Peds Exam 4 Concept Maps
1/84
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
85 Terms
no roomies
arthritis, muscular dystrophy
developmental dysphagia of the hips
abnormality of head of femur and acetabulum, frog legs are good, can be bilateral, cartilage turns to bone in 6 months, dysplasia -> subluxation -> dislocation
developmental dysphagia of the hips risks
girls, breech birth, multiple births, large baby, oligohydramnios, family history, swaddle methods
oligohydramnios
too little amniotic fluid
developmental dysphagia of the hips signs first month
clicks or clunks in ortolani maneuver (hips out) and/or Barlow maneuver (hips in)
developmental dysphagia of the hips signs older infant
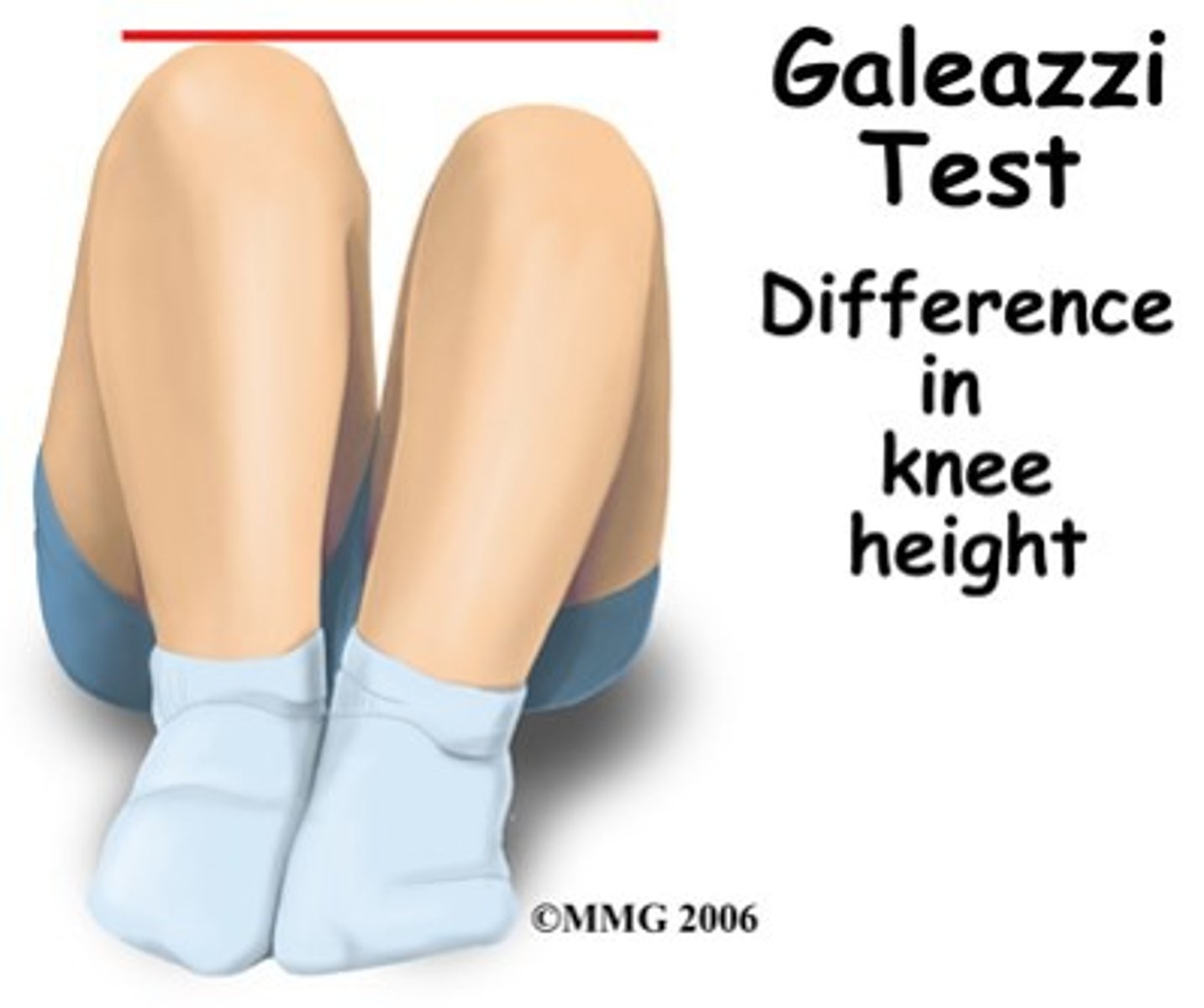
limited abduction, shorter leg, galeazzi sign, increased skin folds
galeazzi sign
developmental dysphagia of the hips signs older child
delayed walking, limp/gait, Trendelenburg sign (stand on one leg, look for droop)
developmental dysphagia of the hips diagnosis
Xray > 6mos, US < 6mos
developmental dysphagia of the hips treatment
<6mos pavlik harness for 3 months, parents dont adjust
if contracture, then bryats traction 102 weeks and then hip spica for 3 months
orthotic hip 1 year
developmental dysphagia of the hips considerations
cast care, skin tx care
juvenile idiopathic arthritis
chronic and autoimmune, genetic plus trigger, collection of diseases, exacerbations and remissions, normally resolves in teens
juvenile idiopathic arthritis symptoms
swelling, decrease ROM after rest or sleep and in AM, slightly warm joints, pain
juvenile idiopathic arthritis treatment
NSAID, DMARD - methotrexate or sulfasalazine, steroids, dont expose to sick people, encourage self care, pool exercises
sulfasalazine
sulfa allergy
methotrexate
risk for infection, use condoms
systemic arthritis signs
fever with ups and downs thats lower in PM, rash, spleen and liver enlarged, cardiac complications aka carditis
oligoarthritis signs
<4 joints affected, asymmetrical, uveitis/iridocyalitits (eye floaters and eye inflamation)
enthesitis
<4 joints, more common in boys, uveitis/spondylitis (joints of spine fuse and eye inflamation)
polyarthritis
can be RF + or -, >5 joints, symmetrical, affects large and small joints, long term joint problems
systemic arthritis labs
ESR/CRP - Pos
Increase WBC - pos
ANA - neg
RF - neg
HLA - neg
Oligioarthritis and enthesitis labs
ESR/CRP - pos
Increase WBC - neg
ANA - pos
RF - neg
HLA - pos
polyarthritis labs
ESR/CRP - pos
Increase WBC - neg
ANA - pos
RF - pos or neg
HLA - neg
ACL sprain
doesnt repair self, tear of ligament, hx of injury with "pop"
decrease ROM function and increased pain
RICE, will have OR repair and crutches for 3-4 weeks
SCFC
hip problem, head of femur displaced from neck, > boys, bilateral, puberty, tall or high BMI
pain, limp, external rotation of leg, decrease ROM
bucks traction, no ambulation, no weight-bearing postop, no contact sports until 20's
Surgery has risk for shorter limb, osteomyelitis, osteoarthritis
Legg-Calve-Perthes Disease
hip problem, head of femure has blood supply problem, becomes mushy, 4-8 YO, >boys, bilateral
insidias limp/pain, decrease ROM, +/- external rotation
no wt bearing, NSAIDS, Hip spica for 2-4 years OR surgery and hip spica for 3 months
Surgery has risk for shorter limb, osteomyelitis, osteoarthritis
Osgood-Schlatter disease
tendonitis, overuse injury (running or jumping)
knee bump and pain, no redness, +/- bilateral
change sports, rest, ice, compression no elevate
osteomyelitis
can be from SCA, salmonella, MRSA, staph, self infection generally or open fracture, happens in school age kids
increase temp, swelling, pain, redness, wamth, decrease function appetite and fluids, increased WBCs CRP and ESR
ABX 6wk-4mos, picc line, no wt bearing, check CRP/OSR, splints and casts
Osteosarcoma
bone tumor, teens - 20's, >Boys, mets to lungs
pain, swelling, decrease ROM, limp, decrease appetitie
sunburst xray
increase in calcium phosphorus and alkaline phosphate in blood
surgery, biopsy, chemo NO RADIATION, implanted CVC, no wt bearing
spina bifida
congenital neural tube defect, multifactorial, low folate in pregnancy, >white and hispanics, maternal diabetes obesity and fever increase risk, have latex allergy
Spina Bifida oculate
meningocele
mylomeningecele
signs of increased ICP in infants
respiratory problems, caugh, not move shoulders, cant use nipples, stridor
spina bifida oculate signs
has dimple on back with tuff of hair, +/- tethered cord, +/- infection
meningocele signs
sac on back without cord, +/- tethered cord, +/- infection
mylomeningecele signs
sac on back with cord, any nerve below is paralyzed, keep sac intact until OR, risk for infection (look for instability of temp), increase ICP = Chiari malformation
increase risk for seizures, constipation, UTI, neurogenic bladder
chiari malformation / increase ICP treatment
VP shunt
spina bifida considerations
bowel management program, self cath, check VP shunt for infection and blockage
spina bifida complications
club feet, hip dysplasia, contractures
spinabifida treatment
OR 12-72 hours, position on abd, no diaper, damp cloth, check head circumference and fontanel, +/- seizure meds
Duchene Muscular Dystrophy (DMD)
progressive degredation, x linked boys, girls are carriers always, death in early 20's by heart or lung problems, starts in feet and moves up, missing dystrophin protein, "woody" feeling muscles
increase in age decrease in moblility
Duchene Muscular Dystrophy (DMD) signs infants
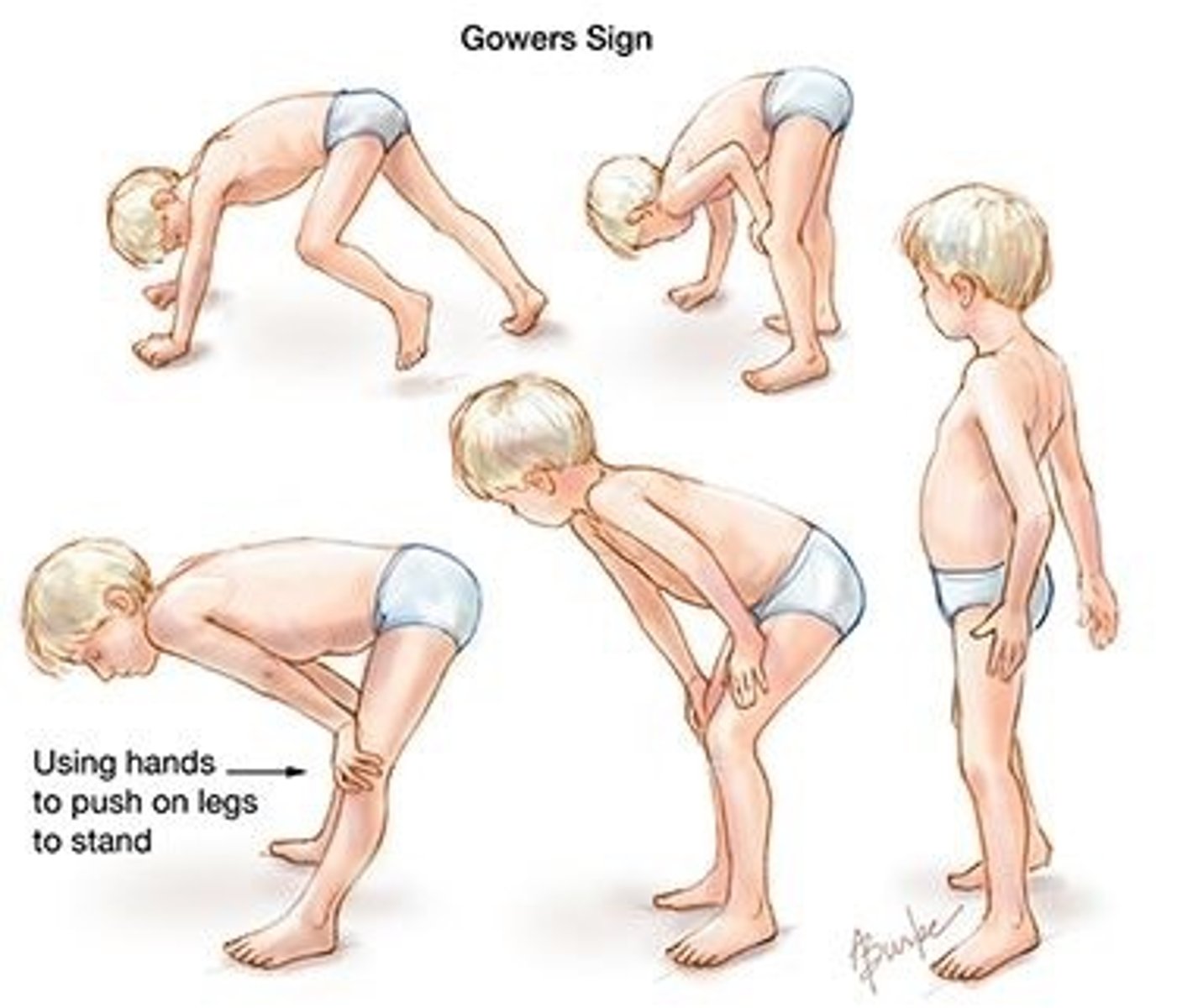
delayed, 3YO stumbles and falls often, no running or climbing, + grower sign, big calves
grower sign
Patient uses upper extremities to help stand up
Classically seen in Duchenne muscular dystrophy, but also seen in other muscular dystrophies and inflammatory myopathies (polymyositis)
Duchene Muscular Dystrophy (DMD) 12 year old + signs
wheelchair bound, muscular wasting, increase obesity, contractures, cardiomyopathy -> CHF, decreased verbal cognition
Duchene Muscular Dystrophy (DMD) diagnosis
CPK/CK, PCR, prenatal, EMG - keeps track of how muscles are functioning
Duchene Muscular Dystrophy (DMD) treatment
roids (watch for increase wt), ROM respiratory and mild strength exercises,bipap, vaccines, no roomies, avoid sick people, check for CHF, independent living, bowel management program, check for skin breakdown
Cerebral palsy
non progressive problem, prenatal event such as infection, genetics, decrease O2, prmie, exposure to drugs
Cerebral palsy problems
motor, vision.hearing, seizures, cognition, language, GER
Cerebral palsy signs newborn
floppy/hypotonic, decrease feeding and reflexes, not symmetrical, +/- irritable
Cerebral palsy signs infant
spastic, arch back, irritable, developmental delay, change oin mobility,
lack of:
3mos
head control
hand open reflex
social smile
6mos
spoon feeding -> push spoon out
clothing self
8mos
sit on own
Cerebral palsy treatment
speech therapy, PT, botox - relaxes muscle, baclofen (muscle relaxant), diazepam/valium (muscle relaxants), OR for tendon release - risk for hip dislocation or scoliosis, dental/oral care
neuroblastoma
cancer of sympathetic nervous system (fight or flight), starts in adrenal medulla, mets to lymph nodes, bones, liver, ABD mass similar to wilms tumor
neuroblastoma staging
1 - local
2 - unilateral
3 - past midline
4 - mets
4s - <1yo
neuroblastoma signs
large abd mass, bulging eyes, bruises around eyes, neck lumps, airway obstruction, blueberry skin, increased wt loss and fatigue
increase BP and temp
decreased plts, RBCs, WBCs
large liver
neuroblastoma labs
n-myc, MIBG scan, urine for VMH and HVA
neuroblastoma treatment
stage 1 and 2 - OR and chemo
stage 3 and 4 - OR and chemo with biopsy and radiation
vitamin A and retin A
medulla blastoma
aka brain tumor, infratentorial, in cerebellum, mets to spinal cord
medulla blastoma signs
increase IOP, headache, vomiting, clumsy, change in LOC, fatigue decrease appetite, C/O x2 vision, head tilt, bulging fontanels, papiledema
increase BP
Decrease Hr and RR
medulla blastoma treatment
OR, chemo, and radiation
postop - ICU with coma, check airway circulation dressing and reflexed, clear drainage on dressing bad, cooling blankey, +/- VP shunt
position flat and on side, stool softners, no suctioning, tylenol for HA, low stem enviroment
manitol to decrease ICP
less fluid than segars
meningitis
inflammation of brain coverings, bacterial (H. flu, s. pneumonia, N meningitis) or viral, transmitted by nasopharyngeal secretions
prevention of meningitis
vaccines
meningitis diagnosis
lumbar puncture, viral has normal glucose and protein, bacterial has low glucose and high protein because bacteria eats sugar and dies protein
meningitis signs bacterial
fever, chills, vomiting, change in LOC, photophobia, nuchal rigidity (kernig and brudzinski signs), DIC and septic shock - late stages
meningitis signs neonate viral
increase fontanel and head circumference, temp unsteady, decreased feeding, change in respiration, decrease muscle tone, diarrhea
meningitis signs infant viral
fever, decreased feeding, increase fontanel and head circumference, high pitch cry, jaundice
meningitis treatment bacterial
ICU, isolation for 24hr worth of abx, cephalosporin, roids (decadron), mannitol (decrease ICP), HOB 15-30 degrees, no suction, low stim, no pillow, side lying, tylenol for HA
meningitis treatment viral
start like bacterial, when cultures come back viral, then dc abx and isolation and remove from ICU
explain to parents less severe
epilepsy
>2 episodes of seizures
status epilepticus
>30 min seizure
seizure > 5 min
emergency
seizure causes
infection/fever, brain bleed, tumor, metabolic function, meds/drugs/toxins, decreased O2, lytes off
partial seizure
simple or complex
general seizure
tonic/clonic, absence, atonic
not a seizure
fainting, breath holdings, tics, migrains, sleep disorders, arythmias
seizure questions
onset, description, family history, family hx of early death, prenatal development
simple partial seizure
no loss of consciousness, good prognosis
complex partial seizure
has aura, change in LOC, lasts longer than simple, poor prognosis
tonic/clonic seizure
+/- aura, change in LOC, fall, sleepy, check airway, increased secretions
Absent seizure
change in LOC, "day dream", motor ability ok, no aura, 5-10 seconds
atonic (drop) seizure
no aura, no motor control, helmet needed, fall to floor
infatile spasms
baby has intense jerking
febile seizure
1mos-5 yr, fever, outgrown
seizure tx home
rectal valium, if repeat seizure than seek help
seizure tx hospital
lorazepam IV/buccal, diazepam IV/rectal, midazolan/versed IV IM PO buccal
>30 mins -> dilantin/phenobarbital
seizure assessment
check airway, side lying, O2, record seizure, VS and neuro check after, look for cause, provide privacy
seizure considerations
rest at school, no swimming w/o supervision, helmets always, no climbing
seizure prevention
2 years no episode then ween off med, meds, keto diet, vagal neurostimulation