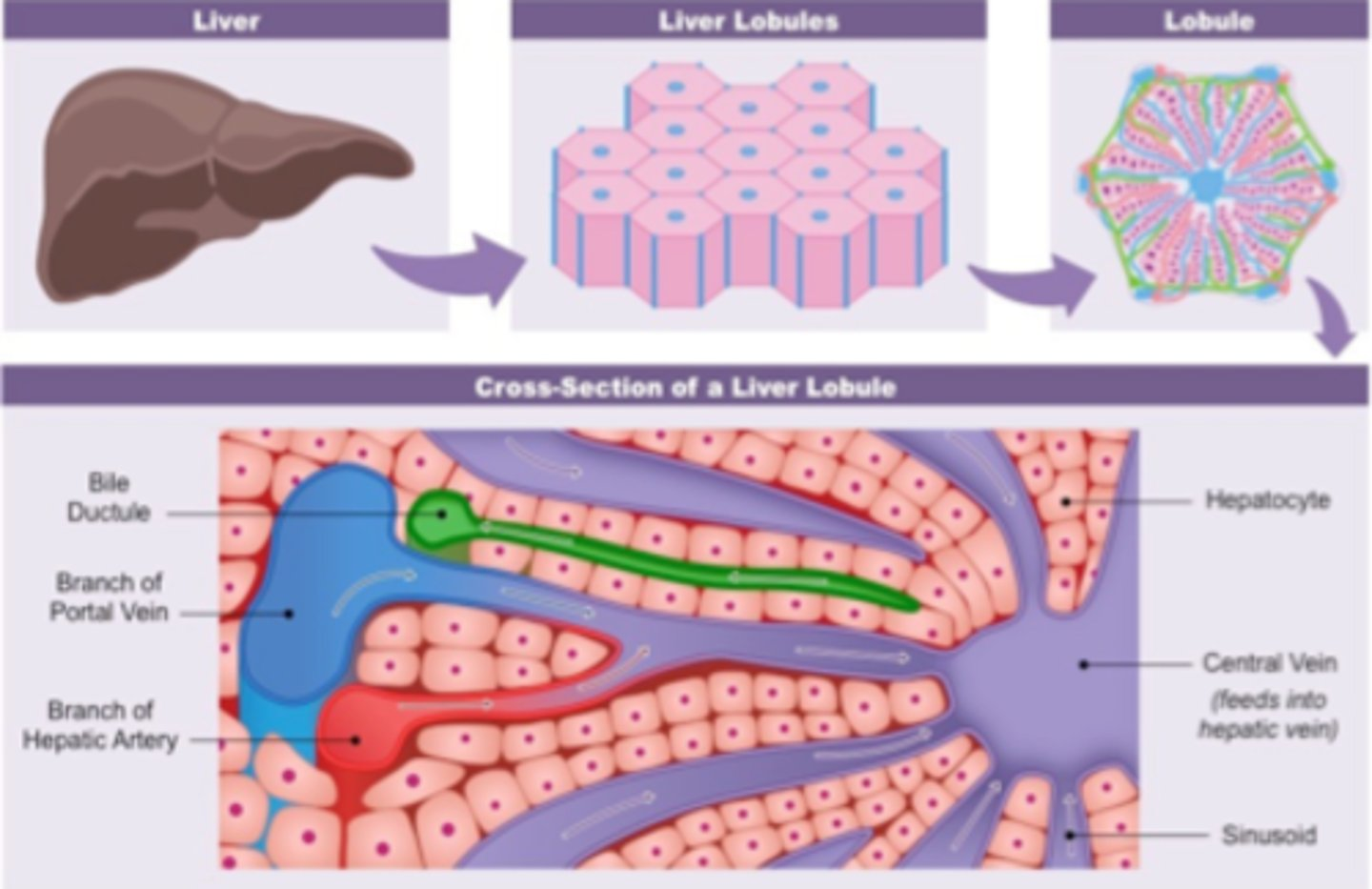
What's the central vein?
Hepatic vein
Sinusoids
Spaces surrounded by hepatocytes
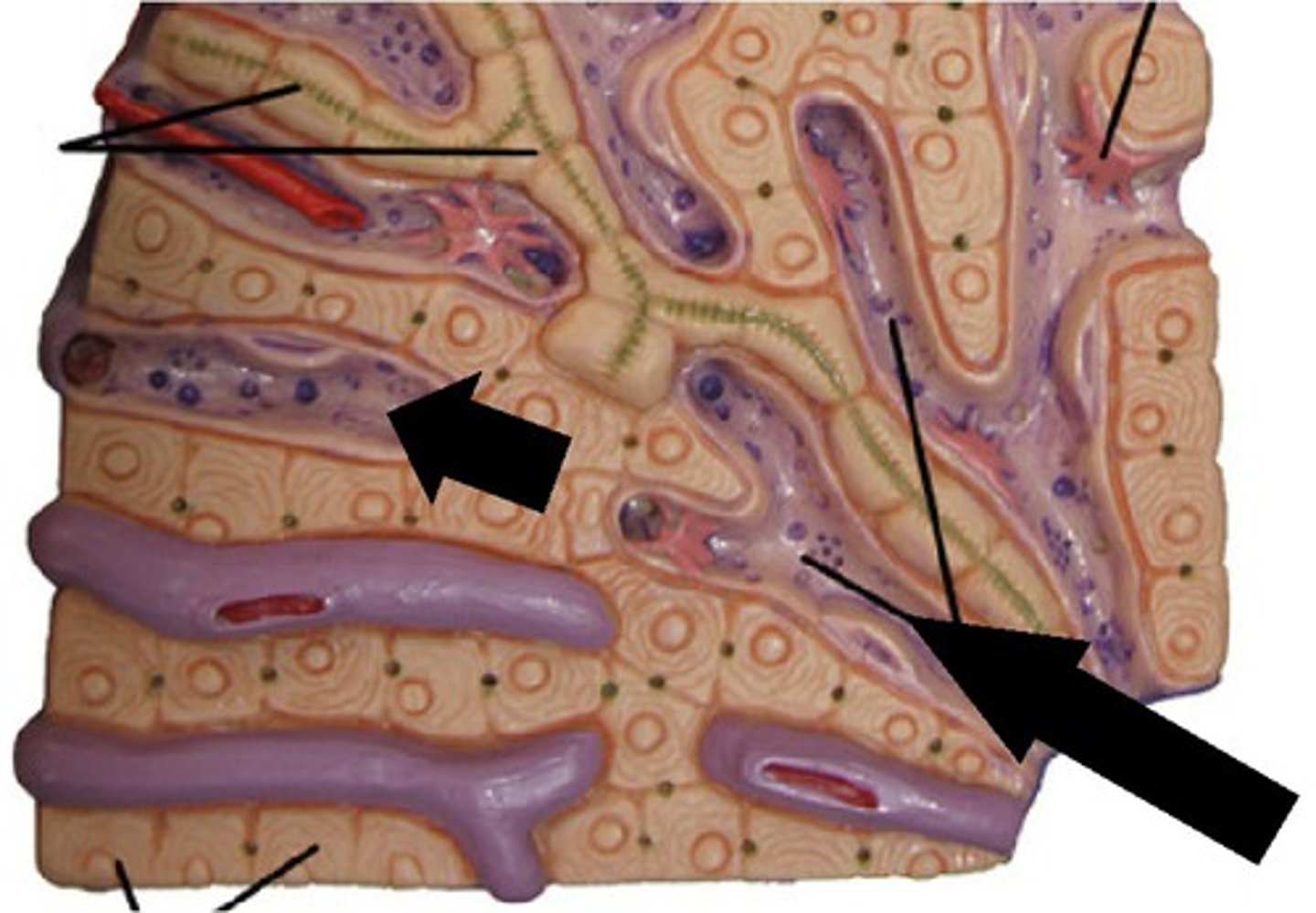
What do sinusoids do?
Connects the hepatic artery to the hepatic vein, allowing hepatocytes to remove harmful substances from the blood
The blood from the hepatic artery and hepatic portal vein is mixed in the sinusoids. The mixing increases the oxygen content of the blood from the hepatic portal vein, supplying the hepatocytes with oxygen
Difference between hepatic portal vein and hepatic artery
Hepatic portal vein has a larger lumen
Portal triad
Hepatic artery, hepatic portal vein, bile ducts
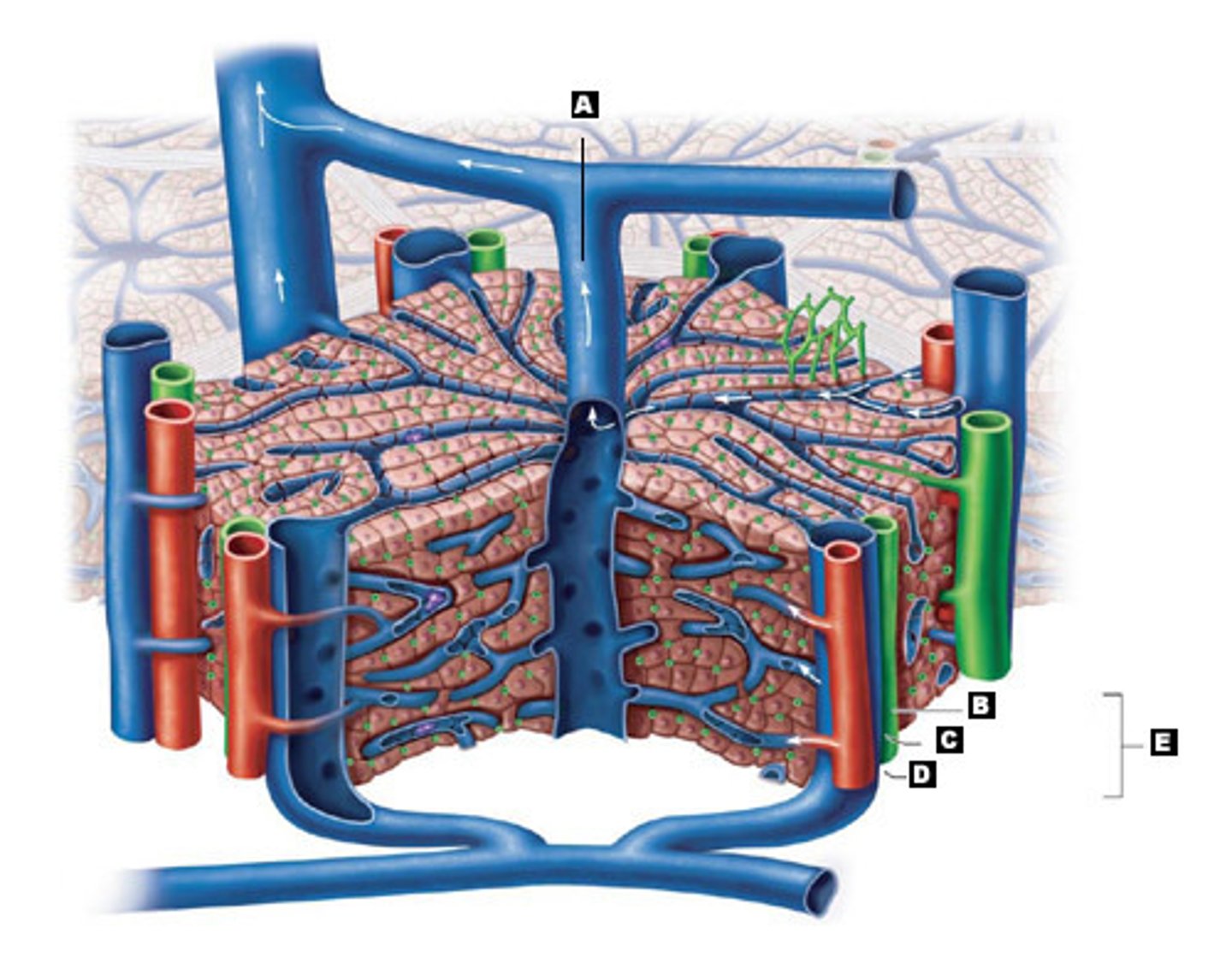
What's contained in the sinusoids?
Kupffer cells
What are Kupffer cells, where are they, and what do they do?
Macrophages in the liver
Attached to the walls of the sinusoid
They remove bacteria, break down red blood cells, ingest foreign particles, and help protect against disease
How are Kupffer cells adapted for what they do?
Thin flat cells with a short diffusion distance
Fenestrated to increase permeability
What are the 3 things hepatocytes do?
Break down harmful products, e.g. drugs and alcohol.
Store glycogen and some vitamins and minerals
Combine ammonia and carbon dioxide via the ornithine cycle
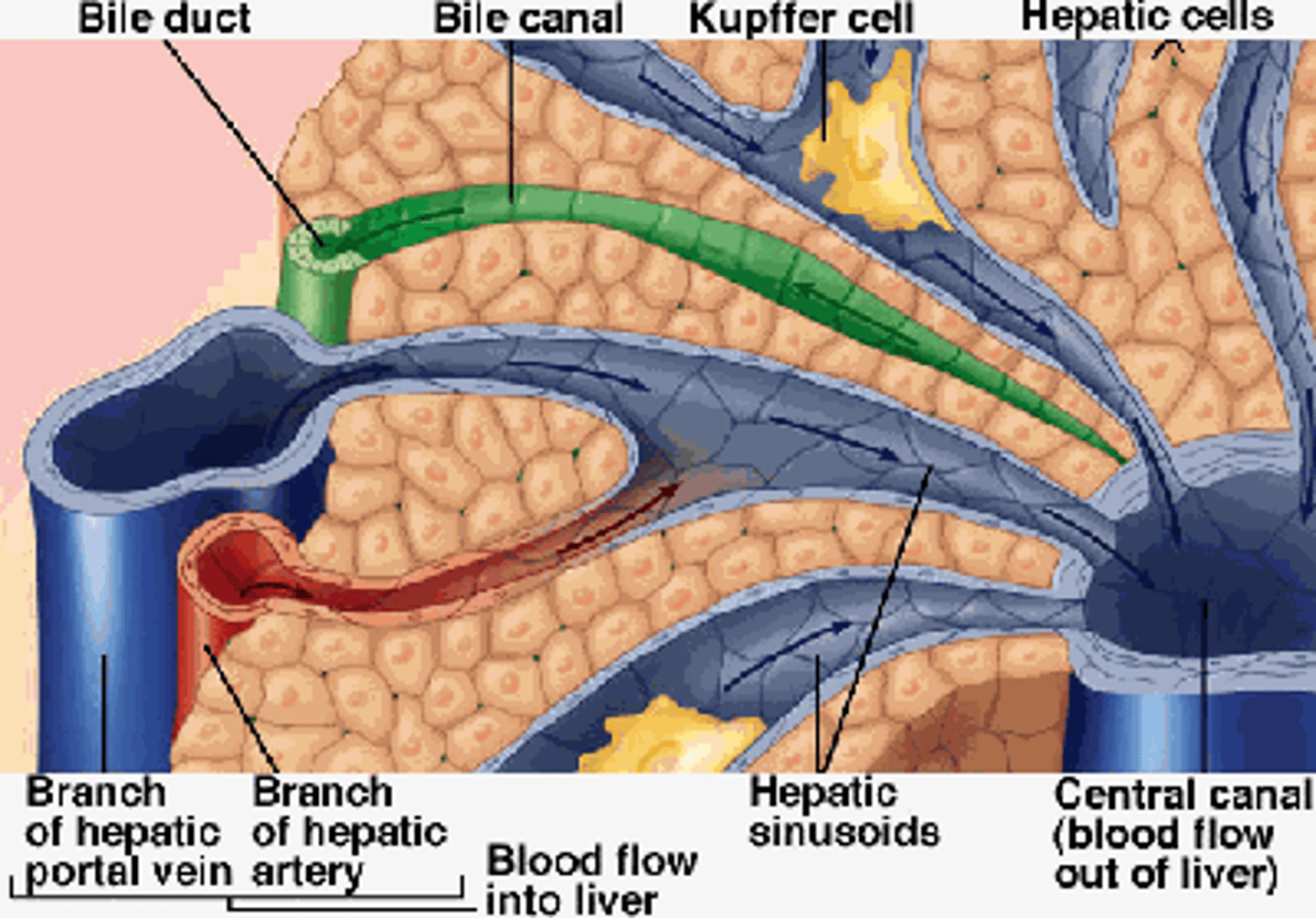
Hepatocytes and bile. What happens to the bile produced?
The breakdown of the blood leads to bile being secreted into canaliculi.
Bile drains into the bile ductules which take it to the gall bladder
3 Functions of the Liver
- Storage of glycogen
- Detoxification
- Urea formation
What is glycogen's structure?
a-1,4 glycosidic bonds
a-1,6 glycosidic bonds
Forms a branched molecule and is ideal for storage as it is insoluble and doesn't affect osmosis
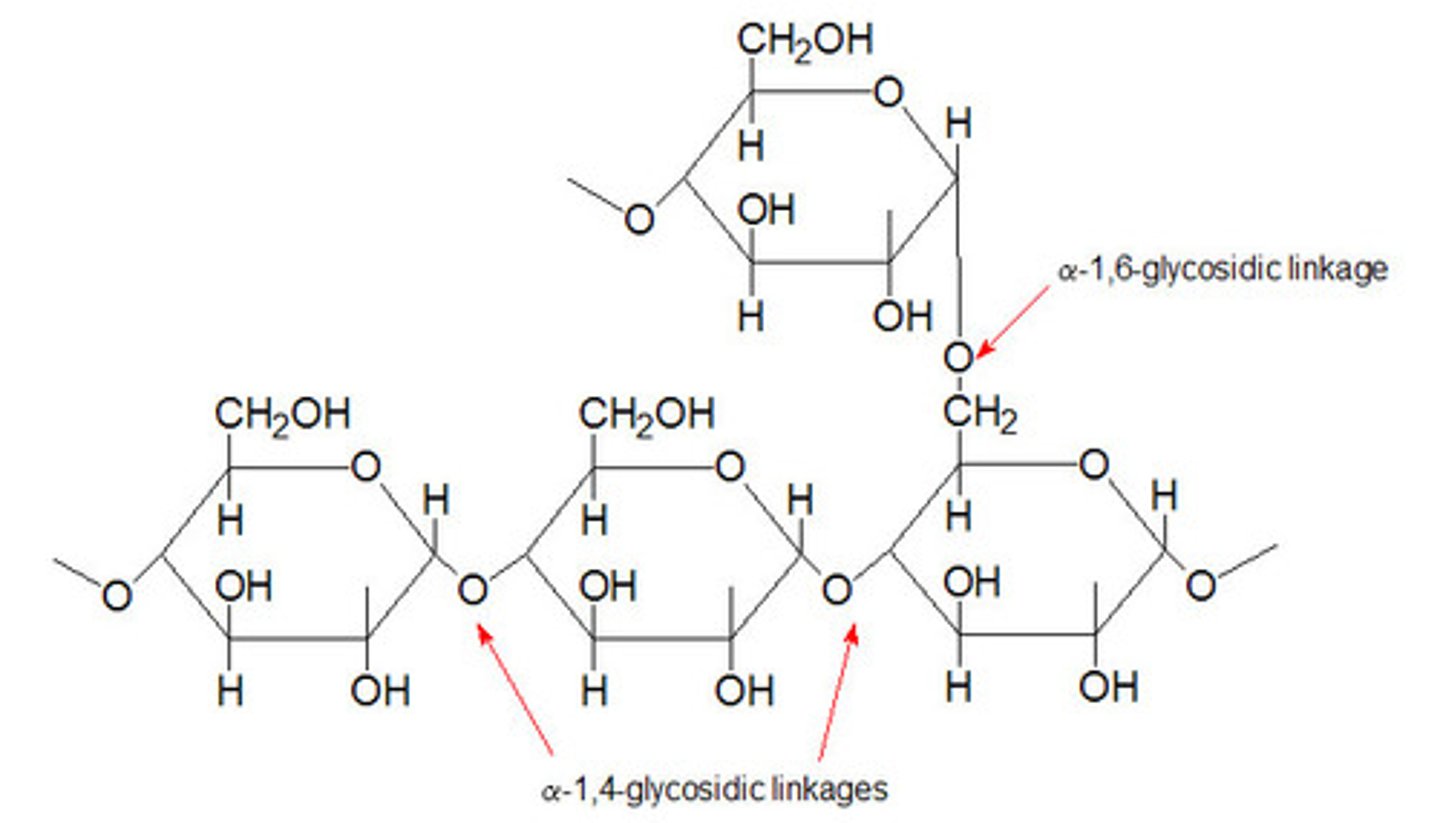
When glucose levels rise...
...insulin levels rise and stimulate hepatocytes to convert glucose to glycogen
When glucose levels fall....
...hepatocytes convert the glycogen back to glucose under the influence of the hormone glucagon.
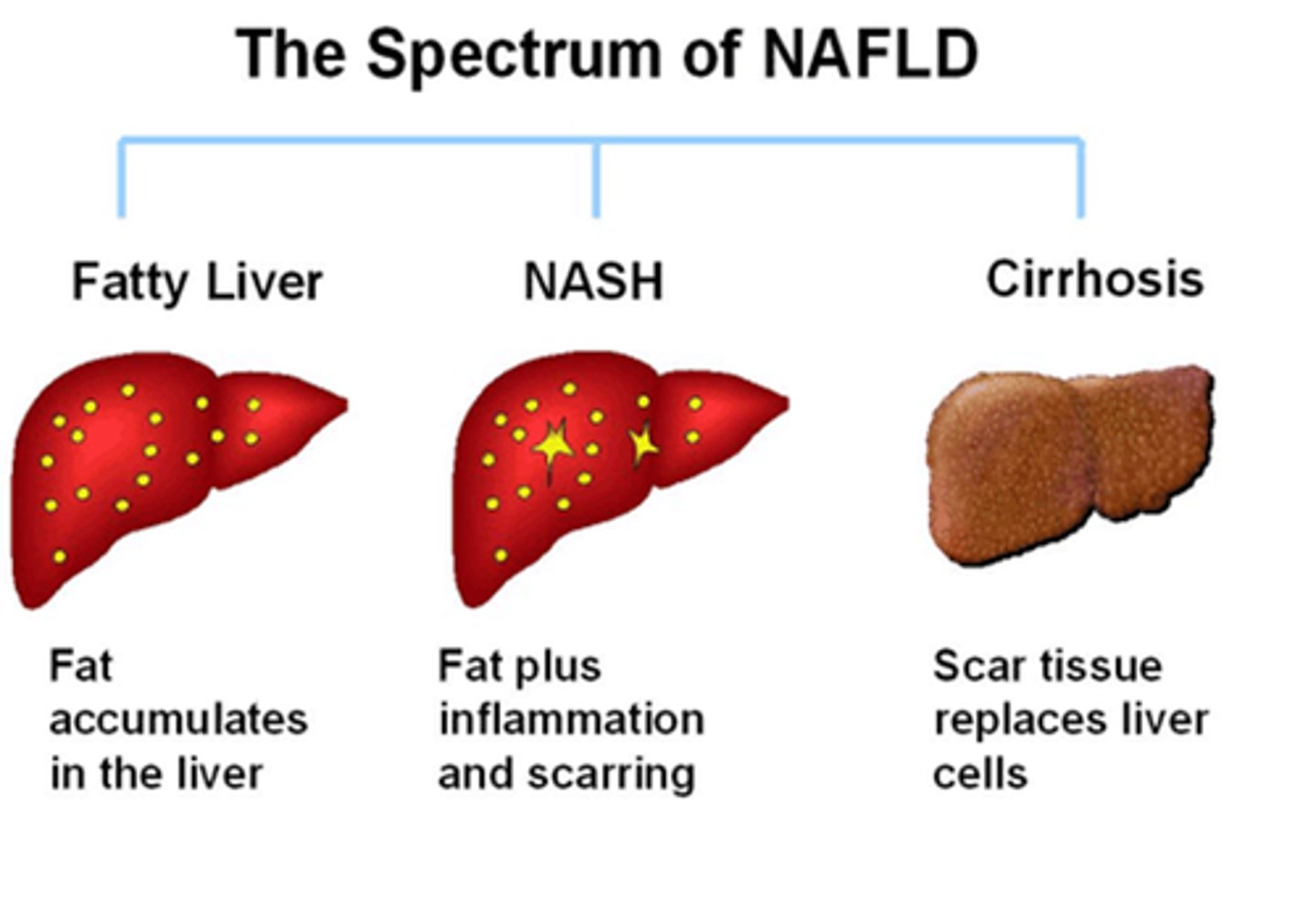
What is detoxification?
Apart from urea, many other metabolic pathways produce potentially poisonous substances
We also take in a wide variety of toxins by choice, such as alcohol and drugs.
The liver is the site where most of these substances are detoxified.
Detoxifying hydrogen peroxide (H₂O₂)
Hepatocytes contain the enzyme catalase.
Catalase splits the H₂O₂ into O₂ and H₂O.
Detoxifying the alcohol we drink
Alcohol has ethanol
Hepatocytes contain the enzyme ethanol dehydrogenase, breaking down ethanol to ethanal by the removal of H
The H is added on to NAD to form reduced NAD
Ethanal is then converted to ethanoate (acetate) by accepting the H back from the redNAD using the enzyme ethanal dehydrogenase.
What happens to the ethanoate (acetate)?
May be used to build up fatty acids or it enters the Krebs cycle
Excessive alcohol intake can lead to...
Cirrhosis
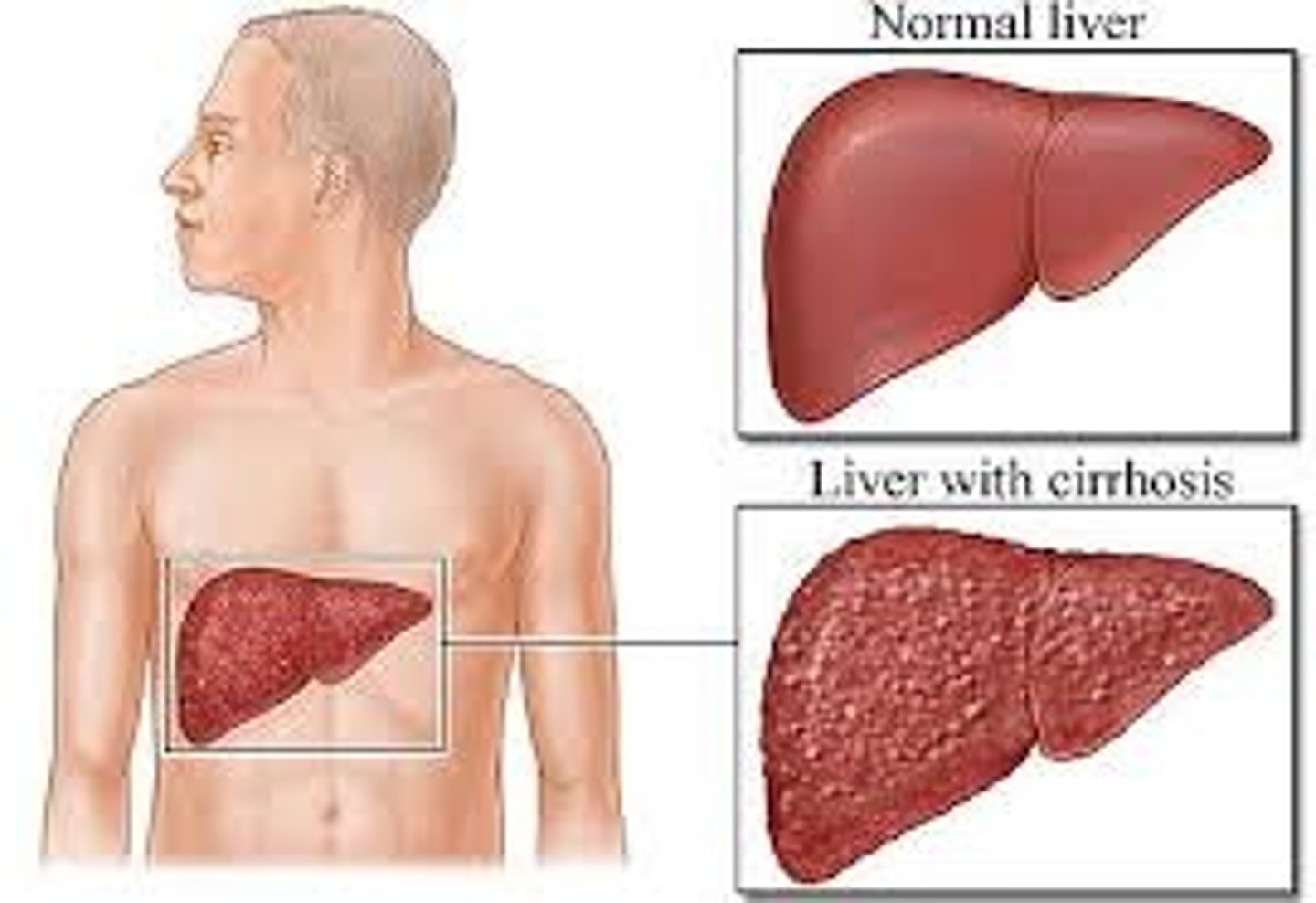
What is NAD used to do in the liver?
Oxidise fatty acids
What happens if NAD is reduced?
Then it cannot oxidise the fatty acids. Fatty acids then accumulate and are converted into fat.
The fat is deposited in the liver.
Urea formation
Urea is formed from 2 processes:
- Deamination
- Ornithine cycle
Deamination Equation
Amino acid + Oxygen → Keto acid + Ammonia
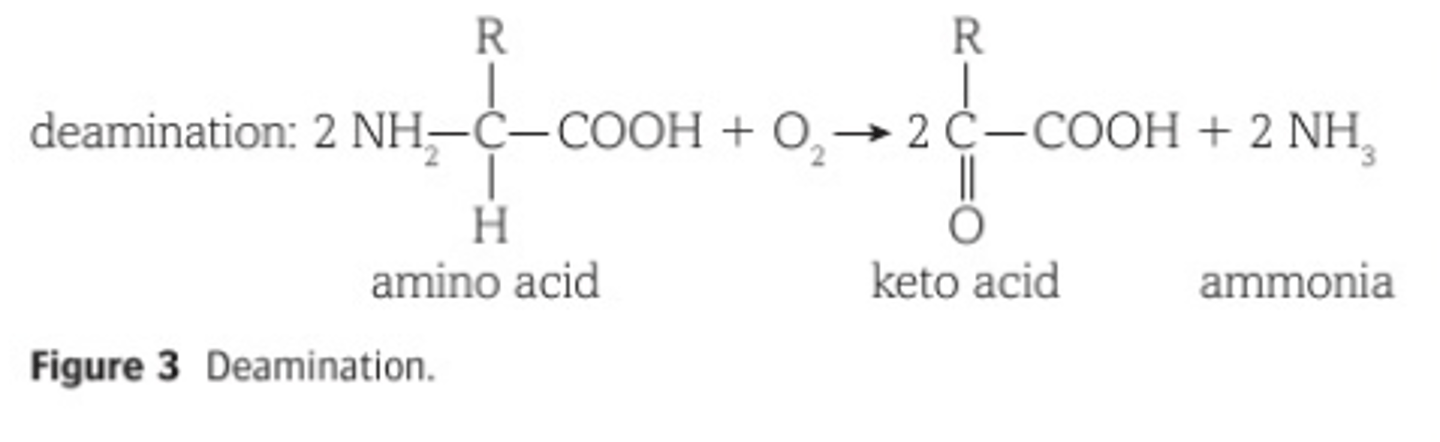
What is deamination?
- Uses excess amino acids
- Amino group (NH₂) of each amino acid is removed
- Ammonia (NH₃) is formed which is highly soluble and highly toxic
- Keto acid can enter respiration to release energy or be stored as fat
Ornithine cycle
The ammonia produced in the deamination of proteins (which is very toxic) is converted to urea via the ornithine cycle
Where does the ornithine cycle take place?
In the hepatocytes
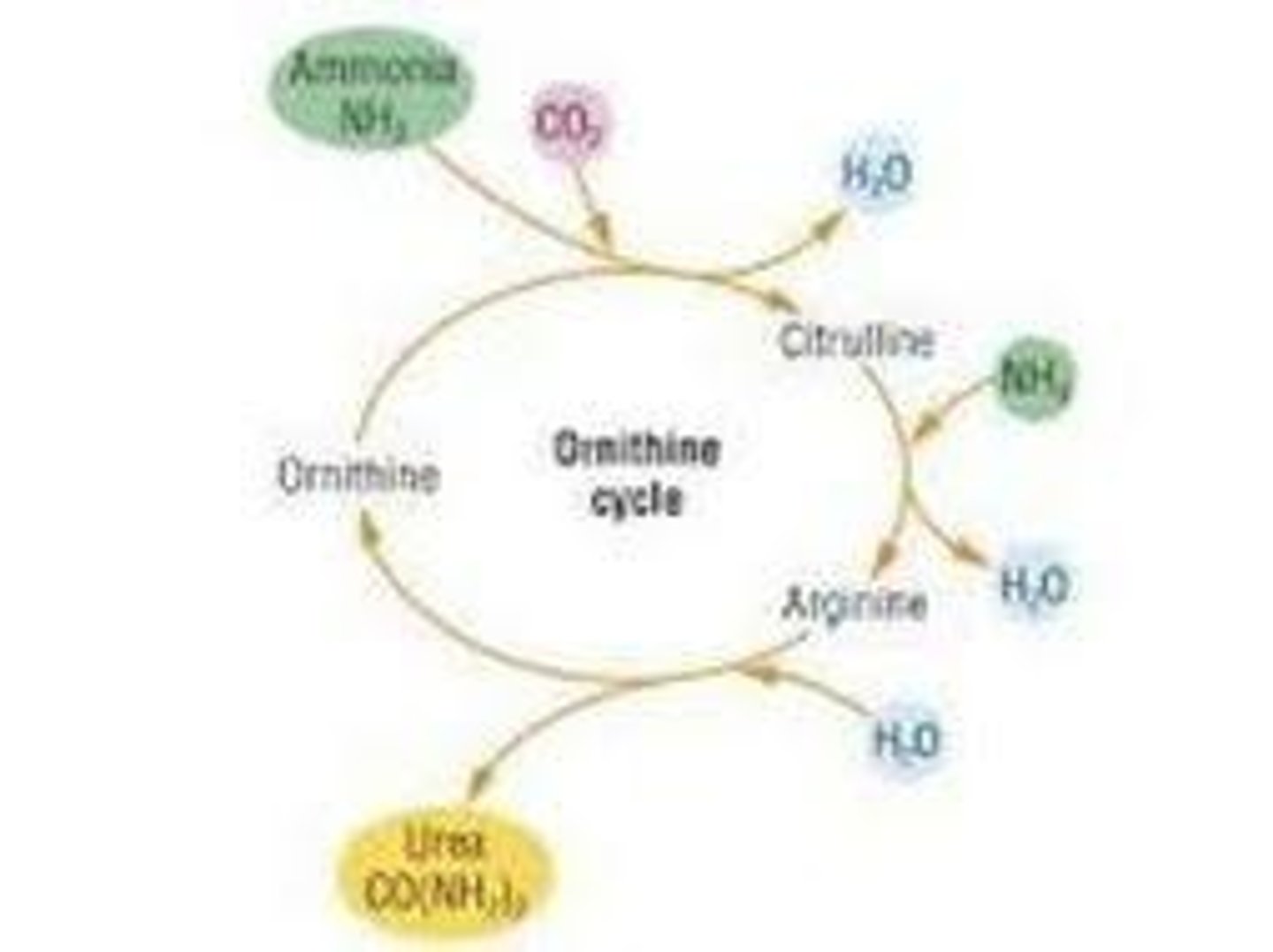
Urea formation Equation
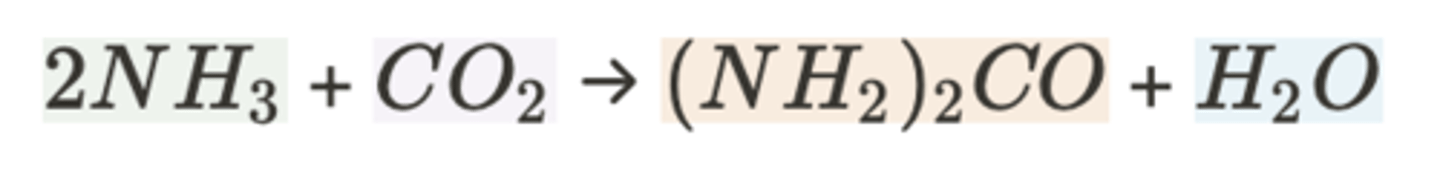
What happens to urea?
It is transported from the liver to the kidneys in the blood stream, where it is excreted, dissolved in water, as urine.
What are 3 ways to describe the excretion of urea?
Removal of metabolic wastes
Removal of substances in excess
Removal of toxic products
Is urea a metabolic waste?
Yes because it is a metabolic breakdown product from amino acids
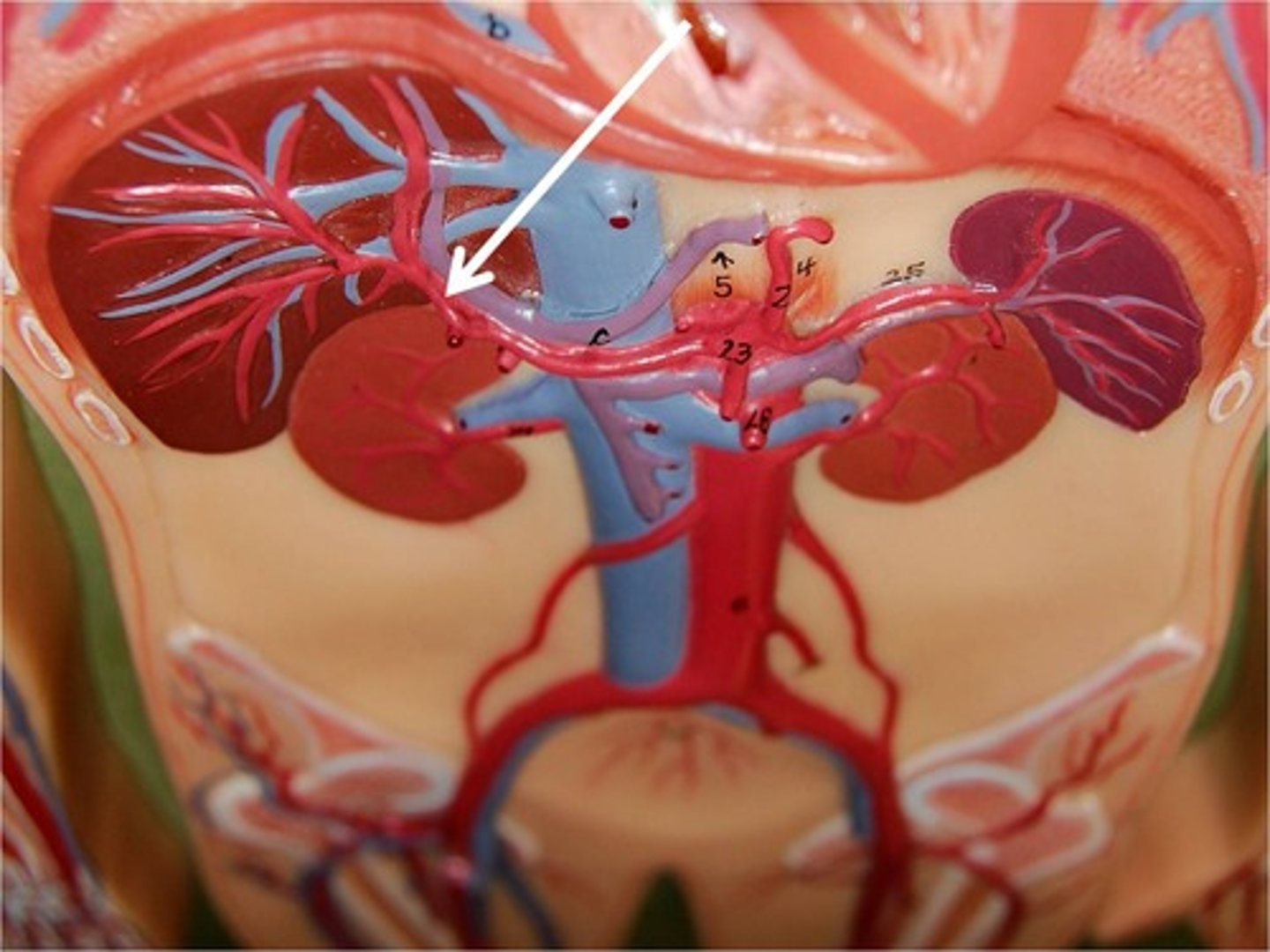
Where are the kidneys?
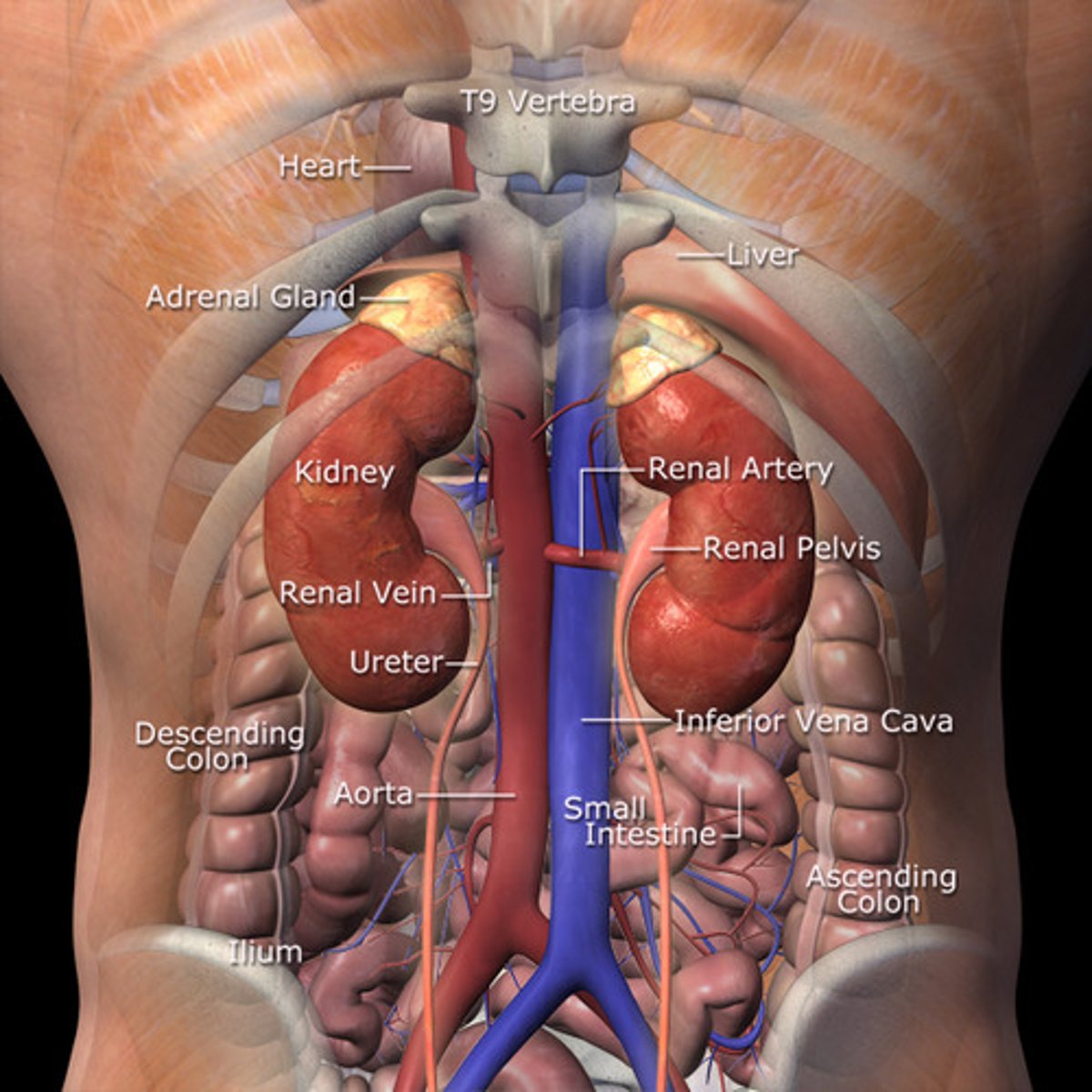
Kidney cut in half
Capsule (the like outline of everything)
Cortex
Medulla
Renal artery supplies the kidney with oxygenated blood
Renal vein takes deoxygenated blood away from the kidney
Ureter is where the urine is extracted from the blood and sent to the bladder
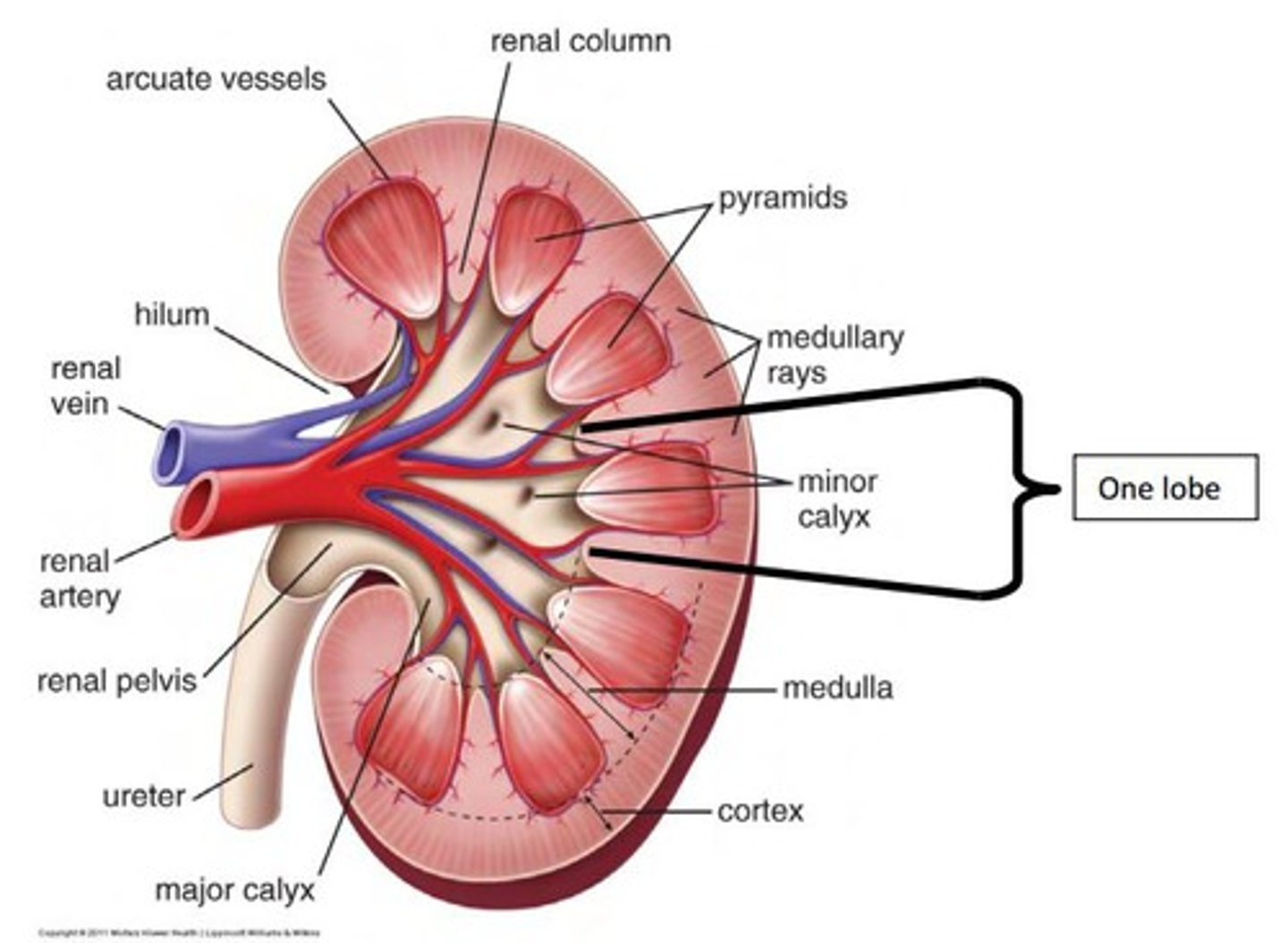

Dissection of a kidney
1. Renal cortex
2. Renal pyramids (the darker coloured bits in the medulla)
3. Renal columns (connecting the renal pyramids to the renal pelvis)
4. Renal papillae
5. Renal pelvis (white bit in the centre)
6. Ureter (the long tube thing)
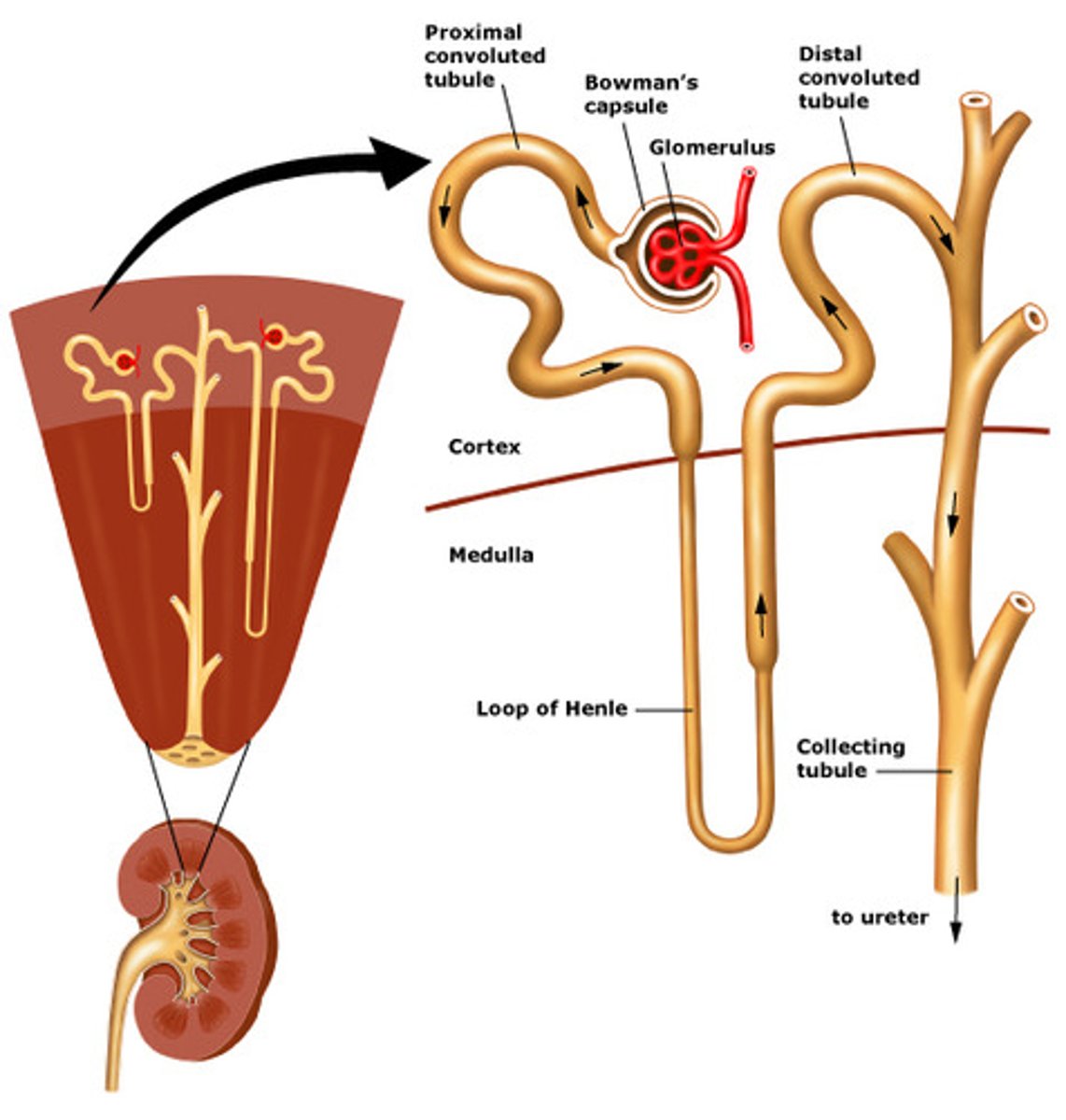
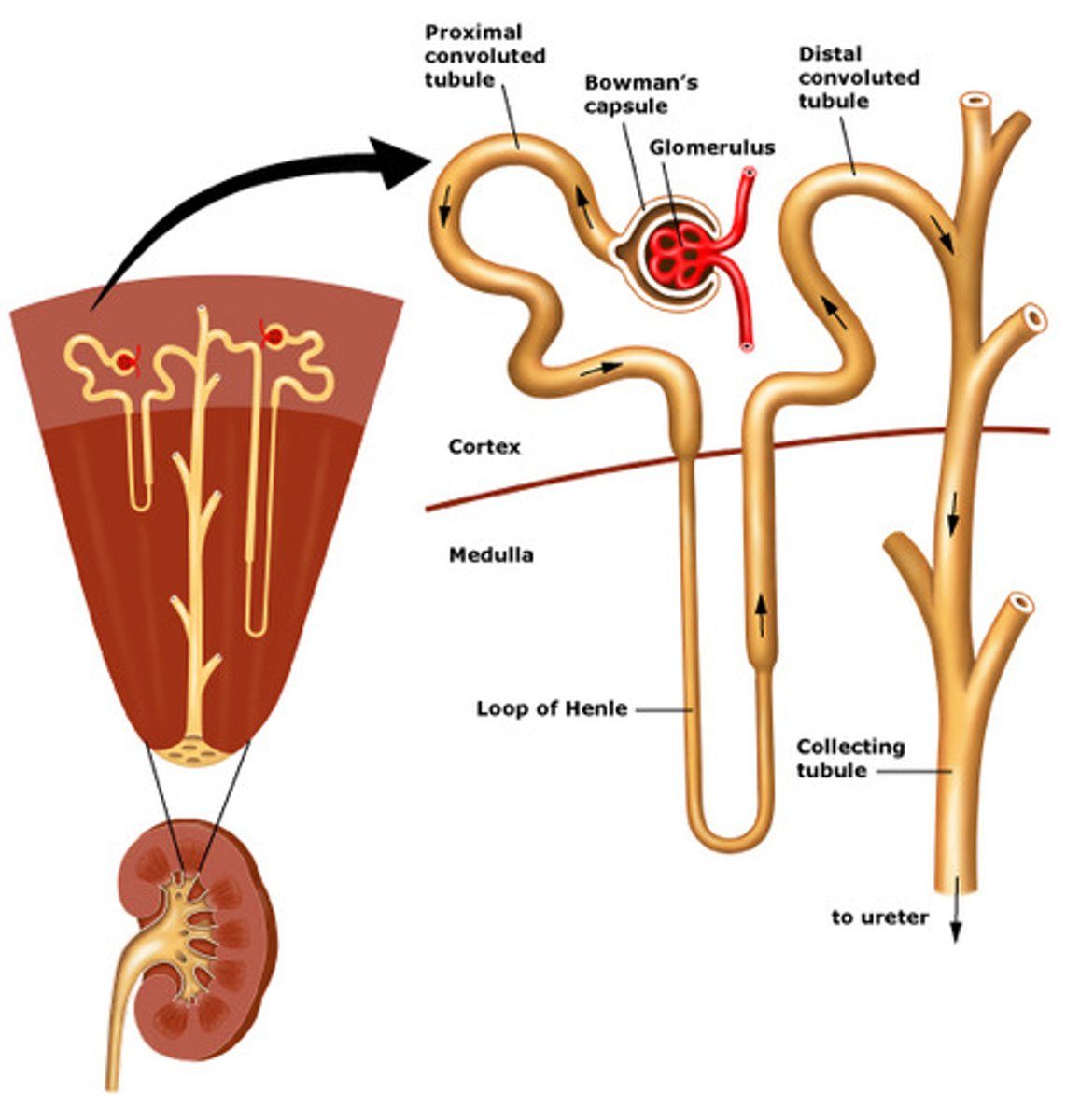
Name everything in a Nephron
1. Renal artery. Afferent arteriole brings blood into the glomerulus, efferent arteriole is where the blood leaves.
2. Glomerulus (a network of capillaries)
3. Glomerulus is inside the Bowman's capsule
4. Proximal convoluted tubule leaving the Bowman's capsule
5. Descending limb of Henle
6. Ascending limb of Henle
7. Distal convoluted tubule
8. Collecting duct
What occurs in the distal convoluted tubule?
It is involved in the regulation of blood pH as well as the concentration of particular ions in the blood
Nephron
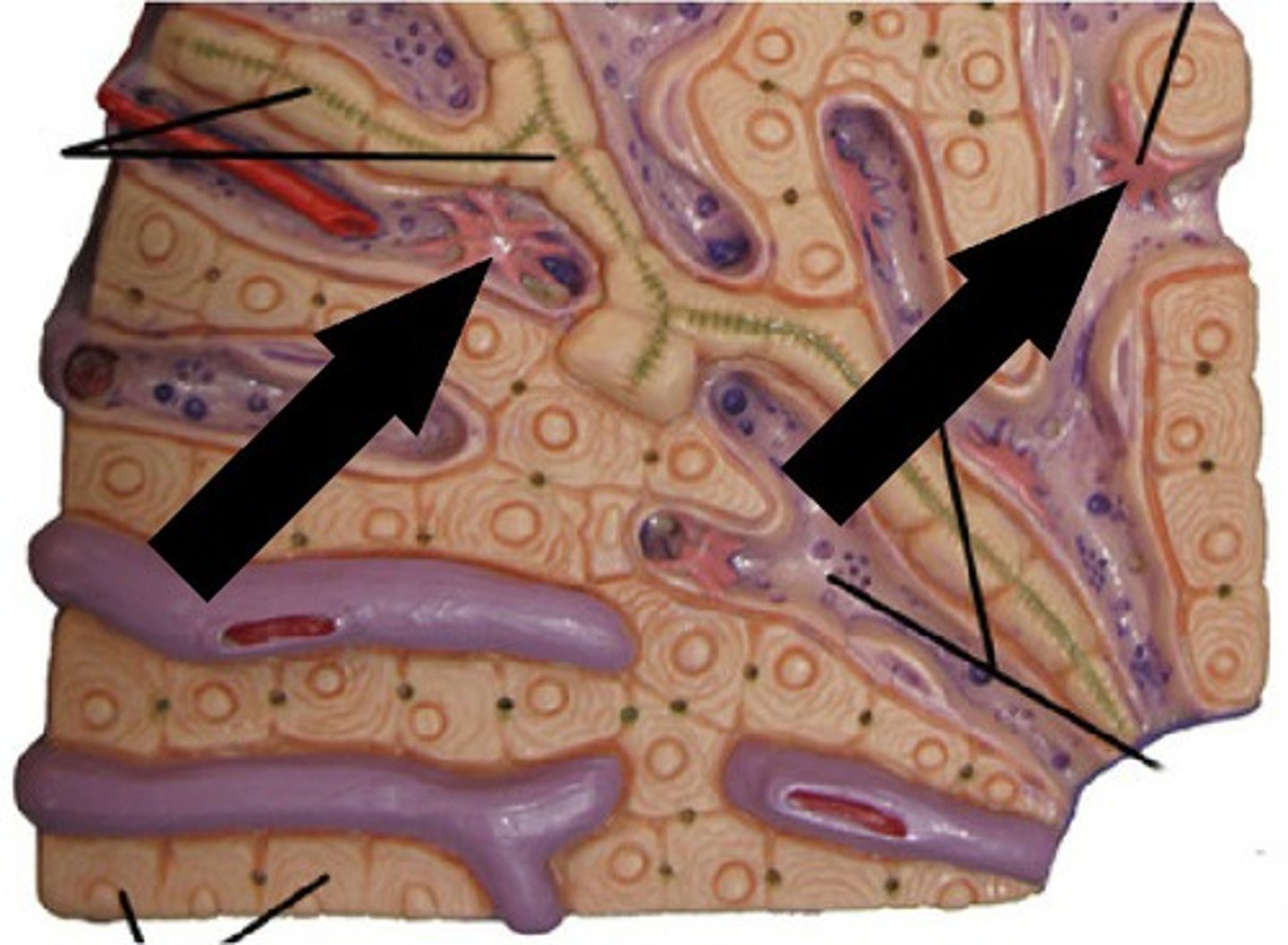
Nephron under microscope
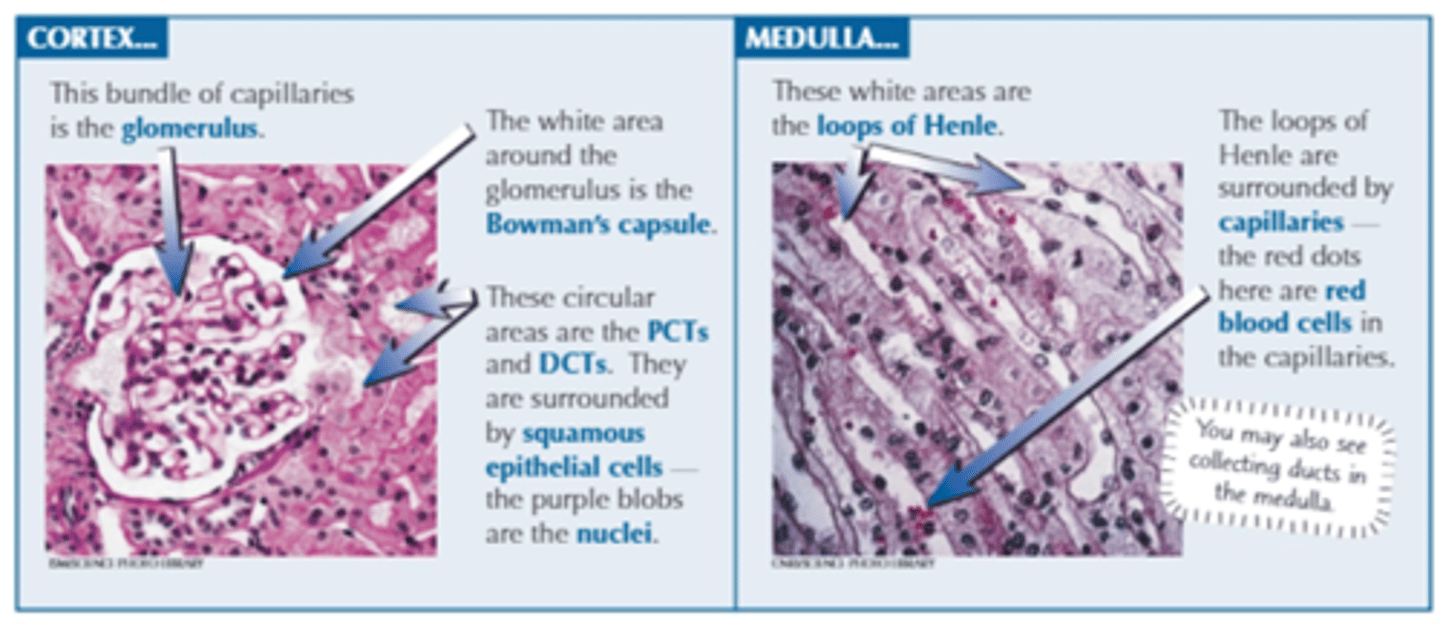
Exam tip when looking at kidney histology
In an exam question, if you have to identify the structure of the nephron under a microscope slide, check where the slide is taken from (either cortex or medulla)
If slide is taken from the cortex, it will have glomerulus, Bowman’s capsule, PCT, DCT, blood vessels
If slide is taken from the medulla, it will have collecting duct and loop of Henle
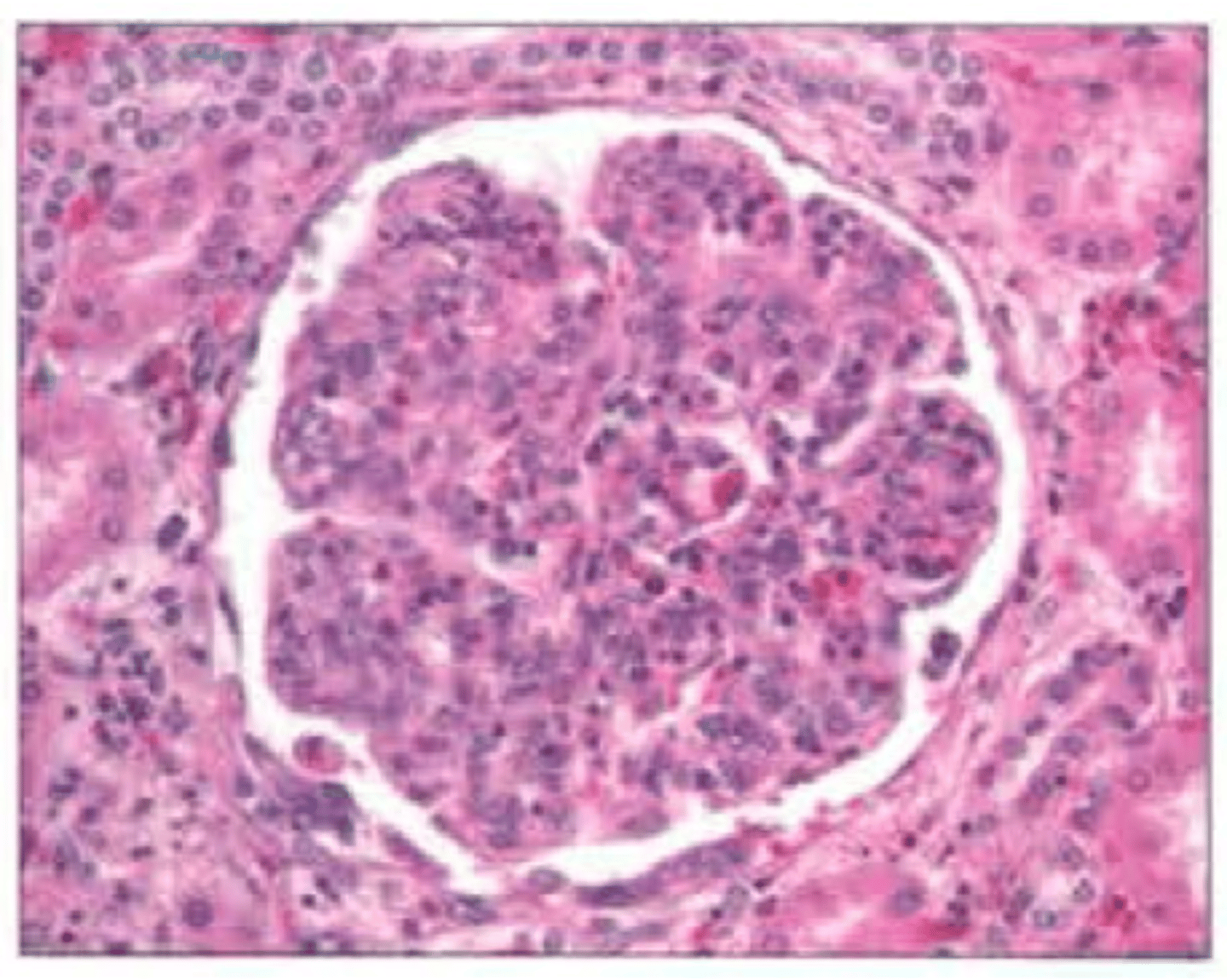
What’s in this image? It was taken from the cortex of the kidney.
Glomerulus (network of capillaries inside the Bowman's capsule)
Bowman's capsule (the white outline)
Things surrounding the Bowman's capsule could be the proximal convoluted tubule and/or distal convoluted tubule
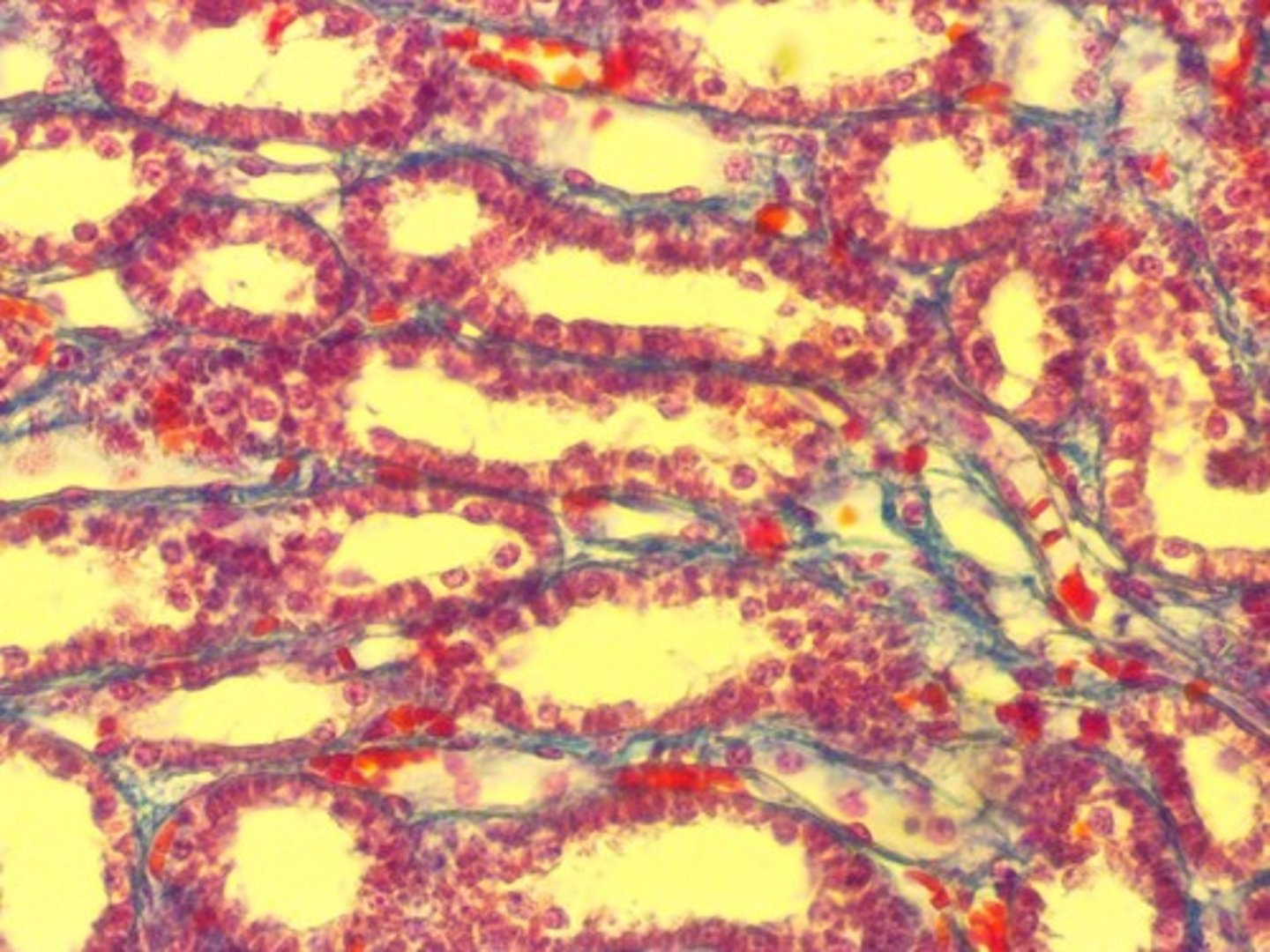
What’s in this image? It was taken from the medulla of the kidney.
Loop of Henle
Collecting duct
Urine sampling
Urine contains many waste products of metabolism. This can be tested and used to diagnose illness.
The presence of glucose in urine is a symptom of what?
Type 1 and 2 diabetes
What can urine sampling be used for?
Early diagnosis of pregnancy
Evidence for misuse of drugs
Pregnancy Testing
Uses monoclonal antibodies to test for the presence of hCG in the urine
Pregnancy Testing Process
The stick is dipped into urine to the line
hCG has a complementary shape to the monoclonal antibodies.
hCG binds to the monoclonal antibodies to form a "hCG antibody complex" which moves up the stick with the urine
The hCG complex binds to the immobilised antibodies (due to the complementary shape) in the lower band if the woman is pregnant
2 lines on a pregnancy test means =
the woman is pregnant
1 line on a pregnancy test means =
Just the control so woman is not pregnant
What molecules could be used to detect the presence of GH (growth hormone) in a urine sample?
Monoclonal antibodies
What are steroids derived from, and what do they do?
Derived from cholesterol. They are lipid soluble
They increase protein synthesis inside the cell
What are anabolic steroids?
Anabolic steroids stimulate anabolic reactions in the body. Large molecules are built up from smaller ones.
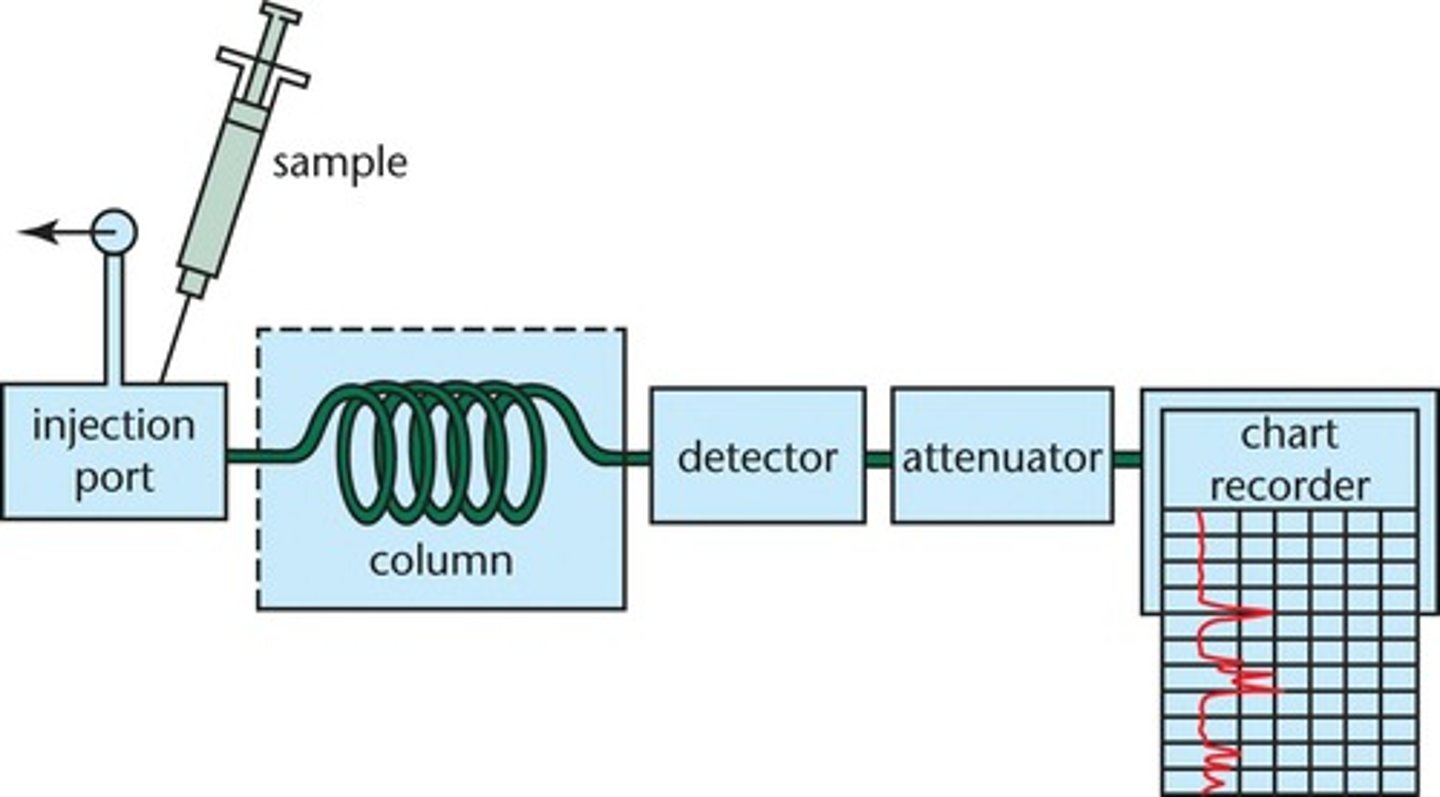
How are anabolic steroids normally detected?
Urine is passed through gas chromatography to create a chromatogram.
The chromatogram can then be read to show the presence of the drugs.
Why can urine be tested for drugs (including alcohol)?
Drugs and metabolites (breakdown products of drugs) are filtered through the kidneys and stored in the bladder. It is therefore possible to find drug traces in the urine some time after a drug has been used.
Drug testing from a Urine sample
The urine sample is first tested with an immunoassay using monoclonal antibodies to bind to the drug or its breakdown product
If this shows positive, it is then tested through a gas chromatograph / mass spec to confirm and determine which drug was used
What causes kidney failure?
Kidney infection, where the structure of the podocytes and tubules are damaged or destroyed
Raised blood pressure, damaging the structure of the epithelial cells and basement membrane of the Bowman's capsule
Genetic conditions such as polycystic kidney disease, where the healthy kidney tissue is replaced by fluid filled cysts, or damaged by the pressure from cysts
If kidneys are infected or affected by high blood pressure, what are the 2 effects?
Protein in the urine
Blood in the urine. Filtering process is no longer working here.
Why would there be proteins in the urine?
If the basement membrane or podocytes of the Bowman's capsule are damaged, they no longer act as filters and large plasma proteins can pass into the filtrate and are passed out into the urine
If kidneys fail completely, what happens?
The concentrations of urea and mineral ions build up in the body.
What are the 4 effects of kidney failure?
Build up of toxic urea in the blood
High blood pressure, causing a range of health issues like strokes
Weakened bones as the calcium/phosphorous balance in the blood is lost
Loss of electrolyte balance because the body cannot excrete excessive Na+, K+, and Cl- ions. This causes osmotic imbalances in the tissues, and eventual death.
How to investigate if a kidney is functioning?
Estimate a person's GFR
GFR stands for what
Glomerular filtration rate
What is creatinine?
A breakdown product of muscles

How is the rate of filtration measured?
A blood test measures the level of creatinine in the blood
If the levels of creatinine in the blood go up, then it's a sign the kidneys are not working properly
Why does GFR vary?
GFR decreases with age
Men typically have more muscle mass than women, so more creatinine
How do you treat kidney failure?
Dialysis
2 types of dialysis:
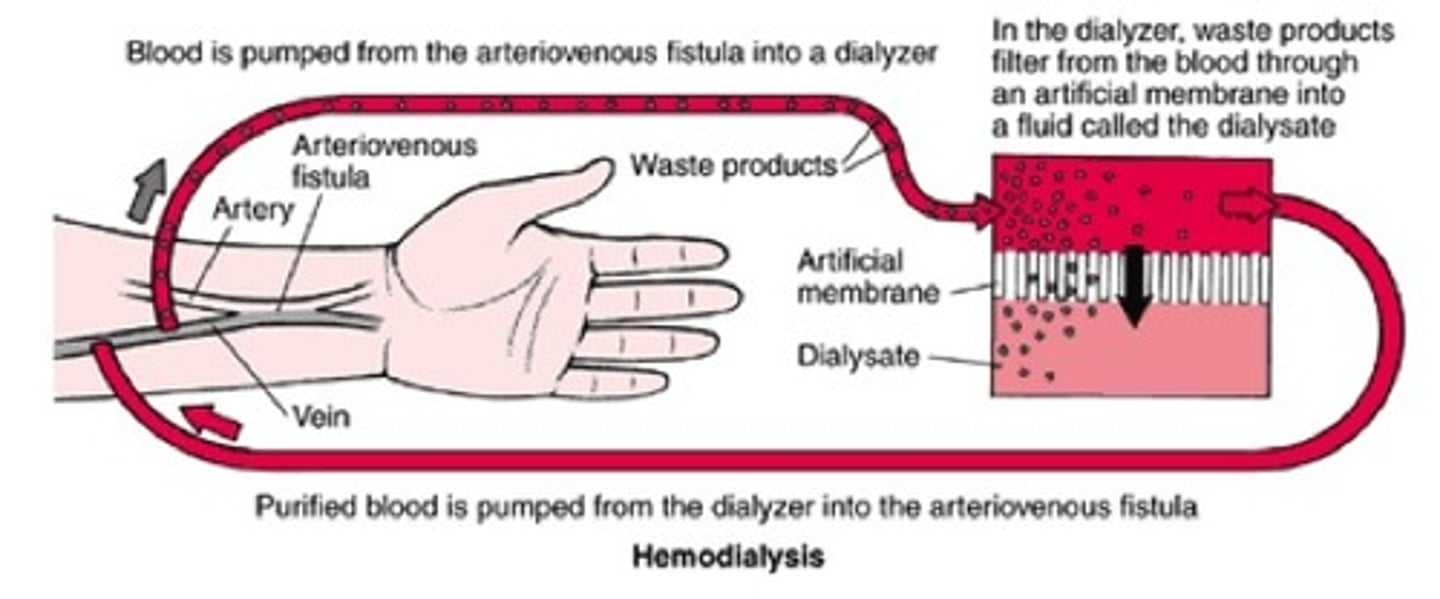
Haemodialysis
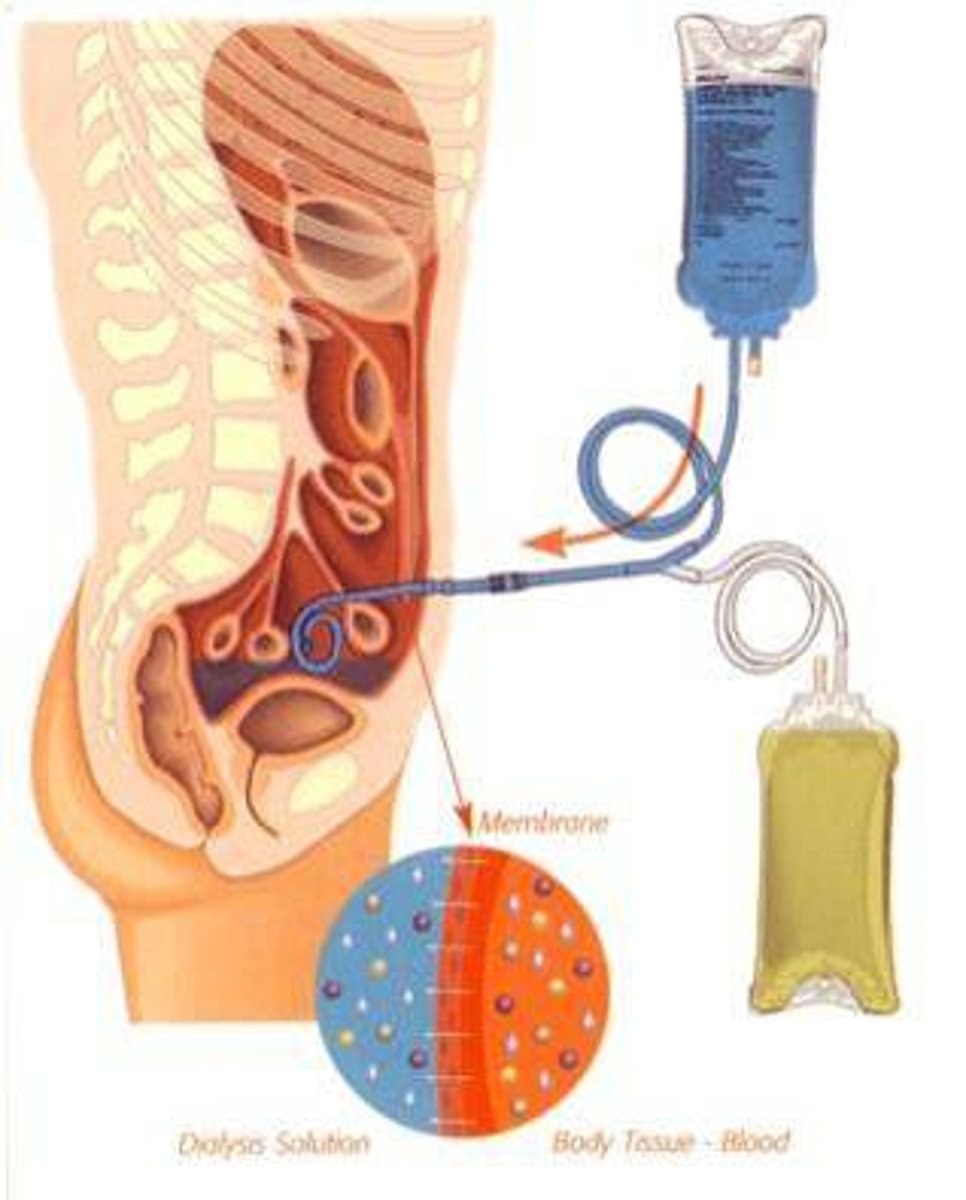
Peritoneal dialysis
Haemodialysis
Removes blood from an artery
Passes blood through a machine that filters out the urea and restores the correct water potential and ion concentrations of the blood
Returns the blood to the person's body into a vein.
Peritoneal dialysis
The abdomen has a lining called the peritoneum
Dialysis fluid is inserted into the abdomen through a catheter
It is left there for several hours, and urea and excess mineral ions pass out of the blood capillaries into the tissue fluid, and then out across the peritoneal membrane into the dialysis fluid
The fluid is then extracted from the abdomen
The water potential and ion concentration in the blood has been restored
How else can you treat kidney failure?
By transplant
Kidney transplants
A single healthy kidney from a donor is placed within the body
The blood vessels are joined and the ureter of the new kidney is inserted into the bladder
If the transplant is successful, the kidney will function normally
What are the issues with transplants?
Risk of rejection.
The antigens on the donor organ differ from the antigens on the cells of the recipient, and the immune system will likely recognise this, resulting in rejection and destruction of the new kidney
How to reduce the risk of rejection?
A donor kidney can be used with a same tissue type, similar to the recipient.
The recipient is given immunosuppressant drugs for the rest of their lives, suppressing their immune response and prevent rejection
Issues with immunosuppressant drugs
They prevent the patients from responding effectively to infectious diseases.
Pros of Dialysis
Dialysis is more readily available than donor organs and enables patients to lead a relatively normal life
Cons of Dialysis
Patients have to monitor their diet carefully and need regular sessions on the machine
Long term dialysis is much more expensive than a transplant, and can eventually cause damage to the body
Pros of Transplants
A kidney transplant means they are free from restrictions of regular dialysis sessions and dietary monitoring
Cons of Transplants
There is a shortage of donor kidneys