Peds: Chap.10 Assessment and Treatment of Feeding
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
16 Terms
Feeding, Eating, and Swallowing: Overview, Mealtime, and Cultural Influences
Feeding: Bringing food to mouth; includes self-feeding and caregiver feeding.
Eating: Keeping and manipulating food in the mouth; chewing and swallowing.
Swallowing: Complex process of moving food/liquid from mouth to stomach.
Mealtime – Significance and Considerations
Developmental Importance: Promotes bonding, communication, social skills, and routine.
Structure: Predictable routine encourages regulation and learning.
Environment: Calm, distraction-free settings help children focus on feeding.
Family Dynamics: Mealtime reflects parenting styles, expectations, and interaction.
Cultural Influences on Feeding
Dietary choices: Some foods/textures may be introduced earlier/later based on cultural norms.
Feeding practices: Hand-feeding vs. self-feeding, bottle vs. breast, use of utensils.
Mealtime routines: Where, when, and with whom meals are eaten vary across cultures.
Perceptions of picky eating: Cultural norms influence whether behaviors are seen as problematic.
Caregiver roles: Different expectations for child independence in feeding.
Feeding Disorders: Incidence and Influences
Gastroesophageal Reflux (GER)
Stomach contents flow back into the esophagus
Symptoms: pain, vomiting, food refusal, arching during feeds
Can affect growth and feeding success
Food Allergies
Immune response to specific foods (e.g., dairy, nuts, eggs)
Symptoms: rash, swelling, vomiting, diarrhea, anaphylaxis
May lead to limited diet and food aversion
Oral Motor Functions, Sensory and Behavioral
Oral Motor Function
Involves coordination of lips, tongue, jaw, cheeks
Impairments can affect sucking, chewing, swallowing
May result in drooling, food loss, gagging, or fatigue during meals
Sensory Issues
Over- or under-responsiveness to food textures, temperatures, smells, or tastes
Can cause food refusal, limited food repertoire, or distress at mealtimes
Often addressed with sensory integration and graded exposure
Behavioral Issues
May include food refusal, tantrums, or rigid mealtime routines
Often develop in response to medical or sensory challenges
Managed with consistent routines, caregiver education, and behavioral strategies
Role of the
Occupational Therapist
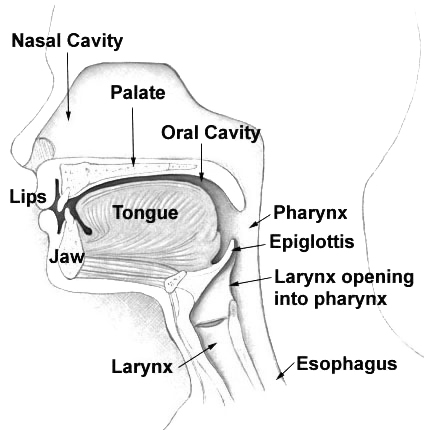
Anatomy & Physiology:
Includes lips, tongue, jaw, cheeks, palate, pharynx, larynx, esophagus – all must coordinate for safe swallowing and efficient eating.Growth & Developmental Milestones:
Suck-swallow-breathe: birth
Spoon feeding: ~4–6 months
Chewing/mashing: ~8–12 months
Self-feeding: ~12–18 months
Nutrition:
Essential for growth, brain development, and immune function; includes adequate intake of protein, fats, vitamins, minerals, and fluids.Medical Conditions:
Examples: prematurity, cerebral palsy, GERD, cleft palate. Can cause oral motor delays, fatigue, food refusal, or need for alternative feeding methods.Social & Emotional Factors:
Family stress, mealtime conflict, trauma, or caregiver interaction styles can negatively affect feeding behavior and appetite.
Development of Oral Structures
Oral Cavity:
Small and filled by the tongue in infancy; grows to allow more refined movements for chewing and speech.Pharynx:
Short and compact in infants; lengthens with age to separate respiratory and digestive tracts more clearly.Larynx:
Positioned high in the neck at birth (closer to epiglottis); lowers as the child grows, allowing for speech but increasing aspiration risk.Trachea:
Airway passage that is narrow in infants; grows in diameter and length with age, improving respiratory safety during feeding.Esophagus:
Immature peristalsis in infancy; matures to support more efficient swallowing and reduced reflux over time.
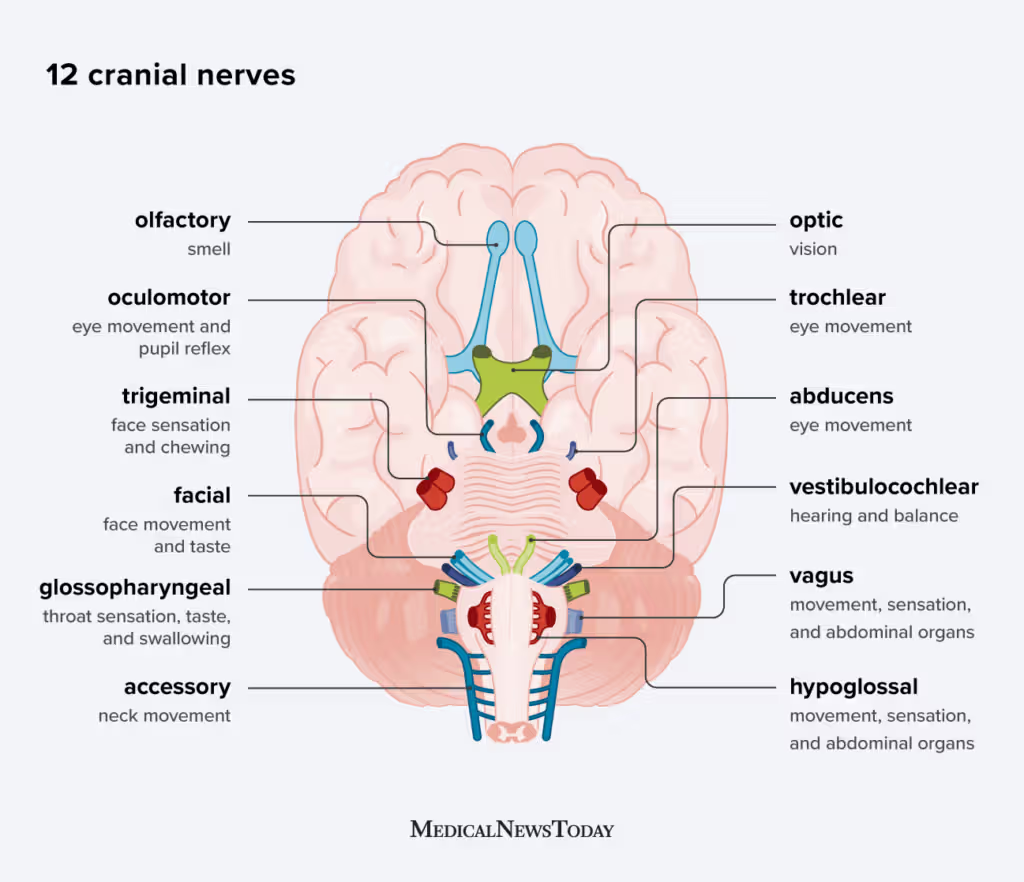
Cranial Nerves
CN V – Trigeminal
Function: Sensation to face & mouth; motor to muscles of mastication
Role in Feeding: Chewing, jaw movement, oral sensation (e.g., detecting food in mouth)
CN VII – Facial
Function: Facial expression; taste to anterior 2/3 of tongue
Role in Feeding: Lip closure, cheek movement (buccinator), salivation, taste
CN XII – Hypoglossal
Function: Motor control of the tongue
Role in Feeding: Tongue movement for chewing, bolus formation, and propulsion during swallowing
Phases of Swallowing
Oral Preparatory Phase
Voluntary
Food is chewed and mixed with saliva to form a bolus
Lips close, cheeks control food, tongue moves food for chewing
Oral Phase
Voluntary
Tongue pushes the bolus to the back of the mouth toward the pharynx
Pharyngeal Phase
Involuntary
Soft palate rises, airway closes, and bolus moves through pharynx
Risk of aspiration if coordination is poor
Esophageal Phase
Involuntary
Bolus moves down the esophagus to the stomach via peristalsis
Comprehensive Feeding & Swallowing Evaluation
Initial Interview & Chart Review
Review medical history, diagnoses, growth patterns
Interview caregivers about feeding concerns, routines, and goals
Structured Observation
Observe typical mealtime at home or clinic
Note posture, oral motor skills, sensory responses, behavior, caregiver interaction
Assessment Tools
Examples:
Schedule for Oral Motor Assessment (SOMA)
Dysphagia Disorder Survey
Behavioral Pediatric Feeding Assessment Scale (BPFAS)
Additional Diagnostic Evaluations
Videofluoroscopic Swallow Study (VFSS)
Fiberoptic Endoscopic Evaluation of Swallowing (FEES)
Allergy testing, pH probe, upper GI series (if needed)
Key Considerations for Feeding Difficulties
Feeding problems often have multiple underlying factors (medical, sensory, behavioral).
If left unaddressed, they can lead to new complications (malnutrition, oral aversion).
Problems typically occur frequently and across settings (home, school, clinic).
Always assess for medical and nutritional issues that may be contributing.
Feeding challenges often demand increased caregiver time and energy.
Interventions should aim to support and maintain family routines, not disrupt them.
Feeding Intervention Strategies
Environmental Adaptations
Reduce distractions (noise, screens)
Establish consistent mealtime routines
Use calming sensory input (dim lighting, soft music)
Positioning Adaptations
Follow 90-90-90 rule (hips, knees, ankles at 90°)
Ensure head and trunk alignment
Use supportive seating (e.g., booster, Rifton, footrests)
Adaptive Equipment
Built-up or angled utensils
Nosey cups or cut-out cups
Non-slip mats (e.g., Dycem), plate guards, divided plates
Feeding Strategies and Dysphagia Management
Self-Feeding
Encourages independence and motor skill development
Use hand-over-hand assistance, adaptive utensils, and consistent routines
Start with easy-to-grasp foods and finger foods
Modifications to Food Consistencies
Pureed: smooth texture for limited oral motor skills
Mechanical soft: mashed, ground, or finely chopped
Regular: typical textures for age/development
Modifications to Liquids
Thin: like water or juice
Nectar-thick: slightly thicker (e.g., tomato juice)
Honey-thick: pours slowly (e.g., milkshake)
Thickening may reduce aspiration risk in dysphagia
Dysphagia
Swallowing difficulty that may lead to aspiration, choking, or poor nutrition
Requires coordinated care (OT, SLP, medical team)
Interventions: positioning, pacing, texture modification, swallow techniques
Common Feeding Challenges
Sensory Processing Disorders
Over- or under-reactivity to food textures, smells, tastes
May gag, refuse, or avoid certain foods
Intervention: sensory desensitization, graded exposure, play-based feeding
Behavioral Feeding Issues
Learned behaviors like refusal, tantrums, or mealtime control struggles
May result from past negative feeding experiences or inconsistent routines
Intervention: structured mealtimes, positive reinforcement, caregiver training
Food Refusal or Selectivity
Child eats a limited variety or avoids entire food groups
Often linked to sensory, medical, or behavioral issues
Intervention: food chaining, modeling, repeated exposure
Delayed Transition to Textured Foods
May resist moving from purees to solids
Causes: oral motor delays, sensory aversion, anxiety
Intervention: introduce small texture changes gradually, oral motor support
Delayed Transition from Bottle to Cup
Can be due to oral motor weakness, sensory preferences, or habit
Intervention: offer cups early (around 6 months), use transition cups, model cup use
Special Considerations in Feeding Interventions
Neuromuscular Interventions
Focus on improving strength, coordination, and tone
Techniques: oral motor exercises, jaw stabilization, cheek support, pacing
Often used in conditions like cerebral palsy, muscular dystrophy
Transition from Nonoral to Oral Feedings
Gradual process for children with feeding tubes
Goals: build oral tolerance, positive associations with eating
Use play, taste exposure, and oral motor prep to support transition
Cleft Lip and Palate
Structural gaps in the lip/palate affect suction and swallow
Use special bottles (e.g., Haberman), upright positioning
Surgical repair typically required; long-term feeding and speech support may be needed
Other Structural Anomalies
Examples: micrognathia, glossoptosis, laryngeal cleft
May require surgical correction, adaptive feeding strategies, or referral to specialists
Feeding plan must be individualized and medically coordinated
IDDSI – 7 Levels of Food Consistencies
7 | Regular | Normal food with no modifications |
6 | Soft & Bite-Sized | Soft, tender food cut into ≤15mm pieces (adult); requires some chewing |
5 | Minced & Moist | Moist, soft foods, finely chopped (≤4mm); minimal chewing needed |
4 | Pureed | Smooth, lump-free; holds shape but requires no chewing |
3 | Liquidised / Moderately Thick | Can be drunk from a cup; no chewing; pours quickly but not as thin as water |
2 | Mildly Thick | Thicker than water; flows off spoon easily; suitable for slow swallowers |
1 | Slightly Thick | Similar to nectar consistency; barely thicker than water |
0 | Thin | Regular liquids like water, juice |