1. Male Reproductive System Disorders
1/168
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
169 Terms
Testes
Ducts
Semen
Penis
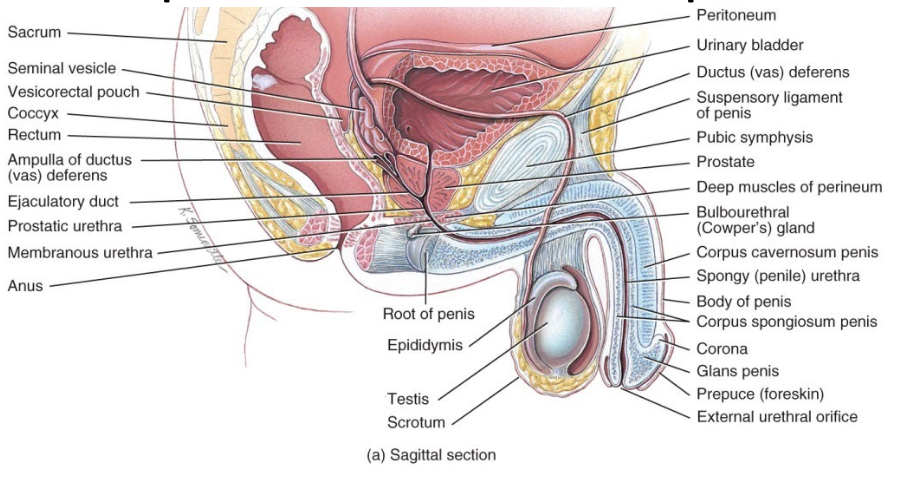
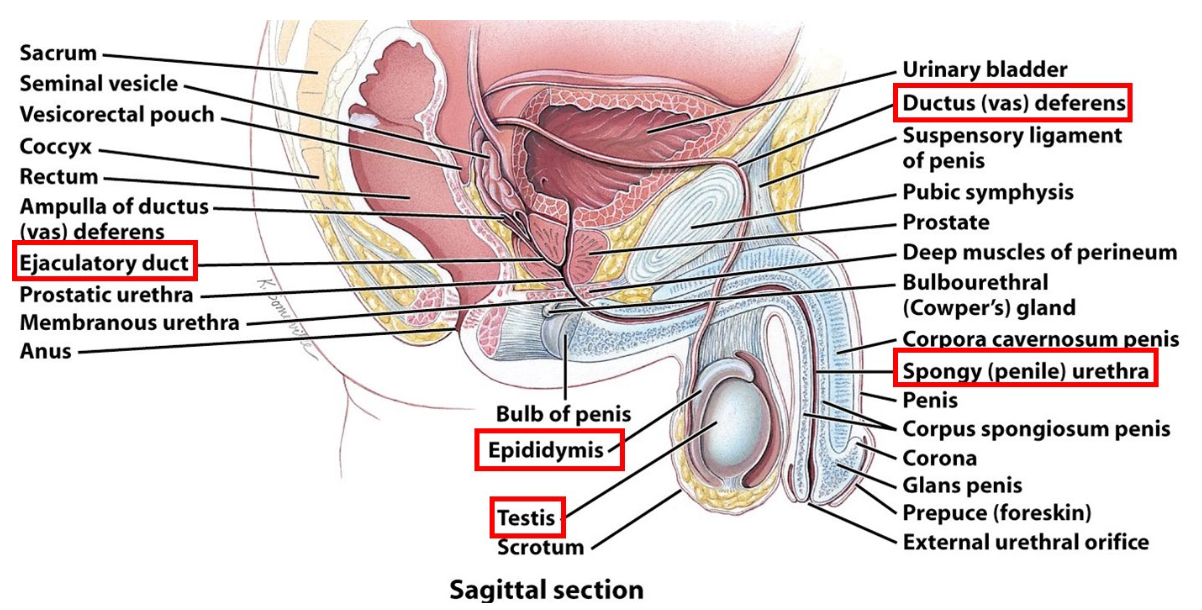
Male Reproductive System:
____ make sperm and secrete hormones
_______ transport and store sperm, assist in their maturation, and convey them to the exterior
______ contains sperm plus secretions of sex glands
_____ delivers sperm to the female reproductive tract
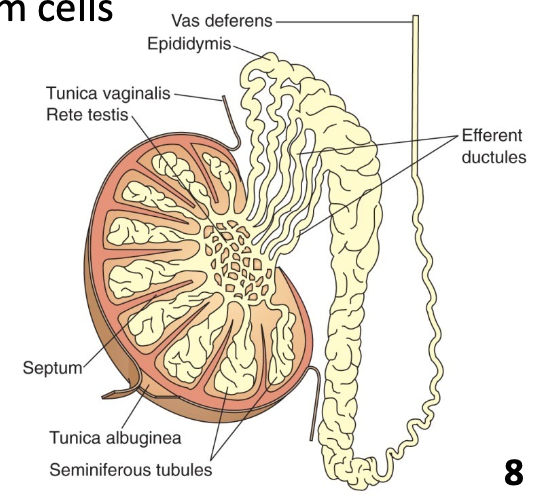
Testes (Testicles)
Paired oval glands in scrotum
Develop on posterior abdominal wall and descend into scrotum through inguinal canals
Each lobule is filled with 2 or 3 seminiferous tubules where sperm are formed (spermatogenesis)
Meiosis occurs to produce haploid sperm cells
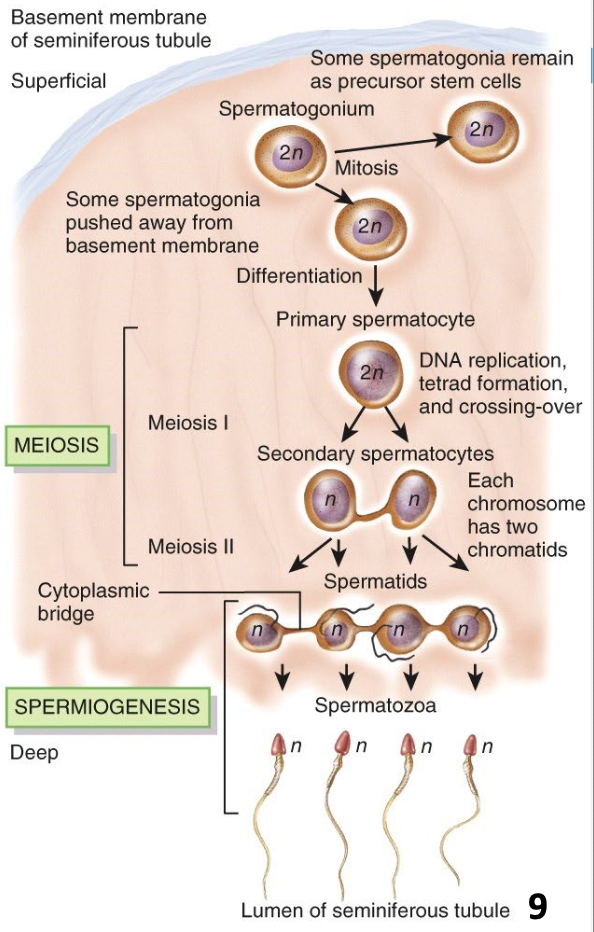
Spermatogenesis
Spermatogonia (2n) → primary spermatocytes (2n) → secondary spermatocytes (n) → spermatids (n) → mature sperm
One primary spermatocyte gives rise to 4 spermatozoa (n)
Pathway of Sperm Flowing through Ducts
Seminiferous tubules → ductus epididymis → ductus (vas) deferens → ejaculatory ducts → urethra
Semen
A mixture of sperm and seminal fluid
Secretions from seminiferous tubules (sperm), seminal vesicles, prostate, and bulbourethral glands (stay tuned…)
Volume ~2.5 – 5 mL
50 – 150 million sperm / mL
If < 20 million sperm / mL, likely infertile
Slightly alkaline pH (7.2 – 7.7) → counters vaginal acidity
Coagulates after ~ 5 min and re-liquefies after ~10 – 20 min to allow for sperm motility through cervix of uterus
ANSWER: B
What’s the point of clotting, why does semen coagulate?
we evolved for purpose of reproduction, evolutionary perspective
if it does not clot after ejac, the pt get up, get out, no deliver
A failure of semen coagulation, which could be caused by abnormal/low/absent clotting factors, would most impact:
a. Sperm viability
b. Sperm delivery
c. Sperm motility
d. Sperm morphology
ANSWER: C
if stay coag = no helpful, b/c sperm big journey ahead of them to find oocyte
A failure of semen reliquification, caused by defective/low/absent proteolytic enzymes, would impact:
a. Sperm viability
b. Sperm delivery
c. Sperm motility
d. Sperm morphology
e. Sperm ATP production
Seminal vesicles
Prostate
Bulbourethral glands
Acessory Sex Glands:
______________
Secrete alkaline fluid with fructose, clotting proteins
______
Secretes slightly acidic fluid with citric acid, proteolytic enzymes
Bulbourethral glands
Secrete alkaline fluid and mucus
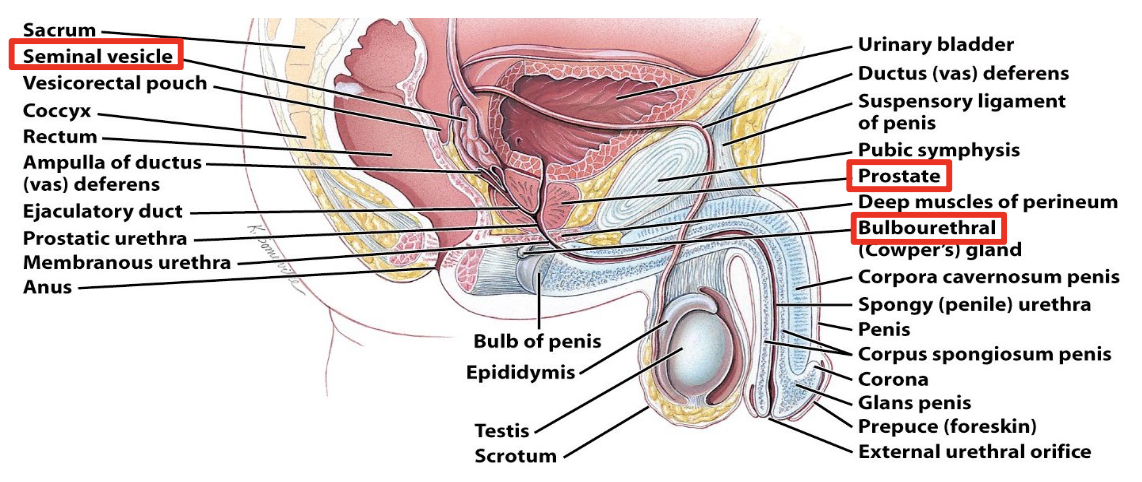
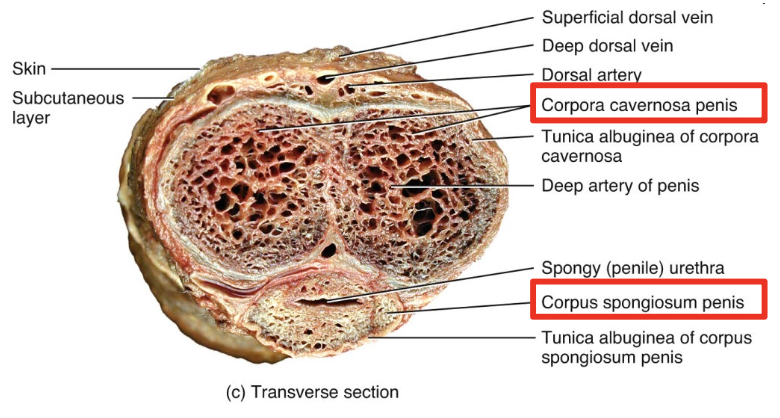
Penis
Contains three masses of erectile tissue
Spongy structures composed of blood sinuses lined by endothelial cells and surrounded by smooth muscle and elastic CT → fill with blood during erection
Two corpus cavernosa: dorsolateral, for maintaining erection
Corpus spongiosum: contains spongy urethra and keeps it open during ejaculation
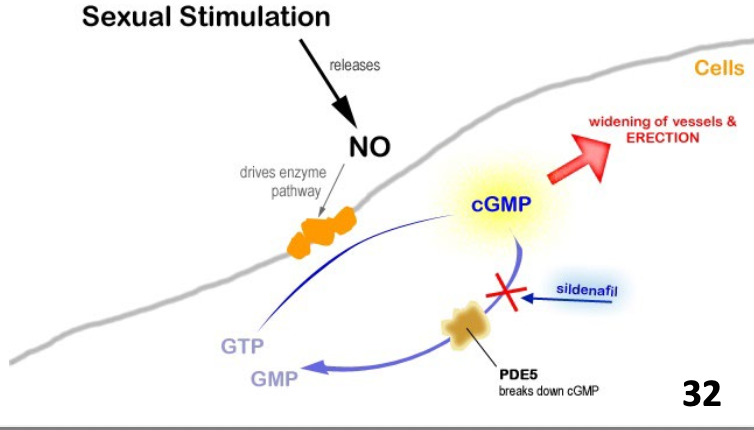
Erection
Parasympathetic reflex causes erection
Sexual stimulation → dilation of arteries supplying penis (nitric oxide mediates local vasodilation)
Expansion of blood sinuses compresses the veins, trapping blood in penis to maintain erection
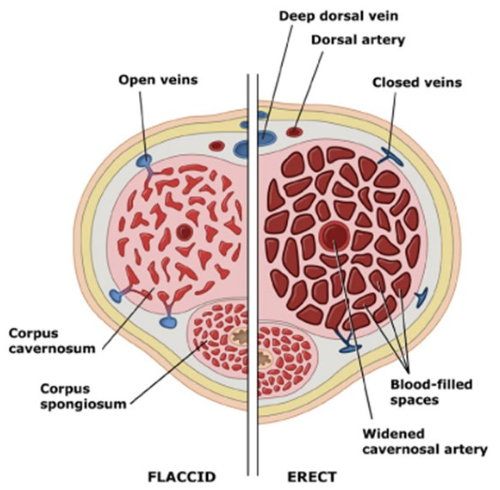
Ejaculation
Ejaculation is a sympathetic reflex
Peristalsis in epididymis, ductus deferens, seminal vesicles, ejaculatory ducts, and prostate propel semen into spongy urethra
Urination is prevented during ejaculation
After ejaculation, arterioles supplying erectile tissue constrict and smooth muscles within erectile tissue contract, making blood sinuses smaller and relieving pressure from veins → blood allowed to drain
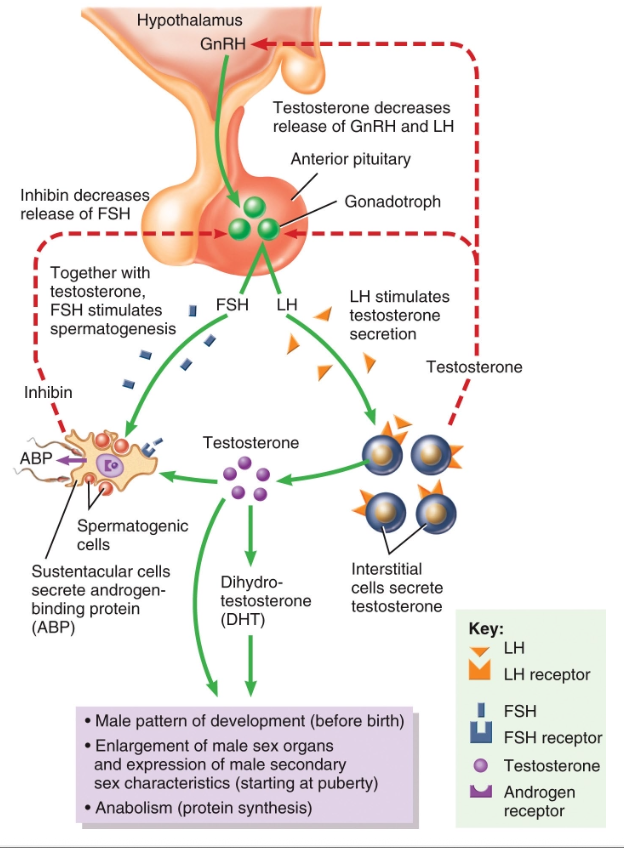
Testosterone
Male Sex Hormones:
_________ is the primary androgen
Produced by interstitial cells in testes
Can be converted to other androgens in periphery (skin/liver) e.g. dihydrotestosterone (DHT)
5x more potent than ________
embryogenesis
male sexual
Anabolic
Functions of Testosterone:
Important in _________
Development and maintenance of _________ characteristics
______ effects e.g. protein synthesis, musculoskeletal growth
Spermatogenesis
Sex drive
Hypospadias and Epispadias
Urethritis and Urethral Strictures
Phimosis and Paraphimosis
Balanitis
Peyronie Disease
Priapism
Male Sexual Dysfunction
Carcinoma of the Penis
Disorders of the Penis and Urethra
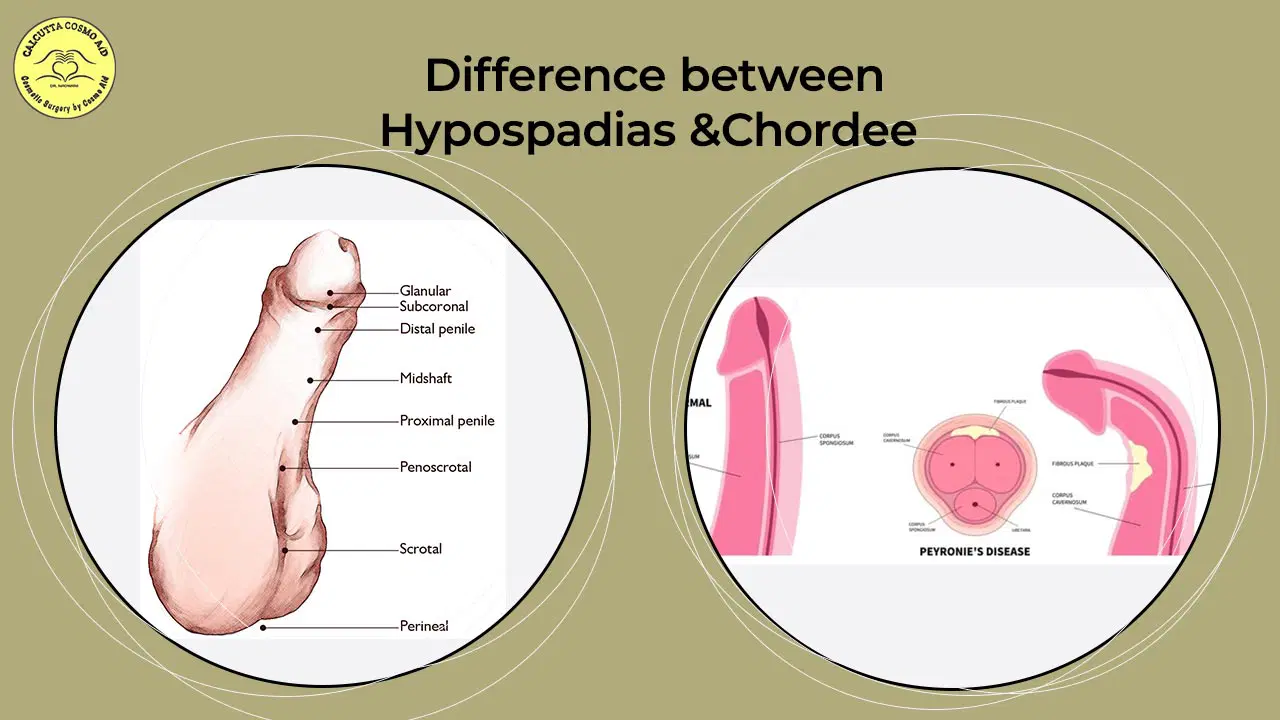
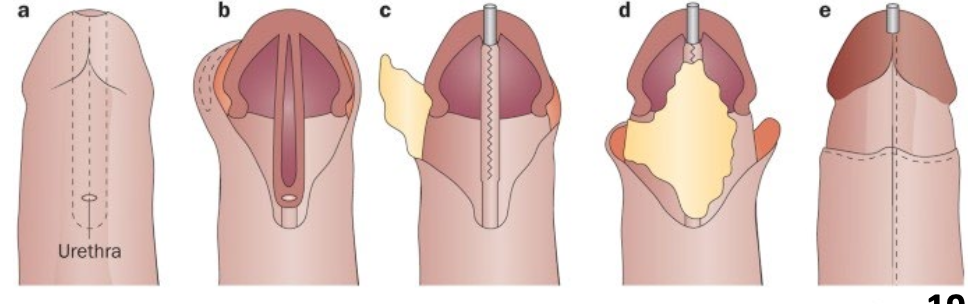
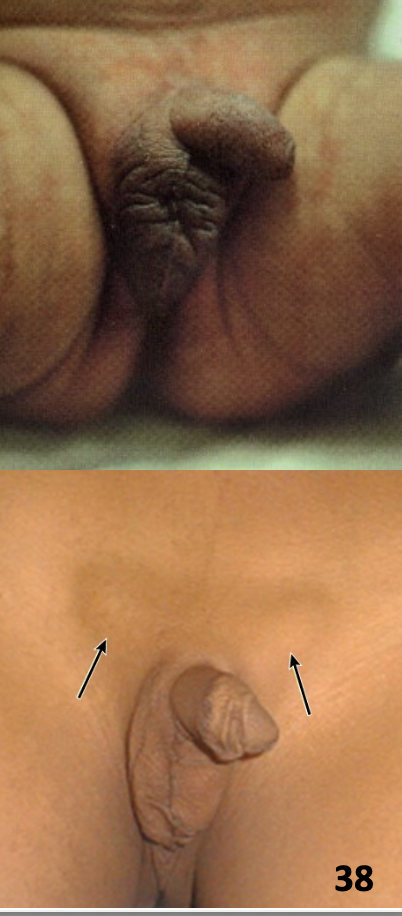
Hypospadias
Congenital abnormality in which the urinary meatus is located on the ventral surface of the penis
Incidence: 1/300 male infants
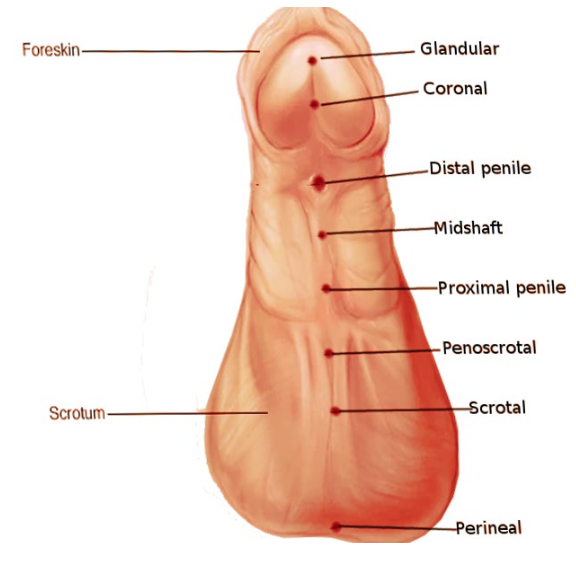
Disruption of androgen stimulation during development (genetics or prenatal exposure to toxins, estrogenic compounds)
Results in embryological defects in development of the urethral groove and penile urethra
Often associated with:
Chordee (ventral bowing of penis)
Cryptorchidism (undescended testes)
Partial absence of foreskin
Hypospadias Etiology and pathogenesis:
standing
Hypospadias signs and symptoms:
Inability to urinate in ______ position
Ejaculatory dysfunction
Inability to penetrate during coitus
Possible urinary tract obstruction
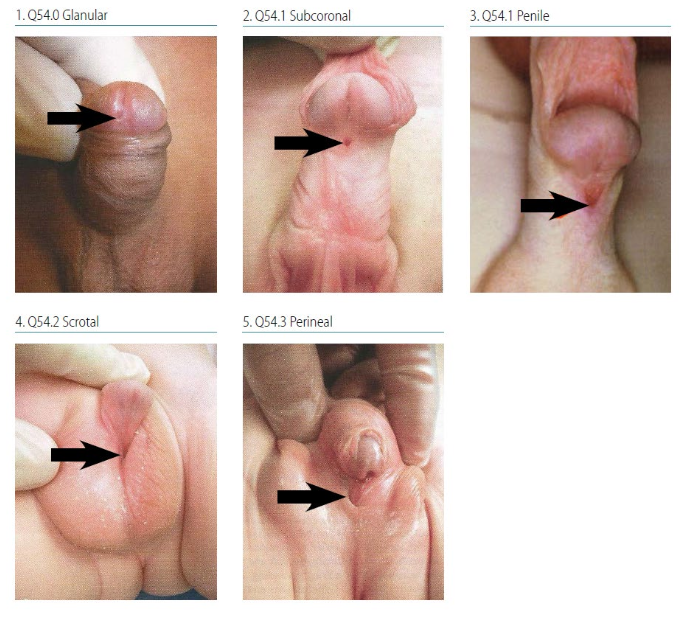
Surgical
Treatment of Hypospadias:
_______ repair
Improved micturition and sexual function
Epispadias
Congenital abnormality in which the urinary meatus is located on the dorsal surface of the penis
Incidence: 1 in 20,000 live births
Embryological defect in abdominal wall development → herniation of lower abdominal organs e.g. bladder exstrophy
Epispadias is a mild form where urethra fails to close normally
Epispadias Etiology and pathogenesis
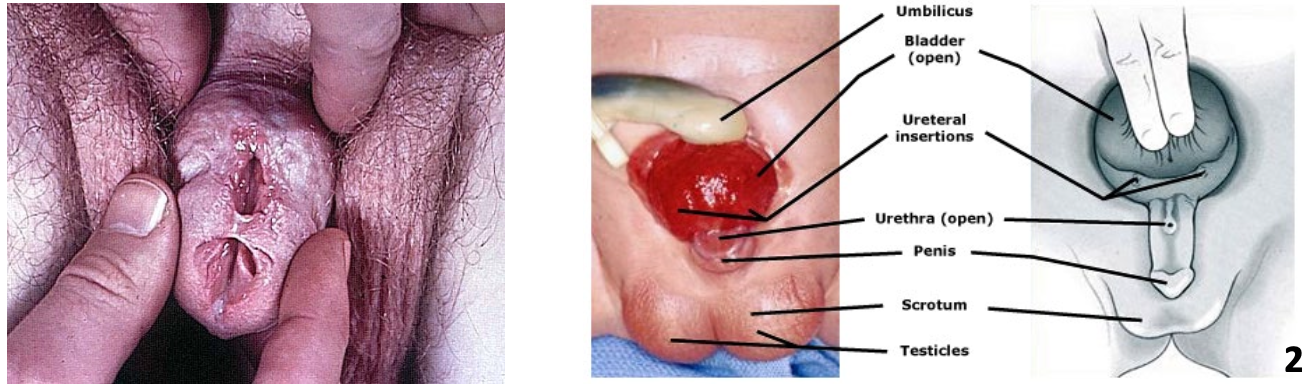
Varying degrees of severity
Open bladder and exposed urethra
Penis and prostate defects are common
May involve anal atresia, hypoplasia of the colon and small intestine, and abnormalities in the vertebral column and pelvic bone
Signs and symptoms of Epispadias
Surgical management to preserve urinary continence and cosmetic appearance of genitalia
Treatment of Epispadias
Urethra
Common structure of both the urinary and reproductive systems in males
Urethritis
inflammation of the urethra
Infectious causes e.g. gonorrhea, chlamydia → STIs
Other causes e.g. urologic procedures, anatomical abnormalities, trauma (Catheterization)
Dysuria, pruritis, purulent discharge
Urethral stricture
scarring and fibrotic narrowing
Commonly due to infections or iatrogenic trauma
Urethral discharge, urinary retention, hydronephrosis
Phimosis and Paraphimosis
The foreskin (prepuce) is a retractable double-layered fold of skin and mucous membrane that covers the glans penis and protects the urinary meatus
Phimosis
Inability to retract foreskin from the glans of the penis (distal to proximal)
Tight foreskin that cannot be retracted to expose glans
Normal in young children; 99% of cases resolved by age 16
Poor hygiene
Etiology and pathogenesis of Phimosis:
___________ leading to chronic inflammation and infection →scarring and narrowing of prepuce
Irritation and bleeding
Purulent discharge
Painful erection
Dysuria, chronic urinary retention
Signs and symptoms of Phimosis
Stretching exercises of the prepuce
Topical corticosteroids, antibiotics
Circumcision
Treatment of Phimosis
Paraphimosis
Inability of foreskin that has been retracted to be replaced in its normal position (proximal to distal)
Foreskin is trapped behind corona of the glans penis
Incidence ~1% in adult males
Phimosis, chronic inflammation
Iatrogenic e.g. foreskin retracted for cleaning, catheter placement
Trauma e.g. body piercings = swelling
Etiology and pathogenesis of Paraphimosis
Penis swelling and pain
Dysuria and urinary obstruction
Ischemia and necrosis → tight foreskin → contricts glans penis = no blood flow
signs and symptoms of Paraphimosis
Pain control e.g. topical anesthetics
Manual reduction
Dorsal slit incision
circumcision
Treatment of Paraphimosis
Balanitis
Inflammation of the glans penis
Incidence ~3% of men globally
hand in hand w/ phimosis/paraphimosis

Inadequate hygiene, infections, chemical irritants
Buildup of sweat, debris, and exfoliated skin (smegma) between foreskin and glans → inflammation
Etiology and pathogenesis of Balanitis
Redness, pain, and swelling
Thick white discharge under foreskin
Phimosis
Painful urination
Signs and symptoms of Balanitis
Genital hygiene
Topical antifungals, antibiotics or steroids
Circumcision
Treatment of Balanitis
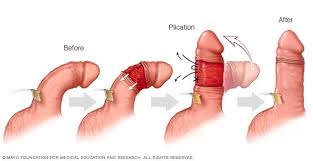
Peyronie disease
Localized fibrotic disorder of the tunica albuginea
Incidence ~5% in adult men

Genetics, trauma, and tissue ischemia
Localized abnormal wound healing → upregulation of cytokines and growth factors → fibrous plaque that alters penile anatomy
etiology and pathogenesis of Peyronie disease
Penile pain and deformity (often causes curve)
Palpable plaque or nodule
Erectile pain and dysfunction
signs and symptoms of Peyronie disease
Oral phosphodiesterase inhibitors → coping strategy using viagra to vasodilate penis
Intralesional collagenase injection → enzymes break down the collagen
Surgery – plication, grafting
treatment of Peyronie disease
Priapism
Persistent painful erection of the penis in the absence of sexual desire or stimulation
May last from hours to days
Incidence ~1:100,000 men; can occur in any age group
Most are idiopathic
Underlying disease
Hematologic – e.g. sickle cell disease
Metabolic – e.g. diabetes
Drugs
E.g. antipsychotics, impotence treatments
Spinal cord trauma
etiology of Priapism
Obstruction of venous drainage → ischemia and structural damage to erectile tissue
pathogenesis of Priapism
Painful and rigid erection
May present with penile gangrene
signs and symptoms of Priapism
Oral analgesics
Decompression by aspirating blood
Intracavernosal injections of sympathomimetics
Surgery e.g. shunt procedures
treatment of Priapism
Duration of priapism strongly associated with subsequent erectile dysfunction
90% of men with ischemic priapism lasting >24 hours lose ability to have sexual intercourse
prognosis of Priapism
Male Sexual Dysfunction
Any disorder that interrupts cycle from arousal to orgasmto resolution
E.g. decreased libido, erectile dysfunction, ejaculatory disorders
May be due to psychological, emotional, or physiological factors
Survey data indicate ~30% of men aged 18 – 59 suffer from sexual dysfunction; incidence increases with age
Neural
Vascular
Hormonal
Psychological
Components of normal sexual function:
_______ – perceive sensory input; autonomic output
______ – sufficient blood flow and nitric oxide (NO) activity
_______ – testosterone enhances libido and NO synthesis
___________ and social factors
Erectile Dysfunction
Consistent inability to acquire or sustain an erection of sufficient rigidity and duration for sexual intercourse
Estimated prevalence 16% in men 20 – 75 years old
Age
Obesity
Smoking
Local penile factors e.g. Peyronie disease
Trauma e.g. pelvic fracture, iatrogenic procedures
Endocrine disorders e.g. hypogonadism
Chronic medical problems e.g. diabetes, hypertension, CKD, MS, PD
Drugs e.g. antidepressants, antihypertensives, alcohol
Psychogenic e.g. trauma, anxiety, stress
Etiology and pathogenesis of Erectile Dysfunction
Address underlying etiology
Lifestyle modifications e.g. smoking cessation, exercise
Testosterone therapy
Phosphodiesterase-5 inhibitors e.g. sildenafil (Viagra)
Vacuum devices
Surgery e.g. revascularization, prosthetics
treatment of Erectile Dysfunction
Premature Ejaculation
Rapid ejaculation that occurs with brief latency, inability to delay ejaculation, and causes negative personal consequences
Estimated prevalence up to 30% of all males
Unclear; biological and psychosocial factors involved
Low serotonin in the brain, hormonal abnormalities
Depression, anxiety, unrealistic expectations about sexual performance, poor body image
etiology and pathogenesis of Premature Ejaculation
SSRIs
Topical anesthetics, condoms
Psychotherapy
treatment of Premature Ejaculation
Carcinoma of the Penis
Squamous cell carcinomas account for 95% of penile carcinomas
Rare (<1% of cancers in men) in developed countries, but accounts for ~10 – 20% of cancers in Africa, Asia, and South America

Age
Medical conditions of the penis e.g. UTIs, phimosis
Infections e.g. HPV, HIV
Smoking
etiology of Carcinoma of the Penis
Skin abnormality or palpable lesion on penis
Majority present on the glans or prepuce
Rash
Bleeding
Balanitis
signs and symptoms of Carcinoma of the Penis
Topical chemotherapy
Radiation
Partial or total penectomy
Removal of lymph nodes
treatment of Carcinoma of the Penis
If localized to penis, 5-year survival ~85%
If metastasized beyond inguinal lymph nodes, 5-year survival is less than 10%
prognosis of Carcinoma of the Penis
Disorders of the Scrotum and Testes
Cryptorchidism
Varicocele, hydrocele, and spermatocele
Testicular torsion
Epididymitis and orchitis
Testicular cancers
Male infertility
Cryptorchidism
“Hidden testes” – a testis that is not within the scrotum, or does not descend spontaneously by 4 months of age
Testis may be undescended, absent, or ectopic
Can be unilateral or bilateral
Incidence ~1% in male infants at 1 year of age
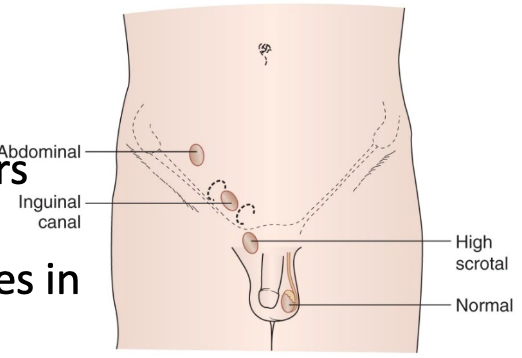
Premature birth or low birth weight
Prenatal exposure to endocrine disruptors e.g. pesticides
Genetic disorders leading to abnormalities in development or endocrine function
Interaction between mechanical, hormonal, and neurotransmitter effects required for normal testes descent
etiology and pathogensis of Cryptorchidism
Empty or hypoplastic scrotum
Undescended testes may be palpable
signs and symptoms of Cryptorchidism
Testicular torsion
Testicular trauma
Infertility
Malignant transformation
complications of Cryptorchidism
Palpation
Imaging – ultrasound, CT scan
diagnosis of Cryptorchidism
Human chorionic gonadotropin (hCG) injections
Orchidopexy
Surgical operation in which undescended testis is mobilized and fixed within scrotum
Generally performed before 2 years of age
Orchiectomy
Performed if cryptorchidism is identified after puberty
treatment of Cryptorchidism
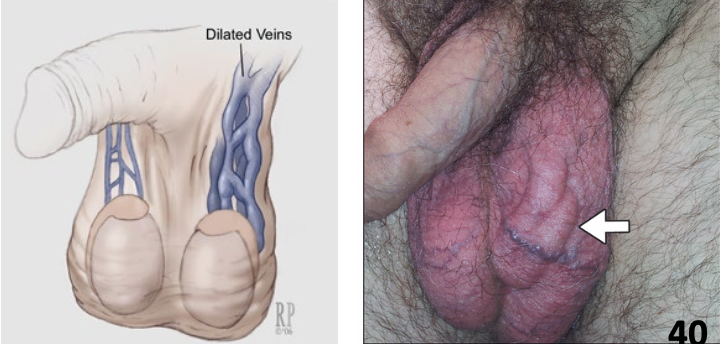
Varicocele
Varicosities in pampiniform plexus that supplies the testes
Found in ~20% of post-pubertal males, mostly on left side
Incompetent or absent valves in testicular veins
etiology and pathogensis of Varicocele
‘Bag of worms’ upon palpation
May be asymptomatic or associated with pain and scrotal fullness
Testicular atrophy and decreased fertility
clinical features of Varicocele
Surgical ligation
Venous embolization
treatment of Varicocele
Hydrocele
Collection of peritoneal fluid between layers of the tunica vaginalis
More common in men >40 years of age
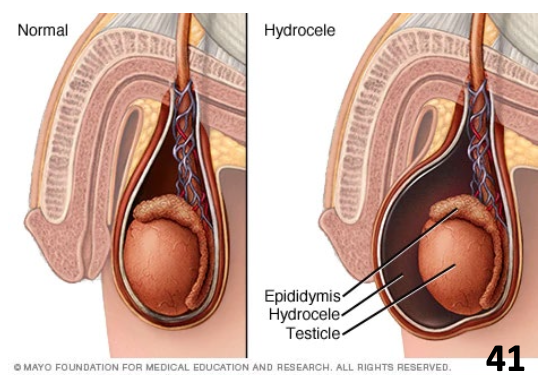
Imbalance of fluid secretion and reabsorption
Idiopathic or secondary to inflammatory conditions (e.g. STIs, epididymitis, orchitis)
etiology of Hydrocele
Can be small and soft, or large and firm
Pain proportional to size of cystic mass
Transilluminates well
clinical features of Hydrocele
Surgical excision of hydrocele sac
treatment of Hydrocele
Spermatocele
Painless, sperm-containing cyst that forms at the end of the epididymis
May be difficult to distinguish from hydrocele, but aspirated fluid from spermatocele contains spermatozoa
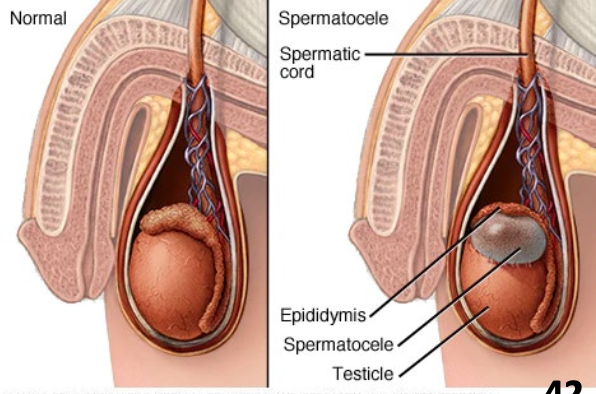
Idiopathic or secondary to infections, trauma
etiology and pathogenesis of Spermatocele
Generally asymptomatic
May cause chronic pain
clinical features of Spermatocele
Surgical excision
treatment of Spermatocele
Testicular Torsion
Urologic emergency where testis twists on spermatic cord
More common in neonates than adults
Accounts for 25 – 50% of hospitalizations for acute scrotal pain
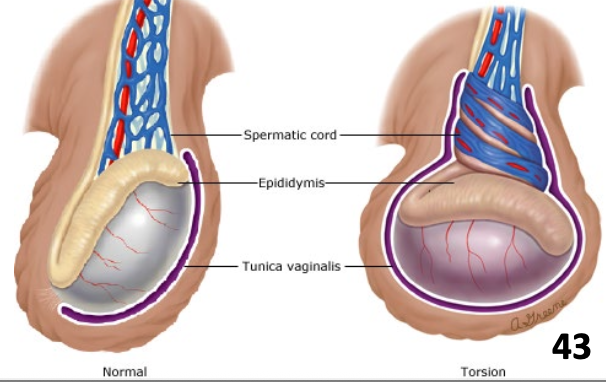
May be spontaneous or triggered (e.g. trauma)
Lower pole of testis is inadequately fixed to tunica vaginalis → testis twists → ischemia and infarction
Irreversible testis damage after several hours
etiology and pathogenesis of Testicular Torsion
Acute onset of moderate to severe testicular pain
Nausea, vomiting, and diffuse lower abdominal pain
Asymmetric high-riding testis
Swelling and redness of scrotal wall
Palpable ‘knot’ superior to the testis
signs and symptoms of Testicular Torsion
Manual detorsion
Surgery for detorsion and fixation of testis
treatment of Testicular Torsion
Epididymitis
Inflammation of the epididymis
Most common cause of acute scrotal pain in adults
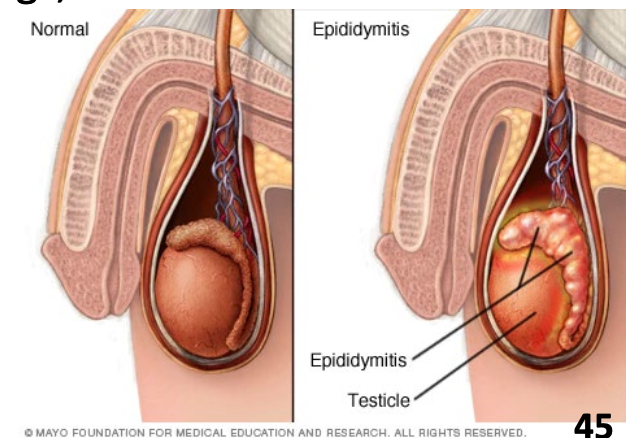
Males ages 20 – 40: STIs e.g. gonorrhea, chlamydia
Elderly males: UTIs, retrograde urine flow e.g. E. coli
Other causes: sports trauma, drugs, viruses
etiology and pathogenesis of Epididymitiss
Intra-scrotal pain and swelling
Possible fever, UTI symptoms
signs and symptoms of Epididymitis
Antibiotics
Bed rest and scrotal elevation
treatment of Epididymitis
Orchitis
Inflammation of the testes
Usually occurs in conjunction with epididymitis
Most cases of isolated orchitis are due to mumps infections

Viral: mumps, rubella
Bacterial: E. coli, Klebsiella, Pseudomonas, Staphylococcus, Streptococcus
etiology and pathogenesis of Orchitis
Acute onset of testicular pain and swelling
Fever, malaise, chills
Testicular atrophy → sterility
signs and symptoms of Orchitis
Antibiotics for bacterial causes
Analgesics and antipyretics
Scrotal support
treatment of Orchitis
Testicular Cancers
Account for 1% of all male malignancies, but are the most common cancers affecting males between ages 15 – 35
Majority (>90%) of testicular cancers are malignant
Good prognosis – 5-year survival rate >95%
Germ cell tumours (90%)
Derived from cells that give rise to spermatogonia
Broadly classified as seminomas and non-seminomas
Sex cord-stromal tumours (5%)
Derived from ‘support’ cells in the testes
Include Leydig (interstitial) cell tumours and Sertoli (sustentacular) cell tumours
Genetic associations
Cryptorchidism
Prenatal exposure to estrogens
Risk factors for Testicular Cancers
Testicular enlargement that may become painful
Heavy sensation in lower abdomen, perianal area, or scrotum
Metastasis
Lungs – cough, dyspnea, hemoptysis
CNS – visual defects, dizziness, seizures
Gynecomastia if tumour produces hCG or estrogens
signs and symptoms of Testicular Cancers
Testicular examination
Scrotal ultrasound
Serum tumor markers (e.g. hCG, alpha fetoprotein, lactate dehydrogenase)
Radical inguinal orchiectomy
Retroperitoneal lymph node dissection
diagnosis of Testicular Cancers
Orchiectomy and node dissection
Some males require hormone replacement therapy, sperm banking
Chemotherapy or radiation
treatment of Testicular Cancers
Seminomas
Account for ~45% of testicular cancers
Malignant tumour derived from seminiferous epithelium that retains characteristics of primary spermatogonia
Neoplasm generally consists of a single cell type
Slow growth and lymphatic spread
Mostly limited to testicle or retroperitoneal nodes
Good prognosis due to radio-sensitivity
