Pneumothorax
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
Fluid in the Pleural Space
Small amt of fluid in the pleural space that allows the lungs to move smoothly
Negative pressure
Extremely important because it helps to keep the lungs expanded and inflated
Pneumothorax definition
Increased amount of air in the pleural space that causes positive pressure in the lungs and can lead to lung collapse or respiratory distress
Air exchange will be the most effected
Open vs closed pneumothorax
Open: when there is an open wound in the chest wall, allowing air to enter the pleural space from the outside environment
Closed: when there is no open wound. Something is happening within the body that causes air (positive pressure) to enter the pleural space and collapse the lungs
Two types of a Spontaneous/Closed pneumothorax
Primary: usually occurs in healthy people
Secondary: usually occurs in people with an underlying lung disease
Air blebs in primary closed pneumothorax
Air blebs (bubbles) occurs on the visceral part of the pleura
Found most often in tall and thin people
Secondary to rupture of an air bleb (when the bleb ruptures, it is adding air to the space which is creating positive space and the positive space is causing the lung to collapse)
Why do blebs rupture?
Changes in air pressure (changes in altitude)
Sudden deep breaths
Smoking
not all blebs rupture and not all blebs rupture at once
Secondary closed pneumothorax and most common cause
Occurs with people with existing lung diseases that cause trapping of gasses and destruction of lung tissue
Most common cause: emphysema
Closed/Spontaneous pneumothorax solution
Can resolve itself
Tension pneumothorax
Occurs when air builds up in the pleural space with no escape route, causing increasing pressure on the lung and surrounding tissues/organs (mediastinal shift) due to a one-way valve effect
Can occur due to a penatrating or non-penatrating chest injury
Two aspects that effect the degree of the clinical manifestations
Size of the pneumothorax
Integrity of the underlying lung tissue (what was the state of the lungs before the pneumo occured)
Spontaneous clinical manifestations
Devel of ipsilateral (same side of the pneumo) chest pain
Tension clinical manifestations
Increase in RR (tachypnea) accompanied by dyspnea
Asymmetry of chest (will hear hyperresonace when percussed - like a drum bc of a air inside)
Breath sounds are decreased or diminished
Subcutaneous emphysema - means an accumulation of CO2
Hypoxemia (not enough O2 in blood or tissues)
How to assess for subcut emphysema
Need to inspect to see air bubbles on skin
Can also palpate the area and if it is present, you would hear a crunchy sound like rice crispies
Mediastinal Shift
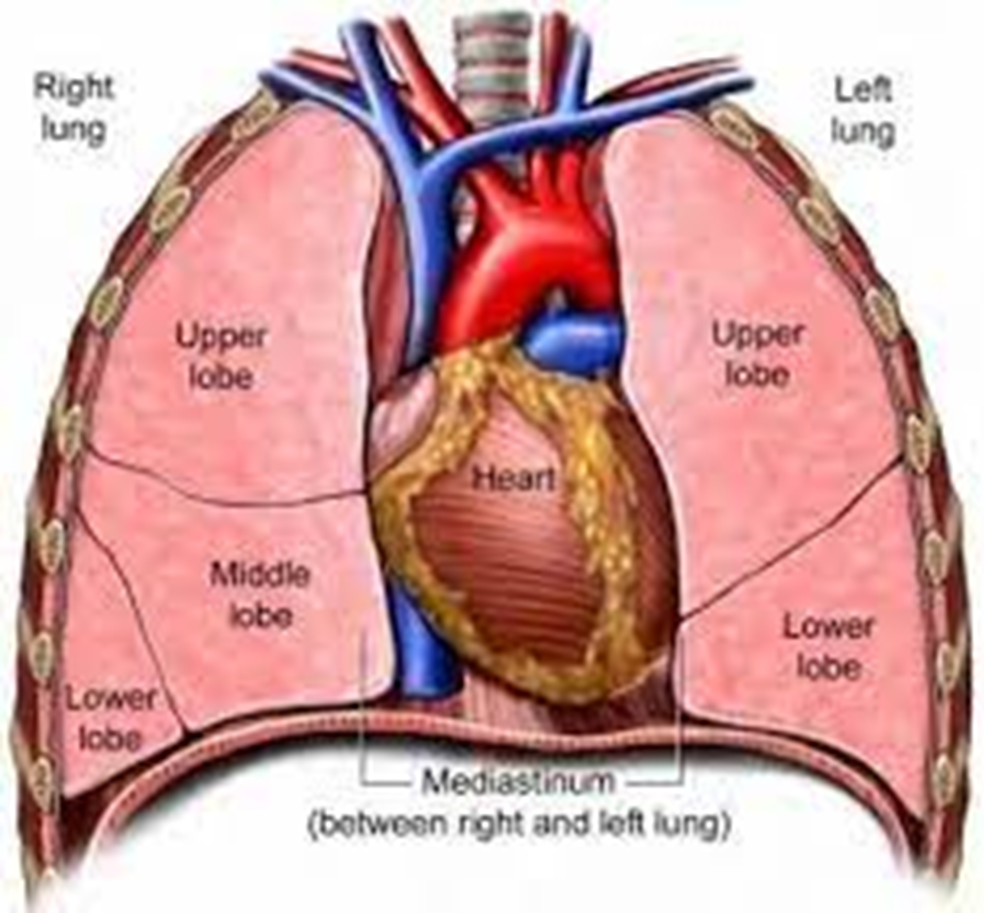
When the organs in the mediastinum shifts to the unaffected space due to increased thoracic pressure
Late and life-threatening sign
Occurs in tension pneumothorax
Trachea location during mediastinal shift + what it affects
Deviated to the opposite side of the collapsed lung
Affect air exchange and resp rate/rhythm
Seen on assessment (pulse ox) and a chest x ray
Heart location during a mediastinal shift + its affects
Deviated to the unaffected side
Stroke volume (amt of blood pumped out during a contraction) is reduced and CO is decreased
Vena cava during the mediastinal shift
It is compressed and decreased venous return
Jugular neck vein distention occurs
Mediastinal shift and pressure
Pressure is now being applied to the unaffected area due to the mediastinal shift
Pneumothorax diagnosis
History and Physical Exam
Chest x-ray
CT scan
Ultrasonography
Pulse ox
Blood gas analysis (expect to see a decrease in O2 and CO2)
Spontaneous treatment
Only requires observation and follow up chest x ray
Supplemental O2 may be used
Needle aspiration
Immediate treatment that removes the air
Allows air to escape from the pleural space, and the lung to re-expand
Needle aspiration details
A hollow needle with a catheter is inserted between the ribs and into the pleural space
Needle is removed and a syringe is attached to the catheter
Syringe is used to remove the excess air
Chest tube purpose
Drain the pleural space
Reestablish negative pressure
Allow for proper lung expansion
Chest tube details
Chest x ray is used to confirm the affected space
Area is cleaned with an antiseptic solution
Provider will use a local anesthetic and make a small incision over the rib
A tube is inserted into the pleural space and attached to a drainage tube to pull the air out
Provider sutures the tube in place and closes the incision with sutures
Nursing considerations to tell the patient about the chest tube insertion
Arm will be raised above the head on the affected side to expose the mid-axillary area
Elevate pt’s head of bed 30-60 degrees to lower the diaphragm and reduce the risk of injury
Chest tube insertion site recovery
Wound is covered with an occlusive dressing (dressing filled with petroleum (airtight) gauze)
What to monitor after a chest tube insertion?
Vitals - pay close attention to resp rate and rhythm
Assess the function of the closed drain system
Potential complications of a chest tube insertion
Infection
Hemorrhage
Injury to the lung
Most impt thing if you had a patient come in with a very clear pneumothorax?
Apply a gauze dressing and tape it over the open wound on three sides
Allows air to leave the wound (creates a flap)