Connective tissue histology
1/41
Earn XP
Description and Tags
Year 1 - Semester 1
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
types of ordinary connective tissue
loose and dense
types of loose connective tissue
aerolar, adipose, reticular
features of aerolar tissue
empty spaces between sections of tissue, loose open framework of collagen, elastic and reticular fibres, lots of ground substance
ground substance
a hydrated, gel-like material that fills the spaces between cells and fibers
function of aerolar tissue
supports epithelial linings of GI, respiratory and urinary tracts, loose packing between cells of other organs
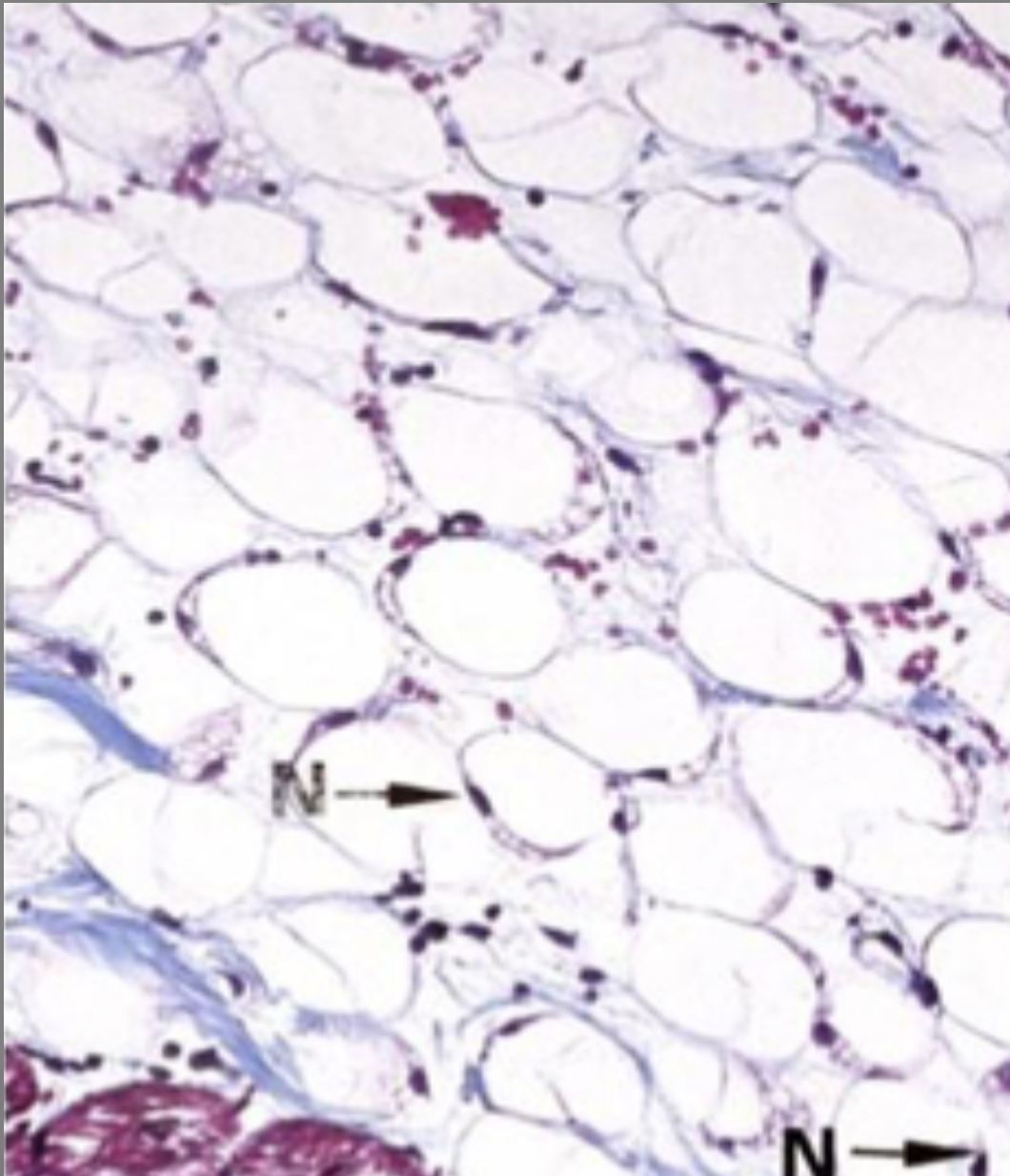
features of white loose adipose tissue
‘chicken wire’ appearance, each adipocyte is supported by delicate network of collagen and reticular fibres, fibrocytes, mast cells, sparse amorphous ground substance, rapid turnover of lipid
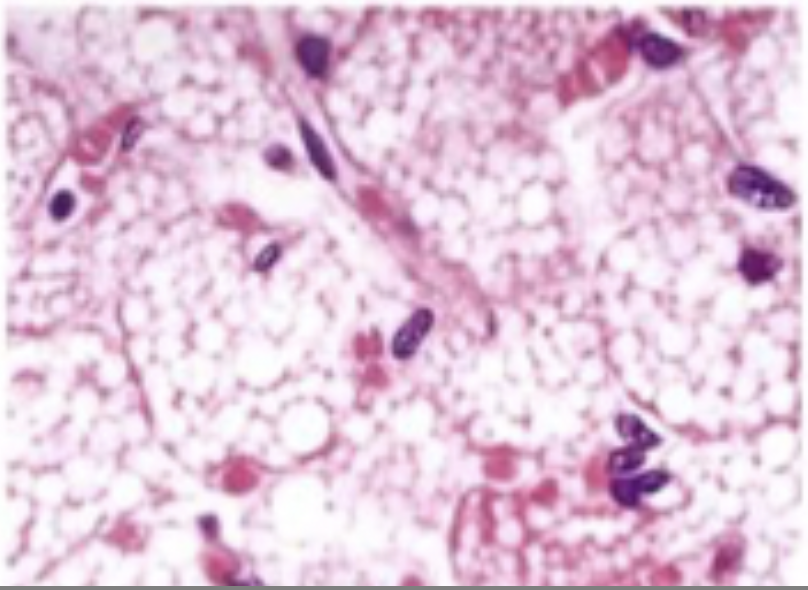
features of brown adipose tissue
large, rounded nuclei, vacuolar-looking tissues inside cell instead of large cytoplasm space
function of adipose tissue
energy storage, insulation, supports and protects organs
function of brown adipose tissue
thermoregulation in young and small mammals by dissipating stored energy as heat
features of loose reticular tissue
3D mesh of collagen reticular fibres and reticular cells, loose ground substance
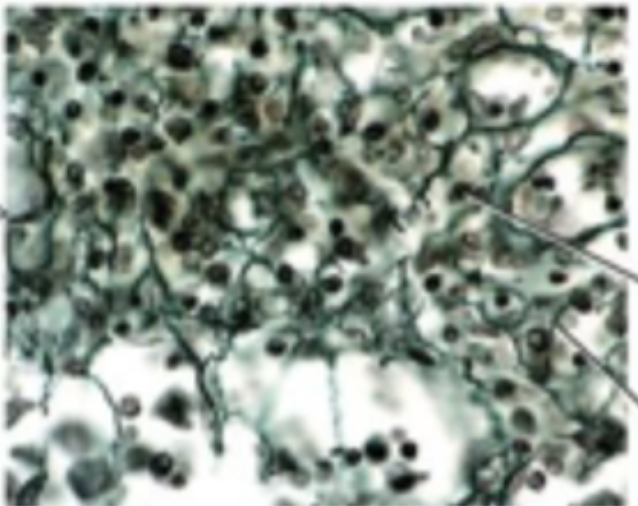
function of loose reticular tissue
provides framework for lymphoid and hematopoietic organs, acts as a filter for migrating immune cells, allows exchange of nutrients and waste between blood and parenchymal cells
features of dense irregular tissue
little ground substance, dense network of randomly interwoven collagen fibres and extracellular proteins, few fibroblasts
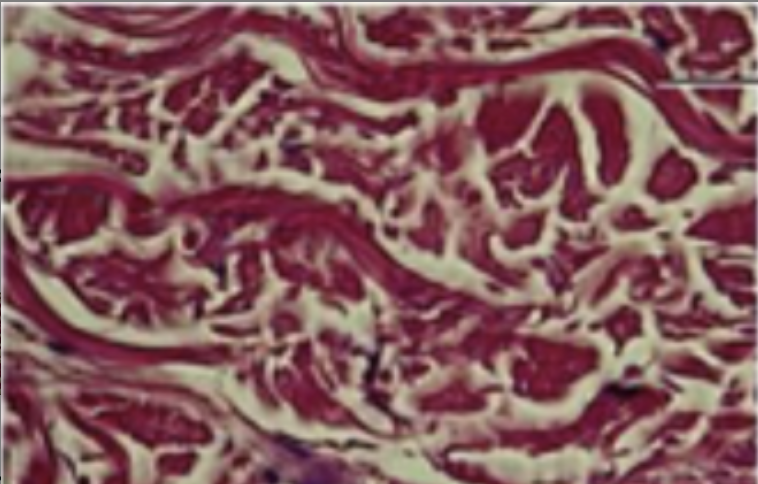
function of dense irregular tissue
provides strength, stability and protection by withstanding forces from multiple directions so prevents tearing in skin dermis, organ capsules and joint capsules
features of dense elastic tissue
high concentration of elastic and collagen fibres
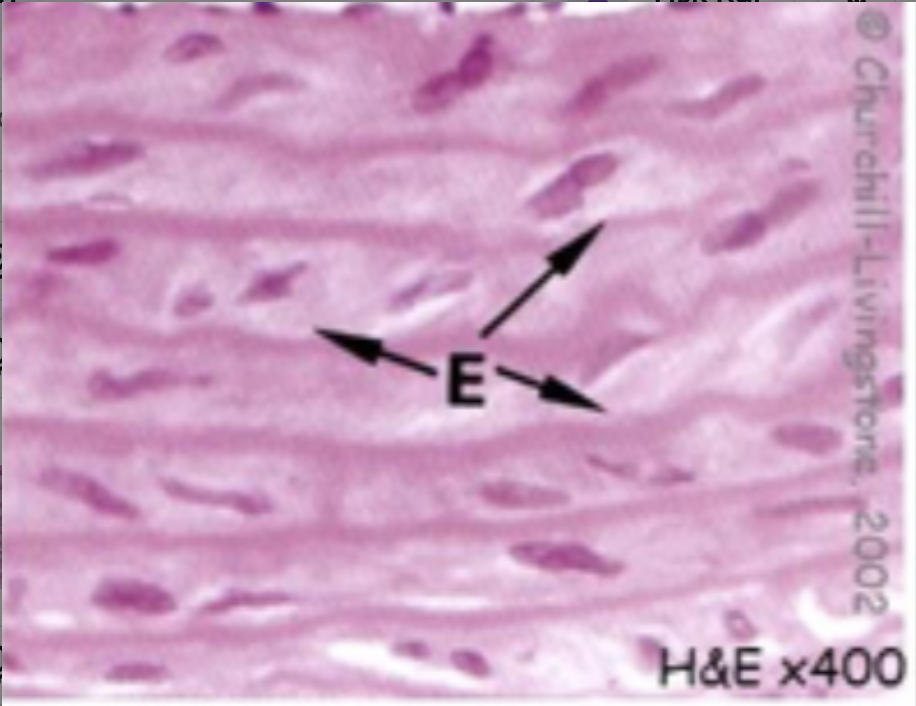
function of dense elastic tissue
allows recoil of tissue following stretching, maintains pulsatile flow of blood through arteries, aids passive recoil of lungs following inspiration
liquid support tissue
specialised connective tissue with a fluid extracellular matrix, can be blood or lymph
function of liquid support tissue
to transport substances, homeostasis, defence
function of basement membrane
cell adhesion, diffusion barrier, regulation of cell growth
types of cartilage tissue
hyaline, fibrocartilage, elastic
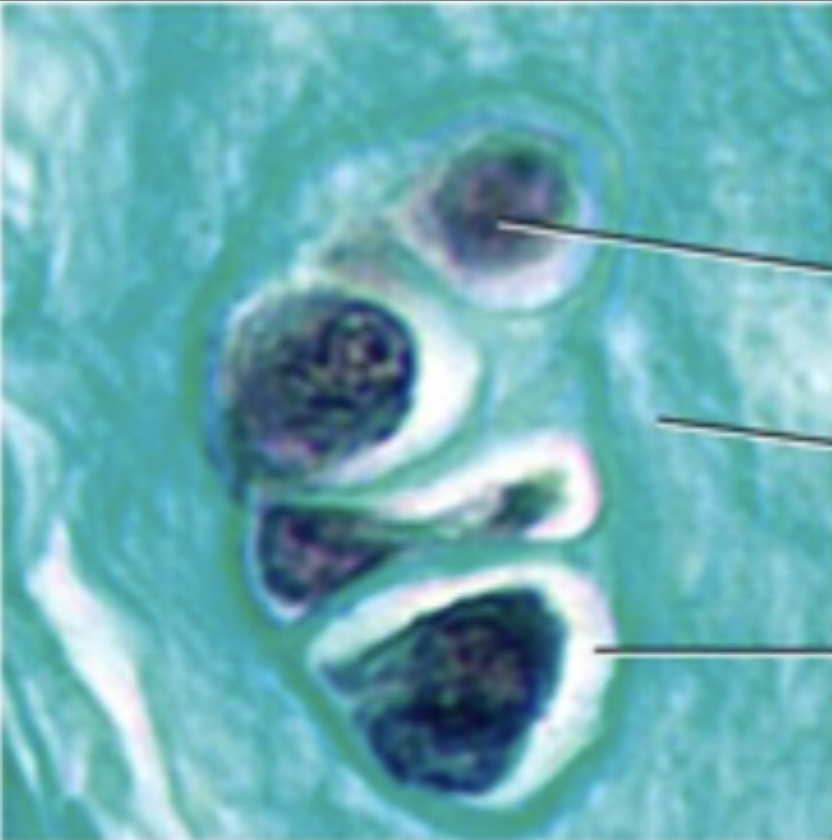
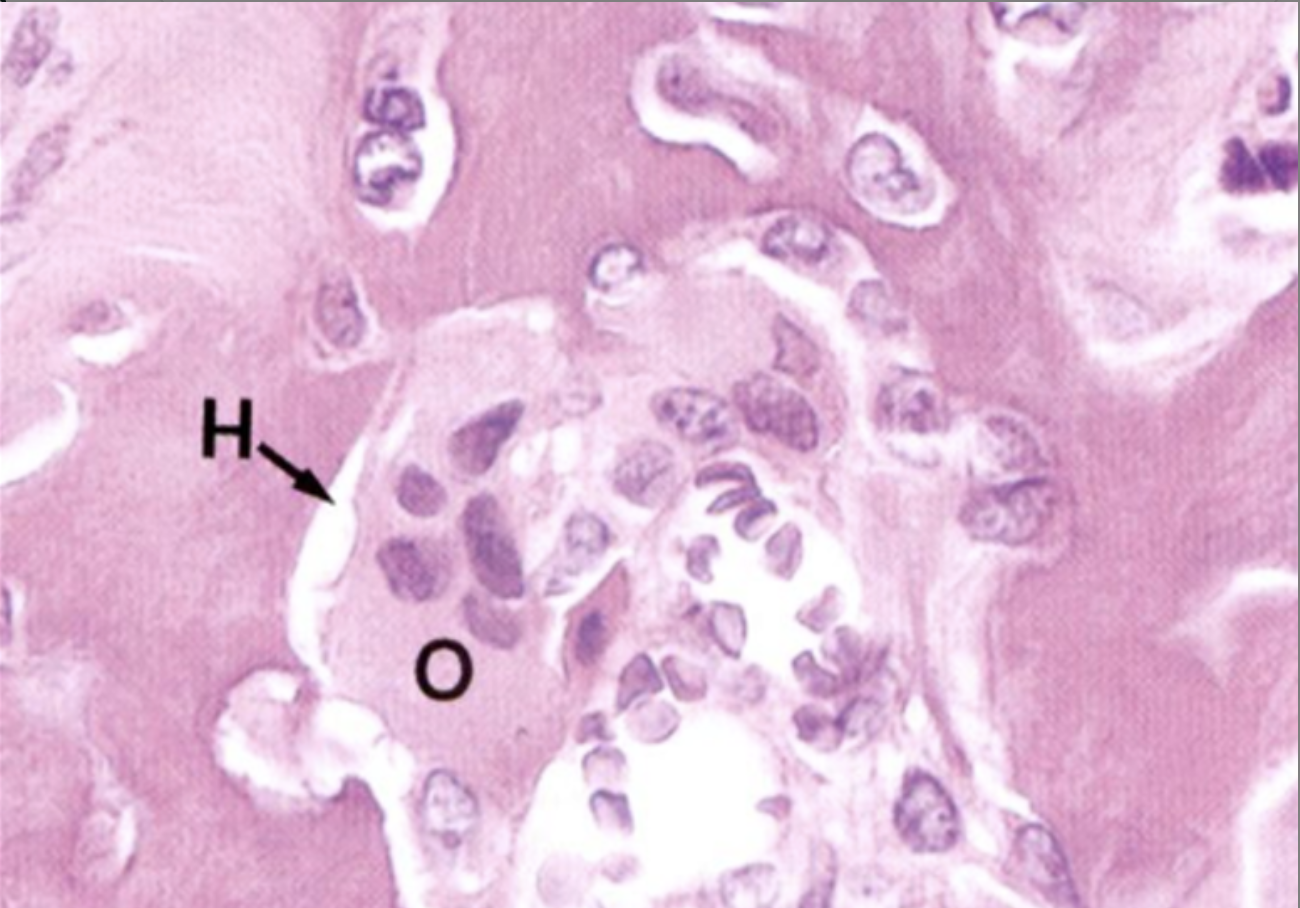
features of hyaline cartilage
chondrocytes in lacunae often clumped together, glassy matrix, no visible fibres

function of hyaline cartilage
to provide a smooth, low-friction surface for joints, protect bones, supportive framework for structures
features of fibrocartilage
chondrocytes in lacunae, collagen fibres in ground substance, fewer chondrocytes, chondrocytes aligned in rows
function of fibrocartilage
to provide shock absorption, structural support and stabilisation to intervertebral discs
annulus fibrosis of intervertebral disc
compact outer ring of fibrocartilage surrounding gelatinous core (nucleus pulposus)
features of elastic cartilage
large, clear cytoplasm, large nuclei, elastic and collagen fibres in ground substance
what is the most common type of cell in adult connective tissue?
fibroblast
what is the most common type of fibre produced by fibroblasts?
collagen
functions of bone
support soft tissue and attachment for skeletal muscles, protection of internal organs, assists movement, mineral homeostasis, blood cell production from red bone marrow, triglyceride storage as yellow bone marrow
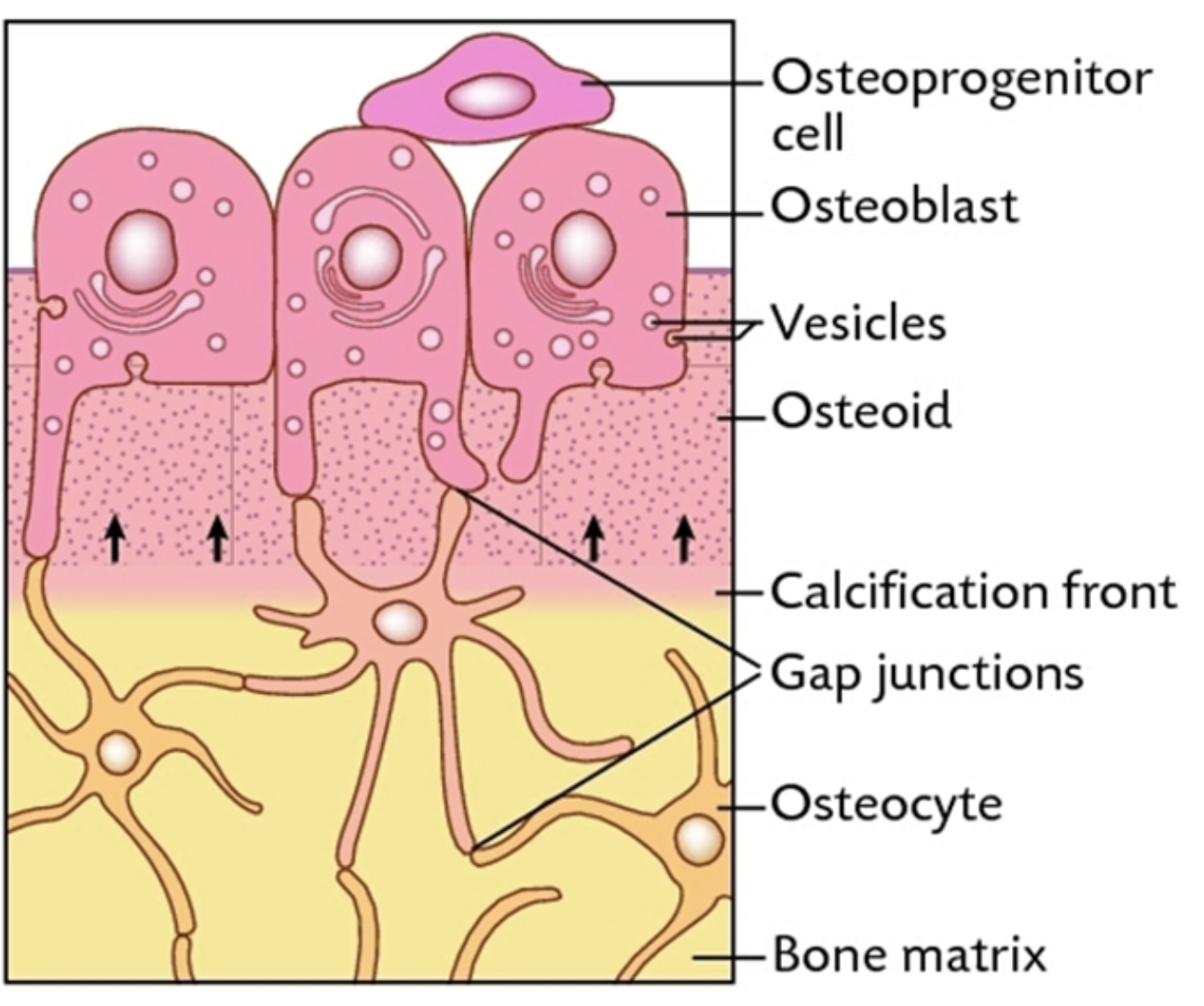
osteogenic cell
cell capable of forming new bone tissue
osteoprogenitor
specific mesenchymal stem cell found in periosteum and endosteum that differentiates into osteoblasts, found just beneath the connective tissue layer
process of bone formation
osteoprogenitors differentiate into osteoblasts which secrete osteoid (organic matrix)
mineral crystals are added to the osteoid which causes the matrix to calcify, cells die leaving cavities, calcium ions and other electrolytes are released from osteoblasts by exocytosis
osteoblasts deposit bone on cartilage template and become entombed in the bone matrix, causing them to become osteocytes
bone resorption
osteoclasts attach to bone surface and release weak acid and enzymes into bone matrix to dissolve it, causing calcium and phosphate ions to be released which diffuse into capillaries
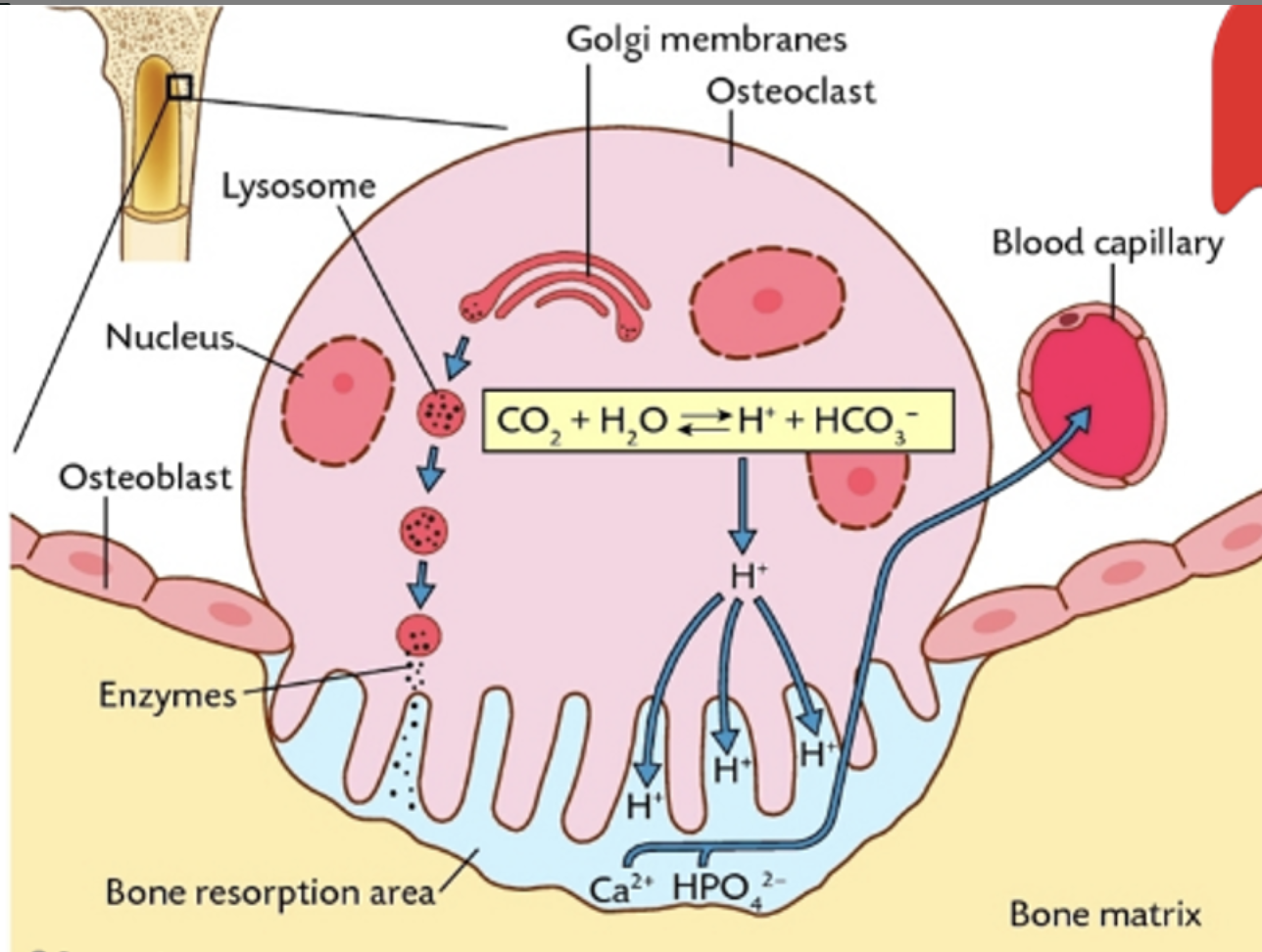
Howship’s lacuna
a depression resorbed from bone surface, into which acid and proteolytic enzymes are released from osteoclasts
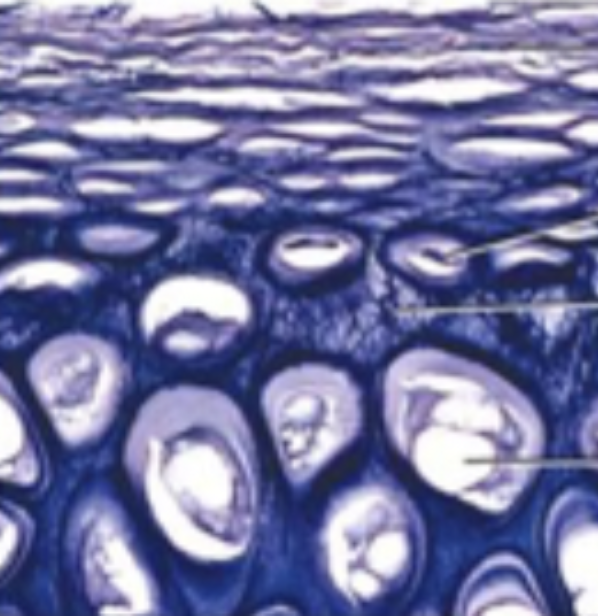
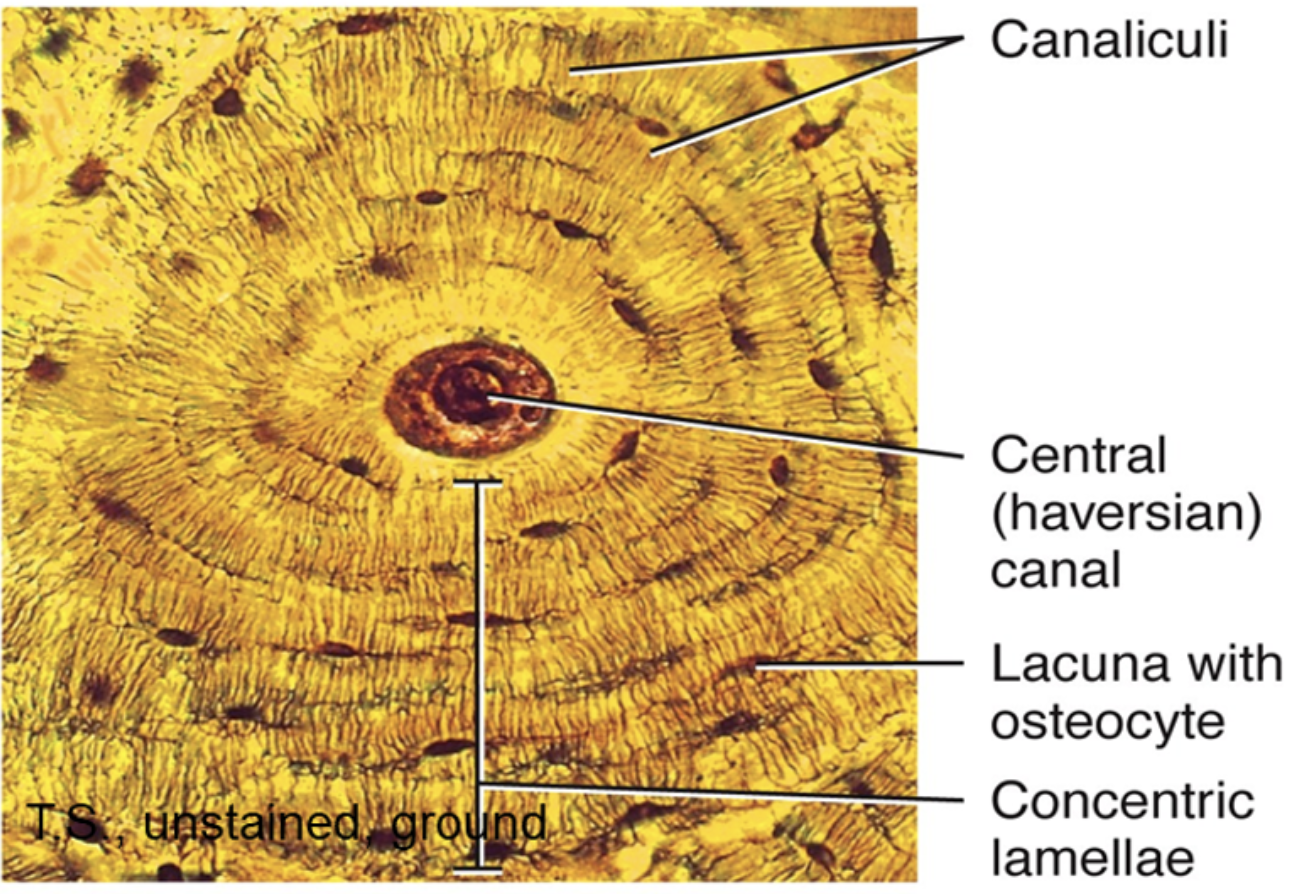
Haversian system
the structural and functional unit of compact bone, consists of a central Haversian canal containing blood vessels and nerves, surrounded by concentric rings of bone matrix called lamellae

histological features of compact bone
osteons with Haversian canal, concentric lamellae, lacunae with osteocytes (elongated brown specks arranged in concentric layers around Haversian canals), canaliculi visible as fine lines, periosteum, Haversian systems visible in transverse sections, interstitial systems
periosteum
a double-layered membrane that covers the outer surface of compact bone, protecting it and providing it with blood vessels and nerves
method of flat bone development
intramembranous ossification
flat bone development process
mesenchymal cells differentiate into osteoblasts and blood vessels
osteoblasts gather in clusters to form ossification centres and secrete osteoid
calcium salts deposit on the osteoid, causing it to calcify
osteoblasts become trapped in the matrix and mature into osteocytes
this process continues and the outer layer of tissue becomes compact bone while the inner portion becomes spongy bone
method of long bone development
endochondral ossification
long bone development process
mesenchymal cells are induced to become chondrocytes which secrete a cartilage matrix
chondrocytes near the centre of the model enlarge and the surrounding matrix begins to calcify
calcified cartilage matrix is invaded by blood vessels and specialised cells
osteoblasts and other cells enter the matrix through blood vessels
osteoblasts deposit bone on calcified cartialge, replacing it with bone
tissues found within the marrow cavity
adipose and haemotopoietic tissue
where is fibrocartialge most commonly found?
tendon insertions