WKU Med Surg 2 Exam 2 Dysrhythmias
1/136
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
137 Terms
what is automaticity
hearts ability to automatically start a beat (pacing function)
what is excitability
heart has the potential to respond to an impulse
what is conductivity
allows passage/sends electrical impulse
what is contractility
heart responds to impulse by contracting and pumping blood
what is the conduction pathway in the heart
1. SA node
2. AV node
3. bundle of his
4. right and left bundle branches
5. purkinje fibers
what is the SA node
hearts primary pacemaker that generates a HR between 60-100 bpm
what happens if the SA node fails
the AV node takes over and produces a HR of 40-60 bpm
what happens if both the SA and AV nodes fail
bundle of his takes over and produces a HR of 20-40 bpm
how many different types of leads are there
- 3 lead: white, black, red
- 5 lead: white, black, green, red, brown
- 12 lead: provides 12 views of cardiac electrical activity
how many electrodes are used in a 12 lead
10: 4 on limbs, 6 on chest
what is a 12 lead used for
diagnose dysrhythmias
what should you teach the pt about a 12 lead
lie still and breathe normally
what makes 12 leads different from other leads
not a continuous monitor: only looks at a 1 time still frame
what is a ECG
graphic representation of cardiac electrical activity
what things are included in a ECG
- requires placement of electrodes
- lead systems provide various views from different sides of the heart: determines if SA node is stimulating every part of the heart
what are the different patterns in a ECG
- isoelectric line
- positive deflection
- negative deflection
what is the isoelectric line
flat line part; see no electrical changes at that time (PR and ST segment)
what are positive deflections
waves that go above isoelectric line (P wave, part of QRS)
what are negative deflections
waves that go below isoelectric line (part of QRS)
what does the x axis of a ECG strip represent
duration/ time
what does the y axis of a ECG strip represent
amplitude/ voltage
how many sec are 5 boxes on a ECG
0.20 s
how many sec is 1 box on a ECG
0.04 s
what are the normal parts of an ECG
- p wave
- PR segment
- PRI
- QRS complex
- ST segment
- t wave
- QTI
what does a p wave represent
SA node fired and atrial depolarized (contracted)
what does a PR segment represent
atrial kick (last squeeze from atria)
what does a PRI represent
- contains P wave and PR segment
- full length of time for atrial depolarization
what is the normal time of a PRI
0.12-0.20 s
what does a QRS complex represent
ventricular depolarization (contraction)
what is the normal time of a QRS complex
0.04-0.10 s
what time frame of a QRS complex starts to become concerning
>0.12 s
what does a ST segment represent
- early ventricular repolarization (relaxation) starts
- starts from J point and goes to the beginning of the T wave
which part of a ECG do most lethal dysrhythmias occur
t wave (esp electrolyte imbalances like K which causes a peaked t wave)
what does a t wave represent
completing ventricular repolarization (relaxation)
how tall is a t wave usually
<10 mm
what does a QTI represent
- full time for ventricular depolarize and repolarize
- starts at the beginning of QRS and ends at the end of the T wave
what is the normal time of a QTI
0.32-0.44 s
U wave
never supposed to be part of ECG
opposite of T wave
indicates hypokalemia → bc slowing ventricular repolorization
occurs after T wave
what is the 6 s strip method for determining HR on a ECG
count ventricular rate and times it by 10 (goes for both ventricular and atrial rate)
normal sinus
∙ Rate - 60-100
∙ Regularity of Rhythym - Regular
∙ P wave - round, upright, and symmetrical
∙ P:QRS - 1:1
∙ PRI: 0.12 - 0.20 seconds
∙ QRS: 0.04-0.10 seconds
sinus arrhythmia
gradual change between the distance in the beats
rate: 60-100 → not consistent (increase & decrease_
rhythm - regularity varies w/ breathing (irregular)
p wave - round, upright, symm
P:QRS - 1:1
PRI: 0.12-0.20
QRS: 0.06-0.10
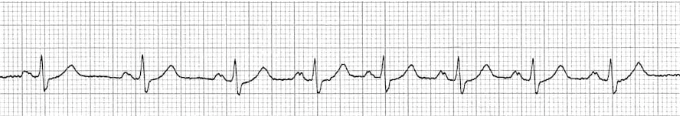
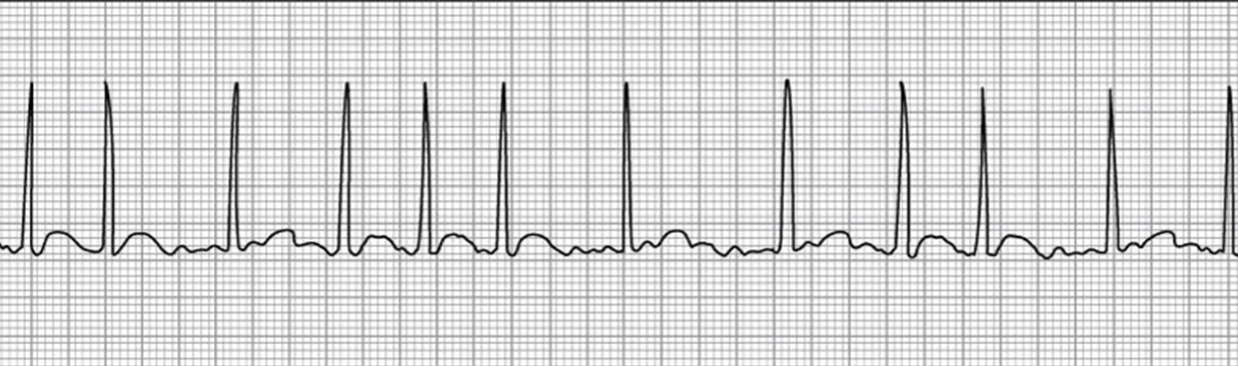
what rhythm is this
sinus arrhythmia
sinus tachycardia
∙ Rate: > 100 beats/min
∙ Regularity of rhythm: regular
∙ P wave: round, upright, and symmetrical
∙ P:QRS = 1:1
∙ PRI: 0.12 to 0.20 sec and constant
∙ QRS: 0.06 to 0.10 sec and constant
what can cause sinus tachycardia
- hypovolemia - losing all volume → HR increases to compensate
- enhanced automaticity
- increased sympathetic (fight or flight) activity
- hypoxia - if can’t breathe → HR increases to try to circulate O2
what are the s/s of sinus tachycardia
- palpitations
- chest pain
- restlessness, anxiety
- SOA
- hypotension
- HF: dyspnea, crackles, JVD, fatigue, weakness
how should you tx sinus tachycardia
tx the cause
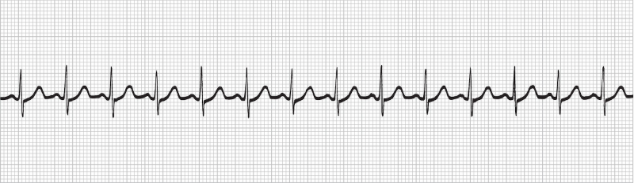
what rhythm is this
sinus tachycardia
sinus bradycardia
∙ Rate: < 60 beats/min
∙ Regularity of rhythm: regular
∙ P wave: round, upright, and symmetrical
∙ P:QRS = 1:1
∙ PRI: 0.12 to 0.20 sec and constant
∙ QRS: 0.06 to .10 sec and constant
what are the causes of sinus bradycardia
- decreased automaticity
- increased parasympathetic (rest and digest) activity: vagal response
when do you tx someone with sinus bradycardia
if they are symptomatic and HR is <50 bpm
need to know if acute/chronic → if it’s something that is baseline w/ no s/s → no tx
what are the s/s of sinus bradycardia
- syncope
- dizziness
- hypotension
- confusion
what is the first line tx for sinus bradycardia
atropine - 1mg q3-5 mins w/max of 3 mg → bolus
what are some other tx options for sinus bradycardia
transcutaneous pacemaker - deliveers smaller stimulus to try and generate pace that is effective
dopamine or epinephrine IV infusions
transvenous pacing: continuous pacemaker used for symptomatic bradycardia
what is a permanent pacemaker
battery powered device that delivers electrical stimulus to the right myocardium which causes a contraction
always sending little stimulus
indicated for symptomatic bradycardia
what should you monitor for/ teach to someone who got a permanent pacemaker
monitor for infection/ hematoma at insertion site: assess for bleeding, swelling, tenderness, redness
monitor for complications
dressing CDI (typically for 24 hrs) → shower day after removed
follow activity restrictions: no lifting, no big arm movements for first 24 hrs → sling used
teach self management → always carry info card
what are some complications of permanent pacemakers
ectopic beat (PVCs)
malfunction
electromagnetic interference: pts cannot have MRIs unless you know the material is not magnetic
stimulation of chest wall due to lead coming unattached from heart and sticks to chest: can cause perforation and cardiac tamponade (s/s: consistent hiccupping)
what is a temporary pacemaker
emergency management of bradycardia
two types
transcutaneous = external → use Lifepak
transvenous system = internal
ACLS: Bradycardia Algorithm Steps
Identify and treat underlying cause
Identify if persistent bradyarrythmia is occurring and causing different symptoms → no (mon and observe) or yes (move to step 3)
Move to administering atropine → is it effective? → yes (move to step 4) or no (administer other)
considering additional things
ACLS: Bradyarrhythmia Step 1. Identify and treat underlying cause
- maintain patent airway; assist breathing as necessary
- O2: if hypoxemic
- cardiac monitor to identify rhythm; monitor BP and oximetry
- IV access
- 12 lead ECG if available; dont delay therapy
- consider possible hypoxic and toxicologic causes
ACLS: Bradyarrhythmia Step 2. persistent bradyarrhythmia - what can this cause/what should you monitor for
- hypotension
- acutely altered mental status
- signs of shock
- ischemic chest discomfort
- acute HF
ACLS: Bradyarrythmia Step 3. Administering Atropine
If atropine ineffective:
Transcutaneous pacing
and/or
dopamine infusion or epinephrine infusion
ACLS: Bradyarryhtmia Step. 4 - after giving tx meds for persistent bradyarrhythmia, what should you consider
- expert consultation
- transvenous pacing
what are premature atrial contractions (PAC)
this is an ectopic or "extra" beat occurring within a rhythm
the atrial beat (p wave) comes early
p wave: abnorm → don’t use to measure PRI
P:QRS - 1:1
QRS: norm
what should you consider/ use to tx for PACs
treat the cause!
caffeine
alcohol
stress, stimulants, anxiety
inflammation/ irritability in heart tissue
electrolytes
need to know if baseline or new
when should you start becoming concerned about PACs
when you have a lot or recurrent ones → frequeny can lead to atrial dysrhythmias
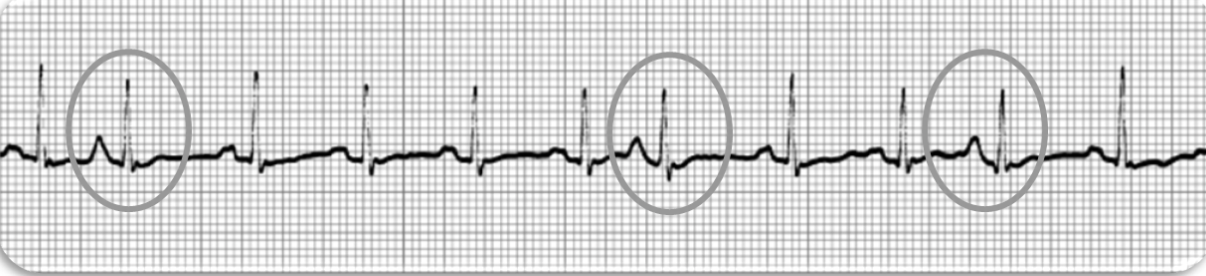
what rhythm is this
premature atrial contractions
Ex: Sinus tachycardia with PAC → how to describe it
what is supra ventricular tachycardia (SVT)
atrial prob bc supra (on top) → above ventricles
rapid stimulation of atrial tissue
occurs rapidly and is consistent → in norm rhythm, then jump into SVT
ECG values for SVT
∙ Rate: 100-280 beats/min (usually > 150)
∙ Regularity of rhythm: regular
∙ P wave: may not be visible
∙ P:QRS = typically unmeasurable
∙ PRI: typically unmeasurable
∙ QRS: norm
what are the causes of SVT
- usually reentry mechanism over stimulation
- starts in atria
what are the s/s of SVT if it persists
- palpitations
- chest pain
- weakness
- fatigue
- SOA
- nervousness, anxiety
- hypotension
- syncope
when should you start becoming concerned when it comes to SVT
when there is cardiovascular deterioration → not enough time for ventricles to stretch and fill → can’t effectively pump
SVT tx for stable pt
vagal maneuvers → can reset conduction pathway → if works, still need to find underlying cause
adenosine IV (1st line) - chemical cardio version → temp send into asystole to send rhythm back into NS
given as stop-cock (med on one side and flush on other) → have to give med and then flush immediately after to push adenosine in all the way
SVT tx unstable pt
- CARDIOVERSION → more likely to resolve condition
- adenosine IV - 6mg for 1st dose, 12 mg 2nd dose as needed
what rhythm is this
supraventricular tachycardia
what is cardioversion indicated for
- symptomatic/ unstable SVT
- afib with RVR
- monomorphic Vtach (with a pulse)
- tachydysrhythmias unresponsive to other txs
what should you consider before cardioversion
- sedation
- turn off O2
- clear from shock
what is important to do during cardioversion
- start slow, charge per order
- sync the rate so that the pt is receiving the same rate the whole time
what should you do after cardioversion
- maintain airway, oxygenation
- assess VS, LOC, and skin
- monitor for dysrhythmias
- administer prescribed antidysrhythmic
- document results
- watch ABGs
what is atrial fibrillation
rapid and irregular electrical impulses in atria → they fibrillate (quiver) instead of contracting → can’t fill ventricles effectively → decreased CO
heart weak in general
ECG values for A-FIB
∙ Rate: Atrial = 350-600; Ventricular = variable (up to 200s)
∙ Regularity of rhythm: irregularly irregular
∙ P wave: unmeasurable; quivering
∙ P:QRS = no P waves; variable
∙ PRI: unmeasurable
∙ QRS: 0.04 to 0.10 sec
∙ T wave is often hidden
what is A-FIB with RVR
A-FIB w/ tachycardia
what are the causes of afib
- HTN, CHF, CAD, hyperthyroidism
- associated with DM, sleep apnea, mitral valve disease
concerns w/ A-FIB
∙ Loss of atrial kick - no PR segment
∙ Loss of ventricular filling time r/t rapid ventricular rate (RVR)
∙ Loss of muscle mass in atria - bc not contracting effectively (so they become weak)
∙ Risk of clotting - blood isn’t effectively moving out, so it is just sitting (stasis)
how do you tx A-FIB
consider underlying cause
ex: if potassium and magnesium imbalanced → correct mag and then k → will see improvement
acute vs. chronic
tx of acute A-FIB
control the rate and convert the rhythm
if stable → meds
IV antidysrhythmics- diltiazem, amiodarone, ibutilide
Beta Blockers (metoprolol, esmolol)
Digoxin (often used in cases with HF)
if unstable → cardioversion
if persistent → anticoagulant (heparin) IV
tx of chronic A-FIB
control the rate and anticoagulate
Same medications for stable, but PO
Anticoagulant
Left atrial appendage closure
Radiofrequency catheter ablation
Biventricular pacing
MAZE procedure
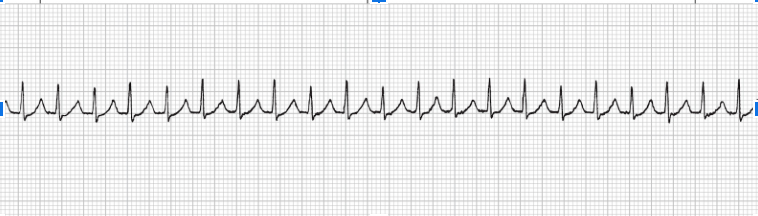
what rhythm is this
atrial fibrillation
what is atrial flutter
routine fluttering of atria → atria going much faster than ventricle
* in most cases, tx same as a-fib
atrial flutter ECG values
∙ Rate: Atrial = 250-400; Ventricular = variable
∙ Regularity of rhythm: usually regular
∙ P wave: saw tooth
∙ P:QRS = variable (Ex: 4:1)
∙ PRI: unmeasurable
∙ QRS: 0.04 to 0.10 sec
∙ T wave is not visible
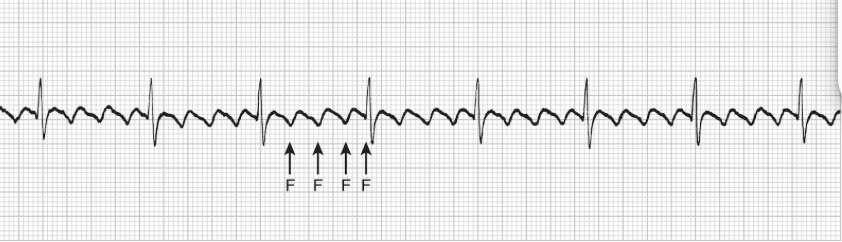
what rhythm is this
atrial flutter
what is the first step in the tachyarrhythmia algorithm according to ACLS
identify a HR of >150/ min
ACLS: Tachycardia Algorithm Steps
Assess appropriateness - HR > 150
Identify and treat underlying cause
Identify is persistent tachyarrythmia is occurring and causing s/s - no or yes (step 4)
Synchronized cardio version
If refractory, consider
ACLS: Tachycardia Algorithm Step 1. - how do you identify and tx underlying causes
- maintain patent airway, assist breathing as necessary
- O2 if hypoxemic
- cardiac monitor to identify rhythm; monitor BP and O2
- IV access
- 12 lead ECG
ACLS: Tachycardia Algorithm Step 2. - Is persistent tachyarrythmia occurring and is it causing these
HOTN
acutely altered mental status
signs of shock
ischemic chest discomfort
acute HF
ACLS: Tachycardia Algorithm Step. 2 - if tachyarrhythmia is not causing s/s, what should you assess for next
wide QRS
ACLS: Tachycardia Algorithm Step 2. - if the pt does not have a wide QRS, what should you do next
- vagal maneuvers (if regular)
- adenosine
- beta blocker or calcium channel blocker
- consider expert consultation
ACLS: Tachycardia Algorithm Step 2. - if someone does have a wide QRS with tachyarrhythmia, what should you consider
- adenosine only if regular and monomorphic
- antiarrhythmic infusion
- expert consultation
ACLS: Tachycardia Algorithm Step 3. - if tachyarrhythmia is causing s/s, what should you do
- prepare for synchronized cardioversion
- consider sedation
- if regular narrow complex, consider adenosine
ACLS: Tachycardia Algorithm Step 4 - if someone has refractory with tachyarrhythmia after cardioversion or med tx what should you consider
- underlying causes
- need to increase energy level for next cardioversion
- addition of antiarrhythmic drug
- expert consultation
what is the dosage for adenosine
6 mg rapid IV push with NS flush for first dose and 12 mg for second dose