Therapeutic exercises (copy)
1/110
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
111 Terms
What are the 3 goals for Therapeutic Exercises?
Achievement of symptom-free movement and function
Carefully graded stresses and forces applied to body (certain tissues can only deal with certain stresses in certain phases of healing ex) post op pts
Applied in controlled, progressive and appropriately planned manner
What are the 4 parts of the NAGI Model?
Pathology
Impairment
Functional Limitation
Disability
What is Pathology in the NAGI Model?
Disease, Disorder, Condition (Rotator Cuff tear)
What is Impairment in the NAGI Model?
consequence of pathology, any loss or abnormality of psychological, physiologic or anatomic structure or function ( ROM, nerve mobility, coordination, balance, muscle power loss)
What is Functional Limitation in the NAGI Model?
a limitation from an impairment that is not disabling, yet interferes with daily function (Thing pt is having trouble doing in daily life) ( postal worker cant lift up bags of mail)
What is Disability in the NAGI Model?
an inability to undertake normal activities of daily living (ADL's), or tasks at home, work, recreation or in the community
What does the NAGI Model also encompass?
Societal function or lack thereof
What is a PT Diagnosis?
It is the relationship of a patient's impairment to their functional limitations (
(Ex. Decreased Right Glenohumeral ROM (Shoulder flexion 95 deg) resulting in inability to stack boxes on top shelf at work.)
(Ex. Decreased Right Glenohumeral ROM (Shoulder flexion 95 deg) resulting in inability to stack boxes on top shelf at work.) Of this example, what is the impairment and what’s the functional limitation?
impairment: the ROM
Functional limitation: unable to stack boxes on top shelf at work
What does a pt Subjective consist of? And why do you need to capture all the basic info?
"Body chart", case history, description of symptoms (pt SINS)
capturing all the basic info that’s helping drive the pattern recognition
What is an Objective? And the concept
Systematic administration of test or movements to define impairments and its relationship to the functional limitation
systematically do some tests and movement to help pick out impairments (remember the triangle!= and march up that triangle and determine if all systems are good or which of these systems are normal and you will target that system and you will see if that will affect the pts asterisk sign or the functional movement that is painful
What else do you do in objective ?
Observation and Inspection
Provocation
Motion-pain relationship
Resistance Testing
Joint Mobility Testing
Hypothesis Testing
Regarding objective, what does motion - pain relationship mean?
We are trying to decide if pt is pain dominant meaning pain limited, they are irritable or are they resistance limited in their movement which means they are stiff more so than painful
Give an example of hypothesis testing?
ex) is think the pts limited ROM is the cause of their pain, so, I want to restore that” then restore that and see if the functional limitation has improved
What is a Prognosis? A prediction of what? It’s the anticipated length time of what?
A prediction of the patient's optimal level of function expected at the end of treatment
Anticipated length of time needed to reach the specified functional outcome
What are 6 factors that can influence Prognosis?
Complexity, severity, acuity or chronicity of proble (More impairments/pain/inflammation etc means longer it will take for it get better)
General health ( how it affects how active they can be and how quickly their tissues recover)
Patient goals
Patient's motivation
Safety issues ( protocols like early stages of post op)
Extent of support (physical, emotional, social) (more support the better they recover)
What are 6 factors influencing decision when developing a plan?
Impairments, functional limitations or disabilities
Psychological status of patient (pt motivation towards PT)
Socioeconomic and cultural factors
Home environment/ Family support
The patient's and employer's vocational plan (getting them back to work and how physically demanding it is)
Ethical considerations ( how long you will be able to treat them if their are having true impairments unless they are faking it) ex) workers comp has a history of this
What is a Long Term Goal?
how treatment will affect the functional limitations or disability at the conclusion or rehab
Ex) carpal tunnel: returning to a job like typing and using their hands which will cause the reoccurrence of the issue and they should think if they would want to return to that job
What is Short Term Goal?
measurable behavioral objectives affecting the documented impairments
What can Short Term Goals reflect?
May reflect component abilities or skills to achieve functional goals (Ex. Increase strength and ROM)
What are 2 things PT should do when evaluating a plan?
Compare original data with current data at frequent intervals
its important to measure everything in the eval and you’re going to want to reassess the rom and such to see if the pt is getting better or not
Identify goals that have been met, change those that need further modification
What is Strength/Muscle Performance?
The ability of a muscle or muscle group to produce tension
How is Strength/Muscle Performance assessed? (2)
MMT OR Functionally by having pt lift and equivalent weight as in their functional limitation
What are 7 factors that can influence strength?
Cross sectional size
Length-tension relationship
If its Optimal, too short = active insufficiency, too long = passive insufficiency
Recruitment of motor units
Type of muscle contraction (Iso/Con/Ecc)
Fiber type (Type I vs Type II)
Energy store and blood supply
Speed of contraction -greater torque at lower speeds
Motivation of patient
What are 3 ways to increase Neuromuscular strength?
Hypertrophy
Possible Hyperplasia( more cells)
Increased recruitment of motor units ( physically tap that muscle to teach pts to turn it on)
Early strength gain is often due to what?
motor learning (meaning because they are learning to activate those muscles)
What is Hypertrophy? Increased amount in what 3 things?
Tissue protein
Density of capillary beds
Size of Type 2 Fibers
What are 3 types of non-contractile tissue?
Bone, Tendon, Ligament (these benefit from resistance training)
Skeletal tissue strength can increase help with what else? And how?
can help with osteoporosis (muscle pulling on the bone is stress/loading on the bone)
Where can Ligament and Tendons gain strength?
Musculotendinous Junctions and Ligament Bone Interfaces (due to increased load/stress)
What are the 3 guidelines for increased strength?
Overload Principle
High loads, low reps- performed to fatigue
Varying type and structure of exercise program
Don’t give ________ dosages!
random
Regarding varying type and structure of exercise, What type of muscle contraction can you start with?
You can start with isometrics initially then onto eccentric/concentric
What is the Overload Principle?
A load that exceeds metabolic capacity
What is Endurance necessary for?
Necessary for performing repeated motor task in daily living
What are the 2 types of endurance?
Muscle and general body endurance
What is Muscular Endurance? ****
Ability of muscle to contract repeatedly or generate tension, sustain it and resist fatigue over a prolonged period
What is General Body Endurance?****
Ability of a individual to sustain low intensity exercise such as walking; jogging over an extended period
Why is aerobic conditioning/general body endurance very important ? Indicated for what? Helpful for who? How about the people that cant put too much weight?
indicated for LBP likely and helpful for pts that have degenerated issues in their hips and knees…. People that cant put too much weight on their extremities then you can put them on the exercise bike
What is General Body Endurance AKA?
Aerobic conditioning
What are 5 Muscular/ Cardiovascular/ Pulmonary immediate changes?
Inc. blood flow to muscle
Inc. HR
Increased arterial BP due to inc. stroke vol and cardiac output
Increased O2 demand and consumption
Increased respiratory rate and depth
What are long term adaptive strength changes in Muscle?
Capillary bed density increase
What are long term adaptive strength chances in Cardiac and Vascular Changes? What increases and what decreases ?
Cardiac output and stroke volume increase
Resting HR decreases and return to resting from exercise quicker
Guidelines for Developing Endurance: Muscular Endurance
Active exercise performed repeatedly against a moderate load to the point of fatigue
Guidelines for Developing Endurance: General Body Endurance
directly exercising large muscle groups (walking, running, swimming, cycling)
Exercise prolonged > 20 minutes
Exercise every other day
To maintain healthiness its recommended to get some type of what daily???
exercise - josh
Regarding mobility and flexibility, mobility of what is important for what?
Mobility of contractile and non-contractile tissue is important for normal function
What is Normal Motion of muscle?
constant elongation and contraction of tissues
What is Restricted Motion of muscle?
Adaptive shortening
Give an example of adaptive shortening, how did it happen? What could it create in the capsule ?
which means they have had a TKA and no one has helped straighten that knee out, all that swelling which could lead to fibroplasia (more cells being produced) which might allow a contracture in the capsule… so it’s important to reduce this adaptive shortening to increase flexibility and mobility
What is considered a Diseased or Trauma motion of muscle?
Pain, weakness or inflammation which can decrease mobility and result in adhesions and contractures
What do muscles do when stimulated? Relaxes after what? Can be what? Immobilization results into what?
Shortens <<
Relaxes after contraction
Can be passively stretched
Immobilization results in adaptive shortening
Connective Tissue Characteristics (3)
Non-Contriactile
Adaptively shortens
Supple and can be lengthened by passive stretch
Regarding connective tissue, can it contract or relax? How can you lengthen them?
No it cant
With just passive stretching and end range stretching
Scar Tissue Characteristics, does not yield to what? Non what for 2 things, what do you need to avoid?
Does not yield to stretch
Non-resilient
Non-elastic
Avoid prolonged immobilization
Immobilization is _____ and very _____….. when do you want to get them moving by?
Common and very ciritical
Want to get them moving as soon and as safely as possible
Regarding skin, what’s suppleness important??? And what else is important??
it must be stretch for joint motion to occur
Early mobilizations is important
How can skin develop motion limitations?
After burns, trauma, surgeries
What is Stability?
Synergistic co-ordination of neuromuscular system to provide a stable base for superimposed functional movements (Stable base for movement to occur)
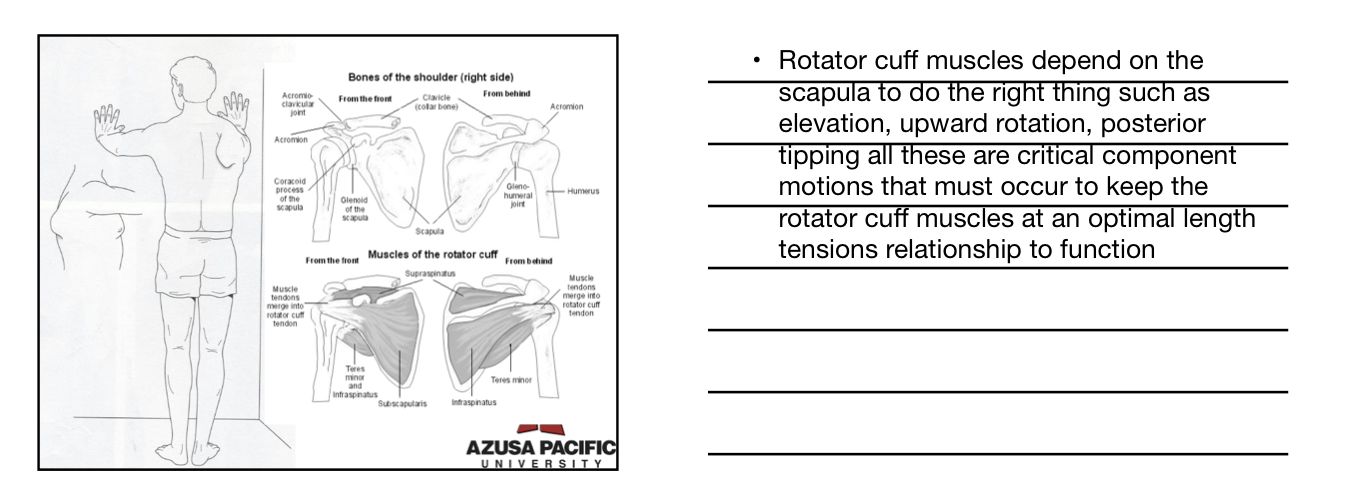
What structures is Stability very important for?
Proximal Structures <<
Trunk
Hip
Shoulder Girdle
What can decreased stability proximally cause?
Excess stress on certain structures w distal mobility
How can a pt develop Stability? Control what? Maintain what? (2)
Pt. must learn to control proximal area
Must maintain stable, well aligned posture
How can they control the proximal area??
by strengthening the muscles in the h proximal area and cure the muscles to fire at the right times
How can a pt develop stability while carrying out a functional task? (4)
Start in single plane motions (be able to maintain stable and well aligned posture while doing functional tasks)
Progress to controlled diagonals (multiple plane motions)
Endurance must be developed in stabilizers (glute med, glute max, mid&low traps)
Work in components then progress to full functional activity (work in short arcs of movement and then progress to full functional activity)
What is Relaxation?
conscious effort to relieve tension in muscles
What occurs after active contraction of muscle?
Reflex Relaxation occurs
What can decrease muscle tone?
Conscious thought
Biofeedback
Transcendental meditation
What are 4 guidelines for Relaxation?
Place patient in comfortable position
All body parts well supported
Pt. taught to progressively contract and relax musculature
Use deep breathing
Give an example of relaxation
What are Coordination, Balance, and Functional Skills dependent on?
Sensory system
Somatosensory and proprioception
What is Coordination?
Ability to use the right muscles at the right time
w/ appropriate sequencing and intensity
What is Coordination the basis of?
Smooth and efficient movement
What is Balance?
Ability to maintain the center of gravity over the base of support; usually when upright
What is Balance a combination of? Give an example
Stability and mobility
Hips need to be strong enough to stay in the right place
Need to have joint motion in ankles and knees for the movement strategies
Where is Balance needed?
Needed to hold a position in space or move in a controlled- coordinated manner
What is Functional Skills?
Refer to varied motor skills necessary to function independently in all aspects of daily living (includes balance, coordination, and stability.)
What are 6 Guidelines of Developing Coordination, Balance, and Functional Motor Skills? Constant repetition of what? Use what type of cues? Progress from what to what? Emphasize Stability before what? Simulate real what? As what improves, what should increase?
Constant repetition of simple → more complex motor activities
Have pt do a mini squat, tap on glute med to prevent pelvis from tipping or off balance, make sure it’s aligned
Use of sensory cues (tactile, visual, proprioceptive, verbal)
Mirrors
Progress from single straight plane to combined motions and diagonals
Emphasize proximal stability before distal mobility
Simulate real specific functional activities
Instead of jumping then go to squats and eventually into deeper squats then short jumps and then full jumps
As quality of motion or motor skill improves, speed and timing should be increased
How can a PT prepare for Exercise Instruction? Do what ahead? What type of relationship (2) ? Identify what 2 things for the pt ?
Plan ahead
Positive therapist/patient relationship
Collaborative relationship (help them understand why your re giving these exercises and don’t give too many)
Identify patient's learning style (decide if they need a vid of themselves or a printed list of exercises)
Identify patient's attitude towards exercise (some pts love to exercises so you need to slow them down, some ppl hate it so you need to give them little by little)
What is Motor Learning? (3) what type of processes? What type of acquisition and retention ? Involves what?
Complex set of internal processes
Relatively permanent acquisition and retention of a skilled movement/task
Involves practice
What are the 3 types of Motor Tasks?
Discrete, Serial, Continuous
What is Discrete Task? Example?
Movement w recognizable beginning and end
Ex. Push up, lifting weights
What is Serial Task? Example
Composed of series of discrete tasks combined in a particular sequence
(Ex. Eating w fork = appropriate grasp, proper positioning scoop up food, move fork to mouth)
What is Continuous Task? Example
Repetitive, uninterrupted movement w NO distinct beginning or end
(Ex. Cycling, walking up and down stairs)
What are the 3 Stages of Motor Learning?
Cognitive, Associative, Autonomous
What is Cognitive Stage? (5) Requires a great deal of what? Patient thinks about what? What’s common? Pts are easily what? Requires a lot of what?
Requires a great deal of thinking
Patient thinks about sequence or each component
Errors in performance common
Pt. easily distractible
Requires a lot of feedback
What is Associative Stage? (6) Pt makes what ? Concentrates on what? Tries to become more what? Use of what type of skills? Modifies activities depending on what? Decrease in need for what ?
Patient makes infrequent errors
Concentrates on fine-tuning the motor task
Patient tries to become more efficient and consistent
Use of problem solving skills
Modifies activities depending on environment
Decrease in need for feedback
What is Autonomous Stage? (5) movements are what? Pt can do what ? Easily adapts to what? Very little what is required? Pts are often what before this stage?
Movements are automatic
Patient can do multiple tasks at once
Easily adapts to variations in task demand
Very little feedback or instruction required
Patients often discharged before this stage...*****
What are 3 Variables that influence Motor Learning?
Pre-Practice Considerations
Practice
Feedback
What is Pre-Practice Considerations? (4) Understanding why what? Ability to do what? Demonstration of what? Pre - practice what that is clear and succinct ?
Understanding why they are doing it
Ability to pay attention
Demonstration of task for patient
Pre-practice verbal instruction that is clear and succinct
What is the MOST important part of Motor Learning?
PRACTICE
What are the 3 Types of Practice?
Part v Whole Practice
Blocked v Random v Random Blocked
Physical v Mental
What is Part v Whole Practice?
whole practice is a jump ( From a deep squat all the way to a full jump). Part practice is just a mini squat (make sure our knees dont drive in or go over our toes
What is Blocked v Random v Random Blocked Practice?
blocked: ask a pt do a sit to stand from a plinth at a fixed height(cue to lean fwd, keep feet underneath them and extend at the hips)…. They are doing the same thing over and over again
Random: ask pt them to do a STS from a chair then stool then a table and a plinth
Random blocked: you are going to do 10 STS from the plinth then 10 more at this chair
What is Mental v Physical Practice?
mental: asking them to picture and think of the alignment in their knees and legs
Physical: actually doing it yourself
What is feedback? What’s being received and by who? When do you give feedback?
Sensory information received by learner
Either during or after performance of task
What 3 things must a PT decide when providing feedback?
Type of feedback
Amount of feedback
Timing of feedback (Before/after)
What are the 6 types of feedback?
Intrinsic
Augmented
Concurrent
Terminal
Immediate
Delayed
Summary
What is Intrinsic Feedback? (3)
Sensory cue inherent in task
Arises from performance of task
Usually proprioceptive, kinesthetic, tactile, visual, audio