Interp 2 Lumbar Spine (EXAM 1)
1/124
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
125 Terms
what makes intervertebral osteochondrosis?
decreased height and vacuum cleft
what are the causes of neuropathic arthropathy?
syringomyelia, tabes dorsalis, and diabetes mellitus
what is the most common neuropathic arthorpathy?
diabetes mellitus
what is the radiographic vertebrae finding of neuropathic arthropathy?
jigsaw vertebrae, tumble block spine
what are the 6 D’s of hypertrophic pattern of neuropathic arthropathy?
distention, dislocation, disorganization, destruction, debris, density increased
what is ankylosing spondylitis?
chronic inflammatory condition primarily affecting axial skeleton in males
what are the features of articular ankylosis?
articular ankylosis, ligament ossification, enthesopathy
what will 50% of patients with AS develop?
large peripheral joint development
what will 30% of patients with AS develop?
small peripheral joint involvement
what is the most sites of peripheral joint involvement with AS?
hip and shoulder
what are the radiograph findings of AS?
bilateral and symmetrical
osteoporosis
60% of AS cases start where?
the thoracolumbar spine
where does the 40% of AS cases not starting in the throacolumbar spine start?
SIJ
what is the hallmark of AS sacroiliac joint disease?
bilateral symmetric involvement
where are the changes from AS in the SIJ more severe?
iliac side due to less cartilage
what is stage one of AS in SIJ?
pseudo widening
what causes pseudo widening in AS SIJ?
resorption of the subchondral bone
what is two of AS in the SIJ?
erosion and sclerosis
what sign or appearance is a result of erosions of the SIJ?
rosary bead sign
what percent of AS SIJ cases go to stage two and resolve?
40%
what is stage 3 of AS in the SIJ?
ankylosis
what happens during ankylosis of the SIJ?
there is a hint of the SIJ after, “ghost joint”
what percent cases of AS develop complete ankylosis?
50%
what is the sign of upper SIJ ankylosis?
star sign
what happens to the corner of the vertebral bod when AS is in the spine?
erosion of the corner of vertebral body
what is erosion of the corner of vertebral body called?
romanus lesion
what are the findings of AS in the spine?
romanus lesion
squaring of vertebrae anteriorly
shiny corner sine
ossification of outer annular fibers
what is the spine finding of AS?
bamboo spine due to marginal syndesmophytes
what other seronegative spondyloarthropathies cause SIJ involvement?
psoriatic, enteropathic arthritis, AS, reactive arthritis
what is osteitis condensans ilii?
isolated sacroiliac arthopathy
what is true of orthopedic test with osteitis condensans ilii?
positive SIJ test with pain, adjust will hurt than quickly resolve
what are the radiographic findings of osteitis condensans ilii?
triangular sclerosis of the ilium
unilateral or bilateral
usually no abnormality of joint itself
sclerosis can regress
what is true of trauma to the spine?
Injury to the thoracolumbar or lumbar region is more likely then mid to upper thoracic spine due to mobility
what translation in the sagittal plane classifies instability of the L/S?
4.5 mm
what degree of sagittal rotation classifies as instability at L1-L4?
more than 15 degrees
what degree of sagittal rotation classifies as instability at L4/L5?
more than 20 degrees
what degree of sagittal rotation classifies as instability at L5/S1?
more than 25 degreees
on neutral radiographs what classifies as instability?
Sagittal translation greater than 4.5mm or 15% of the endplate width
Sagittal rotation (disc angles) greater than 22 degrees compared to surrounding levels
is a spondylolysis always associated with a spondylollisthesis?
no
where do 90% of spondylolysis occur?
L5
what is the common age for spondylolysis occur?
10-15
what is the most common etiology of spondylolysis?
stress fracture
what athletes are at higher risk for spondylolysis?
divers, gymnast, weightlifters and pole vaulter
what is a transverse process fracture secondary to?
avulsion force or direct trauma
what are the most common levels for a transverse process fracture?
L2 and L3
transverse fractures are usually oriented in which direction?
vertical
what needs to be ruled out in regards to a transverse process fracture?
urinary tract damage
what are the 3 types of seatbelt fractures?
chance fracture, Smith’s fracture and horizontal fracture
what is a chance fracture?
horizontal fracture through the spinous process, laminae, pedicles, transverse processes and posterior vertebral body extending into the end plate
what is the radiographic sign of a chance fracture on an x-ray?
empty vertebrae sign
what is the MOI of a chance fracture?
hyperflexion/distraction injury
what area of the lumbar spine is most commonly affected by a chance fracture?
upper lumbar
what else seeds to be evaluated with a chance fracture?
associated visceral damage
what is a Smith’s fracture?
similar to chance, but interspinous ligament is torn instead of SP fracture
what is a horizontal fracture?
fracture all the way through the body without endplate involvement
what are other tpes of fractures or dislocations in the lumbar spine?
vertebral body compression fracture
burst fracture
fracture-dislocation
apophyseal ring fracture
abused child syndrome
what is a limbus vertebra?
triangle shaped corner of vertebral body not attached to main vertebral body
what do limbus vertebra semonstrate?
smooth corticated margine
what are limbus vertebra mistaken for?
teardrop fracture and intercalary bone
what is true of lumbar suppurative infection?
there is about a 21 day latent period before radiographic changes are visible
what does suppurative lumbar infection cause?
rapid destruction of vertebral margin and rapid destruction of the disc with spread to the other endplate
what is the most common cause of lumbar spine non-suppurative infection?
tuberculosis
what is true of lumbar spine non-suppurative infection?
slower process than suppurative and hence can destroy more of vertebral body by the time it is caught
how does lumbar spin non-suppurative infection spread?
sub-ligamentous causing skip lesions and anterior vertebral body scalloping
what may lumbar spine non-suppurative infection demonstrate?
psoas calcification
what can cause unilateral sacroilitis?
suppurative infection of the SIJ
what may be the result of a SIJ suppurative infection?
joint ankylosis
what is the most common benign tumor of the spine?
hemangioma
what are the radiographic signs of hemangioma?
lucent vertebrae with accentuated vertical trabeculae, corduroy cloth appearance
rarely expansil
likes vertebral body
what is the ddx for a hemangioma?
pagets or osteoporosis
what is a chordoma?
malignant neoplasm that develops from a remnant of the notocord
where is the most common location for a chorodma?
sacrocoygeal area, clivus and the spine (C2)
what age range do cordomas occur?
40-70
what are the radiographic findings of a chordoma?
midline lesions
osteolytic lesion with soft tissue mass
calcification may be present
what age is paget’s disease common in?
55 or older
how many stages does Paget’s disease have?
4
what is true of the pain with Paget’s disease?
dull, boring, constant pain not exacerbated by activity
what are the stage 3 paget’s disease findings?
bone enlargement, thick cortices, trabecular accentuation
what do the radiographic features of stage 2 paget’s give the apperacne of?
picture frame vertebrae
the diffuse increase in bone density with stage 3 Paget’s diseas gives what apperance?
Ivory vertebrae
what are the ddx for ivory vertebrae?
blastic metastasis
Paget’s
hodgkin’s lymphoma
what are the complications of paget’s?
spinal canal and forminal stenosis from bony overgrowth
early osteoarthritis
malignant degeneration into osteosarcoma
paget’s diseas can leed to what type of malignany?
osteosarcoma
what are the primary malignant neoplasms of bone?
osteosarcoma (conventional)
chondrosarcoma
Ewing sarcoma and primitive neuroectodermal tumor
myeloproliferative disorders
plasma cell myeloma
plasamacytoma
Hodgkin disease
leukemia
what are primary benign neoplasms?
Enostosis
Osteochondroma
Osteoid osteoma
Aneurysmal bone cyst
Giant Cell tumor
osteoblastoma
what are tumor like lesions?
neurofibromatosis type 1 and langerhans cell histiocytosis
what is vertebra plana?
vertebral body is significantly flattened, with minimal height remaining anteriorly and posteriorly.
what are the radiographic findings of sickle cell?
bony changes
granular skull
hair on end skull
H vertebrae
osteoporosis
what conditions lead to posterior vertebral body scalloping?
Achondroplasia
Acromegaly
Hurlers/Morquio’s
Spinal tumors (meningioma, ependymoma)
Hydrocephalus
Neurofibromatosis
what conditions may cause anterior vertebral body scalloping?
Aortic Aneurysms
Lymphadenopathy
Normal variant
Tuberculosis

what is seen here?
spondylosis

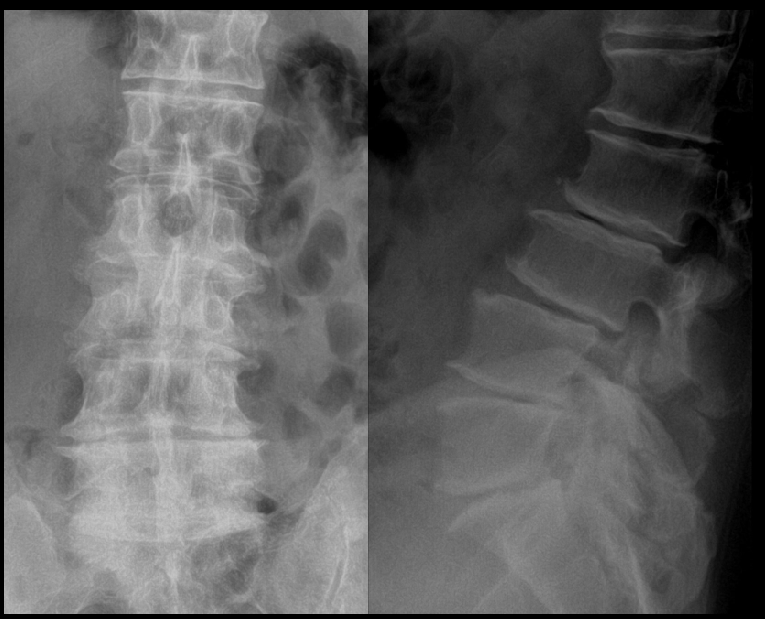
what is seen here?
multiple intervertebral osteochondrosis

what is seen here?
degenerative disc
what is seen here?
facet arthrosis

what is seen here?
neuropathic arthropathy at L2/L3

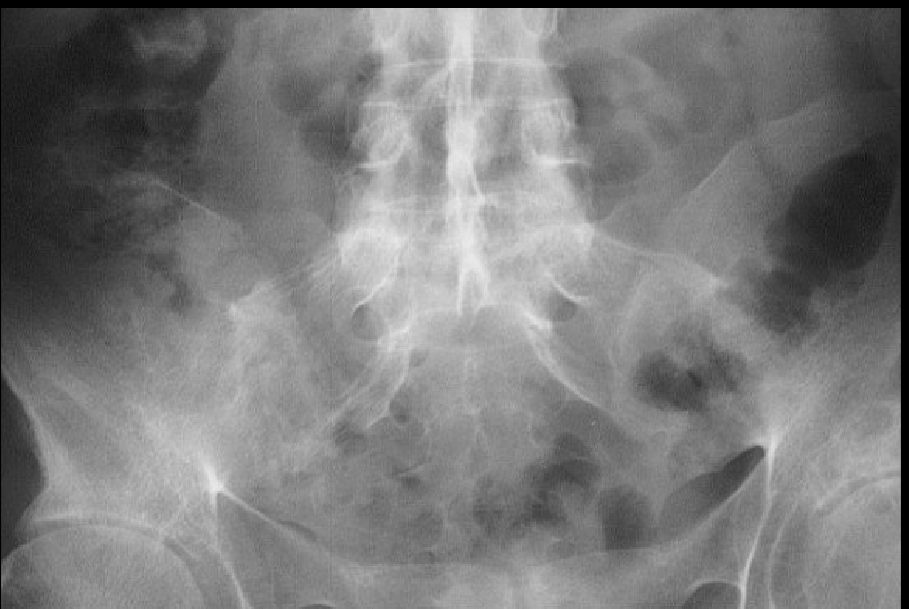
what is seen here?
AS with stage 2 SI joint involvement
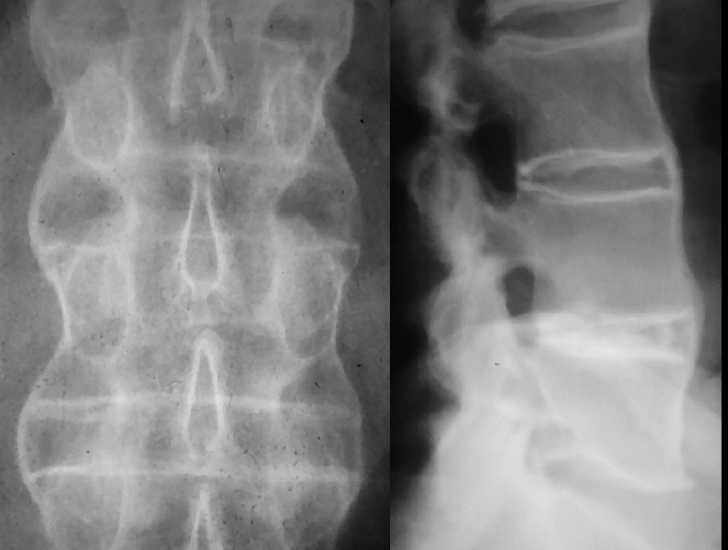
what is seen here?
AS with stage 3 SIJ involvment

what is seen here?
AS

what is seen here?
AS
what is seen here?
AS