PERIO W12/13 Basic Concepts of Immunity and Inflammation; Host Immunoinflammatory Response to Biofilm
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
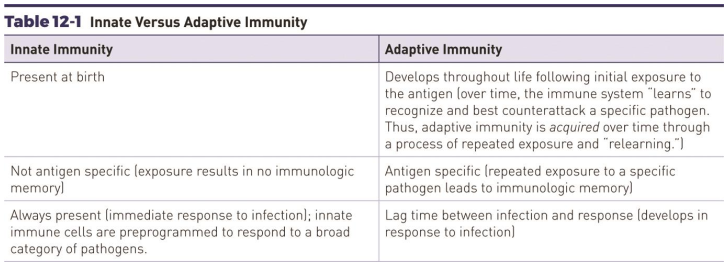
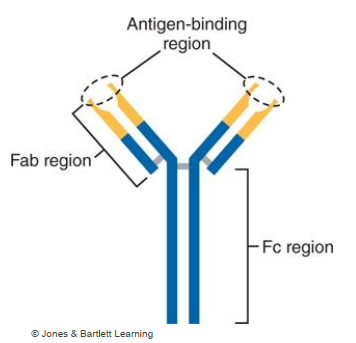
Compare and contrast Innate vs Adaptive Immunity
Innate Immunity
Onset: Immediate, non-specific.
Cells: Neutrophils, macrophages, dendritic cells, NK cells.
Mechanisms: Phagocytosis, inflammation, complement system, physical barriers.
Memory: None. Responds the same way every time.
Adaptive Immunity
Onset: Delayed (days), antigen-specific.
Cells: B lymphocytes (antibody production), T lymphocytes (helper, cytotoxic).
Mechanisms: Antigen presentation, clonal expansion, antibody-mediated and cell-mediated responses.
Memory: Yes. Faster, stronger response upon re-exposure.
Comparison
Work together: innate provides first line + presents antigens to activate adaptive.
Innate = broad defense; adaptive = targeted, long-lasting protection.
The body’s response to infection is called? What is it’s main purpose?
Host response → to defend the life of the host by identifying foreign substances in the body.
The immune system can become so intense that its response harms the host body while trying to protect the host. What is an example?
Rheumatic Heart disease
Invasion of Streptococcus pyogenes (strep throat bacteria)
Immune system acts against it by releasing cytokines
some structures in heart tissue are similar to s.pyogenes so the immune mediators attack the cardiac tissue.
What are the functions of Polymorphonuclear leukocytes (PML)?
Phagocytosis
Release lysosomes
Release powerful regulatory proteins (cytokines) that signal the immune system to send additional phagocytic cells to the site of infection
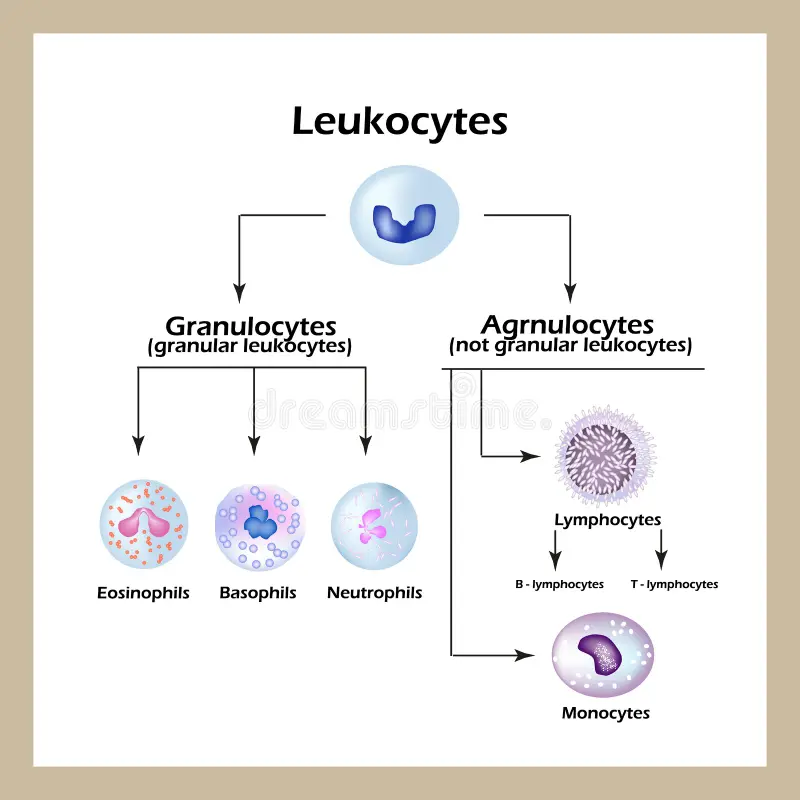
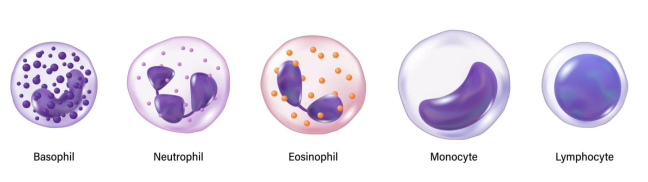
PML = Neutrophil, Eosinophil, Basophils
What are the functions of Macrophages?
Phagocytosis
Release of Lysosomes
Release cytokines to call additional phagocytic cells to site of infection
What are the functions of B-lymphocytes and T-lymphocytes?
B-cells → production of immjunoglobulins
T-cells → amplify the immune response
What are the functions of Immunoglobulins?
Neutralize bacteria or bacterial toxins
coat bacteria to facilitate phagocytosis
Activate complement system.
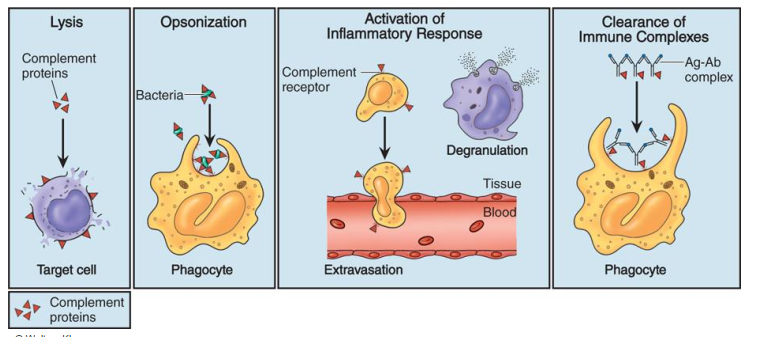
What are the functions of the Complement System?
Lysis of cell membranes of certain bacteria
Recruitment of additional phagocytic cells
Clearance of immune complexes from circulation
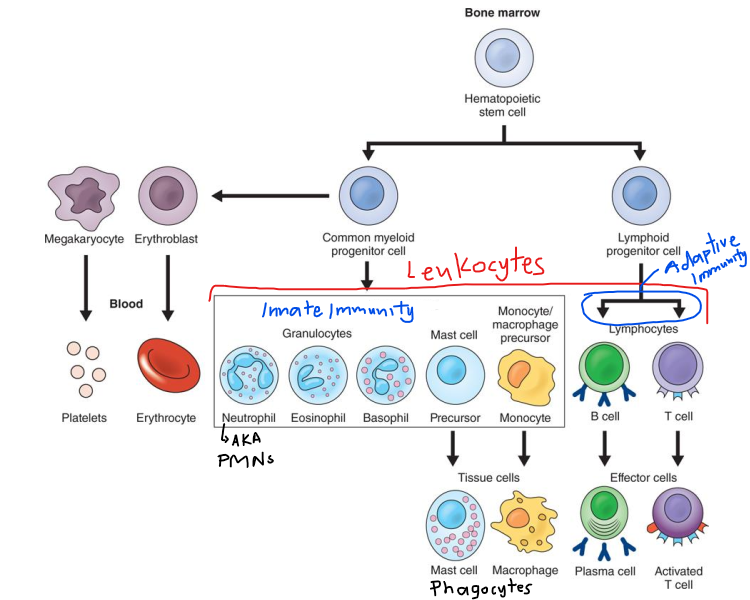
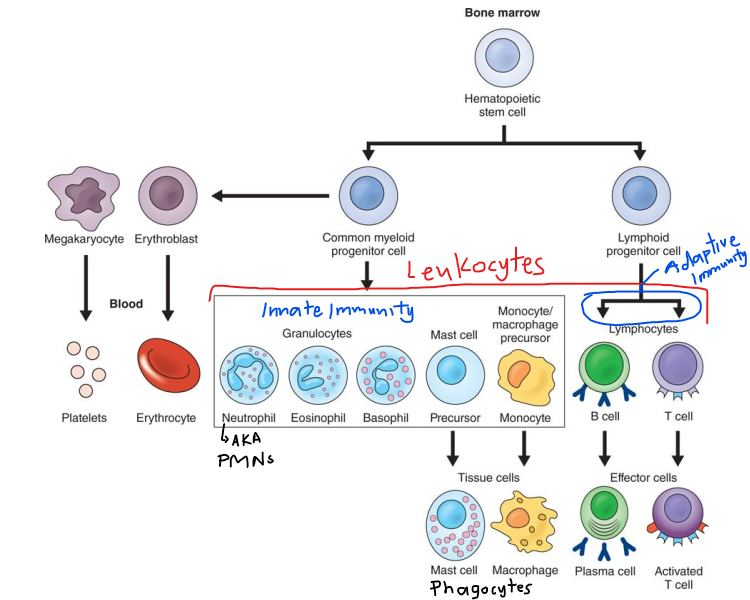
Leukocytes are categorized according to the presence or absence of…?
Cytoplastic granules
Agranulocytes → lymphocytes and monocytes/macrophages
Polymorphonuclear leukocytes (PML) → does not include mast cells (mononuclear)
Describe Fx of Neutrophils AKA polymorphonuclear neutrophils (PMNs)
First immune cells deployed → Rapid responders providing first line of defense
Most abundant
Can pass through capillary wall through chemotaxis
Short-lived cells → die when they are engorged with bacteria
contains bactericidal digestive enzymes
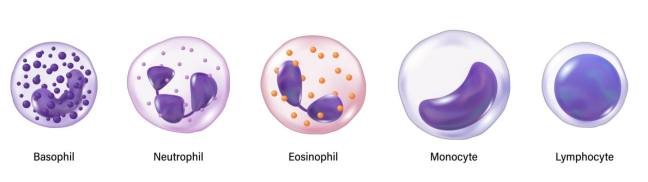
Describe Fx of Eosinophils
Primarily combat parasitic infections
Collaborates with mast cells and basophils to regular allergic response
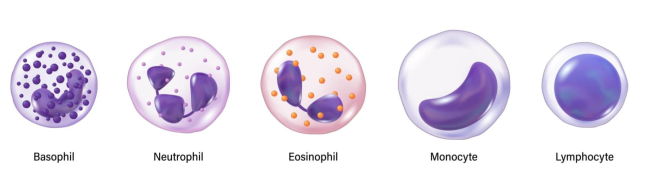
Describe Fx of Basophils
Primarily involved with allergic response
Coordinates activity against immune diseases
Describe Fx of Mast cells
Protects against pathogens and
Releases key inflammatory mediators that modulate allergic response
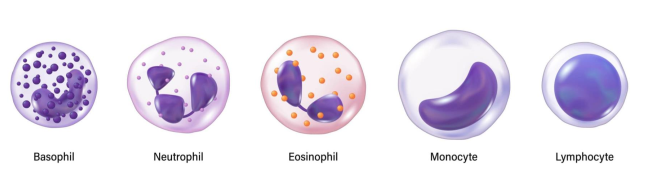
Which immune cell has a single irregular, kidney-shaped nucleus, lacks granules and performs phagocytosis?
Monocytes
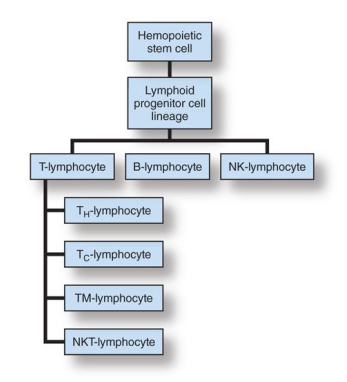
Describe Lymphocytes. What are the 3 types?
B-lymphocytes (B-cell)
T-lymphocytes (T-cell)
NK-Lymphocytes (Natural Killer cell)
What are the 2 subclasses of B-cells? What are their functions?
Plasma B-cell → produces antibodies
Memory B-cell → remembers previous exposures
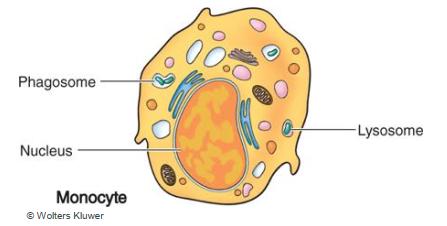
Describe Antibodies.
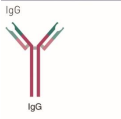
Y-shaped proteins composed of:
FAB = fragment antigen binding region
Fc = fragment constant → tail end that binds to immune cells and proteins of complement system.
**Antibodies are also called immunoglobulins.
What are the 5 major classes of Immunoglobulins?
Ig M, D, G, A, E,
(my dentist gave me an exam)
Which immunoglobulin is the only one that can pass through placental barrier? It is also the most abundant antibody.
IgG - potent activator of complement system; responds to invading pathogens.
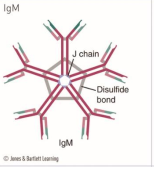
Which is the largest antibody that has a pentamer structure and the first to respond to initial exposures to antigens in blood and lymph?
IgM
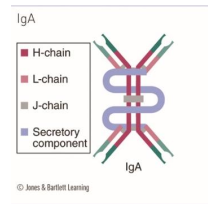
Which Immunoglobulin can pass through breast milk to the baby and is the principal defense at mucosal barriers
IgA
Which Immunoglobulin is involved with allergic response?
IgE

Which Immunoglobulin is the least abundant and least understood antibody?
IgD
How do antibodies eliminate invading agents?
Antibodies will coat the target, marking the foreign substance for immune cells to phagocytose.
Also activates the complement system.
What are the 4 subtypes of T-cells?
T-helper (CD4) → regulates b-cell maturation
T-cytotoxic (CD8) → directly attacks pathogens by releasing perforin (destroys plasma membrane of target cells)
T-memory (Tm-lymphocyte) → remembers past exposures
NKT (natural killer T) → first line defense against some bacterial and viral infections; attributes of innate and adaptive immunity
How are NK-Lymphocytes different from NKT-lymphocytes?
NK cells are part of the INNATE immunity
NK-Cell mature and develop in circulation
NK-cell DO NOT require pre-activation.
NKT-cells are bridge the innate and adaptive immune system
NKT-cells secrete cytokines to modulate immune response
NKT-cells require activation.
What is the complement system?
Complement system is composed of inactive, non-nucleated proteins that patrol the body for potential invaders.
They directly or indirectly neutralize them upon exposure to invaders
Work together with antibodies and phagocytes to neutralize pathogens
Fx:
Destruction of pathogens
Opsonization of pathogens
Recruitment of phagocytes
Immune clearance
The complement system creates a protein called ____ to destroy MO by forming pores in their cell membranes.
membrane attack complex (MAC)
What is opsionization?
opsonization = capture and destruction of bacteria by phagocytosis completed by the complement system.
**it is the most important action of the complement system.
Describe the function of immune clearance by the Complement system.
Immune clearance = removing immune complexes from circulation as an act of “house keeping”
Which immune cells are important for the control of Periodontal disease?
PMNs
Macrophages
B-cells
T-cells
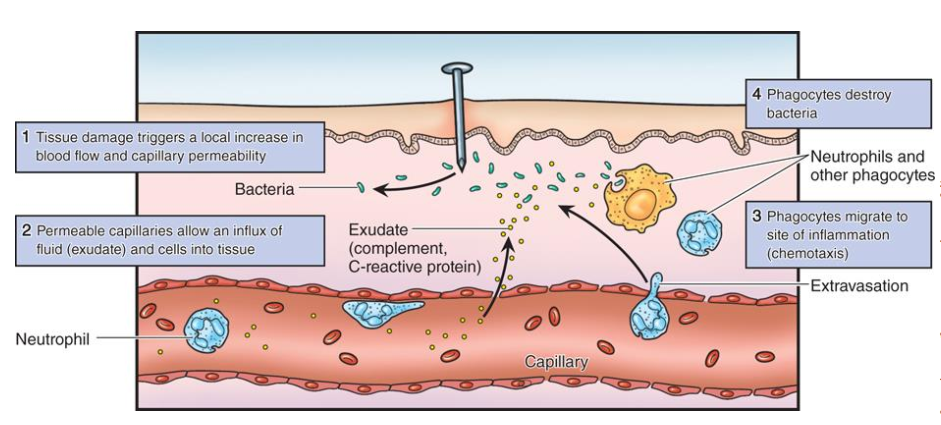
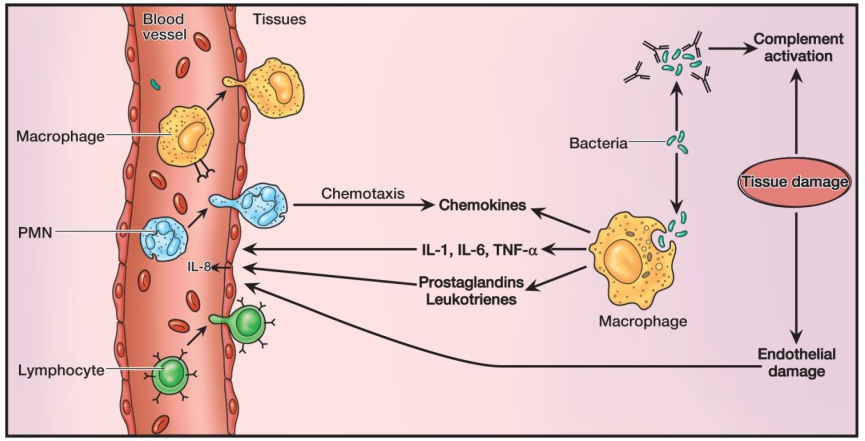
What is Chemotaxis?
The process in which leukocytes migrate towards the infection site in response to bioactive compounds released by leukocytes.
Swarm like migration pattern of neutrophils.
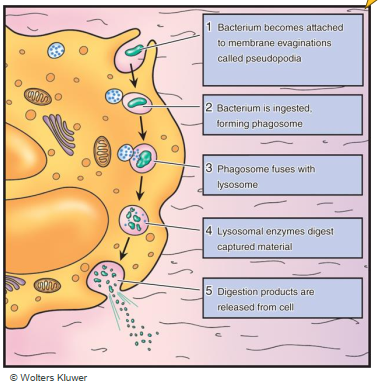
List the 5 steps of Phagocytosis.
Bacteria get attached to Phagocyte pseudopedia (membrane extensions)
bacteria get ingested forming a phagosome
Phagosome fuses with Lysosome
Lysosomal enzymes digest captured material
Digested products are released from the cell.
What is the purpose of Inflammation?
Increase blood flow to deliver immune defending cells to the site of infection/invasion.
Dilation of blood vessels
Increased permeability of blood capillaries
Leukocyte migration into tissues
Describe the symptoms of Acute inflammation.
heat
redness
swelling
pain
loss of function
short-lived
The acute inflammatory response process is initiated by…?
blood vessels near injured tissue
Why does chronic inflammation occur?
occurs when acute inflammatory response was not effective in eliminated the invading MO.
Immune response is defective or aggravated
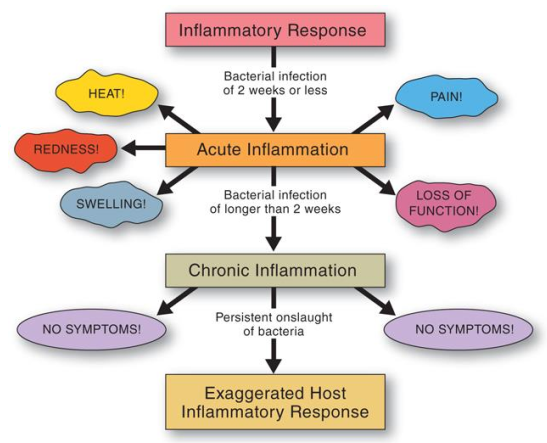
What are the unique signs of chronic inflammation in comparison to acute inflammation?
Chronic inflammation:
Classic inflammatory signs are absent
clinically no pain
Problem may go unnoticed by the host
prolonged inflammation can result in varying degrees of tissue injury
What are the 4 chronic inflammation mediators?
IL1, IL6, IL8 (cytokine)
Leukotrienes
Prostaglandin
TNF-Alpha (cytokine)
What are the effects of IL-1 as a inflammatory biomechanical mediator?
increased vascular permeability
T-cell and B-cell activation
Fever
What are the effects of IL-6 as a inflammatory biomechanical mediator?
increased vascular permeability
T-cell and B-cell activation
Fever
Increased immunoglobulin synthesis
What is the effect of IL8 as a inflammatory biomechanical mediator?
Attraction of neutrophils (PMNs) to infection site
What is the effect of Leukotrienes as a inflammatory biomechanical mediator?
Allow leukocytes to exit the blood vessel and move into CT
What is the effect of Prostaglandin as a inflammatory biomechanical mediator?
Causes Vasodilation (increasing permeability/increasing blood flow)
fever and pain
trigger osteoclasts to destroy alveolar bone
promote overproduction of MMP enzymes (destructive)
What is the effect of TNF-alpha as a inflammatory biomechanical mediator?
Increased vascular permeability
Chemotaxsis
T-cell and B-cell activation
Fever
Systemic effects of inflammation such as loss of appetite, increased HR.
What are some examples of disease conditions associated with chronic inflammation? (7)
Rheumatoid arthritis
Diabetes
Neurological disorders
Cardiovascular disease
Asthma and COPD (Chronic obstructive pulmonary disease)
Gingivitis
Periodontitis
T or F - The presence of periodontal pathogens is sufficient to cause tissue destruction seen in periodontitis.
F - Presence of periodontal pathogens alone is INSUFFICIENT to cause tissue destruction seen in periodontitis.
The host immunoinflammatory response is the direct cause of nearly all destruction seen in periodontal disease
T or F - the host’s defences are employed to save the life of the host and NOT to preserve the tooth or its supporting periodontal structures.
T
What is virulence factor?
Virulence factor is the mechanism that enable biofilm bacteria to colonize and damage tissue of periodontium.
Examples:
lipopolyssachride (LPS) presence on bacteria membrane
bacterial ability to invade
bacterial ability to produce enzymes (acid to weaken enamel)
Which cells are involved in host response to acute inflammation?
inflammatory cells
PMNs
Antigen-presenting cels
T and B cells
Gibroblasts
Epithelial cells
What is Catabasis?
Catabasis is the return to homeostasis after inflammatory process
What are the proinflammation mediators in periodontitis?
Prostaglandins
Thromboxane
Prostacyclin
Leukotrienes
What are pro-resolving lipid mediators?
AKA shut-down mediators
They work to:
terminate PMN recruitment
stimulate macrophages to remove dead cells
Promote antibacterial activities
Promote tissue repair and regeneration
What are biochemical mediators? What are the 3 most important ones?
Biochemical mediators are biologically active compounds secreted by immune cells that activate the bodys inflammatory response
Most important BMs:
Cytokines
Prostaglandins
Matrix Metalloproteinases (MMPs)
Which biochemical mediator is capable of initiating and perpetuating irreversible tissue destruction and bone loss in chronic inflammatory diseases?
Cytokines → IL1, IL6, IL8, TNF-alpha
Which prostaglandins types are important? Which one specifically plays a role in bone destruction in periodontitis?
Prostaglandin types: D, E, F, G, H, I
Prostaglandin E (PGEs) = bone destruction in periodontitis.
Which immune cells produce MMP (matrix metalloproteinases)? What is its function?
PMNs
Macrophages, Gingival fibroblasts
JE cells
Fx: enzyme that acts together to break down CT matrix.
______ balance helps maintain the integrity and health of connective tissue.
MMP-TIMP relationship
TIMP = tissue inhibitors of matrix metalloproteinases
TIMP regulates MMP
Overproduction of MMPs result in ?
results in breaking down of the connective tissue in the periodontium.
High MMP levels = extensive collagen destruction
Summarize the biomechanical mediators local effects in Periodontitis.
IL1 → stimulate osteoclast activity causing bone resorption; break down collagen matrix in periodontium
IL6 → stimulates bone resorption and inhibits bone formation
IL8 → stimulates CT destruction and bone resorption
TNF-alpha → stimulates bone resorption; break down collagen matrix in periodontium
PGE → stimulates MMP secretion and bone resorption
MMP enzymes → induces break down of collagen matrix in periodontium
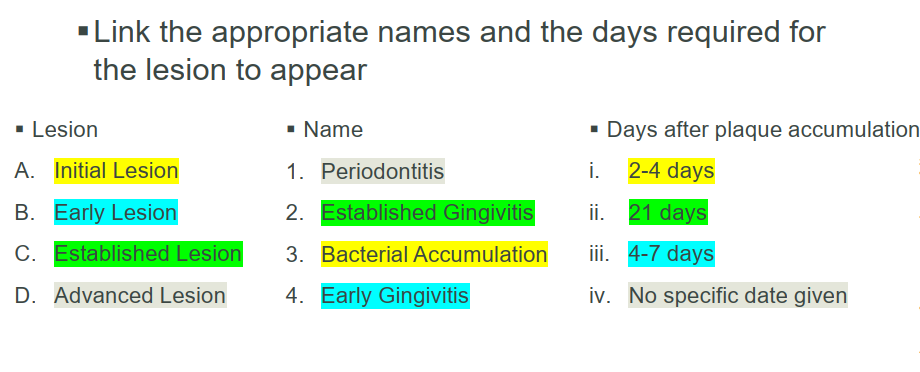
What are the 4 Histologic stages of Periodontal Disease development?
Initial Lesion AKA Bacterial Accumulation (2–4 days)
Acute inflammation, vasodilation, ↑ neutrophils, ↑ gingival crevicular fluid.
Clinically: gingiva looks healthy
Host response successful if most bacteria destroyed (gram neg)
Early Lesion AKA Early Gingivitis (4–7 days)
Forms “wall of cells” between biotilm and sulcus wall, releasing more cytokines
Macrophages recruited
JE proliferates, SE forms epithelial ridges
Clinically: inflammatory changes, erythema, edema, bleeding on probing.
Established Lesion AKA Established gingivitis (21-days after biofilm acc.)
JE loosens attachment to root surface, being to form pocket epithelium
Clinically: chronic gingivitis, persistent inflammation, bleeding.
Patient education is vital in controlling bacterial challenge
Advanced Lesion AKA Periodontitis (no specific date)
Plaque biofilm grows laterally and apically along root surface
Irreversible tissue destruction by PGE2 (destroy alveolar bone)
Clinically: periodontal pocket formation, BOP, Periodontium destruction, furcation, tooth mobility
Chronic infection induces chronic inflammation = more damage to periodontium