12 Cardiac Pathophysiology
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
What determines blood pressure?
Cardiac output
Vascular
Blood volume
Regulation by CNS and Endocrine systems
What is the function of the heart?
Pump blood, creating hydrostatic pressure to perfuse the body
Endocrine organ: secretes Atrial Natriuretic Peptide (causes kidney to add salt into urine to decrease BP and is a vasodilator)
How does the heart affect blood pressure?
By increasing cardiac output, the heart can increase blood pressure. To decrease BP, the heart decreases its output.
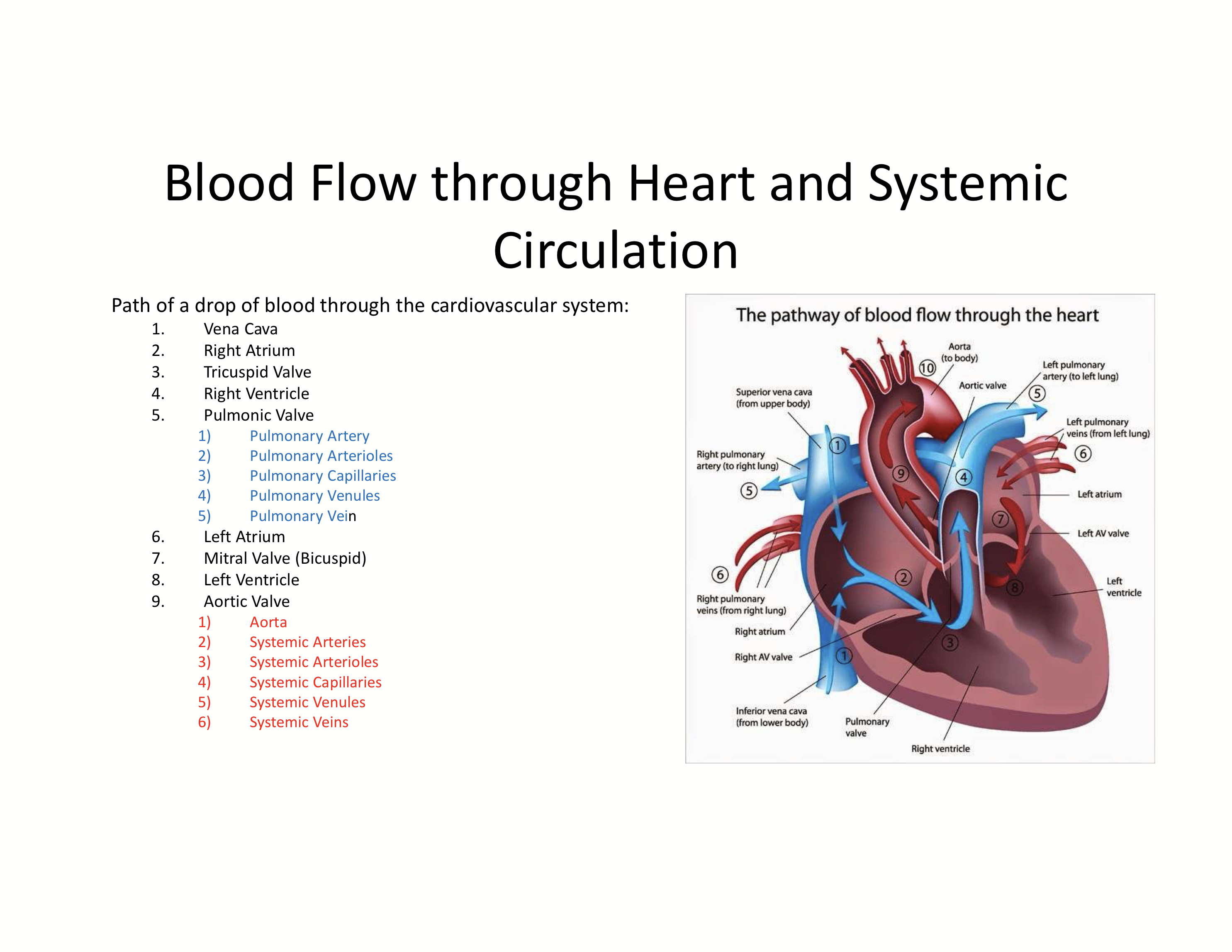
What is the path blood travels through the cardiovascular system starting at the vena cava?
Vena Cava → Right atrium → Tricuspid valve → right ventricle→ pulmonic valve → pulmonary artery → pulmonary arterioles → pulmonary capillaries → pulmonary venules → pulmonary vein → Left atrium → mitral valve (bicuspid) → left ventricle → aortic valve → aorta → systemic arteries → systemic arterioles → systemic capillaries → systemic venules → systemic veins
What is the purpose of the valves?
To produce a one-way blood flow and slow electrical conduction to allow proper ventricular filling.
How does valve create a one-way blood flow?
Leaflets open and close based on pressure
Papillary muscles contract with the chamber to prevent prolapse and regurgitation
What are the valves made up of?
Connective tissue, they are a part of the fibrous skeleton
Where are the papillary muscles connected to?
The valve flaps and the heart muscles to prevent valve inversion. It is connected to the valve leaflets by chordae tendinae.
What are the layers of the heart?
Endocardium: continuous with endothelium
Myocardium: pacemaker cells and cardiac myocytes
Pericardium or pericardial sac
Visceral pericardium: contains coronary arteries and veins
Parietal pericardium
What are the functions of pacemaker cells?
Set heart rate = chronotropy
Exhibit automaticity, bringing themselves to threshold via voltage-gated channels
How are pacemaker cells organized?
Sinoatrial nodes (SA) around the atriums with 100 betas/min; With vagal brake = 70 bpm
Atrioventricular node (AV): 40 bpm
Bundle of His: Transmits electrical impulses from AV to ventricles
Purkinje Fibers: ensure the ventricles contract simultaneously
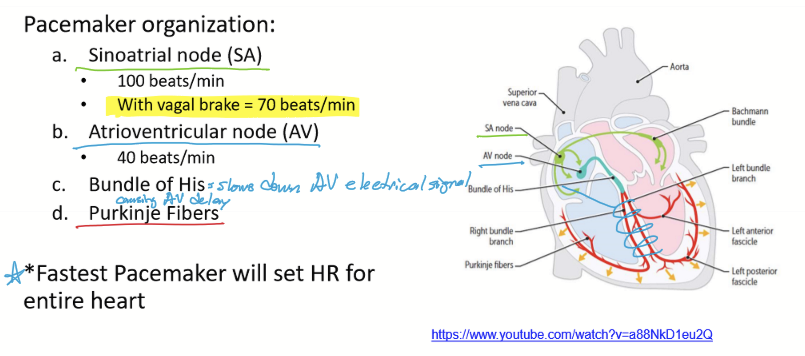
How does the impulse propagate?
SA nodes causes atrial myocyte depolarization and contraction
AV delay, slowing conduction of AP through node allows the ventricles to fill
Bundle of His and Purkinje fibers cause depolarization of ventricles and contraction
What are the phases of an AP of pacemaker cells?
Pacemaker potential brings cell to threshold: funny channels = Na influx = funny current; transient calcium channel opens at end = Ca influx
Depolarization phase from DHPR channels/L-Type Ca Channels = Ca influx
Repolarization Phase from K Channels = K efflux
Immediately begins pacemaker potential: no static rest
How are pacemakers regulated?
ANS regulates HR/chronotropy
SA and AV nodes under reciprocal control:
SNS = B1 adrenergic receptors: Increases effect/HR
PNS = M2 receptors: Decreases effect/HR
How can chronotropy be increased/positive chronotropy?
B1 stimulation by SNS/agonist
M2 blocker
Thyroid= High T3/T4 causes increase in B1 receptors
How can chronotropy be decreased/negative chronotropy?
B1 Antagonist/blocker
M2 Agonists
T3/T4 is low, causing a reduction in B1 receptors
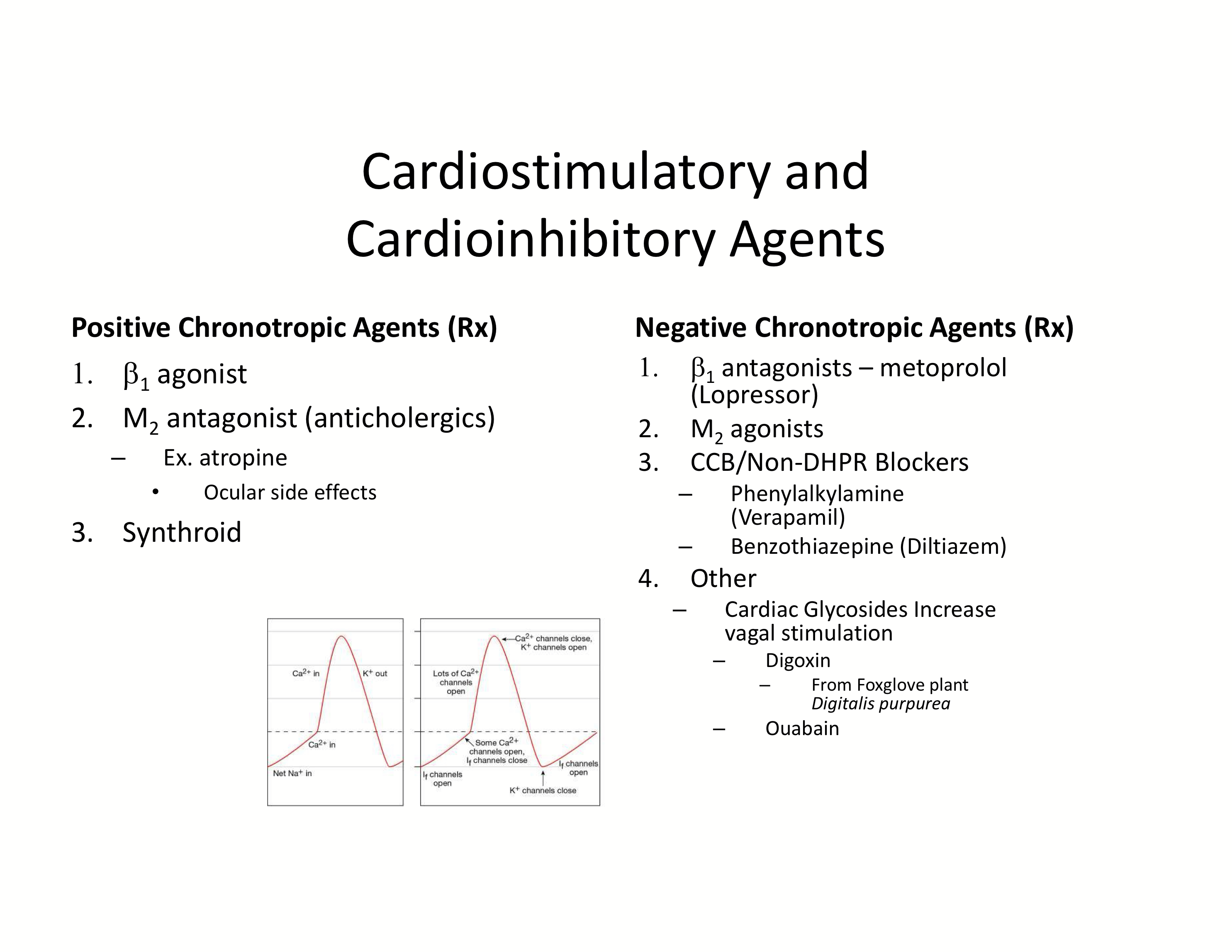
What are some Rx to change chronotropy?
Positive Chronotropic Agents
Beta1 agonists
M2 antagonists (anticholergics): Atropine (causes mydriatic iris)
Synthroid
Negative Chronotropic Agents
Beta1 antagonists: metoprolol (Lopressor)
M2 agonists
CCB/Non-DHPR Blockers: Phenylalkylamine (Verapamil) for cardiac specific; Benzothiazepine (Diltiazem) for cardiac and vascular
Other: Cardiac Glycosides to increase vagal stimulation: Digoxin and Ouabain
What are the differences between skeletal fibers and cardiac myocytes?
Cardiac myocytes are mononucleated, branched with intercalated discs full of gap junctions for electrical synapses, and regulated by the SNS
How does the SNS affect the cardiac muscles?
An increase in SNS innervation causes an increase in contraction force. A decrease in SNS innervation causes a decrease in contraction force.
What does the cardiac myocytes excitation-contraction coupling include?
And action potential and twitch.
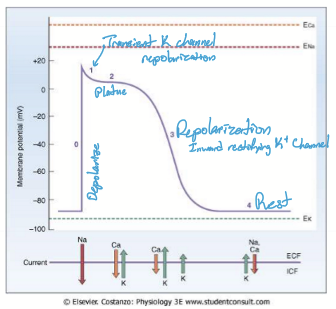
What are the phases of an AP of a cardiac myocyte?
Phase 0: Depolarization; Na channels open
Phase 1: Slight repolarization: Na channels close, transient K channels open
Phase 2: Plateau: transient K channels open and L-type Ca channels open (DHPR)
Phase 3: Repolarization: L-type Ca channels close (DHPR) and K channels open
Phase 4: Reset
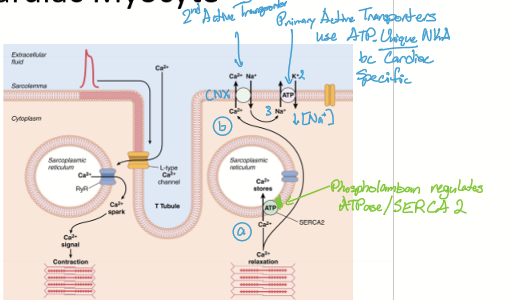
What are the steps of a cardiac myocyte contraction?
Depolarization by pacemaker or adjacent myocytes
AP begins: voltage-gated DHPR channels open, Ca influx
Ca from ECF binds to RyR and opens it
Ca released from SR (CICR = Ca induced Ca release) = spark [most important source]
Ca binds troponin, myosin heads crossbridge and contraction occurs
Repolarization of AP: all voltage-gated channels reset
![<ol><li><p>Depolarization by pacemaker or adjacent myocytes</p></li><li><p>AP begins: voltage-gated DHPR channels open, Ca influx </p></li><li><p>Ca from ECF binds to RyR and opens it</p></li><li><p>Ca released from SR (CICR = Ca induced Ca release) = spark [most important source]</p></li><li><p>Ca binds troponin, myosin heads crossbridge and contraction occurs</p></li><li><p>Repolarization of AP: all voltage-gated channels reset </p></li></ol><p></p>](https://knowt-user-attachments.s3.amazonaws.com/1f08878d-ad65-4db9-87b4-122fa39c37c1.png)
How is Ca removed from the ICF?
SERCA pumps Ca into SR for the spark in the next contraction
Pump Ca into ECF via NKA (Sodium Potassium ATPase) or CNE (calcium sodium exchanger)
Why is the refractory period important in cardiac muscle?
It prevents tetany (sustained contraction) by ensuring that each contraction is followed by full relaxation before another AP occurs.
How are AP and twitch linked in cardiac myocytes?
The calcium used in the action potential is also involved in the muscle twitch for contraction.
Why is there no tetany in cardiac muscle?
The refractory period lasts almost as long as the contraction, preventing repeated stimulation before relaxation occurs. AKA, no latent period for build up of AP to increase contraction force.
What mechanisms regulate contraction strength?
Inotropy: regulation of calcium in ICF
Preload: length-tension relationship
What affects the cardiac myocytes contraction strength?
The strength of contraction is based on Ca2+ in the cell
What do positive inotropic agents do?
The increase Calcium in the cell to make a stronger contraction.
What do negative inotropic agents do?
Decrease Ca in the cell to make a weaker contraction
What are some positive ionotropy?
Beta 1 agonists=- decease heart size and heart rate
increase thyroid = increase number of Beta1 receptors
What are some negative ionotropy?
Beta1 blocker
Decrease thyroid = decrease number of beta1 receptors
What is the difference between chronotropy and inotropy?
Chronotropy is heart rate, inotropy is contraction strength
What does high SNS do to inotropy/contractility?
High SNS stimulates inotropy by enhancing intracellular Ca²⁺ levels.
Epinephrine (Epi) and Norepinephrine (Norepi) bind to β₁-adrenergic receptors.
This leads to phosphorylation of:
DHPR (L-type Ca²⁺ channels): Increases Ca²⁺ influx.
RyR2 (Ryanodine Receptors): Enhances Ca²⁺ release from the SR.
SERCA (SR Ca²⁺-ATPase): Increases Ca²⁺ reuptake, leading to stronger and faster contractions.
What does low SNS do to inotropy/contractility?
Low SNS inhibits inotropy by decreasing the amount of calcium in the cell.
What are some drugs that inhibits inotorpy?
Beta1 antagonists: Metoprolol or lopressor
Calcium-channel blockers/cardioinhibitory
Benzothiazepine: Diltiazem
Phenylalkylamine: Verapamil (cardiac-specific)
What are cardiac glycosides?
A class of drugs that increase cardiac contracility (positive inotropy) and decreases the heart rate (negative chronotropy) to cause an overall increase in CO. It is cardiostimulatory
What is preload?
The volume of blood loaded into the heart before ventricular contraction
What are the other names for preload?
Venous return
End-diastolic volume
Frank-Starling Law of the Heart
How does the volume of blood filling the heart affect contraction strength?
Sarcomeres are stretched as the heart fills with blood. The changes in the length of sarcomeres will determine the strength of heart contraction.
How can the sarcomere determine the amount of stretching/changes in length it experiences?
The amount of myosin-actin overlap
What is the relationship between length and tension?
Linear. Lower preload/length = lower tension. Higher preload = higher tension
What things can affect preload?
Venoconstriction by SNS
Muscle pump: veins between skeletal muscles pump blood toward heart
Respiratory pump: during inspiration, throacic pressure drops, drawing blood into the heart
What is Systole?
Isovolumetric contraction and ejection of blood
What is diastole?
Isovolumetric relaxation, with active and passive ventricular filling
Starting at last diastole, what are the phases of the cardiac cycle?
Late diastole: Passive filling as atrioventricular valves are open semilunar valves closed
Atrial systole (diastole): Atria depolarize and contract to actively fill the ventricles through the atrioventricular valves
Isovolumetric contraction (Systole): Ventricles depolarize and start to contract. All valves are closed and pressure is building up [First heart beat sound]
Ejection (Systole): BLood ejected into aorta and pulmonary artery as semilunar valves open and atrioventricular valves remain closed
Isovolumetric relaxation (diastole): ventricular repolarization as all valves close. No bloove movement and pressure drops [second heart beat sound]
How is cardiac output measured?
In liters per minute. Typically rate is 5L/minute
How to cardiac output change?
Change stroke volume and/or heart rate.
What determines Cardiac output?
Chronotropy/Heart Rate: activity of pacemaker cells and chronotropic agents
Stroke Volume: Due to inotropy/contractility, preload, and afterload
What is afterload?
resistance to ejection caused by:
hypertension
Valve disease