child abuse
1/89
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
90 Terms
any recent act or failure to act on the part of a parent or caretaker which results in death, serious physical or emotional harm, sexual abuse or exploitation; or an act or failure to act which presents an imminent risk of serious harm
child maltreatment (federal definition)
types of child maltreatment
physical abuse, sexual abuse, medical child abuse, emotional abuse, neglect (including supervisory, medical, educational, dental, physical, and emotional)
most common form of child abuse
neglect (74.3%)
what is more common, only having one type of abuse present or multiple kinds
one kind
if you do have a combination of abuse kinds whats the most common combo
neglect and physical abuse
most commonly abused age group
infants (most dependent on parents and less adults are involved in their care)
who is a mandated reporter
YOU are a mandated reporter, as is any personal engaged in the examination, care or treatment of persons
in texas EVERYONE is a mandated reporter, and you dont have to be a mandated reporter to report child abuse
when should you report child abuse
whenever you suspect a child is being physically/sexually abused or neglected
you do NOT have to know that abuse is definetely occuring
ways to report child abuse
phone hot line (no special number for medical ppl, just one number for all of tx) and a website (but takes 24-48hrs to be reviewed and is NOT good for cases of immediate danger)
things to do when you call TDFPS to report suspected child abuse
give as much info as you can (kids name and DOB, mom’s name and DOB, address w appt number, phone number, what your concerns are, name and DOB of other kids in the home)
can you get in legal trouble for reporting concerns for child abuse when there isnt any
no (immunity from liability)
can you get in legal trouble for NOT reporting concerns for child abuse when you knew about concerning signs
yes
is CPS reporting anonymous? is it confidential?
no longer anonymous (so CPS knows who you are and can contact you with follow ups or ask if youre a healthcare provider for extra validity) but still confidential (family wont know who called)
when is the only time you should NOT tell parents youre gonna call CPS (according to prof)
only dont tell them if you think itll put the kid or medical staff in risk of immediate harm, otherwise tell them
how should you tell families youre gonna report to CPS
straight-forward, non-judgmental approach, explain why, never use it as a threat
outcomes for abuse cases that are missed
return to same abusive environment, concern that perpetrator will escalate
acts of omission that cause intangible consequences (developmental delay) and often attract less attention
neglect
acts of commission that have tangible consequences (bruises, fx, etc) that evoke intense response from professionals, public, and media
abuse
what is the spectrum of neglect
optimal care (no neglect) to life threatening neglect (easier to spot, but less common) and then the middle area is most common
how do we identify neglect
ask if the caretaker did what is minimally necessary for safety, growth and development (not what is optimal or what you think they should do) (what is reasonable)
must cause or threaten harm
subtypes of neglect
physical (inadequate food, clothing, shelter, hygiene)
medical (failure to provide prescribes medical care or tx and/or failure to seek appropriate medical care in a timely manner)
supervisory (failure to provide age-appropriate supervision)
psychological/emotional (failure to provide nurturance/affection, psychological support, or allowing kids to use drugs/alc/other illegal activities)
exposure to domestic violence
potential causes of physical neglect
lack of resources, education, transportation, often present w “failure to thrive”
examples of medical neglect
asthma pt not being given their meds, T1D young kid being expected to handle ALL of their diabetes management too young, severe injury not being brought to the hospital
most common type of neglect
supervisory (depends on kid themselves, age, environment, length of time, circumstance, no offical legal age in texas)
examples of psychological/emotional neglect
kid expresses mental health issues/suicidal ideation and parents dont get them help, allowing kids to do illegal shit
if kids are in a home with domestic violence (or youre seeing an adult pt who is victim of DV) what do we need to watch for
kids in homes with DV are 15x more likely to be physically abused and neglected, 12% of kids present during DV get injured as well, consider where the kids are when the DV happens, if theyre at home/hearing it (psychological trauma), if theyre involved
if an adult pt in a DV situation comes in and they have kids need to call CPS
any non-accidental or inflicted physical injury including cutaneous injuries (bruises, abrasions, lacerations, and burns) and fractures/head injuries/abdominal injuries regardless of intention to cause harm
physical abuse
most fatal form of physical abuse, second most fatal form of physical abuse
#1 head trauma, #2 abdominal trauma (rare)
most common presentation of physical abuse, seen in over half of abuse victims
cutaneous injuries (mostly bruises)
a minor, detectable, and poorly explained cutaneous injury in infants, and often missed that leads to more/worse injuries (first signs, must catch early)
sentinel injury
common mechanisms for bruises
blunt force trauma, squeezing, crushing
common mechanisms for fractures
compression, bending, twisting
how are we evaluating injuries for potential abuse
figure out if the history lines up with the mechanism and if the history lines up with the development of the child (2wk old isnt rolling off the bed on their own)
check for other injuries and patterned injuries (accidental injuries are rarely patterened)
let the parent tell you how it happened and see if that mechanism lines up
if you dont cruise you dont ___
bruise
aka mobile kids (ones who can pull up and stand/walk) will have more bruises than non-mobile kids)
where is bruising concerning for abuse on an immobile infant
bruising ANYWHERE on an immobile infant (5mo or less) is concerning for physical abuse

what is this
congenital dermal melanosis (seen often in african american and asian infants, often on sacral-gluteal region, shoulder, flank, extremities or anywhere else)
described as a grey-blue macule with indefinite borders seen in first years of life and often disappears at about 3yo)
how do we tell difference between congenital dermal melanosis and a bruise
time (bruise will change in a few days, this wont), and document everything (can check old docs to see if this was seen)
bruise locations NOT concerning for abuse in mobile kids
forehead, nose, chin, elbows, forearms, hips, knees, shins (anterior bony prominences)
concerning bruise locations for mobile kids
torso (chest, abdomen/belly, back (except lower back on spinous process), genitals, butt (if spanking leads to injury lasting more than a few hrs its abuse)
ears
neck
frenulum (inside mouth, often from forceful insertion of an object and seen as its healing)
angle of the jaw
cheek (squishy part)
eyelids
subconjunctival hemorrhage (esp in infants, more normal in older kids/adults)
patterned injuries suggest
suggestive of an object, do not have to determine what the object is but can make generalizations about it (flat, textured, flexible)
how would you describe a bruise suggestive of a hand print
“multiple linear parallel bruises with sparing in between”
a cell mediated delayed hypersensitivity reaction to psoralens (found in lemons, limes, dill, figs, parsley, parsnip, carrots, celery, or the sun) that presents as an erythematous macule ± bullae that may blister and look like a burn, but it leaves a positive imprint (unlike a neg imprint bruise) and can last months-years
phytophotodermatitis
a common accidental injury that may be caused by trauma at base of the skull or forehead contusion that mimics an injury resulting from direct periorbital trauma from physical abuse
periorbital ecchymosis
what is key when evaluating for physical child abuse
history (if its absent, inconsistent w injury or child development, or has big changes those are all red flags)
most common agent for both accidental and abusive burns
scalding by hot liquid (often water)
what do abusive burns look like
most commonly from immersion in hot tap water, symmetric with sharp demarcations and usually without splash marks
what do accidental burns look like
smaller, less severe, without a pattern, and have irregular depth
most common skin infection worldwide, over 70% of impetigo cases and often caused by staph aureus, or group A beta-hemolytic strep. often on the face and needs a preceding break in skin and may have regional adenopathy
impetigo non-bullous
skin infection seen in infants and young kids that can look like a burn, caused by staph, and can be found anywhere on the body that does NOT need a preceding break in skin and hx will tell you the diff between a burn and this
bullous impetigo
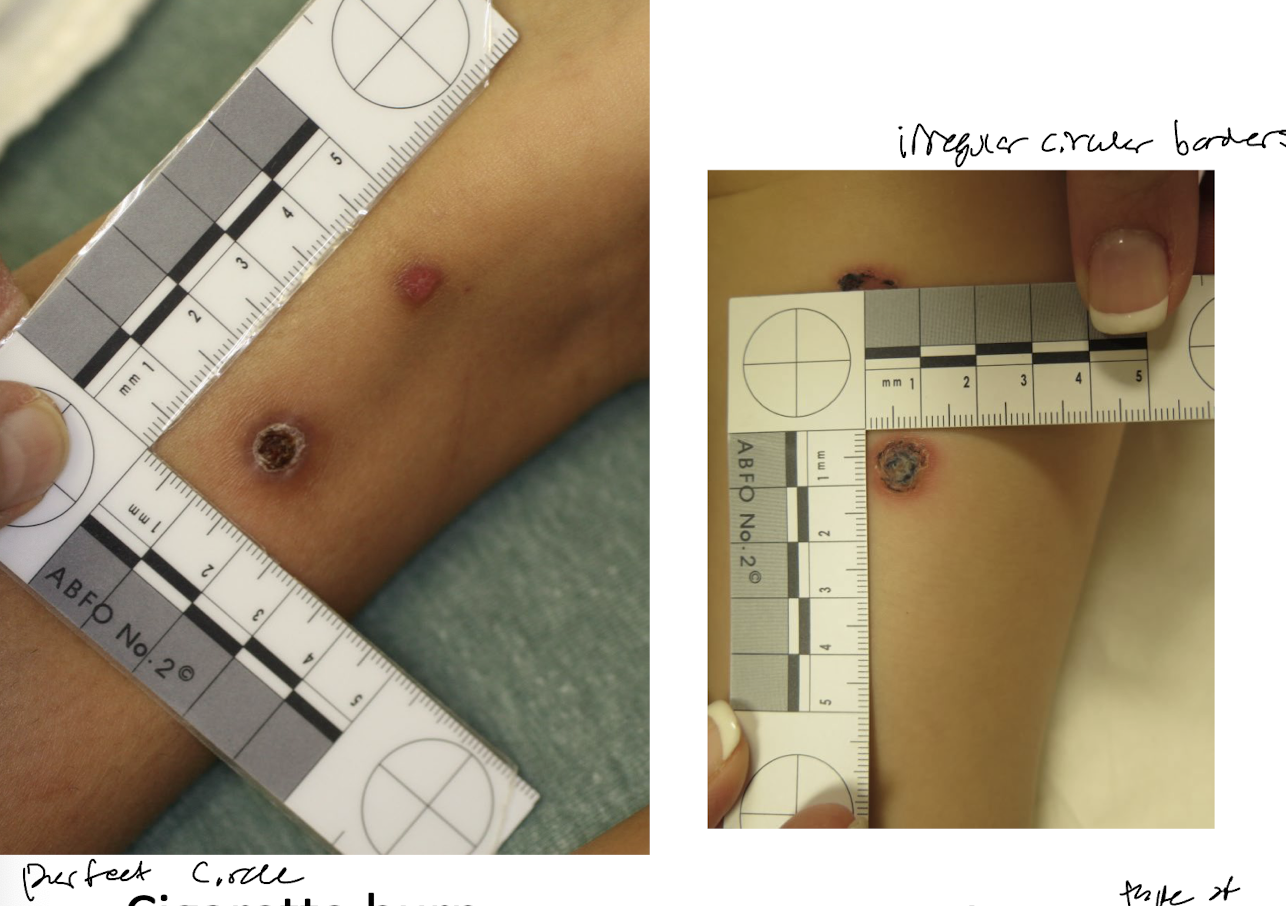
a skin infection that is ulcerative through the epidermis into dermis, with a “punched out” lesion, yellow crust, raised red borders and can look like a cig burn (but with slightly irregular circular borders)
ecthyma

burns aused by exposure of the skin to diarrhea, often w a hx of laxative ingestion or eating a ton of apples/takis etc, will have a diamons shaped lesion, linear borders lines up w diaper edge and sparing of skin folds
laxative induced burns
what do inflicted immersion burns on a baby butt look like
donut sparing shape and sparing behind knees

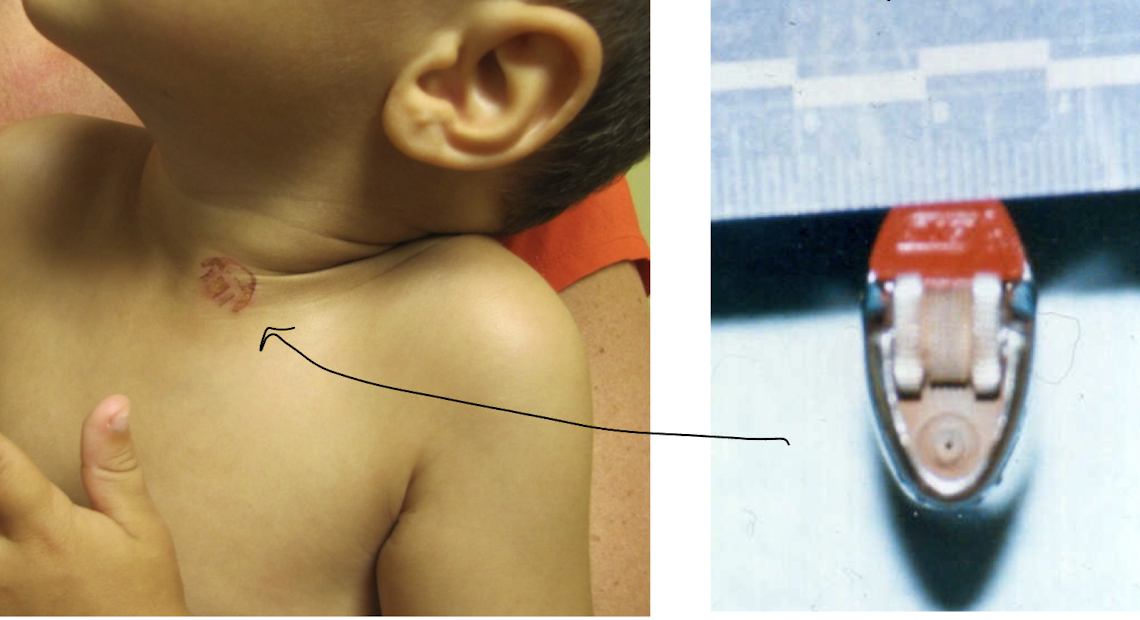
what is this burn from
a cig lighter (lighter must be heated for a while and must be held there to get this perfect shape and depth this shit is deliberate as hell)
___ fracture in a normal child of ANY age without a plausable accidental mech of injury
ANY (fracture type doesnt matter, all can be caused by abuse)
a spiral fracture requires what kind of force
twisting
a transverse fracture requires what kind of force
perpendicular force and high energy
a buckel fracture requires what kind of force
compression on axis
a oblique fracture requires what kind of force
twisting and bending
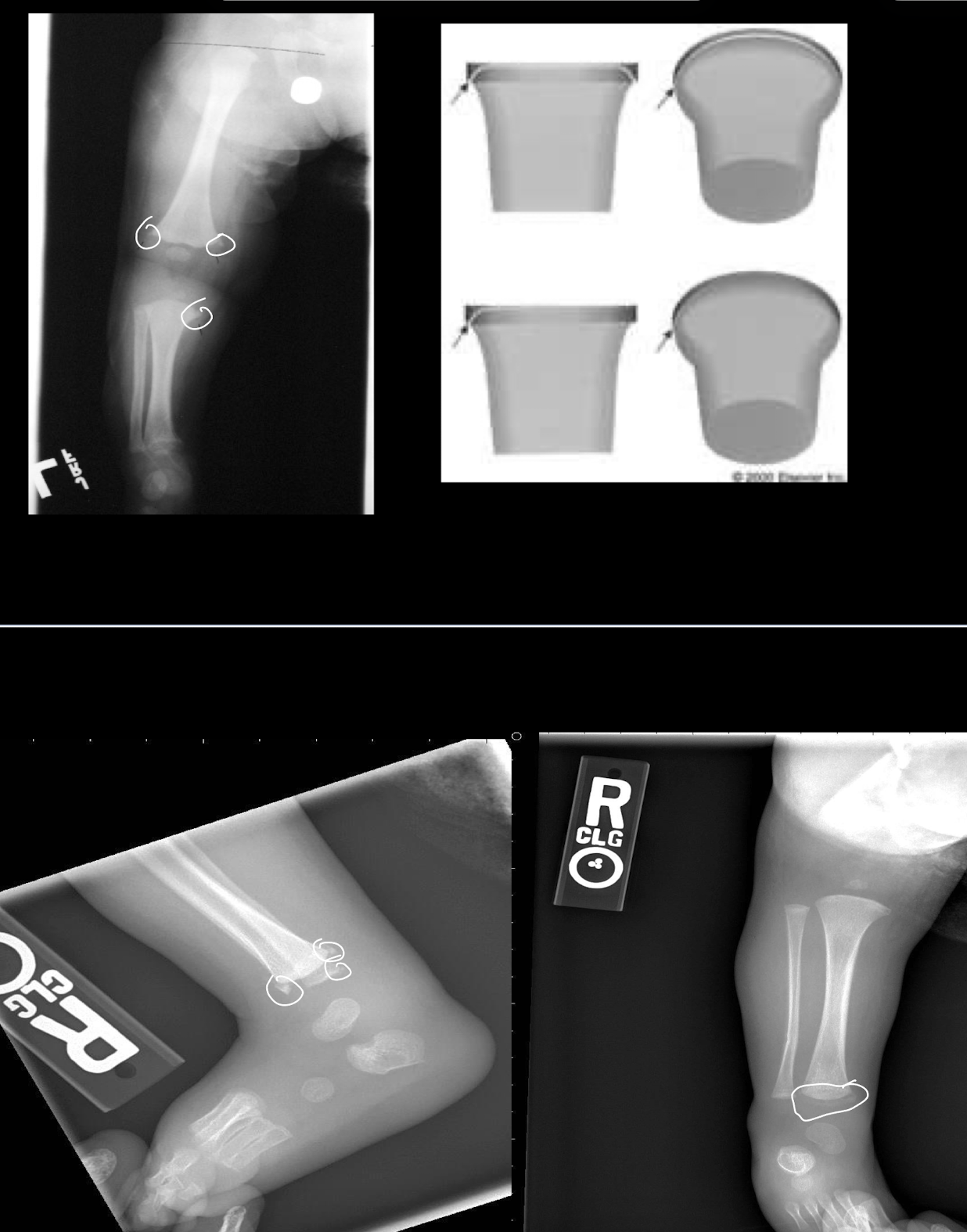
fractures with high specificity for abuse
rib fractures, esp posteromedial (from anterior-posterior rib compression) (easier to see as theyre healing rather than acute)
classic metaphysial lesions, but only under 18 months old
scapular fractures, spinous process fractures, or sternal fractures (bc all high energy)
a fracture occuring in the immature end of the bone from twisting/pulling/yanking/shaking that an infant cannot exert enough force to do on their own and should NOT be seen in normal parenting, and is not from a fall and is RARELY accidental (unless from club foot manipulation or in c-section delivery)
classic metaphyseal lesions AKA corner fractures AKA bucket handle fractures
common fractures in kids that are NOT specific for abuse
clavicular fracture (direct impact or FOOSH, caregiver may not even know its broken till they see lesion from it healing)
long bone shaft (most common fx in kids)
linear skill fracture (esp parietal skill, could be fall from sitting, doesnt need lots of energy)
injury to the skull or intracranial contents of an infant or young child (under 5yo) due to inflicted blunt impact and/or violent shaking
abusive head trauma
a whole head acceleration or deceleration (with or w/o impact) where because the head is tethered to the body by the neck the acceleration/deceleration is rotational
inertial head circumference
what is an additional vital sign for babies that can change in cases of abusive head trauma or other brain/head/csf concerns
head circumference (must document it well, and an increase in it warrants abuse workup)
presentation for abusive head trauma
varies a lot, including fussiness, vomiting, BRUE, macrocephaly, bulging fontanelle, facial injury, difficulty breathing, cardiac arrest
must do a FULL physical on presentation regardless of how theyre presenting
when does a child need further medical evaluation
any injury in a kid 0-6mo
any patterned bruises, lacerations, or burns (esp in kids 5 or younger)
kids that are non-verbal/speech delayed
widespread injuries (regardless of age) or severe injuries (including head trauma, burns, fractures, chest, abdominal injuries)
kid tells you theyve or someone saw them get hit in the face, hit with an object, whipped, punched, slapped, kicked, or beaten
kid looks malnourished or starved or demonstrated deprivational behaviors (eats out of trash, begs for food, hoarding food)
siblings or housemates of kids w serious injury or neglect (highest priority is infants under 2, then kids under 5, then other aged kids)
child seems to be intoxicated, drugged, or otherwise not normally responsive
what is the medical evaluation for abuse
complete history w allllll the details (medical hx, social hx too)
complete head to toe physical
photodocumentation
screening for occult injuries (complete skeletal survery in all kids under 24mo or 3-5yo if severe, series of 22 xrays looking at all bones) (LFT’s and abdomen/pelvic CT w contrast) (head CT w/o contrast for all kids 6mo or younger, → 3D recondstruction if real bad sx or polytrauma, brain MRI w/o contrast, ophthalmology exam if intracranial blood on CT)
test for bleeding disorders (CBC w platelet, PT/PTT, INR)
test for bone disorders (mg, phos, ca, alk phos, VitD)
employment, use, persuasion, inducement, enticement or coercion of any child to engage in or assist any other person to engage in, any sexually explicit conduct or simulation of such conduct for the purpose of production a visual depiction of such conduct. including the rape, and in cases of caretaker or interfamilial relationships, statutory rape, molestation, prostitution or other form of sexual exploitation of children or incest with children
sexual abuse
who is most likely to be sexually abused and when
girls (by a lot), more likely to be sexually abused or assaulted during their teen years than any other time in their life
myths of sexual abuse
perpetrators are strangers
perpetrators who sexually abuse boys dont sexually abuse girls
children tell about the abuse immediately
children tell fantasies
any child victim with penetration will have an abnormal examination
50% of children will have sexual behavior before age
13
things to consider when interpreting sexualized behavior and whether or not its appropriate
kids age, cognitive age (for those with developmental disabilities), observer’s feelings about normal behaviors, family sexuality/nudity, peers, access to porn
normal sexualized behaviors in children
self-stimulation, exhibitionism, behaviors related to personal boundaries
should be transient, respond to parental redirection, involve age similar children (exploratory and cooperative), and NOT coercive or aggressive
when does sexualized behavior in kids get concerning
no single sexualized behavior that indicated abuse, concerning sexualized behavior is often a part of other behavioral problems
factors that increase concern for child sexual abuse
sexual expression is more adult than child like, frequently disruptive to others, resistant to distraction, involves kids more than 4 years apart, sexualized behaviors involving others is physically aggressive, behaviors that involve coercion
how is sexual abuse detected
child tells someone (over 90%), someone witnesses it (rare), perpetrator confesses (rare), child has genital sx/sees a provider and injuries/STD is diagnosed (very rare)
what is the most important evidence that sexual abuse or assault has occured
the child’s disclosure
what to do if a child discloses sexual abuse to you
believe them and provide support!!!!
reassure
listen carefully
tell them they did the right thing by telling you
contain your emotional response
document what the child says, how the disclosure was elicited and the context
avoid direct or leading questions, do NOT conduct an interview
why kids dont disclose sexual abuse
not developmentally ready (acts werent “bad”)
psychological manipulation (threatened or bribed)
trapped and helpless
fears no one will believe
feel responsible, overwhelmed, guilt/shame
protect their parent/family (those who did it and those who didnt)
dissociation and repression
things to ask to see if the kid is safe (at the present moment at least) when talking to them about the sexual abuse
is the perpetrator in the home, are the parents supportive/will believe them, are they suicidal
myths of the hymen
girls can be born without it, its always injured with sexual contact, its not resilient, it cant heal, its presence is proof there has been no penetration, straddle injuries tear the hymen
the absence of ___ does NOT rule out the possibility of sexual abuse and/or penetration
physical findings
95% of cases with known sexual abuse have ___ physical findings
normal
why are normal physical findings in sexual abuse cases so common
depends on type of sexual abuse, tissue is stretchy and heals fast, there might be a long time between the abuse and disclosure
hymen appearance on physical in general
highly variable, can be crescent or ring shaped but NEVER absent at birth
estrogenized hymen characterisitcs
0-3yo and 9-10+ yrs
thickened, redundant, pale, flexible, can tolerate gentle touch after pubrety
unestrogenized hymen characterisitcs
3-9yo
thin, sharp, vascular, very sensitive and painful to touch
straddle injuries description
site of impact often anterior, external to hymen, unilateral, painful, may have significant bleeding, and occasional penetrating trauma to hymen with external to internal injury
non-specific findings that could be associated with abuse but could also be associated with other causes
erythema, labial adhesions, vulvovaginitis, anal fissures
if a child comes in with gonorrhea, chlamydia, syphilis, HPV, trich, HPV, or genital herpes what does that mean
either diagnostic or highly suspicious for abuse and needs reporting
(if its bacterial vaginosis thats inconclusive and needs medical follow up to determine if its abuse)