Pathophysiology Midterm: Chapter 22 (Assessment of the Respiratory System)
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
23 Terms
Nasal Cannula
- used at flow rates of 1 to 6 L/min.
- Oxygen concentrations of 24% (at 1 L/min) to 44% (at 6 L/min) can be achieved
- often used for chronic lung disease and for any patient needing long-term oxygen therapy.

Simple Face Mask
- deliver oxygen concentrations of 40% to 60% for short-term oxygen therapy or in an emergency
- A minimum flow rate of 5 L/min is needed to prevent rebreathing of exhaled air.
- Care for the skin under the mask and strap to prevent breakdown.

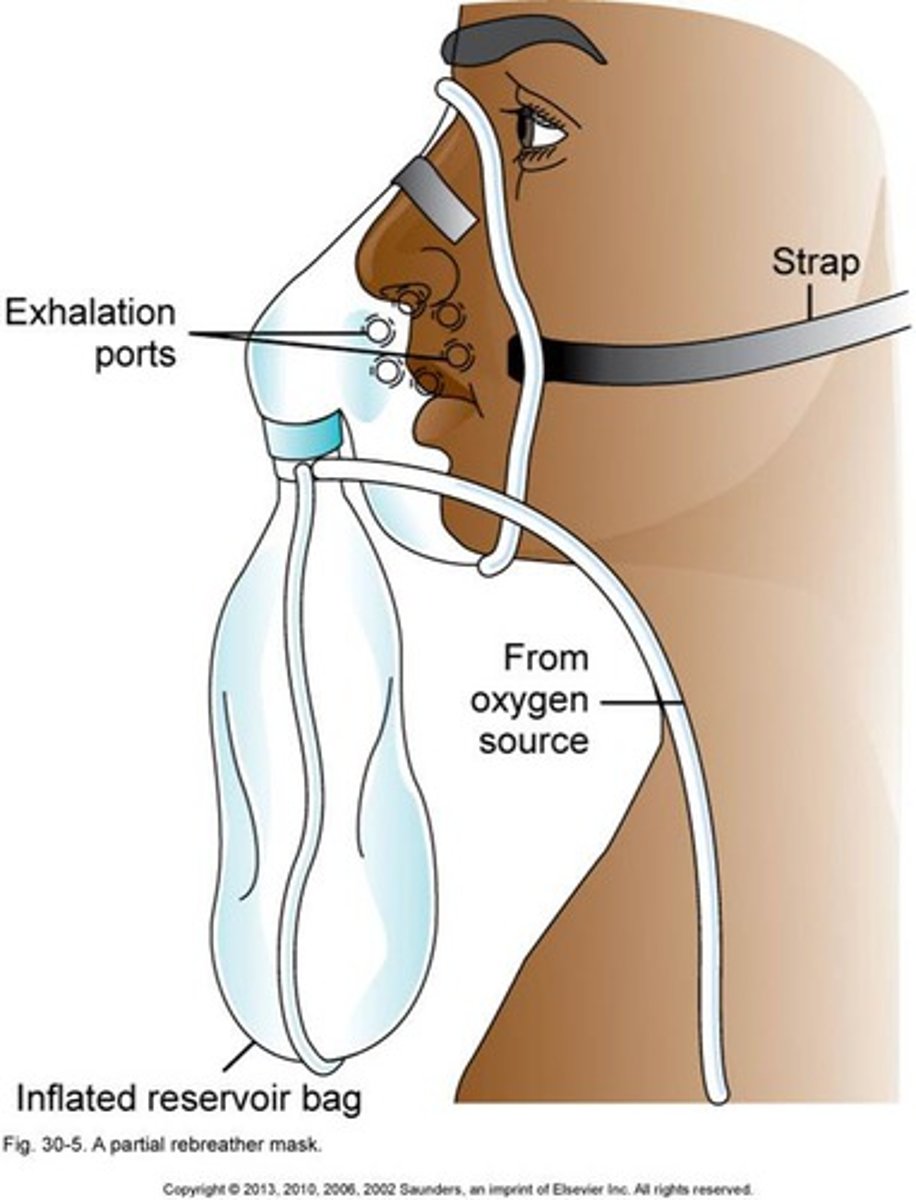
Partial Rebreather Mask
- Provide oxygen concentrations of 60% to 75%
- flow rates of 6 to 11 L/min.
- With each breath, the patient rebreathes one-third of the exhaled tidal volume, which is still high in oxygen and increases the fraction of inspired oxygen (FiO2)
Nonrebreather Mask
- provide the highest oxygen level of the low-flow systems and can deliver an FiO2 greater than 90%, depending on the patient's breathing pattern.
- This mask is often used with patients whose respiratory status is unstable and who may require intubation.
- The flow rate is kept high (10 to 15 L/min)
Fio2 Delivered: (Nursing Considerations)
24%-40% FiO2 at 1-6 L/min
≈ 24% at 1 L/min
≈ 28% at 2 L/min
≈ 32% at 3 L/min
≈ 36% at 4 L/min
≈ 40% at 5 L/min
≈ 44% at 6 L/min
- Ensure that prongs are in the nares properly to prevent hypoxemia and skin breakdown with loss of tissue integrity.
- Apply water-soluble jelly to nares PRN to reduce mucosal irritation from the drying effect of oxygen therapy.
- Assess the patency of the nostrils to detect conditions that prevent effective oxygen delivery such as congestion or a deviated septum.
- Assess the patient for changes in respiratory rate and depth because these changes reflect how well oxygen is being delivered.
Fio2 Delivered: (Nursing Considerations)
40%-60% FiO2 at 5-8 L/min; flow rate must be set at least at 5 L/min to flush mask of carbon dioxide
≈ 40% at 5 L/min
≈ 45%-50% at 6 L/min
≈ 55%-60% at 8 L/min
- Be sure that mask fits securely over nose and mouth because a poorly fitting mask reduces the FiO2 delivered.
- Assess skin and provide skin care to the area covered by the mask because pressure and moisture under it can cause loss of tissue integrity.
- Monitor the patient closely for risk for aspiration because the mask limits the patient's ability to clear the mouth, especially if vomiting occurs.
- Provide emotional support to the patient who feels claustrophobic to decrease anxiety and increase acceptance of the device.
- Suggest to the respiratory health care provider to switch the patient from a mask to the nasal cannula during eating to promote gas exchange while eating
Fio2 Delivered: (Nursing Considerations)
60%-75% at 6-11 L/min, a liter flow rate high enough to maintain the reservoir bag two-thirds full during inspiration and expiration
- Make sure that the reservoir does not twist or kink, which results in a deflated bag that can decrease the amount of oxygen delivered and increases rebreathing of exhaled air.
- Adjust the flow rate to keep the reservoir bag inflated to meet the patient's oxygen needs.
Fio2 Delivered: (Nursing Considerations)
80%-95% FiO2 at a liter flow rate high enough to maintain the reservoir bag two-thirds full
- Interventions as for partial rebreather mask; this patient requires close monitoring to ensure proper functioning of the device.
- Make sure that valves and rubber flaps are patent, functional, and not stuck. Valves must open during exhalation and close during inhalation to prevent dramatic decrease in FiO2, which could lead to suffocation.
- Closely assess the patient on increased FiO2 via nonrebreather mask to determine whether the patient's oxygen needs are adequately met or if intubation is needed.
Assessment of the Patient Receiving Oxygen Therapy: General
- Airway patency
- Respiratory rate and effort
- Lung sounds
- Pulse ox
- Level of Consciousness
- Skin breakdown
Assessment of the Patient Receiving Oxygen Therapy: Nose and Sinuses
- Inspect the patient's external nose for deformities and the nares for symmetry of size and shape. To observe the interior nose, ask the patient to tilt the head back for a penlight examination.
- Inspect for color, swelling, drainage, bleeding, and polyps. Nasal mucous membranes normally appear redder than the oral mucosa but are pale, engorged
Assessment of the Patient Receiving Oxygen Therapy: Pharynx, Trachea, and Larynx
- Assessment of the pharynx begins with inspection of the mouth.
- Inspect the neck for symmetry, alignment, masses, swelling, bruises, and the use of accessory neck muscles in breathing.
- Gently palpate the trachea for position, mobility, tenderness, and masses.
Assessment of the Patient Receiving Oxygen Therapy: Lungs and Thorax-
- Inspect the front and back of the thorax with the patient sitting up.
- Observe the chest and compare one side with the other.
- Examine the shape of the patient's chest, and compare the anteroposterior (AP, or front-to-back) diameter with the lateral (side-to-side) diameter.
Oxygen Toxicity
- related to the concentration of oxygen delivered, duration of oxygen therapy, and degree of lung disease present.
- A continuous oxygen level greater than 50% for more than 24 to 48 hours may injure the lung and reduce tissue integrity.
Symptoms of Oxygen Toxicity
- Dyspnea, nonproductive cough, chest pain beneath the sternum, GI upset, and crackles on auscultation. - As exposure to high levels of oxygen continues, problems become more severe, with decreased vital capacity, decreased compliance, and hypoxemia.
- Continued exposure to high oxygen levels leads to atelectasis, pulmonary edema, hemorrhage, and hyaline membrane formation.
What should be monitored with oxygen toxicity?
- Monitor arterial blood gases (ABGs) during oxygen therapy, and notify the respiratory health care provider when PaO2 levels become greater than 90 mm Hg.
- Also monitor the oxygen level and length of therapy to identify patients at risk.
I PREPARE Model: I (Investigate)
Ask the patient specific questions to assess for all possible current and past particulate matter exposures to inhalation irritants, including issues regarding current and past geographic living area, home conditions, occupation, and hobbies.
I PREPARE Model: P (Present Work
Ask about exposure to industrial dusts, fumes, or chemicals that may cause breathing disorders. Occupations with higher risk for exposures include bakers, coal miners, stone masons, cotton handlers, woodworkers, welders, potters, plastic and rubber manufacturers, printers, farm workers, those working in grain elevators or flour mills, and steel foundry workers. Ask whether breathing difficulties are less severe when away from the work environment.
I PREPARE Model: R (Residence)
Ask about the type of heat used at home (e.g., gas heater, wood-burning stove, fireplace, kerosene heater). Determine whether other people in the same residence have similar breathing problems. Ask whether any construction, especially in an older home, has recently been performed. Ask about the presence of mold or chronic dampness in the residence.
I PREPARE Model: E (Environment)
Determine the geographic location of the residence and whether it is in an area with higher levels of air pollution. Ask whether heavy industries, factories, farms, airports, or landfills are near
I PREPARE Model: P (Past Work)
Because chronic particulate matter exposure may take years to affect respiratory function, ask the patient about all previous types of work and work environments.
I PREPARE Model: A (Activities)
Ask about hobbies in which the patient or other members of the household may engage, such as painting, ceramics, model airplanes, refinishing furniture, or woodworking, for possible exposure to harmful chemical fumes.
I PREPARE Model: R (Resources and Referrals)
Provide patients with informative pamphlets and websites that can help them understand the risks for particulate matter exposure and what types of protection can be used.
I PREPARE Model: E (Educate)
Determine the patient's literacy level and how the patient best acquires new information. Provide information and encourage the use of credible resources. A few examples include the National Center for Environmental Health (NCEH); Centers for Disease Control and Prevention (CDC) resource General Information on Air Pollution and Human Health; Environmental Protection Agency (EPA); Occupational Safety and Health Administration (OSHA); and National Institute for Occupational Safety and Health (NIOSH).