Respiratory System
1/4
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
5 Terms
Respiratory System in Speech
Key Structures:
Diaphragm: Major muscle for inspiration.
Lungs: Provide the air supply for phonation and speech.
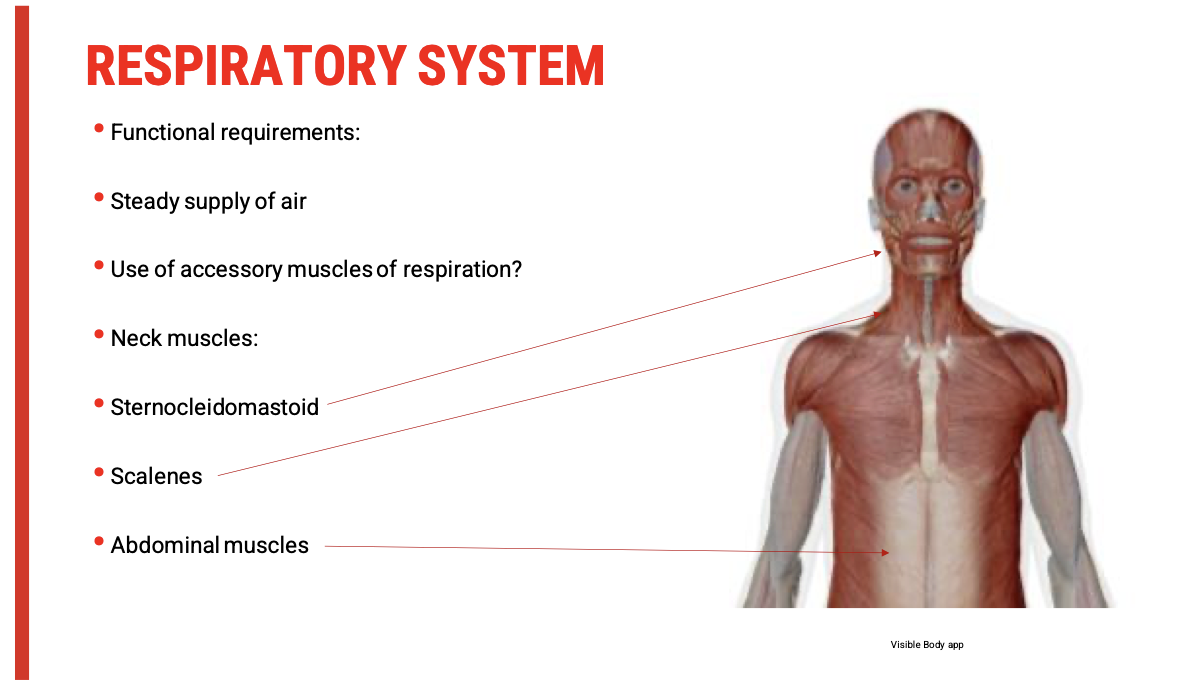
Other associated muscles: intercostals, abdominals, and accessory respiratory muscles support controlled airflow during speech.
Function in Speech:
Generates subglottic air pressure necessary for:
Phonation (voice production via vocal folds)
Speech intensity (volume)
Prosody and phrasing (breath groups)
Controls speech timing and fluency through regulated exhalation.
🧍♀ Relevance to Freda (Parkinson’s Disease)
Parkinson’s impact on respiration may include:
Reduced respiratory drive (due to basal ganglia dysfunction)
Poor breath support for phonation (soft voice)
Monopitch and monoloudness
Short phrases due to limited air support
This contributes to the hypokinetic dysarthria profile.
Types of Respiration Relevant to Assessment
Respiration Type | Description | Relevance to Speech/Assessment |
Quiet Inspiration | Passive breathing in at rest, mostly via diaphragm | Baseline respiratory capacity |
Quiet Expiration | Passive breath out, no muscle activity | Not sufficient for speech needs |
Forced Inspiration | Active engagement of accessory muscles (e.g., sternocleidomastoid, scalene) | May signal respiratory weakness if relied on during speech |
Forced Expiration | Active abdominal and intercostal contraction | Essential for adequate subglottic pressure in speech |
🩺 Assessment Questions to Consider
Is the client using only the diaphragm, or are accessory muscles (e.g., neck and shoulder movements) visibly overactive?
Is speech breathy or weak? → May suggest insufficient subglottic pressure.
Does the client fatigue quickly when speaking?
Are there short utterances or irregular phrasing due to poor breath support?
🧑⚕ How Do We Detect Forced Inspiration?
Observation: Watch for shoulder elevation, neck tension, clavicular breathing.
Palpation: Assess upper chest versus abdominal breathing.
Speech Tasks: Ask client to count aloud, read a passage, or sustain a vowel sound—look for early breath termination.
s/z ratio and maximum phonation time can be used for baseline assessment.
Clinical Insight: Use of Accessory Respiratory Muscles
Overuse of accessory muscles (e.g., sternocleidomastoid, scalenes, abdominal muscles) suggests that quiet inspiration and expiration are insufficient.
This often indicates:
Increased work of breathing
Fatigue during speech
Compensatory strategies due to reduced respiratory efficiency
Underlying neuromuscular weakness or rigidity (common in Parkinson's)
👀 What to Look For
Muscle Group | Signs of Use | What It Might Indicate |
Neck muscles(sternocleidomastoid, scalenes) | Elevated shoulders, neck strain, visible contraction during inhalation | Reliance on accessory inspiration |
Abdominal muscles | Forceful abdominal movement during exhalation, visible tensing | Compensation for weak expiratory drive |
Upper chest | Shallow, clavicular breathing pattern | Reduced diaphragmatic activity |
🩺 Clinical Relevance in Parkinson's Disease
Bradykinesia and rigidity can impair diaphragm movement.
Patients may recruit accessory muscles more readily.
Result: fatigued, breathy, and poorly projected speech.
✅ Assessment Tip
Ask the client to:
Take a deep breath — observe where movement occurs (chest vs abdomen).
Sustain a vowel — time it and listen for volume drop or vocal fatigue.
Read a short passage — note phrasing and breath breaks
Respiratory Pathology and Speech: Key Considerations
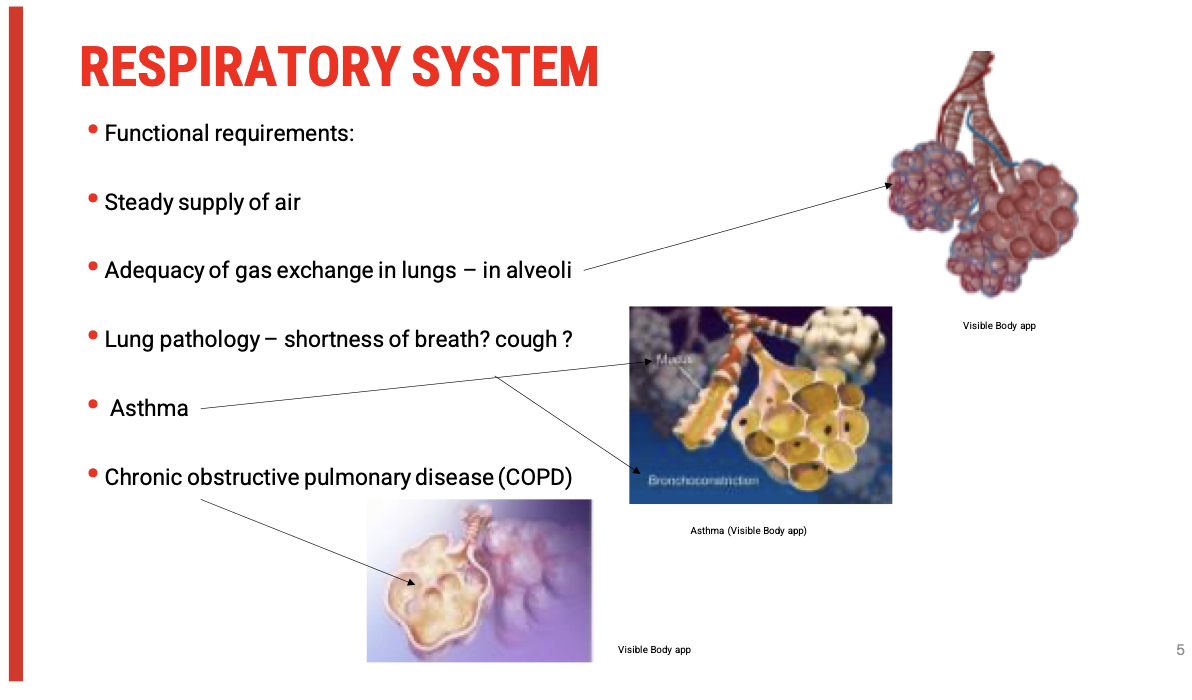
🔄 Gas Exchange & Speech Production
Speech requires a consistent and controlled outflow of air. If gas exchange is compromised (as in asthma or COPD), the client may:
Fatigue easily
Speak in short phrases
Exhibit reduced vocal intensity
Pause frequently for breath
🩺 Common Respiratory Conditions & Speech Implications
Condition | Key Pathophysiology | Effect on Speech |
Asthma | Bronchoconstriction + mucus production | Shortness of breath, cough, difficulty sustaining phonation |
Chronic Bronchitis (COPD) | Chronic inflammation and mucus overproduction | Wet voice, frequent throat clearing, poor voice quality |
Emphysema (COPD) | Alveolar destruction, air trapping, poor oxygen exchange | Reduced breath support, weak voice, effortful speech |
❗ Clinical Red Flags to Observe
Shortness of breath at rest or during speech
Coughing during speech or phonation
Audible wheezing or rattling
Rapid respiratory rate
Difficulty sustaining vowels or phrases
🧠 Integrating This in Clinical Reasoning
Ask yourself:
Is reduced speech intelligibility due to linguistic/motor impairments?
Or is it due to reduced respiratory support from an underlying pulmonary condition?
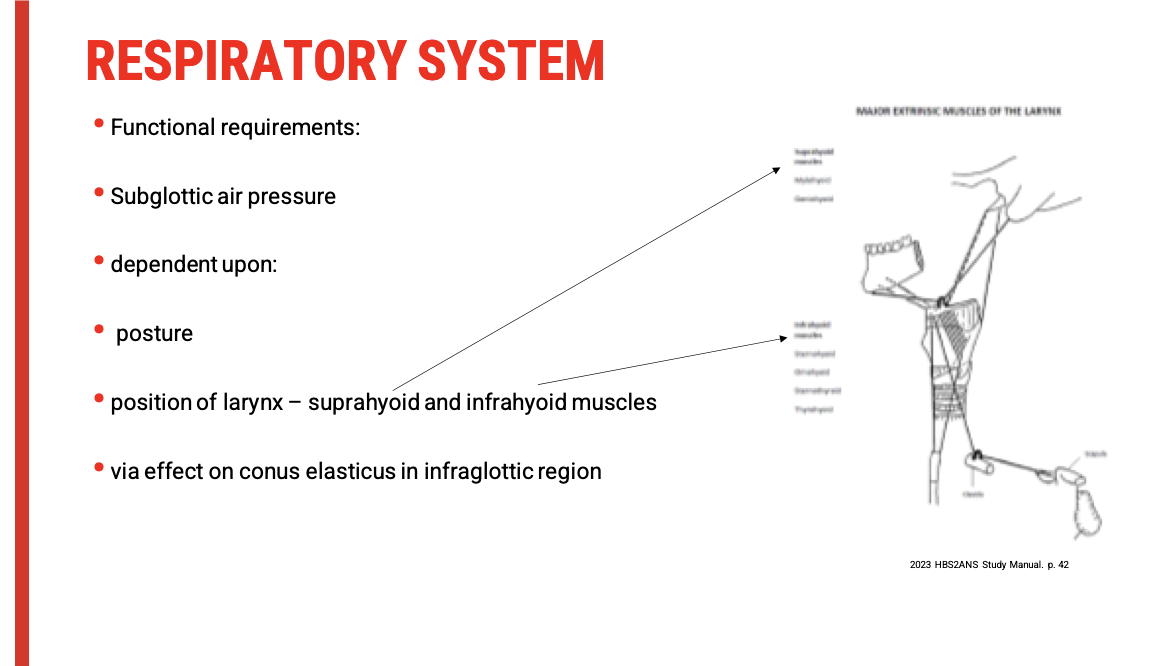
Subglottic Pressure & Posture: Key Clinical Concepts
Subglottic Pressure: What It Does
Required to initiate and maintain vocal fold vibration
Needs to overcome laryngeal resistance to set vocal folds in motion
Affects voice intensity, pitch, and sustained phonation
🧍♀ Postural Influence on Phonation
Postural Element | Impact on Subglottic Pressure |
Spinal alignment | Poor alignment (e.g. kyphosis, slumping) restricts diaphragm efficiency and thoracic expansion |
Neck tension | Increases tone in suprahyoid/infrahyoid muscles, altering laryngeal height and stability |
Jaw and tongue posture | Can pull on the hyoid bone, indirectly affecting the larynx’s vertical position |
🧠 Neuromuscular Considerations
Suprahyoid muscles (e.g. mylohyoid, geniohyoid): Elevate larynx
Infrahyoid muscles (e.g. sternohyoid, omohyoid): Depress larynx
Laryngeal height affects tension in the conus elasticus (supporting the vocal ligaments from below) → influences subglottic pressure and efficiency of vibration
🔍 Clinical Application: What to Observe
Is the client slouching or upright?
Is there visible neck tension (e.g. clavicle/SCM activation at rest)?
Is the larynx visibly elevated or depressed?
Is speech effortful or accompanied by visible strain?