PTE 764: quest 2
1/151
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
152 Terms
what are the public health/exercise recommendations for a patient with cardiovascular conditions?
30 mins of moderate intensity 3-5 days/week
resistance training 2 days/week
what is coronary artery disease (CAD)?
a condition where the arteries that supply blood to the heart become narrowed or blocked due to plaque
what is chronotropic incompetence?
a condition where the heart is unable to increase its rate adequately in response to physical activity or other stressors
patients with CAD fail to achieve predicted maximum heart rate without ___-______.
beta-blockers
the heart rate decreases back to normal following exercise due to which system?
parasympathetic nervous system
an abnormality in heart rate recovery is the delay in the decrease in heart rate of less than __ at 1 minute and less than __ at 2 minutes.
12 bpm; 22 bpm
T or F: in the case of chronotropic incompetence, a patient is unable to increase the heart rate the same rate as healthy individuals.
T
in a patient suffering from chronotropic incompetence, there is a failure to meet his age adjusted HRmax. what %AAHRmax should a therapist strive for this patient during exercise?
~ 85% HRmax
at what range does systolic blood pressure increase per MET?
8-12 mmHg per MET
in patients with CAD, when does their blood pressure usually plateau?
at peak exercise
describe the relationship between blood pressure and patients with CAD.
patients may respond normally or may experience an increase or decrease in blood pressure abnormally at sub-max levels
what is exertional hypotension?
a condition where blood pressure drops significantly during or after physical activity (below resting BP levels)
why does exertional hypotension occur?
a failure to increase systolic blood pressure with an increase in heart rate
a decrease of ≥ ___ in systolic blood pressure during stress is a reason to stop exercising asap.
10 mmHg!
what two disorders can patients with exertional hypotension possibly experience?
left ventricular dysfunction
myocardial ischemia
what is the difference between myocardial ischemia and myocardial infarction?
ischemia: the heart muscle does not receive enough blood flow, leading to a temporary and reversible lack of oxygen and nutrients
infarction: blood flow to the heart muscle is reduced or blocked, leading to damage (via scar tissue) or death of heart tissue
what is the biggest complaint in patients with cardiovascular conditions during exercise?
chest pain
silent heart attacks may be seen mostly in patients with _____.
diabetes
what are some possible causes of exertional hypotension?
congenital: hypothyroidism, idiopathic
metabolic: hypothyroidism, starvation, liquid protein diets
cardiac: brady-arrhythmias, mitral valve prolapse
drug-induced
others: connective tissue disorders, hypothermia, intracranial disease
diastolic blood pressure does not change much during exercise, but a slight decrease may be noted in some individuals. why?
measuring error and/or dilation of skin vessels
an increase in diastolic blood pressure of ___ is associated with CAD.
10 mmHg
an exaggerated response of both SBP and DBP in exercise is associated with what disease?
future of hypertension (aka exercise-induced hypertension)
normally we see an 8-10 times increase in VO2 with peak exercise, but patients with CAD see a ______.
reduction (blunted)
why might a patient with CAD experience a diminished VO2 and a decrease in cardiac output?
chronotropic incompetence
left ventricular impairment
decrease ejection fraction and stroke volume
at what percent can exercise improve VO2 in de-conditioned individuals?
~15-30%
what may occur physiologically during exercise in a patient with CAD?
increase myocardial O2 uptake with exercise
shorten diastole (HTN) (filling time)
shortening coronary perfusion time (increases LVEDP)
T or F: healthy patients can experience a transient O2 deficiency (ischemia).
T
why do ischemic tissues not conduct impulses readily?
due to the pathology of electrical instability (abnormal S-T segments) and dysrhythmias (re-entry dysrhythmias)
what are the three steps of the ischemic cascade?
an imbalance of myocardial O2 supply and demand (due to abnormalities in both diastolic then systolic function)
ECG changes occur
patient experiences angina
what is the product of the ischemic cascade?
angina
T or F: ischemic effects on both diastolic and systolic dysfunction never occur before angina or ECG changes are detected.
F; they can occur before
what medication acts as a vasodilator that may help blood flow in times of emergencies?
nitroglycerin
what is the rate pressure product?
a non-invasive measure of the heart's oxygen demand and workload, calculated by multiplying the heart rate by the systolic blood pressure (RPP = HR × SBP)
what two modifications must occur so patients can lower their RPP in order to perform more activities?
take a beta-blocker to lower HR and contractility of the heart
exercise can lower HR and increase SV (which indirectly affects contractility)
myocardial O2 supply is affected by:
coronary stenosis
microvascular dysfunction (no nitric oxide)
abnormalities in autonomic function
abnormalities in coagulation and fibrinolytic system
what is coronary stenosis?
a narrowing of the coronary arteries due to plaque formation, collateral circulation, and/or endothelial dysfunction
T or F: coronary stenosis can vigorously effect patients with diabetes.
F; patients with diabetes have issues with lipids so the stenosis (plaque buildup) isn’t as vigorous
describe the cardiac (plaque) effects seen at a weekly caloric expenditure of <1000 kcal.
associated with progression of the plaque formation
describe the cardiac (plaque) effects seen at a weekly caloric expenditure of >1400 kcal.
demonstrated improvement in CV fitness
describe the cardiac (plaque) effects seen at a weekly caloric expenditure of >1500 kcal.
slowed the progression of plaque buildup
goal for exercise prescription to see worthwhile benefits
describe the cardiac (plaque) effects seen at a weekly caloric expenditure of >2200 kcal.
partial regression of plaque associated with CAD
______ may also play a huge role in plaque formation.
genetics
describe the endothelial function in a patient with CAD.
coronary arteries constrict in response to acetylcholine
decrease nitric oxide within vascular smooth muscle
the autonomic system mediates changes in:
heart rate, blood pressure, and vascular tone
T or F: in patients with MI or CHF, there are abnormalities in autonomic function that are more easily detected during exercise.
T
what are some abnormalities in autonomic function that are detected during exercise?
decrease parasympathetic and increased sympathetic activity
increase in cardiac morbidity and mortality
increased beat to beat heart rate variability in MI patients
elevated plasma and urinary levels of norepinephrine in CHF patients
relating to heart function, what’s the difference between increased epinephrine and norepinephrine levels?
epinephrine: increases heart rate
norepinephrine: leads to heart failure
what effects does an increase in plaque concentration have on other blood elements in patients with CAD?
increase fibrinogen
increase factor VII
increase platelet hyperactivity
decrease in fibrinolytic activity
describe the impact exercise has on the blood elements.
mod-high intensity exercise = lowers fibrinogen levels
endurance exercise = increases fibrinolytic system
long term exercise = decreases platelet aggregation
T or F: for benefits to occur, exercise should accompany a good diet
T
what caloric expenditure per week is recommended to reduce the causes of mortality from CAD?
1500-2000 kcal/week
what are some general exercise guidelines for patients with CAD?
should gradually increase duration of session until 30-40 mins
exercise large muscle groups with rhythmic activities
train both arms and legs
warm up and cool down periods should be included
what are the components of a dynamic resistance exercise program for a patient with CAD?
use both UE and LE
work towards mod intensity (50% of 1RM)
8-10 regional exercises 2-3 days/week with 10-15 reps
borg score of 11-14
it is important to include activities done at home for patients with cardiovascular conditions to arrive at the ____ kcal/week threshold.
1500
what are some general exercise guidelines for patients with MI?
watch for orhtostasis
ROM exercises
start at lower end of training intensity of 40-60% VO2 or 11-14 on the borg
20-40 mins sessions with 5-10 mins warm up and cool down
why is it important to always use a Borg rating instead of measuring HR to determine exercise intensity/exertion levels on a patient taking beta-blockers?
bc the beta-blockers lower the HR, making it unreliable to measure intensity/exertion
why must therapists avoid UE ROM exercises following a coronary artery bypass graft procedure (CABG)?
the sternum is cracked open during surgery making functional activities with the UE painful and difficult for patients to complete
what are some general exercise guidelines for patients with CHF?
moderate intensity!
allow for rest and self pacing with functional activity
progressively increase duration as tolerated to work up to 60-70% HRR or a borg level of 11-14
in patients with CHF, peak exercise is ______ by 40-50%.
reduced
what are the consequences seen in patients with CHF who exercise at their peak?
decrease peak cardiac output
chronotopic incompetence
decrease stroke volume due to passive insufficiency of cardiac muscle
impaired blood flow to active muscles
what blood elements may arise with impaired blood flow to active muscles?
increased plasma norepinephrine
decreased vascular nitric oxide
what is a motor unit?
a combination of motor neuron and the muscle fibers innervated by that motor neuron
comprised of motor neuron cell body, axon, neuromuscular junction, and muscle fiber
what are the characteristics of smaller motor neurons?
lower membrane resistance
lower threshold (easily excited)
attach to slower muscle fibers
what are the characteristics of larger motor neurons?
higher membrane resistance
higher threshold (harder to excite)
attached to faster muscle fibers
slow motor units are recruited more frequently compared to fast. why?
slow motor units are recruited mostly for activities of daily living such as posture, stereotypical locomotion, etc.
when are fast motor units recruited?
for activities that require higher force or power outputs (combination of speed and strength)
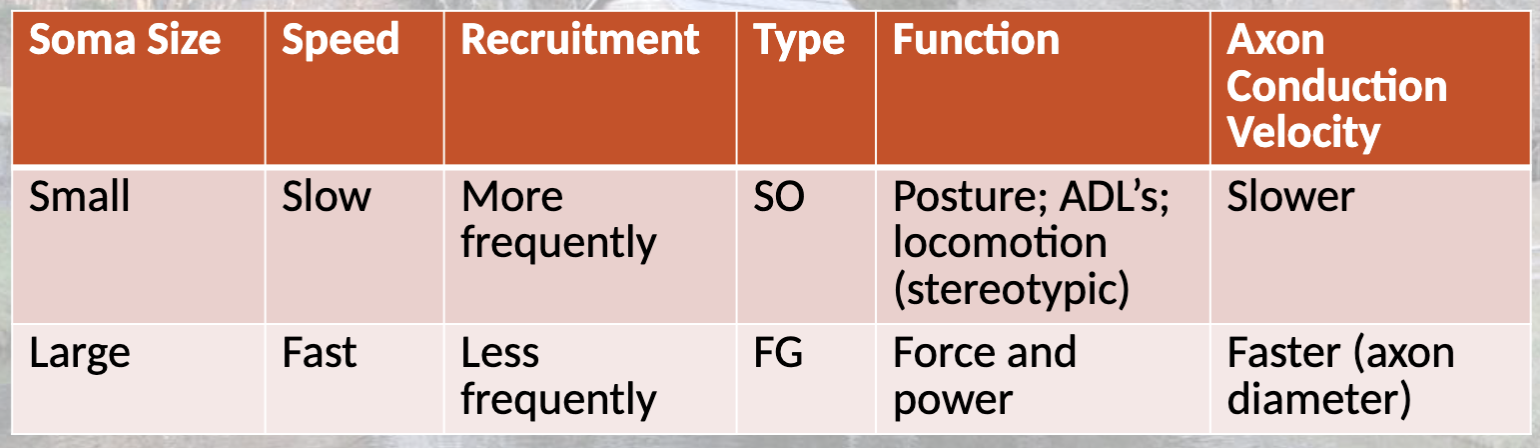
fast vs. slow characteristics
what is after hyper-polarization?
the transient period following an action potential (AP) where the neuron's membrane potential becomes more negative than its resting potential, and it is followed by the membrane potential returning to its normal resting level
occurs immediately following depolarization
the duration of after hyper-polarization determines the frequency (discharge rate) and is considered an ______ relationship.
inverse
longer duration → slower frequency
why do large motor neurons (fast fibers) have a shorter after hyper-polarization?
there’s a necessary increase in potential that leads to an increase in frequency of action potentials bc they require speed
motor units and tetany graph
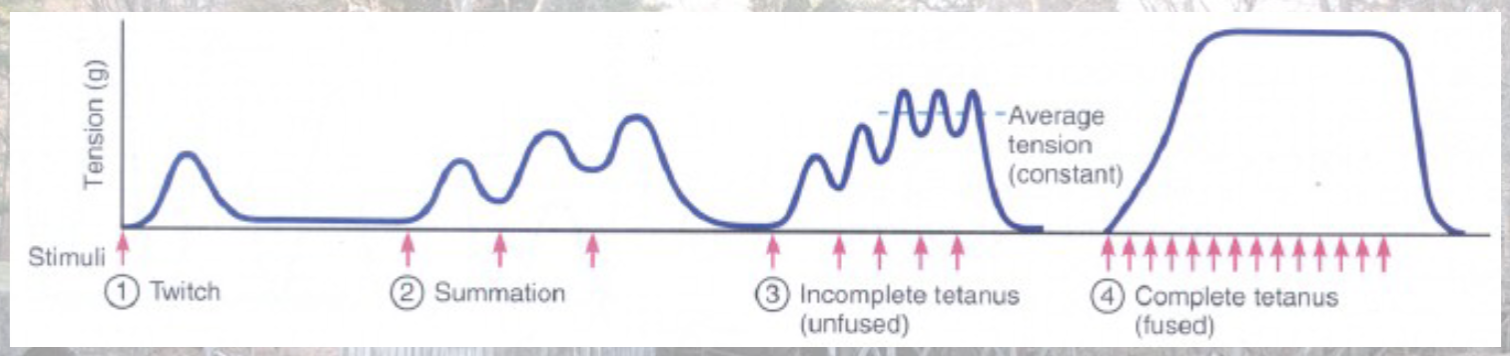
how do muscle units smooth the ripple effect found with un-fused tetanus?
motor units are activated asynchronously (turning some units off and some on at different times)
the number of axon branches corresponds to the _________ ____ of the motor units.
innervation ratio
describe the innervation ratio.
smaller innervation ratio for smaller, more “fine tune” musculature
larger innervation ratio for larger, more forceful musculature
what is neuromuscular junction fatigue?
the alteration of the sequence of events between excitation of the muscle and forced production
what occurs following repeated muscle activation?
depletes the stores of acetylcholine
increase lactate and adenosine which may interfere with neurotransmitter
the resultant fatigue may be protective in preventing overuse injury
high intensity exercise results in the release of hydrogen and lactate ions. hydrogen ions then compete with _______ for binding sites.
acetylcholine
how does the competition between acetylcholine and hydrogen ions effect the muscle?
the H+ ions block Ach → not enough Na+ and K+ channels can open → cannot produce an end plate potential → decreases frequency of action potentials → decrease muscle force output
what other molecule also interferes with the release of Ach after building up in the muscle following prolonged exercise?
adenosine
what are the three categories of motor units?
type I: slow oxidative
type IIA: fast oxidative or glycolytic
type IIB: fast glycolytic
T or F: there are hybrid motor units that contain mixtures of types I, IIA, and IIB.
T
motor units form a continuum to perform a wide variety of tasks. what characteristics are varied to accomplish this?
varied force production
speed of contraction
time of fatigue
metabolism
one motor unit is _____ in that all muscle fibers innervated by a single motor nerve have the same characteristics.
homogenous
muscle cell characteristics are determined more by the “pattern” of nerve stimulation. what are two ways this can change?
training: can be converted through training methods
surgery: in the case of nerve transplantation/ reattachments
what is muscle plasticity?
the ability of muscles to adapt and change their structure and function in response to external stimuli, such as exercise, injury, or disuse
what is muscle phenotype?
the observable characteristics and traits of muscle tissue, including its fiber types, fiber size, biochemical properties, and contractile characteristics
regulated by patterned neural stimulation
T or F: fiber characteristics of a motor unit can be altered through changes in the patterns of activity.
T
describe the pattern of motor unit recruitment.
slower motor units, used for tasks requiring low force production, are recruited first while fast motor units, used for high forces, are recruited last
aka Henneman principle
voluntary exercise can increase the levels of brain-derived neurotrophic factors (BDNF) which can…
stimulate neurogenesis
increase resistance to brain insult
improve learning and mental performance
promote brain plasticity
improve cognitive function
_____ may be an upstream regulator (controller) of BDNFs.
IGF-1 (insulin growth factor)
what is muscle power?
explosive aspect of strength, product of strength, and speed of movement
power = (force x distance) / time
neuromuscular adaptations chart
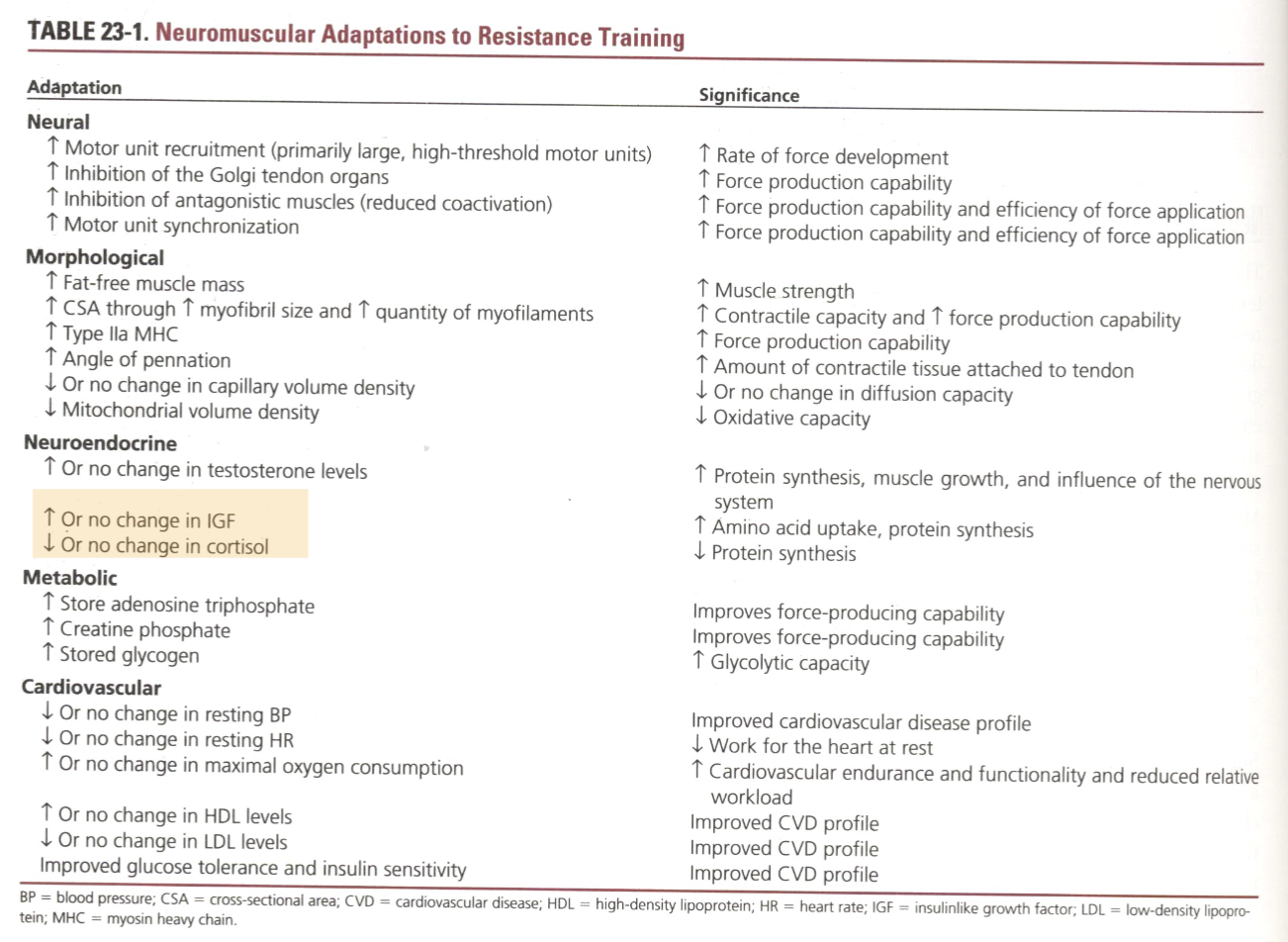
what are the two phases of neuromuscular adaptation?
neurological adaptation
muscular adaptations
what are the main neurological adaptations seen with resistance exercise?
changes in motor unit’s activation strategies and modifications of the function of the neuromuscular junction
what are the main muscular adaptations seen with resistance exercise?
hypertrophy, hyperplasia, fiber-type modification, and architectural changes
the initial increase in strength is due to _____ ______ and subsequently the increase strength in the later stages is attributed to ______ changes.
neural adaption; muscular
to achieve muscular adaptation after the initial neurological changes, what must happen?
increase intensity/ meet recruitment threshold
explain the improved coordination of activation patterns seen with resistance training.
with progressive resistance training, there is an increase in inhibition of GTO reflex allowing more forceful muscle contraction.
allows contraction of the agonist muscle without “fighting” the antagonist muscle
with the inhibition of the GTO reflex, how are connective tissues protected?
the GTOs should adapt and change with the resistance exercise (making the tissues strong too)
how does coactivation provide protection through joint stabilization during rapid agonist contractions?
it prevents the agonist muscles from being fully activated due to the simultaneous activation of two or more muscles that typically work in opposite directions