Advanced Nursing Exam 1
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
88 Terms
Five Rights of Delegation:
a) Right Task
b) Right Circumstance
c) Right Person
d) Right Direction/Communication
e) Right Supervision
What can/cannot be delegated to LPNs?
no education, no discharging/admissions, no teaching
can do NG feeds, wound dressing changes, trach care, low-risk medications
What is evidence-based practice?
problem-solving approach to clinical decision making (Best practice + patient preference + clinician expertise = EBP)
Steps of the EBP Process:
- Step 1 of the EBP process is asking a clinical question in the PICOT format: P = patients/populations, I = intervention, C = comparison, O = outcome, T = time period
- Step 2 – thorough collection of evidence based on the clinical question.
- Step 3 – critically appraising and synthesizing evidence found in the search.
- Step 4 – implementing the evidence in practice.
- Step 5 – evaluating the outcome in the clinical setting.
- Step 6 – share the outcomes of the EBP change so that other health care providers and patients benefit from what you learned from your experience.
Cultural Factors which Influence Healthcare: Native American
Use folk healers, ghost sickness (ghosts cause living people to get sick), rarely circumcise boys
Cultural Factors which Influence Healthcare: Hispanic
- Strong family values, typically use folk healers, high risk for obesity and diabetes, multi-generational living in one home
- Recent immigrants may be at risk for physical and mental health problems
Cultural Factors which Influence Healthcare: African American
Less positive healthcare outcomes, high risk for cardiovascular diseases and HTN
Types of Assessment: emergency
rapid history while maintaining vital functions
Types of Assessment: comprehensive
head-to-toe assessment w/ detailed history
Types of Assessment: focused
focused on body system with the main concern
Steps of the Nursing Process:
- Assessment — Subjective and objective data are collected and will be the bases of the plan of care.
- Diagnosis — Assessment data are analyzed and a judgment about the problem is made. It includes identifying and labeling human responses to actual or potential health problems or life processes.
- Planning — patient outcomes or goals are developed for the diagnosis, and nursing interventions are identified to accomplish the outcomes.
- Implementation — activation of the plan; the nursing interventions are performed.
- Evaluation — continual activity; it is determined whether the patient outcomes were met as a result of the nursing interventions.
Order of physical assessment:
- General survey - what you can see right when you walk in the room or with a brief interaction
- Inspection, palpation, percussion, auscultation (except for GI where auscultation is second)
How to best teach adults:
- Adult education will occur in steps & must encourage motivational interviewing
- Self-efficacy is important to strengthening commitment to change
- Nurse should not use medical terms during education
- Teach-back technique is most effective for adults
- Teach them what they want to learn first!
Stages of Transtheoretical Model of Health Behavior Change:
Precontemplation - not considering change or learning
Contemplation - thinking about change
Preparation - planning change, gathering info on how to change
Action - change has begun
Maintenance - change becomes part of regular behavior
Termination - change is now part of lifestyle
When using the Transtheoretical Model of Health Behavior Change during patient teaching, the nurse identifies that the patient who states, "I walked regularly for about a year to help prevent osteoporosis, but recently I haven't been motivated to continue," is in the stage of:
Action
Role of caregiver in teaching/learning:
- Caregiver needs should be identified before teaching to promote the patient's care and prevent complications after discharge
- Caregivers are most often women
- Caregiver stress can lead to burnout and potential abuse (encourage journaling, exercise, and use of humor)
Clinical manifestations of frailty:
unintentional weight loss, self-reported exhaustion, weakness, slow walking speed, low level physical activity
SCALES Nutritional Assessment:
-Sadness
-Cholesterol (High)
-Albumin (low)
-Loss or gain of weight
-Eating Problems
-Shopping and food preparation problems
Changes in older adult cognitive functioning:
- Most healthy older adults experience no noticeable decline in cognitive abilities.
- Short term memory recall may decline with age, but long-term and crystallized intelligence should not decrease
What is a durable power of attorney?
patient designates a surrogate to make medical decisions in event he/she loses decision making capacity
What is medicare?
- Medicare is federally funded insurance for people >65; covers those < 65 with disabilities or end-stage kidney disease
- Part A covers inpatient care, part b covers outpatient care, part d covers prescription drugs
- Does not cover long-term care, custodial ADLs or IADLs care, dental care or dentures, hearing aids, or eyeglasses
What is medicaid?
- State-administered program to assist people in poverty with medical expenses
- Can qualify for both Medicare and Medicaid
How to best manage a chronic illness:
- Most persons 65 y.o.+ have at least 1 chronic illness; the incidence of chronic disease triples after age 45
- Main goal of management is to prevent & manage crises to avoid exacerbation
- Patients should adhere to prescribed regimen, know s/s of crisis onset, and have a plan to manage a crisis when it occurs
- Social isolation should be prevented & normalize interactions with others
- Nurses should conduct comprehensive assessments & teach patient and caregiver
Roles in Patient Care: dietitian
help to create dietary plans for patients with illness or disease risk
Roles in Patient Care: speech therapy
assess & treat patients with speech & fluency issues and swallowing concerns
Roles in Patient Care: physical therapist
offer preventative and rehabilitative care to assist in increasing patient physical strength and abilities
Roles in Patient Care: occupational therapist
assist patients in developing, recovering, or improving skills necessary for daily living and employment
What are transitions of care & nurses' role in it?
- Transitions of care refer to patients moving between health care practitioners, settings, and home as their condition and care needs change
- Nurses are an essential part of care coordination by stressing actions that meet patient’s needs and facilitate safe, quality care. Collaborating with other members of the interprofessional team is critical.
Types of burns:
Thermal, chemical, smoke inhalation, electrical, cold thermal
How is the severity of burns determined?
Depth, total body surface area effected, location, patient risk factors
How are burns staged?
Superficial partial thickness (1st degree) - epidermis only
Deep partial thickness (2nd degree) - epidermis & dermis
- Partial thickness burns heal from edges and dermal bed
Full thickness (3rd & 4th) - into muscle and bone; typically experience no pain
- Full thickness burns must have eschar removed and skin grafts applied
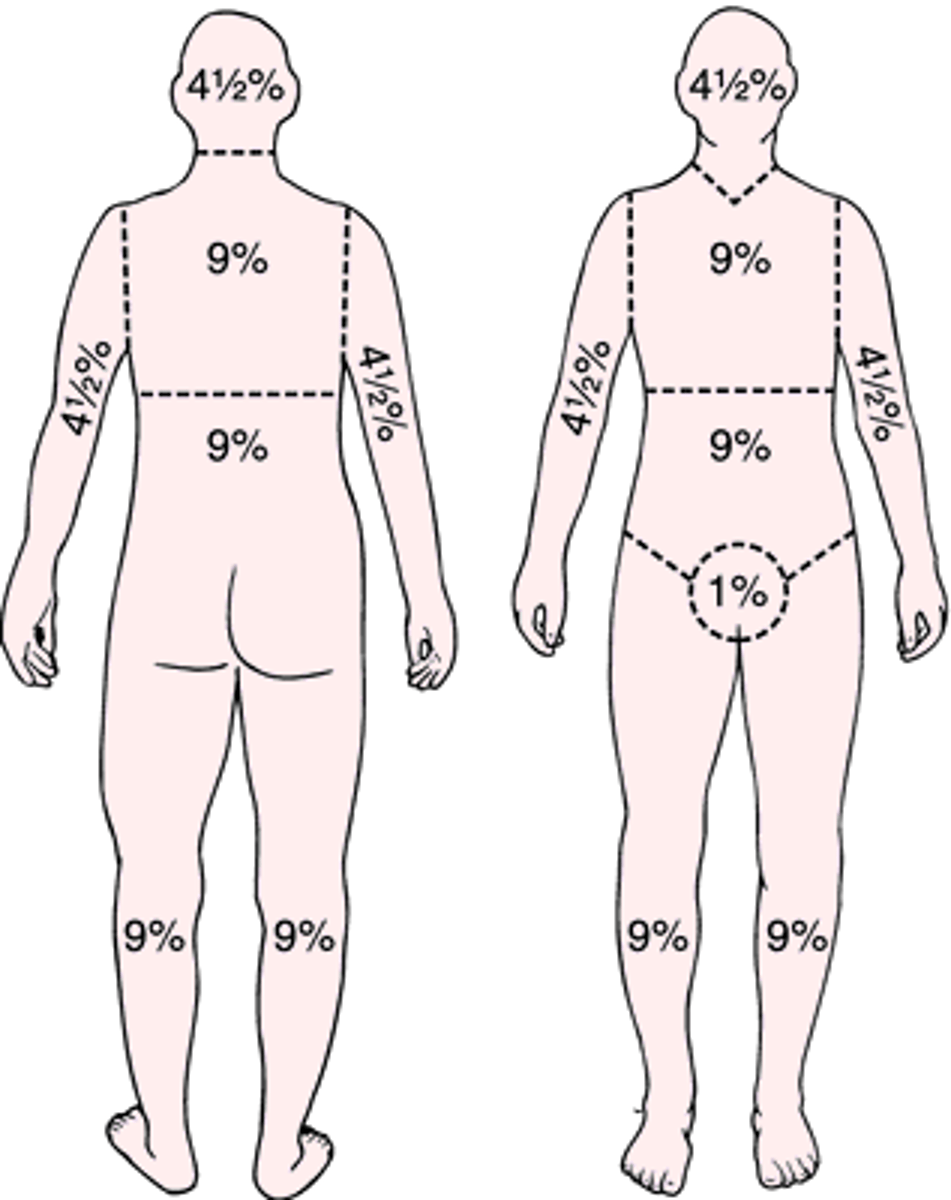
What is the rule of nines?
Thermal burns (causes, severity):
- Caused by flame, flash, scald, or contact with hot objects
- Most common type of burn injury
- Severity of injury depends on temperature of burning agent & duration of contact
Chemical burns (causes, action):
- Caused by acids (household cleaners), alkalis (cement), and organic compounds (gasoline)
- Alkali burns are hard to manage because the damage will continue after neutralization
- Often results in injury to the skin, eyes, respiratory system, and liver & kidneys
- Action: remove clothing, neutralize chemical, monitor for further destruction for 72hrs
Smoke Inhalation (cause, importance, action):
- Damage to respiratory tract from inhalation of hot air or noxious chemicals
- Major predictor of mortality in burn victims
- Action: assess for airway compromise for 12-48hrs
What is metabolic asphyxiation?
- Oxygen is displaced by CO2, leading to inadequate oxygenation
- S/S: red face
- Treat with 100% humidified oxygen
Electrical burns (cause, severity, action):
- Caused from coagulation necrosis by heat from an electric current
- Damage to skin, nerves, vessels
- Severity depends on voltage, tissue resistance (fat & bone offer the most resistance), current pathway, surface area, and duration of flow
- Action: stabilize cervical spine, continue to assess as injury may be difficult to assess, monitor for dysrhythmias, metabolic acidosis, and myoglobinuria (leads to kidney injury)
Pre-hospital care of small thermal burns:
- Remove person from source of burning
- cover with clean, cool, tap water towel
Pre-hospital care of large thermal burns:
- Remove person from source of burning
- If responsive, follow ABC's
- If unresponsive, follow CAB (elevate limb)
- Cool burn for < 10 min
- Remove burnt clothing & wrap in dry blanket
Phases of burn management: emergent (patho, manifestations, concerns):
- Patho: massive shift of fluids (third spacing), neutrophils & monocytes accumulate, fibroblasts begin wound repair within 6-12hrs after injury, immunosuppression
- Manifestations: hypovolemic shock, blisters, paralytic ileus, shivering from inflammation, altered mental status
- Primary concerns are hypovolemic shock & edema
Complications of the emergent phase of burn management:
dysrhythmias, hypovolemic shock, VTE, airway obstruction, acute tubular necrosis due to decreased blood flow
Care of the emergent phase of burn management:
- 100% humidified oxygen
- endotracheal intubation
- escharotomies (to relieve chest tissue tightness)
- high fowler's if not intubated
- two IV lines for > 15% TBSA
Wound care for the emergent phase of burn management:
- delayed until patent airway, adequate circulation, and fluid replacement
- silver sulfadiazine for antimicrobial
Nutritional care for a patient in the emergent phase of burn management:
- Fluid replacement is priority!
- Patient will be in hypermetabolic state, so caloric needs are elevated (use enteral feeds)
Acute/healing phase of burn management (beginning & end, patho, action):
- Begins with the mobilization of fluid & subsequent diuresis; ends with wounds are healed or covered with grafts
- Patho: necrotic tissue will slough, granulation tissue forms
- Action: monitor for infection (S/S: hypo/hyperthermia, tachycardia, decreased BP, decreased urine output)
Pain management for patients with burns:
- Continuous background pain: IV opioid or BID oral slow-release opioid
- Treatment-induced pain: analgesic before treatment
Rehabilitative phase of burn management:
patient begins to cope with new disability or deformity
Electrolyte changes with burns: hypo/hypernatremia
Hyponatremia can develop from excessive GI suction, diarrhea
- Water intoxication - dilutional hyponatremia - avoid with juices, nutritional supplements
Hypernatremia may develop following successful fluid replacement
Electrolyte changes with burns: hypo/hyperkalemia:
- Hyperkalemia may occur if patient has renal failure or a massive deep muscle injury because large amounts of potassium is released from damaged cells
- Hypokalemia occurs with vomiting, diarrhea, prolonged GI suction
What occurs in the vascular inflammatory process?
- Arterioles constrict, histamine is released, and vessels dilate leading to hyperemia
- Fluid in tissue spaces turns from serous fluid to later containing plasma proteins, which exert more oncotic pressure
- Fibrinogen will also enter the tissues to form a clot to trap bacteria
What happens in the cellular inflammatory process?
- Blood flow through capillaries slows and blood viscosity increases
- Neutrophils & monocytes arrive via chemotaxis
- Enzyme cascade of the complement system holds the pathogens so they don't escape
- Lymphocytes arrive to create immunity (memory cells)
- Histamines, serotonin, and kinins are released during this time
What do neutrophils do?
arrive 1st (6-12hrs after injury) to phagocytize bacteria, then explode creating pus
What do monocytes do?
arrive 3-7 days after injury, transform into macrophages, and phagocytize debris
What do histamines do?
released by complement components causing vasodilation
What does serotonin do for inflammation?
stimulates smooth muscle contraction
What do kinins do?
cause the stimulation of pain
What do prostaglandins do?
vasodilate and encourage inflammation
What does thromboxane do?
vasoconstricts and calls platelets to the scene to form a clot
Medications to Inhibit Inflammation:
- Steroids inhibit arachidonic acid which is converted into prostaglandins
- NSAIDs inhibit the cyclooxygenase pathway
Local VS Systemic Inflammation:
- Local: symptoms include redness, heat, pain, swelling, and loss of function
- Systemic: fever, hypotension, tachycardia, nausea, malaise, labs shift to the left
Fever Pathophysiology:
- Onset is triggered by cytokine release to trigger the hypothalamus to increase temperature
- Synthesis of prostaglandins is the most important metabolic change to a fever
- Hypothalamus stimulates the ANS to cause shivering and decreased perspiration
Acute vs Subacute vsChronic Inflammation:
- Acute: no residual damage, heals within 2-3 weeks, neutrophil-dominated
- Subacute: persists past 2-3 weeks; example: endocarditis
- Chronic: lasts for years, lymphocyte & macrophage-dominated; example: auto-immune disease
Nursing Management of Inflammation:
- Recognize early & treat immediately
- Observe pt, monitor VS
- Administer aspirin, acetaminophen, NSAIDs, and corticosteroids for fever
- RICE
Regeneration vs Repair:
- Regeneration: replacement of lost cells and tissues with cells of the same type. The ability of cells to regenerate depends on the cell type.
- Repair: healing as a result of lost cells being replaced by connective tissue. Repair is the more common type of healing and usually results in scar formation
What type of healing is done with pressure ulcers?
Secondary intention
Pressure Ulcer Staging: Deep Tissue Injury
Purple or maroon localized area of discolored intact skin

Pressure Ulcer Staging: Stage 1
Intact skin with non-blanchable redness
Pressure Ulcer Staging: Stage 2
Partial thickness loss of dermis, shallow open ulcer with pink/red wound bed
Pressure Ulcer Staging: Stage 3
- Full thickness skin loss; subcutaneous tissue visible
- Undermining may be present; looks like a crater
Pressure Ulcer Staging: Stage 4
- Full thickness loss that extends into muscle or bone
- Tunneling or undermining may occur
Pressure Ulcer Staging: Unstageable
- Full thickness tissue loss where depth is obscured by slough or eschar
- Dry eschar on the heels should not be removed
What are the most common sites of pressure ulcers?
Sacrum & Heels
Risk Factors for Ulcers:
Advanced age, anemia, contractures, diabetes, elevated body temperature, friction, immobility, impaired circulation, incontinence, mental deterioration
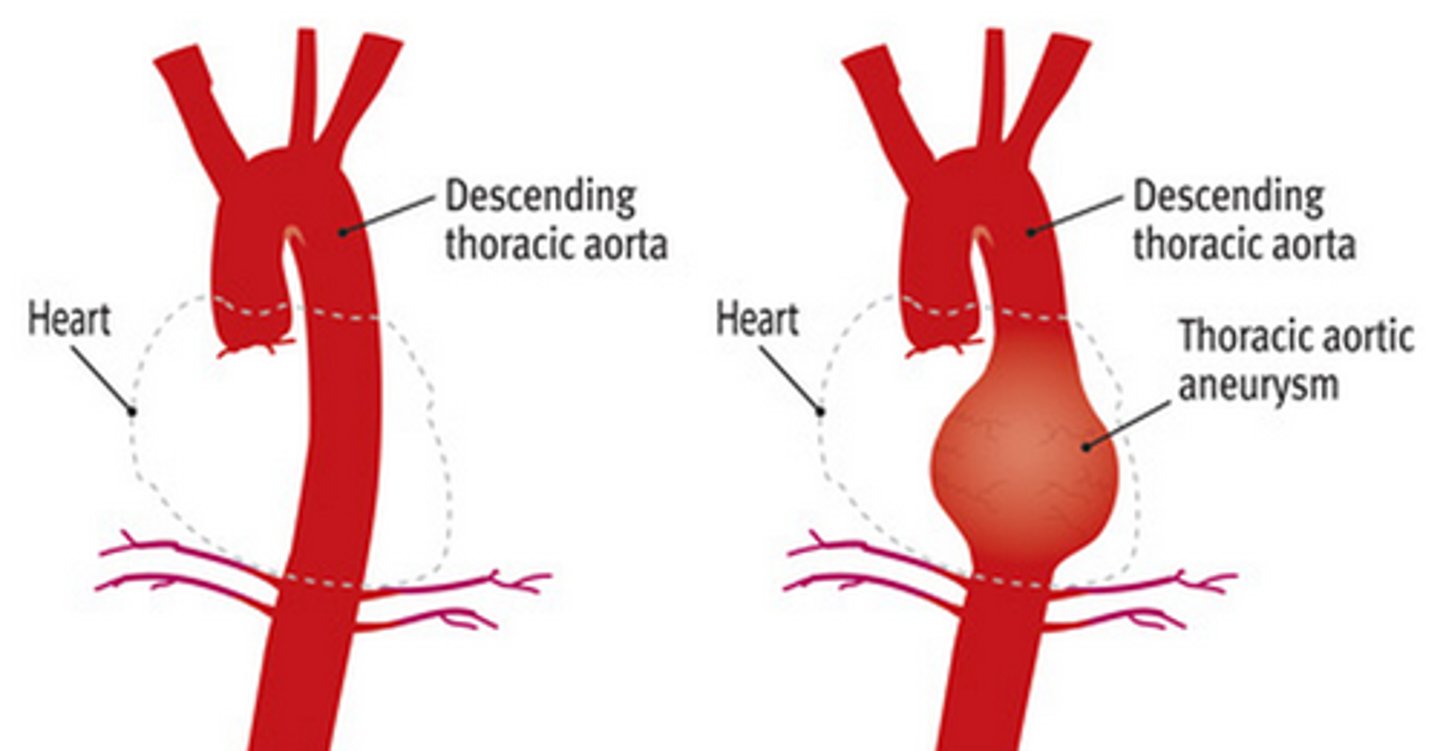
Definition of Aneurysm:
outpouching or dilation of arterial wall where the wall becomes lined with thrombi that can embolize; often seen in the aortic artery
Causes of Aneurysm:
- Atherosclerosis, genetics (Marfan’s), blunt trauma, inflammation, infection
- Risk Factors: age, males, HTN, CAD, family history, smoking
Symptoms of Thoracic Aorta Aneurysm (TAA):
asymptomatic, diffuse chest pain, interscapular pain
Symptoms of Ascending Aortic Arch Aneurysm:
- S/S: angina, TIAs, SOB, dysphagia
- If pressing on the superior vena cava, decreased venous return, JVD, edema of face & arms
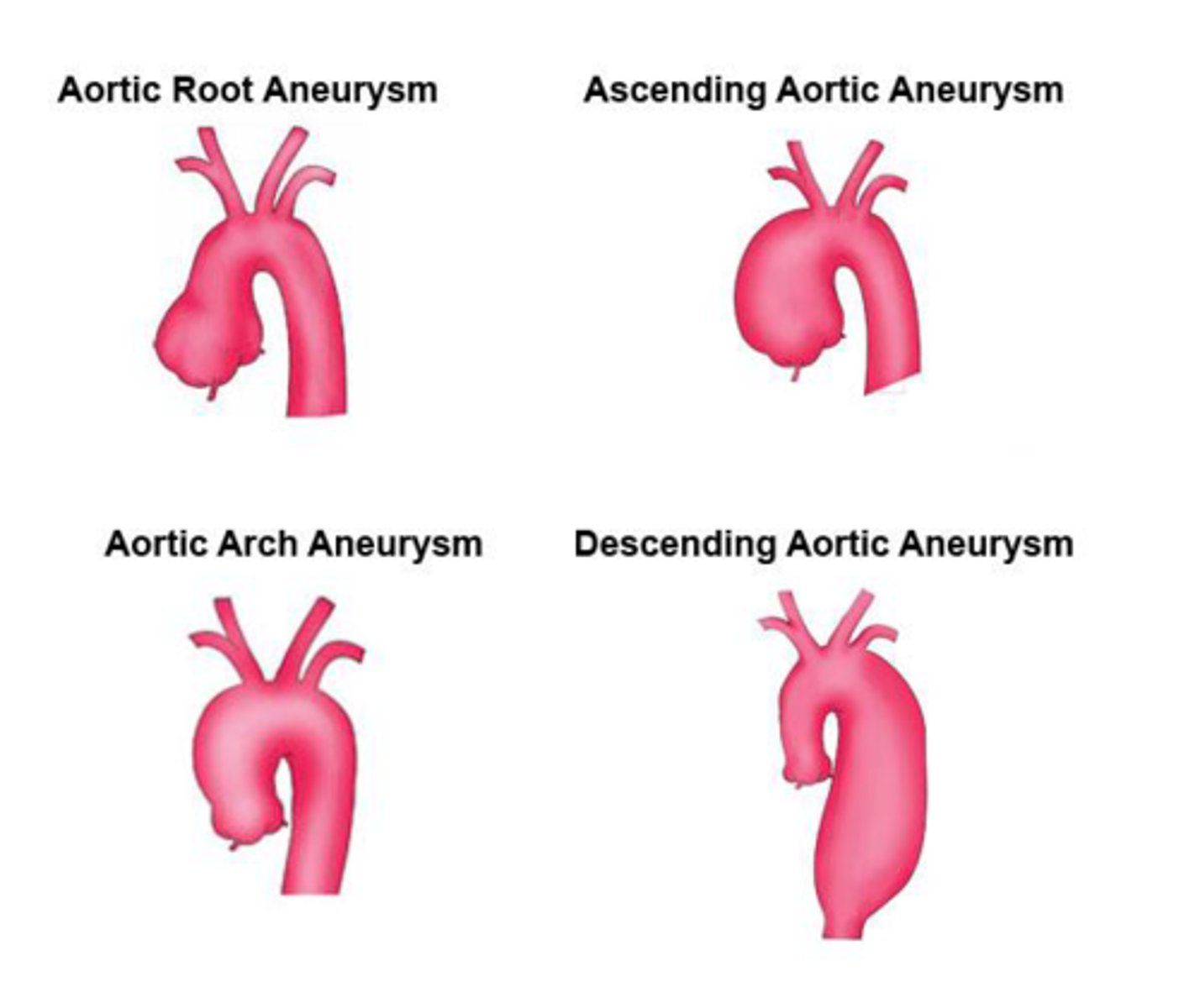
Abdominal Aortic Aneurysm (AAA): (S/S, detection)
- S/S: often asymptomatic, back pain, epigastric discomfort, intermittent claudication, blue toe syndrome (patchy mottling of the feet and toes in the presence of palpable pedal pulses)
- Pulsatile mass in the periumbilical area slightly to the left of the midline with a bruit may be present
- Frequently detected on physical exams and when being scanned for unrelated problems
Dissection/rupture of a AAA:
- Bleeding may be tamponade by surrounded organs preventing death
- will present with severe back pain & Grey Turner's sign
- S/S: diaphoresis, pallor, weakness, tachycardia, hypotension, periumbilical pain, change in LOC, pulsatile abdominal mass
- requires immediate surgery
Grey Turner's sign
bruising in flank area (lower back area)

Purpose of chest & abdomen x-ray and ECG with aneurysms:
- Chest - look if there are any mediastinal involvement
- Abdomen - looks for any calcification within the aneurysm
- ECG - to rule out MI
Purpose of echocardiography, ultrasonography, CT & MRI with aneurysms:
- Echocardiography - diagnosis of aortic valve insufficiency
- Ultrasonography - screens for aneurysm size
- CT - most accurate scan to determine length, diameter, thrombus presence, and surgical repair
- MRI - assess location & severity
What is considered a small aneurysm?
- 4-5.4cm
- Treated with risk factor modification - lower BP, scan to monitor size Q6-12 months
What is the threshold for a repairable aneurysm?
5.5cm +
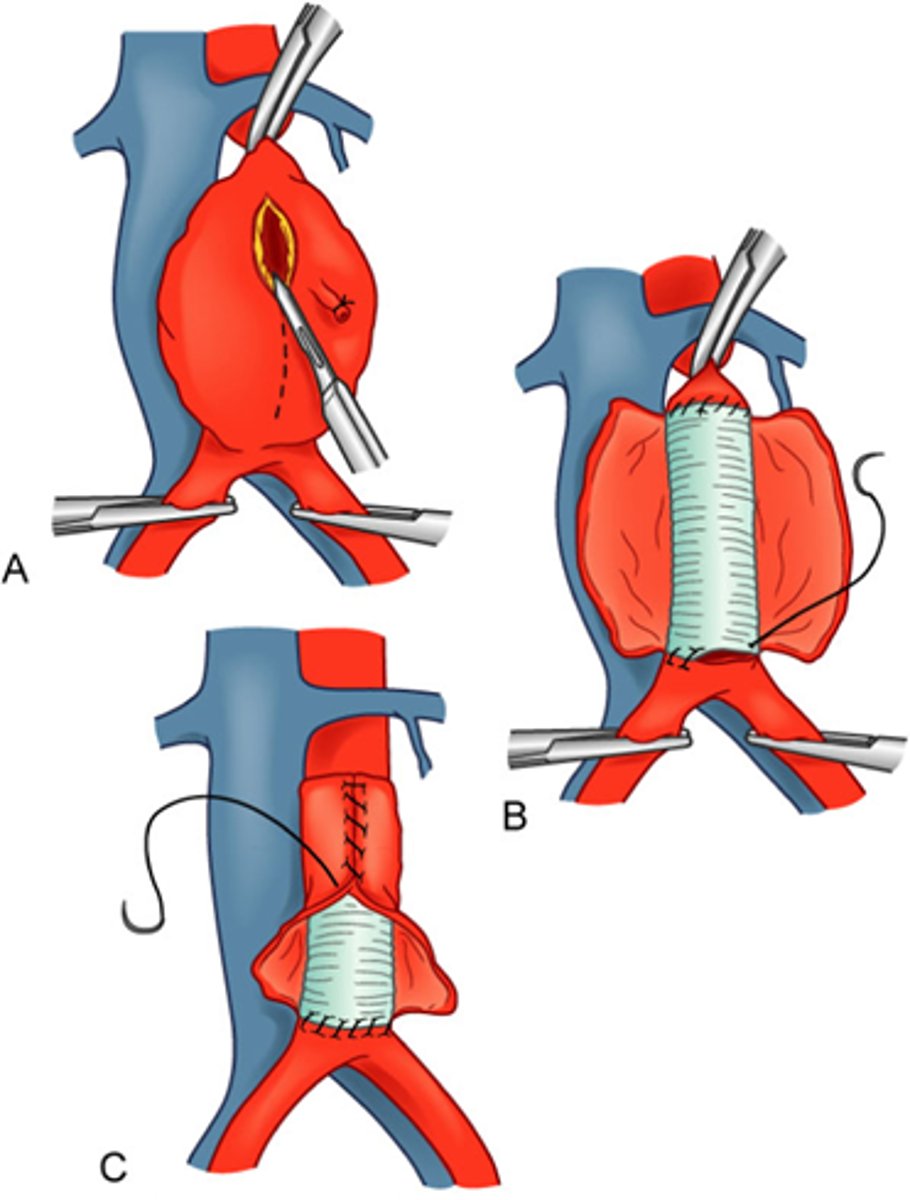
What is an open aneurysm repair (OAR)?
clamp above and below aneurysm, place graft & remove existing plaques, remove clamps; if renal arteries are clamped, you may permanently damage the kidneys
What is an endovascular graft procedure?
- non-invasive alternative to OAR
- Placement of a suture-less aortic graft into the abdominal aorta
- Done through femoral artery
Post-op care for endovascular graft procedure:
- maintain normal BP (systolic around 90)
- IV fluids
- CVP pressure monitoring
- hourly urine output monitoring
- pulse assessment (mark pulse locations with pen, routine ABI)
- NPO post op
- NG placed to low-intermittent suction
- parental nutrition
Complications in an endovascular graft procedure:
endoleak, aneurysm growth, aortic dissection, stent migration, renal artery occlusion, thrombus, infection