BPK 305 Midterm 1
1/160
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
161 Terms
What is the average blood volume? Give a breakdown of its components.
Avg. Blood Volume ~5L
Serum or plasma ~60%
*Serum is what is left when you remove fibrin from plasma
RBC (Erythrocytes, ie. hematocrit) ~40%
WBC (Leukocytes) <5%
Platelets/Thrombocytes <1%
How do you determine a hematocrit?
Hematocrit= Height of RBC's/Total Height
Approximately what percentage of plasma is composed of water?
92% w/v
What electrolytes constitute the blood plasma?
Na⁺ → 145mM
K⁺ →4-5mM
Ca²⁺→ 2-2.5mM
Mg²⁺→ 1.5mM
H⁺→ pH 7.35-7.45
HCO₃⁻→ 24mM
*Regulated by the Renin Angiotensin system
What nutrients constitute plasma?
Glucose → 5mM
Lipids → 7.5mM
Cholesterol → 4-7mM
Vitamins → <0.1mM
Free Fatty Acids → 0.4-2mM
(Fuel of choice for the cardiac muscle)
What waste products are carried around in plasma?
Urea
Creatine
Uric Acid
Bilirubin
Name the specific proteins that are present in blood plasma. Approximately how much of the plasma is composed of proteins?
~7% w/v
Albumin → 4.2g/100mL
*Plays a role in transporting hydrophobic molecules around blood
Globulin → 2.8g/100mL
*Gamma form are antibodies
Fibrinogen → 0.3g/100mL
What gases are present in plasma?
CO₂
O₂
N₂
Briefly outline the role of Calcitonin and Parathormone.
Calcitonin makes calcium go into the blood from bone
Parathormone takes calcium out of the blood and puts it back into bone
What are the cellular constituents of blood?
RBC ~5 million/µL
WBC ~7000/µL
Platelets ~250,000/µL
→ Smaller
Total= ~40-45% blood volume
In hematopoiesis, what percentage of pluripotent stem cells become leukocytes and erythrocytes?
75% of cells produced become Leukocytes
→Lifespan= hours-days
25% cells produced become erythrocytes
→Lifespan 90-120 days
What cytokines regulate hematopoiesis?
Colony Stimulating Factors → Leukocytes
Erythropoeitin (EPO) → Erythrocytes
Thrombopoeitin (TPO) →Platelets
What is the main role of RBC's?
O₂ transport!
→Requires hemoglobin (Hb)
→Hb production requires: iron, B12, folic acid
Describe the structure of hemoglobin.
Hb has 4 global subunits
→Each subunit has a heme group
→The heme group contains Fe to which O₂ binds
Hb binds 4 oxygen molecules
→binding is co-operative (important in maintaining a high saturation of oxygen)
→binding of one oxygen molecule facilitates binding of another
Antigens on RBC surface (ex. A, B, Rh
→implicated in transfusion/rejection
List 3 factors that affect RBC hematocrit.
→Lower in women than men
→Higher at altitude (highest recorded is 78%)
→Higher in athletes
What factors regulate hematocrit?
→Oxygen (via EPO)
→Nutritional status
→Menstruation/hemorrhage (↑ fluid content in blood)
→Hormones
→Vitamin B12 complex
→Folic Acid
What is anemia? What are the 4 types?
Anemia= insufficient Hb
→Hypochromic (low Hb in RBC's due to Fe deficiency)
→Megaloblastic (pernicious and non-pernicious--B12 deficiency)
→Hemolytic (fragile RBC's, inappropriate hemolysis)
→Aplastic (low RBC production--damage to bone marrow)
What is jaundice?
Yellowing of the skin of a newborn, caused by hyperbilirubinaemia (i.e. too much bilirubin)→reversed by urinary excretion
What major importance do platelets serve?
Blood clotting!
Prostacyclin→paracrine/autocrine function in the endothelial cell lining to keep platelets soluble
→Injury to endothelial cells exposes collagen and activates platelets to aggregate (prostacyclin production is reduced)
→Serotonin (5-HT), ADP, thromboxane A2 released (potent vasoconstrictors to minimize blood loss)
What is the sequence of the clotting cascade that maintains hemostasis?
Factors 1→X111
Prothrombin
Thrombin
Fibrinogen
Fibrin (protein that causes the clot)
What are the 3 types of polymorphonuclear granulocytes (PMN's)?
Neutrophils
→make up 50-70% of WBC's
→neutralize foreign substances
Eosinophils
→destroy invading parasites & cells
Basophils
→form mast cells, release histamine, mediate allergic response & inflammation
What are monocytes?
WBC's
→differentiate into macrophages ("big eaters"--digest invaders)
→Antigen presentation
Give 3 examples of lymphocytes.
→B cells
→T cells
→natural killer cells
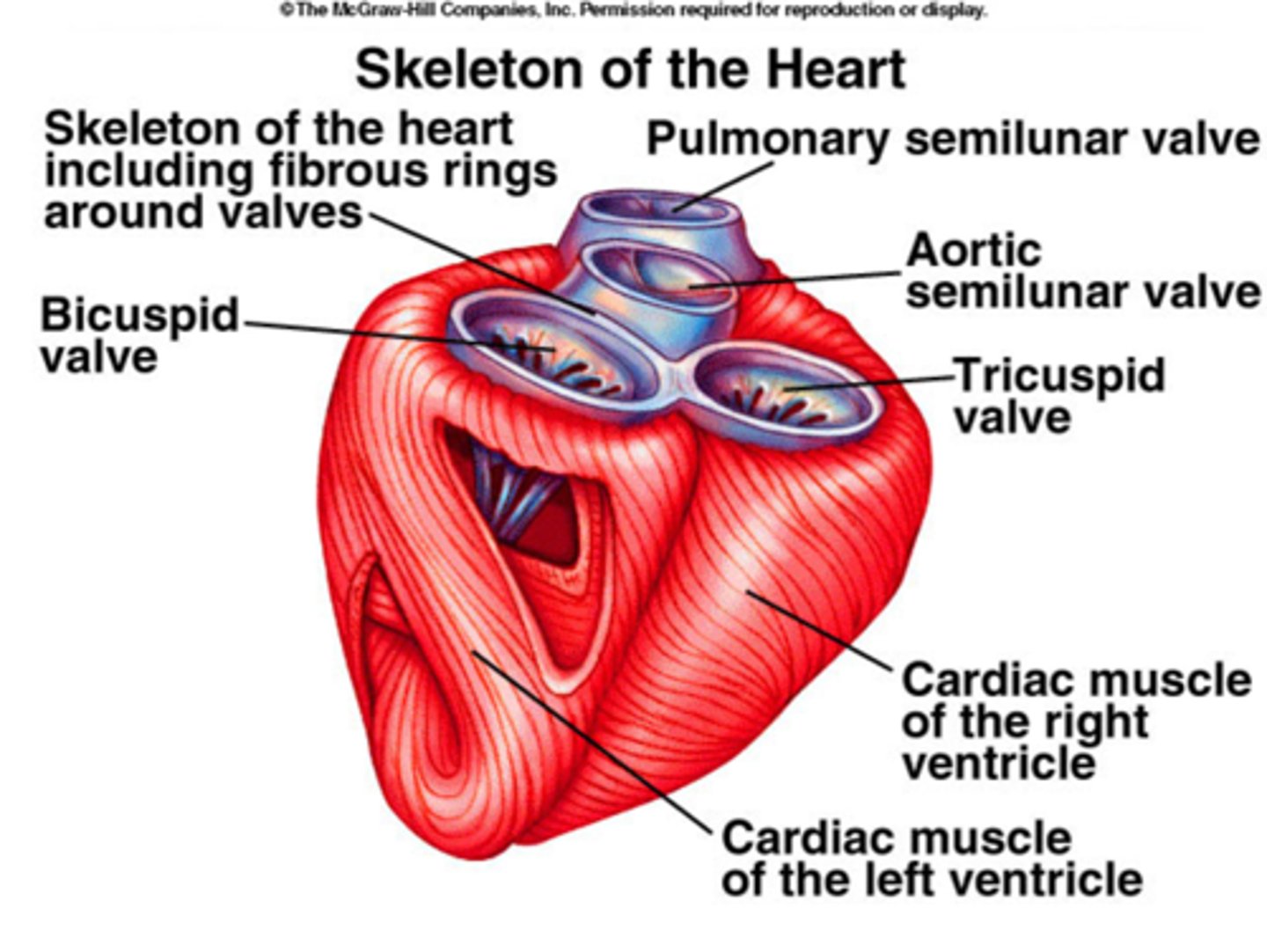
Describe the flow of blood through the heart.
Right atrium
→tricuspid valve
→right ventricle
→pumonary valve
→left atrium
→bicuspid valve
→left ventricle
→aortic valve
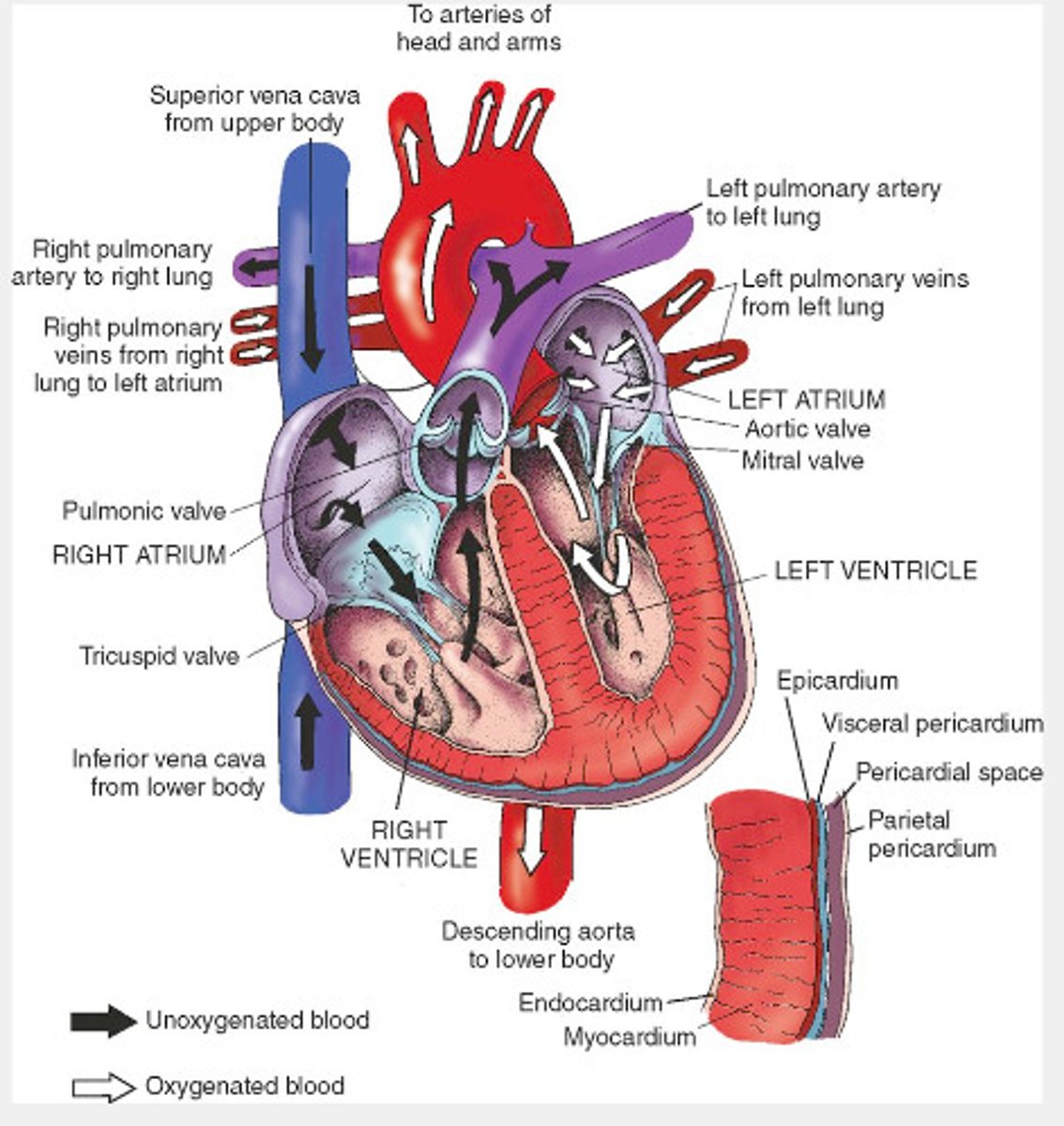
In basic terms, what is the annulus fibrosus?
Tissue around the atria and ventricles that is important for insulation between the atria and ventricles
Describe the structure of the ventricular wall.
Endocardium→inner lining, lined by endothelial cells
Myocardium→middle layer, 95% cardiomyocytes by mass
Epicardium→outer layer

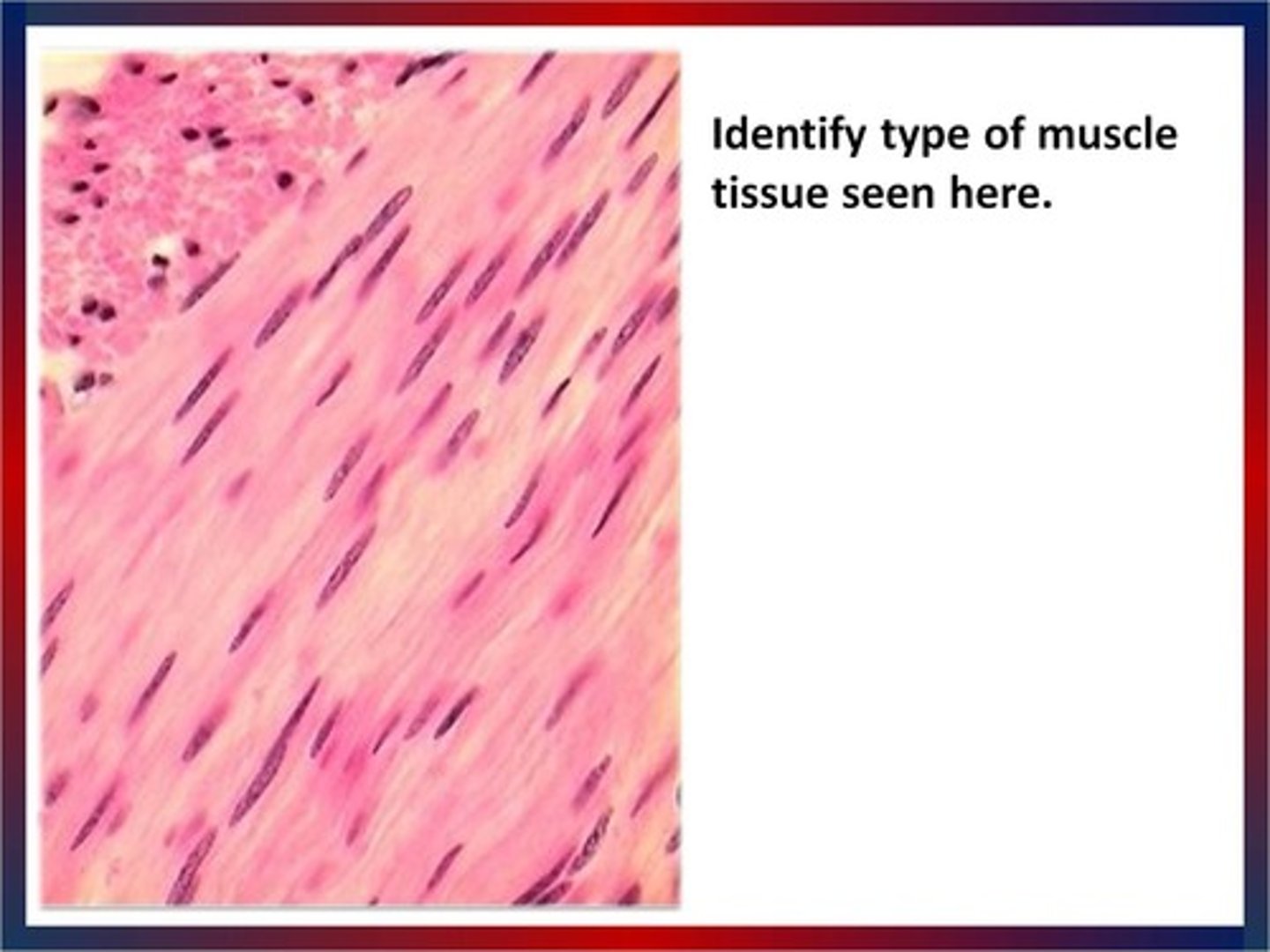
What is the size and general shape of an adult cardiomyocyte?
120-150 µm long
10-20 µm wide
Rectangular shape
*Irreplaceable, do not regrow
What are 2 deviations with pathology/exercise to cardiomyocytes?
Pressure Overload (ex. hypertension or weight lifting)
→increased cell width 2-3 fold
→more parallel contractile units
Volume Overload (ex. valve failure [mitral valve fails & allows some blood to return; heart has to pump more blood than it needs to] or aerobic exercise)
→increased cell length up to 10-20%
→stretching contractile units
What is the:
Z-line
I-band
A-band
H-zone/band
M-line
Z-line
→forms sarcomere boundary
→thin actin filaments run through
→contains α-actin
I-band
→decreases with contraction
→increases with relaxation
→contains actin filaments
A-band
→contains thick myosin filaments
→doesn't change with contraction
H-zone/band
→centre of A band (myosin)
→no overlapping think filaments (no actin)
M-line
→attachment for myosin
What are the 7 cardiomyocyte structural elements?
1. Contractile elements
→50% of cell volume
2. T-tubules
→align with Z-lines
3. Mitochondria
→30-35% cell volume
→subsarcolemmal/intermyofibrillar
4. Sarcoplasmic reticulum
→repository for Ca²⁺
5. Nucleus
→mono or binucleated (cardiomyocyte is much smaller than skeletal muscle cell)
6. Golgi
7. Ribosomes
What are 3 ways in which cardiomyocytes are coupled?
1. Myocyte branching
→provides longitudinal and diagonal coupling
→coupled at intercalated disks
2. Macula adherens or desmosomes
→cytoskeletal proteins
→physical coupling
3. Gap junction or nexus
→connexions
→electrical coupling
→create a functional syncytium
*Physical connections is key to cardiac muscle function; when 1 cell contracts, the next cell also contracts
What is a functional syncytium?
Gap junctions:
→2 connexons per gap junction
→a connexon is a hexamer of six connexions
→Regulated permeability (ex. by acidosis)
*Desmosomes pull the cells together and they all contract together
Compare titin and nebulin.
Titin:
→from M-line to Z-line (half sarcomere)
→the largest known protein: ~30,000 amino acids
→acts like a spring
→→stabilizes position of contractile elements; returns stretched muscle to resting length
Nebulin:
→from Z-line to thin filament ends
→aligns thin filament (stabilizes the actin filament
Describe the components of thick filaments.
Actin filaments:
→helical
→13 molecules per turn
Tropomyosin:
→lies near actin groove
Troponin (Tn) complex:
→TnT = Tropomyosin binding
→TnC = Ca²⁺ binding
→TnI = Inhibitory
Describe the structure of Troponin C.
Troponin C has four Ca²⁺ binding sites:
Site I→ dysfunctional in cardiac muscle
Site II→ binds Ca²⁺ to initiate contraction
Site III & IV→ high affinity
→ always occupied
*Not regulatory sites that control contraction; have a structural role
What is the troponin complex? What is the role of tropomyosin in this complex?
Tropomyosin:
→lies near actin groove
→interferes with myosin binding
Troponin complex:
→TnT binds tropomyosin
→TnC binds calcium
→TnI binds actin
How does Calcium binding to TnC initiate contraction?
-↑ Ca²⁺
-Ca²⁺ binds TnC
-TnI and tropomyosin move
-Exposes myosin binding site
-Crossbridge cycling
-Contraction
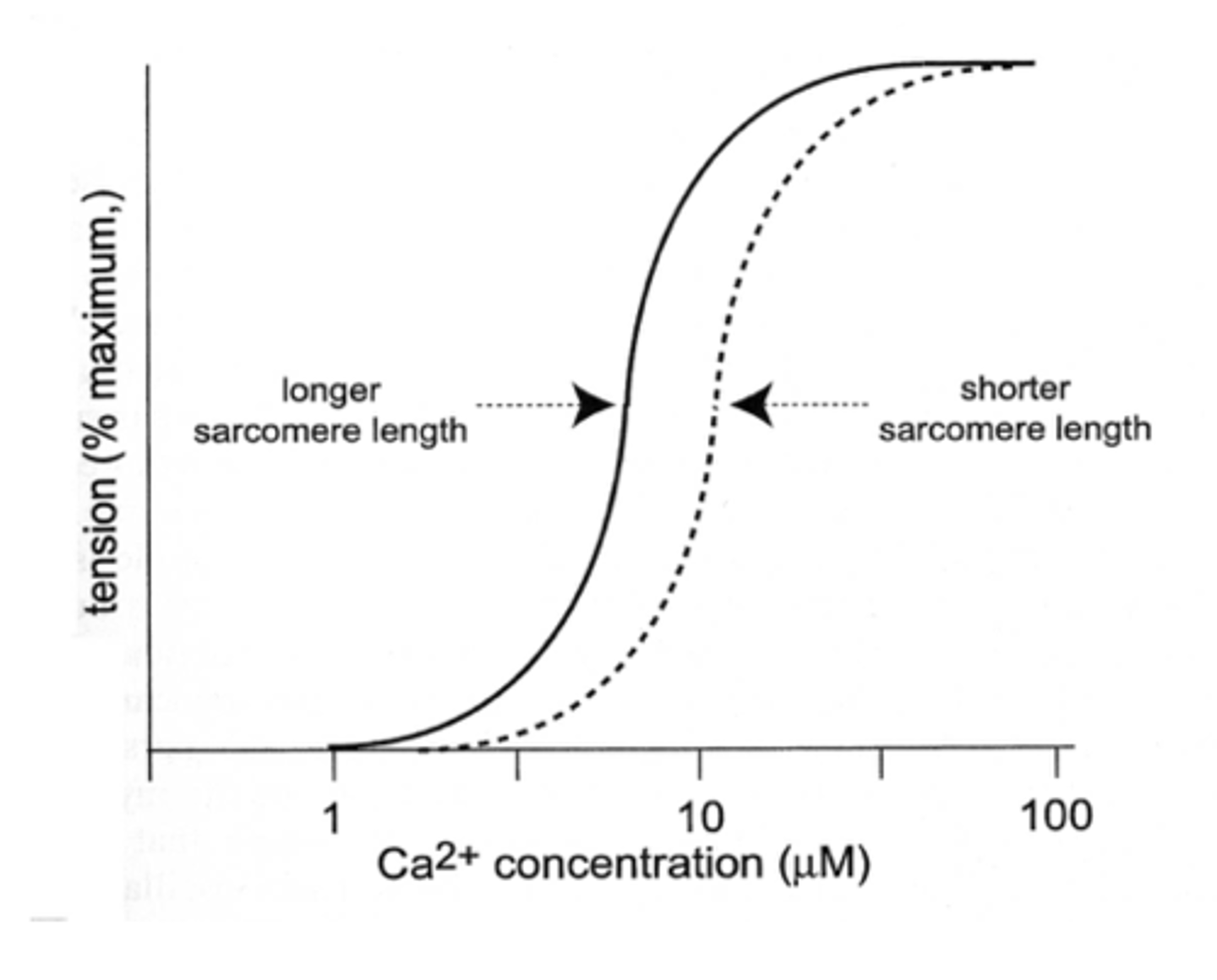
What is the calcium tension relationship?
Tension or force= occupancy of Site II on TnC, reorganization of troponin and tropomyosin, cross-bridge formation
What two kinds of chains make up the thick filament?
Heavy Chains:
→2 chains form coiled helix
→tail and 2 heads; Heads= S1, Binding sites= actin/ATP
Light Chains:
*can alter heavy chain function
→2 pairs
→Regulatory of phosphorylatable
→Essential or alkali (structural role)
Describe the variations in heavy chains in the thick filament.
Heavy Chains:
→α or β isoforms
→so we can have: α-α; α-β, or β-β
→different rates of ATP breakdown
→different rates of contraction
α-α = V1 Fastest
α-β = V2 ↑Thyroxine
β-β = V3 Slowest
*Isoforms are malleable, can change gene expression (ex. hyperthyroid)
Compare preload and after load.
Preload= a load that is place on the muscle BEFORE it contracts
→in the heart, this is the volume of blood in the heart before the heart contracts, i.e.. END DIASTOLIC VOLUME
Afterload= a load that the muscle only see's AFTER it starts to contract
→in the heart, this is the blood pressure
*Hypertension increases after load and causes a change in function
What potent regulator in the force of contraction in the heart greatly affects the length-tension relationship?
Preload!
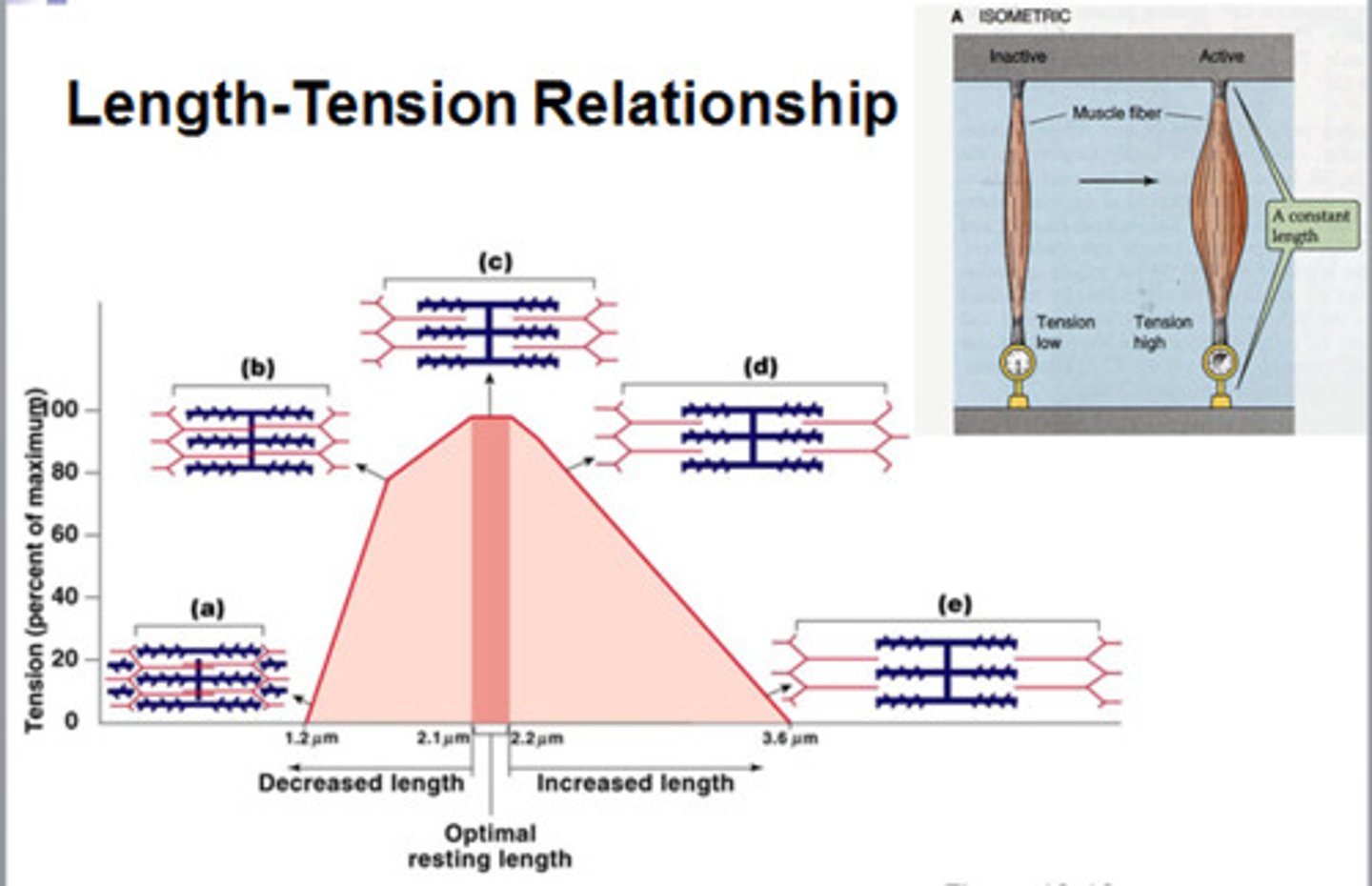
Describe the length-tension relationship of muscle.
If the muscle is too short, the actin filaments bump into each other and cannot generate as much force.
If the muscle is too long, the actin cannot reach the appropriate myosin binding sites and cannot generate optimum force.
*Length-tension relation is ACTIVE because of how length changes with contraction
What is the Frank-Starling mechanism?
Compares stroke volume and EDV. This is a complex mechanism in which force is increased by stretch; inflow must match outflow. The graph is missing the descending part of the curve because the heart has really well developed mechanisms to deal with this.
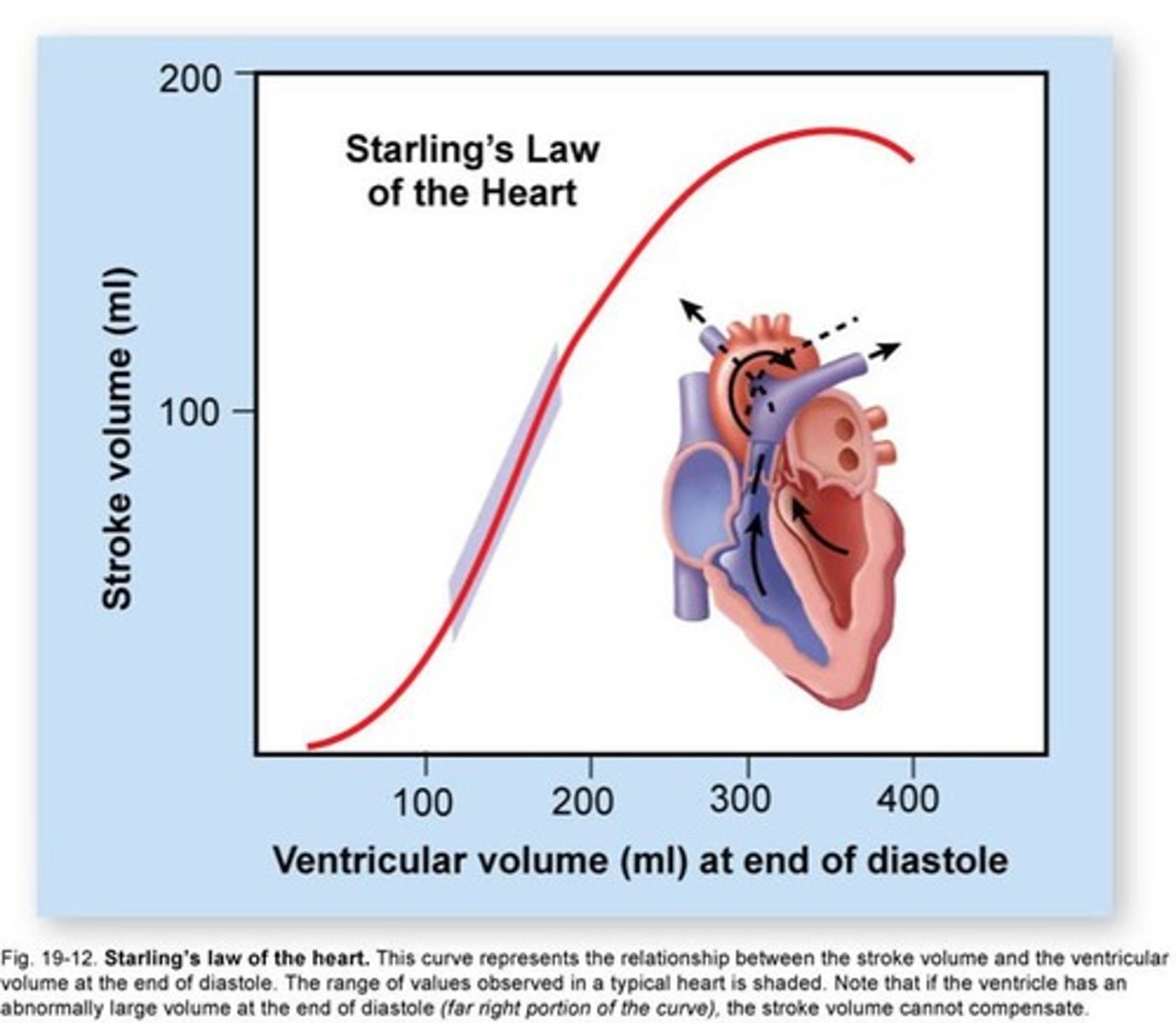
What are 5 factors that can affect the Frank-Starling mechanism?
1. ↑ overlap of actin and myosin
2. ↑ myofilament Ca²⁺ sensitivity (troponin C sensitivity goes up)
3. ↑ SR Ca²⁺ release
4. Geometric changes (stretching makes the sarcomere flatter, actin and myosin are then closer together & more likely to interact with one another)
5. Stretch activated ion channels increase cell Ca²⁺
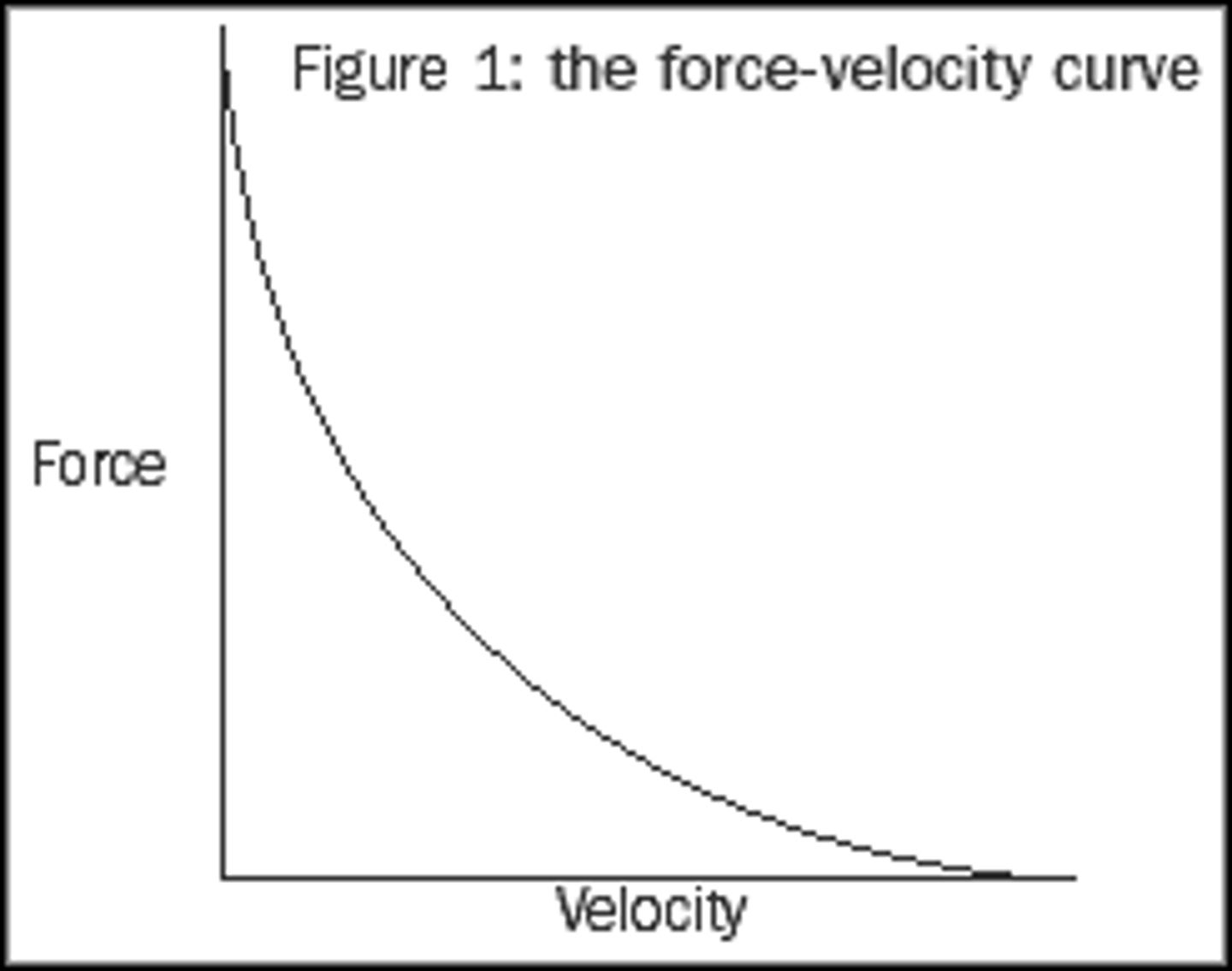
Describe the force-velocity curve.
The the top is Vmax--occurs with zero load (never really happens)
The bottom is Fmax--occurs with zero velocity (isometric contraction), ie. isovolumetric contraction phase of the heart.
The middle is isotonic.
What is Ohms Law?
V = IR
In physiology,
I = VG (Current = Voltage * Conductance)
What are the forces that act on an ion when it moves?
1)Electrical gradient
2) Concentration gradient
=Electrochemical gradient
What is the nernst equation? What does it describe?
The nernst equation dictates the equilibrium potential
Eκ = 60 x log₁₀[K⁺]out/[K⁺]in
~-90mV is a typical equilibrium potential
What are the equilibrium potentials for Sodium, Potassium, and Calcium?
Eκ= -90mV
Eℵα= +60mV
E⊂α= changes
+120mV at rest
+90mV during contraction
**Eκ and Eℵα DO NOT change during the action potential
What is the Goldman-Hodgkin-Katz equation? What does it describe?
Describes the nernst equation for each ion and puts them together→Gives you membrane potential.
Membrane Potential= Vm= (Eκ*Gκ) + (Eℵα*Gℵα) + (E⊂α*G⊂α)/Gκ + Gℵα + G⊂α
G = conductance
In general, what does the GHK equation say about membrane potential and equilibrium potential?
The membrane potential is closest to the equilibrium potential of the ion that permeates the membrane most freely.
If K⁺ permeates, then Em is close to Eκ
If Na⁺ permeates, the Em moves closer to Eℵα
Give an overview of membrane potential: what it is determined by, resting membrane potential, and depolarization.
Membrane potential is determined by the ions passing through it:
→ions follow their electrochemical gradient
→the conductance for an ion depends on: whether ion channels are open, many are voltage gated
Resting membrane potential:
→at rest K⁺=conductance is highest
→ions crossing the membrane are K⁺ ions
→membrane potential is close to Eκ=~-80mV
Depolarization (Upstroke):
→depolarization= Na⁺ channels open
→ions crossing the membrane are Na⁺ ions
→membrane potential moves toward Eℵα (~+65mV)=+30mV
What is the typical shape of the cardiac action potential?
Compare tension regulation in skeletal muscle and cardiac muscle.
Skeletal Muscle:
1) Variable recruitment of muscle fibres
→CNS recruitment α-motorneurons
2)Frequency-dependence
→Summation→→tetanus
Cardiac Muscle:
1) 100% recruitment occurs with every beat
2) No tetany (due to long AP duration)
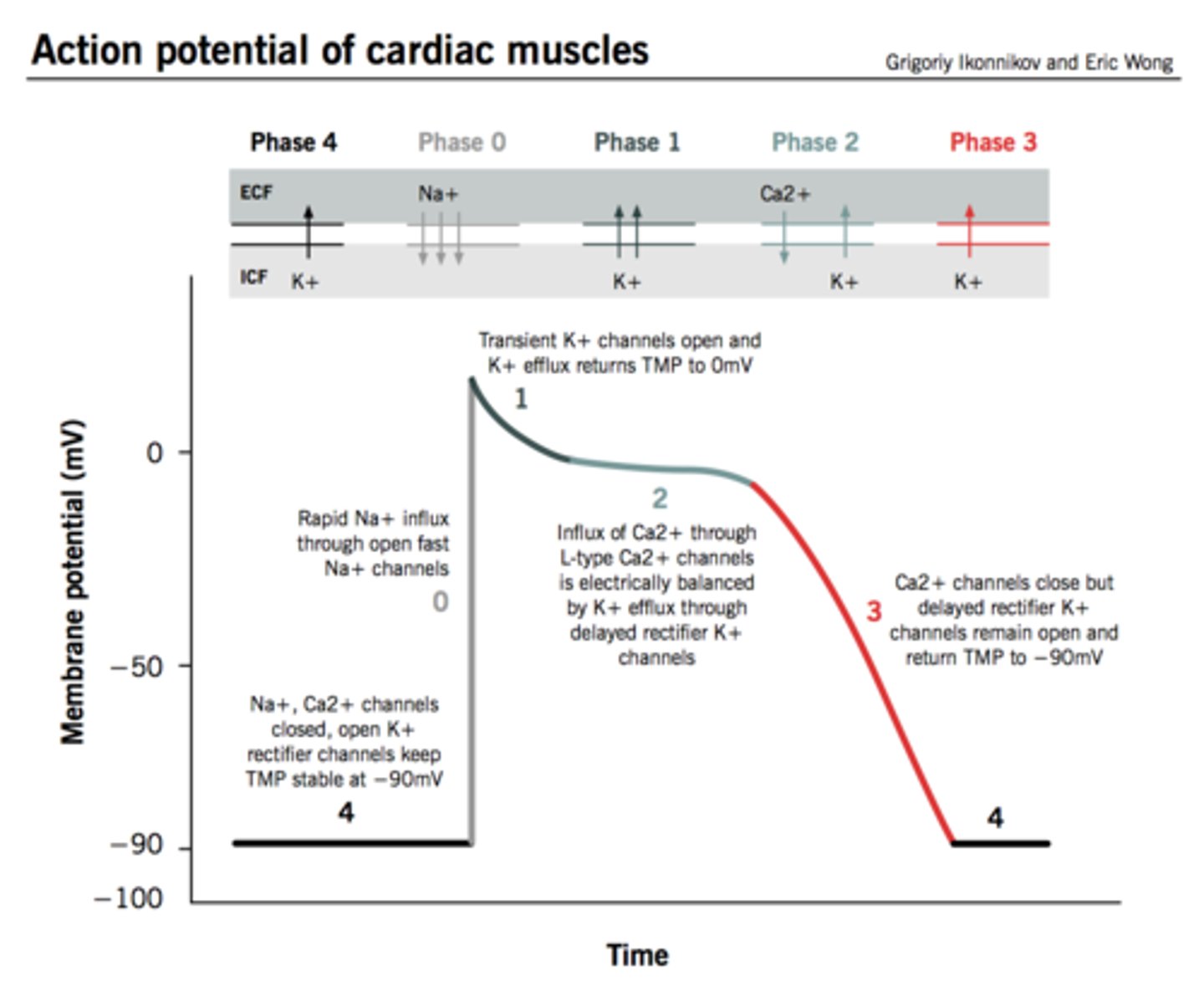
Describe the stages of the cardiac ventricular action potential in order.
4) Resting membrane potential K⁺ current, Iκ₁
→not voltage gated, causes current even at rest
0)Depolarization
→Na⁺ channels open, Iℵα
→Opening threshold ~-55mV
→Sensitive to tetrodotoxin (TTX) [skeletal muscle becomes paralyzed, specifically the diaphragm]
1) Rapid repolarization
→Transient (passive) outward K⁺ current, Iκ,to
2)Plateau Phase
→Unique to cardiac muscle
→Prolongs the AP
→Variable duration; can be different even in the same region of the heart (**Key point in regulation of contraction)
Main currents:
I⊂α--Ca²⁺ entry depolarizes
I(NCX)-- 3Na⁺ in/1 Ca²⁺ out
3)Repolarization phase
→Another K⁺ current:
Iκ,dr--delayed rectifier
What effects does the drug "diltiazem" have on calcium and action potential duration in the heart?
When you increase the dosage of the drug, you decrease the action potential because you have less calcium and the force of contraction therefore decreases.
↓ depolarizing Ica
↓ AP duration
↓ Ca²⁺ entry
↓ force of contraction
What is ion conductance?
How many ions flow across the membrane at a particular time.
What are the 3 main cardiac potassium currents?
1) Transient outward current, I(k,to)
→Rapid early repolarization
→Phase 1
2) Inward rectifier, I(k1)
→Resting membrane potential and long plateau (contribution by absence in plateau phase)
3) Delayed rectifier, I(k,DR)
What does the term "rectification" refer to?
Conductance of ions through a channel is greater in one direction than the other
What are the 3 currents that make up the delayed rectifier current, I(k,DR)?
1) Slow delayed rectifier - I(ks)
→Involved in QT syndrome, leading cause of cardiac death
2) Rapid delayed rectifier - I(kr)
→Faster than slow delayed rectifier but slower than the sodium channels
3) Ultra-rapid delayed rectifier - I(kur)
→Fastest of the delayed rectifier currents but still slower than the sodium channels
Compare inward vs. outward delayed rectifier channels.
Inward:
Passes inward current more easily than outward. Physiologically, outward current is more important.
Outward:
Only passes current in this direction. "Delayed" because slower than Iℵα. Includes Iκs, Iκr, Iκur
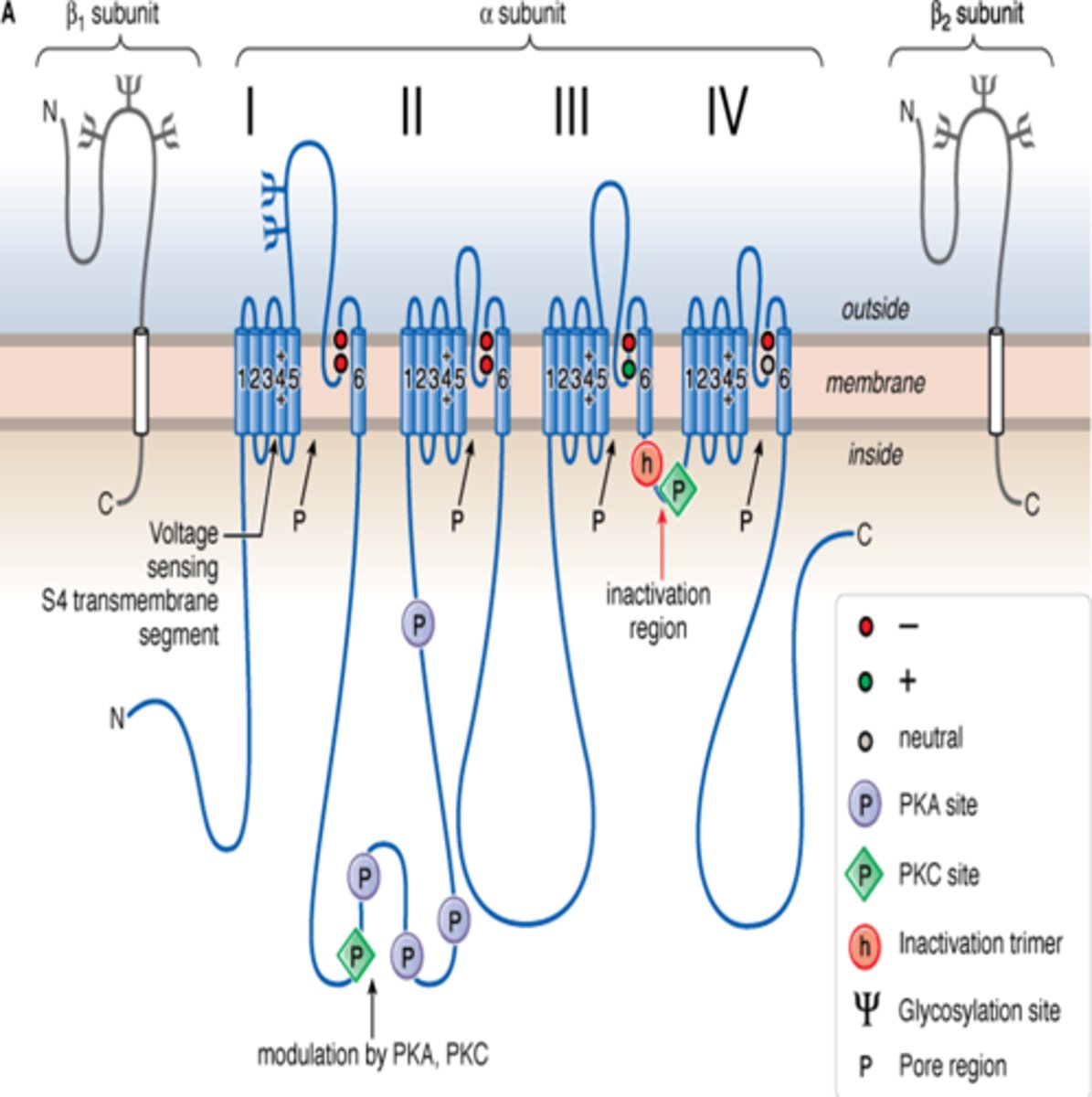
Briefly describe the structure of an ion channel.
Composed of 6, transmembrane spanning proteins. Pore is between protein 5 & 6. Protein 4 is the voltage sensor.
More diversity in K⁺ channels because you have 4 separate parts that come together to make the are not physically connected the way that Na⁺ channels are (has lips that are the selectivity filter--chooses what goes through)
What are the auxillary subunits on sodium and potassium channels?
*Diagram is for Na⁺ channel
Sodium channels have an α subunit which is the main channel, and 2 β subunits.
K⁺ channels have 4 α subunits and 1 β subunit.
→α subunits are the channel, β subunits regulate the channel function.
What are the auxillary subunits on calcium channels?
β subunit
γ subunit
α₂-δ subunit (joined by S-S bond)
Compare the absolute refractory period and the relative refractory period.
Absolute Refractory Period:
→A second response is not possible regardless of strength or duration of the stimulus
Relative Refractory Period:
→A second response can be elicited, but at a greater "cost" (ie. strength and/or duration)
What are the 3 determinants of AP propagation?
1. Difference in voltage between cells
2. Resistance between cells
3. Threshold for AP firing
What is a pacemaker channel?
Sets the pace of the heart.
→Structure like a K⁺ channel
→A non-selective cation channel
→Gated by cAMP
→Called HCN channel (hyperpolarization activated cyclic nucleotide gated channel)
Where does the electrical excitation for a heart beat start and how does it spread?
Sino-atrial node fires an action potential and spreads a wave of depolarization through the atria fairly uniformly, then funnels into the AV node (gateway into the ventricles)
How does a sino-atrial node action potential compare to a basic action potential?
1) Slower upstroke velocity (don't have very many sodium channels in the SA node, Ca²⁺ channels are responsible for causing the depolarization)--lack of Na⁺ channels, depolarized by I⊂α
2) Reduced plateau duration--I⊂α inactivation after upstroke
3) Diastolic depolarization ("don't have a resting membrane potential")--due to pacemaking HCN channel
4) Higher "resting" potential (never get down to -85mV, sits at around -60mV)--lack Iκ₁-important for RMP
Describe the HCN channel.
→Looks like a K⁺ channel, but it passes two different ions (K⁺ and Na⁺).
→K⁺ doesn't really flow during the action potential because the channels are closed however Na⁺ does
→Depolarization will actually close these channels, they open in response to hyperpolarization
What two things is the SA node AP missing?
1. Strong inward rectifier (Iκ₁)
2. Na⁺ channel
How do sympathetic and parasympathetic stimulation affect heart rate?
Sympathetic Stimulation→ ↑ diasoltic depolarization slope= ↑ AP frequency
Parasympathetic Stimulation→ ↓ diastolic depolarization slope= ↓ AP frequency
Describe cAMP gating of HCN channels under sympathetic nervous system control.
Noradrenaline binds to β1 adrenergic receptor
→Activates Gs protein
→Adenylyl cyclase levels increase which causes the conversion of ATP to generate cAMP
cAMP alters the HCN channels and causes them to be more likely to be open and pass more current
*Causes faster diastolic depolarization (↑ HR)
Describe cAMP gating to HCN channels under parasympathetic nervous system control.
Acetylcholine binds to m2 muscarinic receptor
→Activated Gi
→Reduced levels of adenylyl cyclase which reduces the production of cAMP from ATP
→Since cAMP is low, there is little opening of HCN channels and L-type Ca²⁺ channels
*Slower diastolic depolarization (↓ HR)
What are some specialized features of the AV node?
1. Smaller cells
2. Fewer gap junctions
3. Slower intrinsic diastolic depolarization rate
4. More negative Em
What is Wolff-Parkinson-White?
Small gap in the annulus fibrosis (insulation layer) that allows for pre-excitation of the ventricles.
→Accessory AVN pathway
→Delta waves show in an ECG (means that ventricles are being activated by this new pathway, and then again in the normal pathways)
→Causes sudden death
→Seen most often in young people and young athletes
Briefly list the delays in the conduction pathway of the heart.
AVN→bundle of His: 130ms
Bundle of His→apex: 30ms
Endocardium→Epicardium: 30ms
*AV node has created a delay of 160ms, institutes delay in contraction of ventricles
How do Purkinje fibres conduct action potentials so quickly?
→Wider diameter (low resistance)
→Large numbers of gap junctions (low resistance)
Describe briefly what is happening in each stage of an ECG.
P wave→ atrial depolarization
P-Q Segment→ delay in AVN for ventricular filling
QRS Complex→ ventricular depolarization
S-T Segment→ all regions of the ventricle are at the same depolarization
T wave→ repolarization of the ventricles
Why is the T wave bigger than the P wave in an ECG?
T wave is bigger because the ventricles are bigger than the atria
What is the significance of a U wave in an ECG recording?
U wave is not always present and it not universally agreed upon in terms of what it is representing.
→Probably representing repolarization of the bundle branches
Does depolarization occur in the epicardium or endocardium first? Why?
→Depolarization occurs earlier in the endocardium than the epicardium
→Prevents action potentials from cycling within the ventricles
What does an ECG measure? What are the basic conventions?
→ECG measures movement of a positive charge = propagating depolarization
→Upwards deflection = movement of positive charge TOWARDS the electrode (on the surface of the skin)
→Downwards deflection = movement of positive change AWAY from the electrode
→Recording electrode is represented by + (does not mean it has a positive charge, just means it is a recording electrode....opposed to a reference electrode (-))
Why is ventricular repolarization a positive deflection?
Current flow is still towards the electrode so you have a positive deflection on the ECG (depolarization occurs from endocardium→epicardium)
What are the advantages of ECG?
→Simple and cheap
→Information about:
-anatomical orientation of heart (axis)
-Chamber sizes (hypertrophy)
-Arrhythmias and conduction blocks (heart beats are missing)
-Myocardial ischemia (degree and location, ie. insufficient blood supply to a location of the heart)
-Myocardial infarction (heart attack-complete cessation of blood flow through region of myocardium
-Congenital defects
-Changes in cardiac function with time/therapy
How many electrodes do you need for a 12 lead ECG? Where are they located?
12 lead ECG- 10 electrodes
Bipolar leads:
→3 bipolar limb leads
Unipolar leads:
→3 augmented voltage limb leads
→6 precordial or "chest" leads
Reference electrode (on right leg)
What are the 3 standard bipolar leads?
Lead I: Right arm -ve → Left arm +ve
Lead II: Right arm -ve → Left leg +ve
*Lead II views conducting system
Lead III: Left arm -ve → Left leg +ve
*All three together create Einthoven's triangle
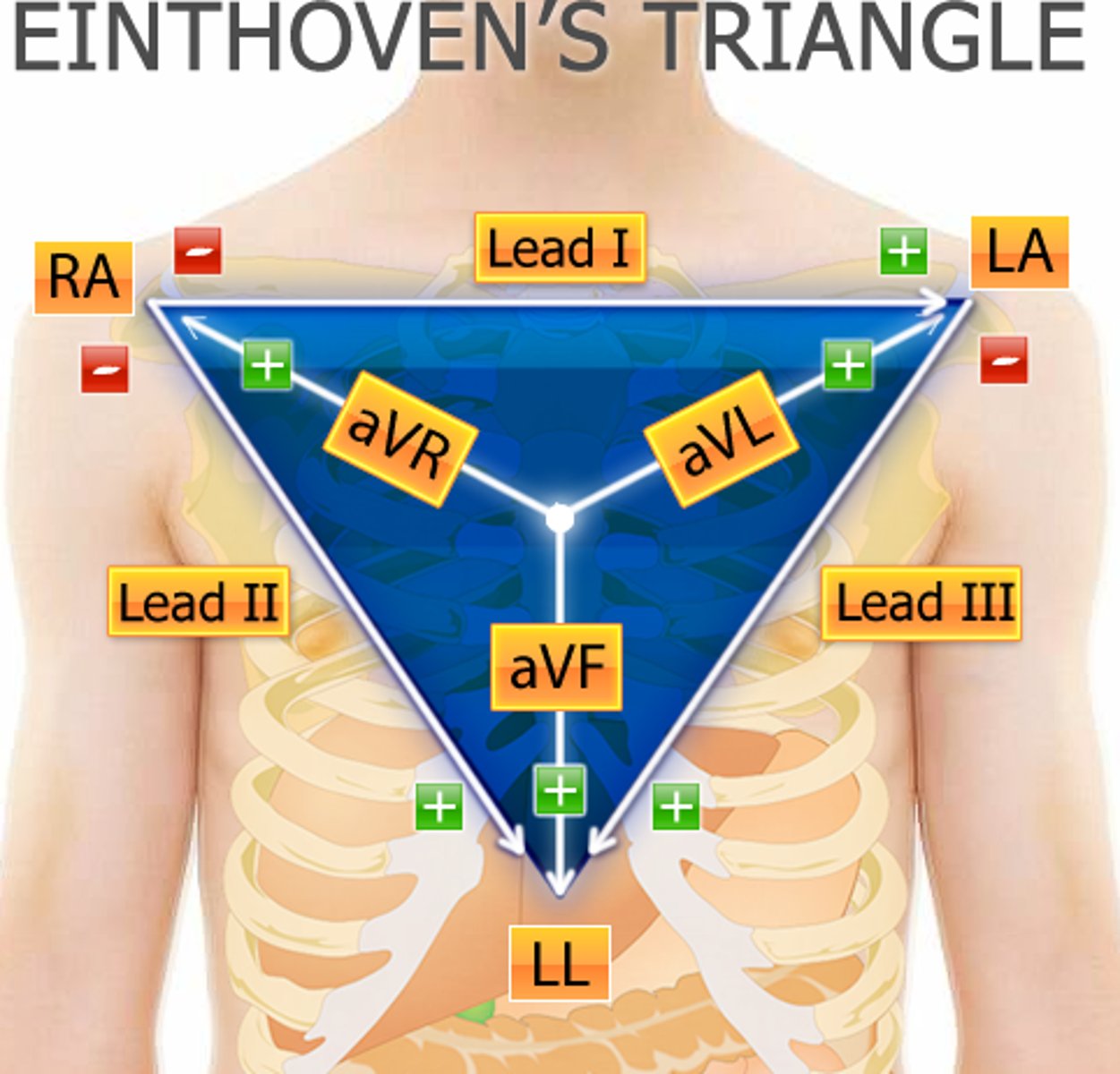
What is Einthoven's law? What does it mean?
Einthoven's Law: I + III = II
→The magnitude of the deflection in lead I plus the magnitude of the deflection in lead III, will equal the deflection in lead II
What are the 3 unipolar "augmented" leads?
Unipolar leads - augmented Voltage (aV)
aVR: right arm
aVL: left arm
aVF: left leg (foot)
Where are the 6 precordial or "chest" leads?
V1 and V2: septal
V3 and V4: anterior
V5 and V6: lateral
List the names of the leads placed on the frontal plane and transverse plane of the body in a standard 12 lead ECG.
Frontal Plane:
→Lead I, Lead II, Lead III, aVL, aVR, aVF
Transverse Plane: V1, V2, V3, V4, V5, V6
*Nothing is on the posterior side in a standard ECG, however you can put electrodes on the back if you need to
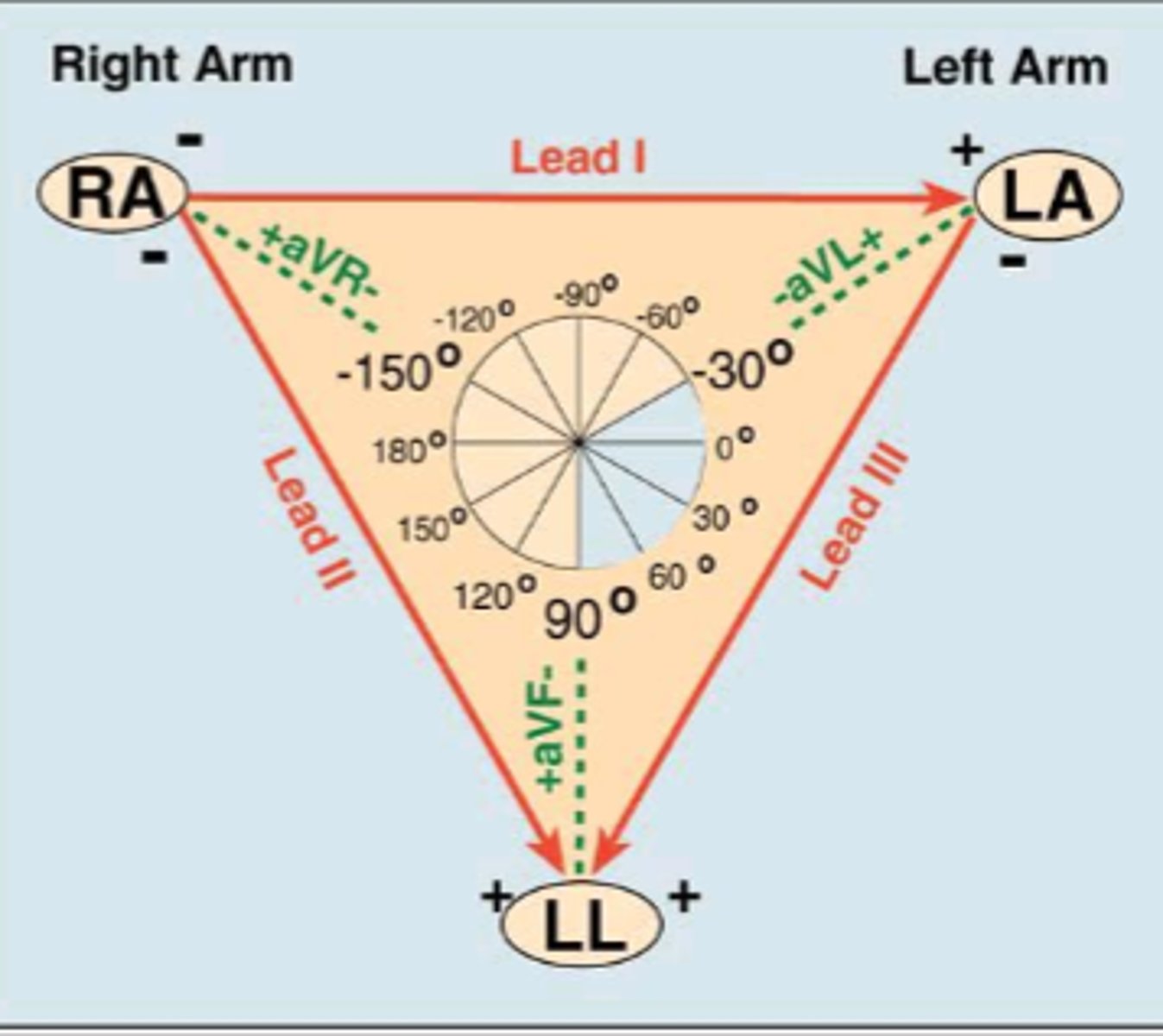
What does an individual lead show in an ECG circle of axes?
Each lead shows a scalar (1-D) projection in that plane of the 3-D vector (on a circle of axes)
What is the average length of the P-R interval? How is this affected by an AV node block, or a pre excitation?
P-R Interval: 120-200ms (represents ventricular filling delay because of AV node→ exercise ↑'s vagal tone and there is a longer delay)
→An AV node block= longer P-R segment
→Pre excitation (WPW)= short PQ Segment
How long is the QRS complex? How does a bundle branch block affect it?
QRS Complex: <120ms
Bundle branch block (BBB) would show up as a broad QRS complex
How long is the QT interval? What are the issues associated with a long or short QT interval?
QT Interval: 360-440ms
Can have Long QT Syndrome or Short QT Syndrome
In the mean electrical axis for an ECG, what quadrant is the normal axis? What direction are Lead I and aVF going?
Bottom right corner. Lead I and aVF are upright
→Because heart is tilted in that direction in the chest
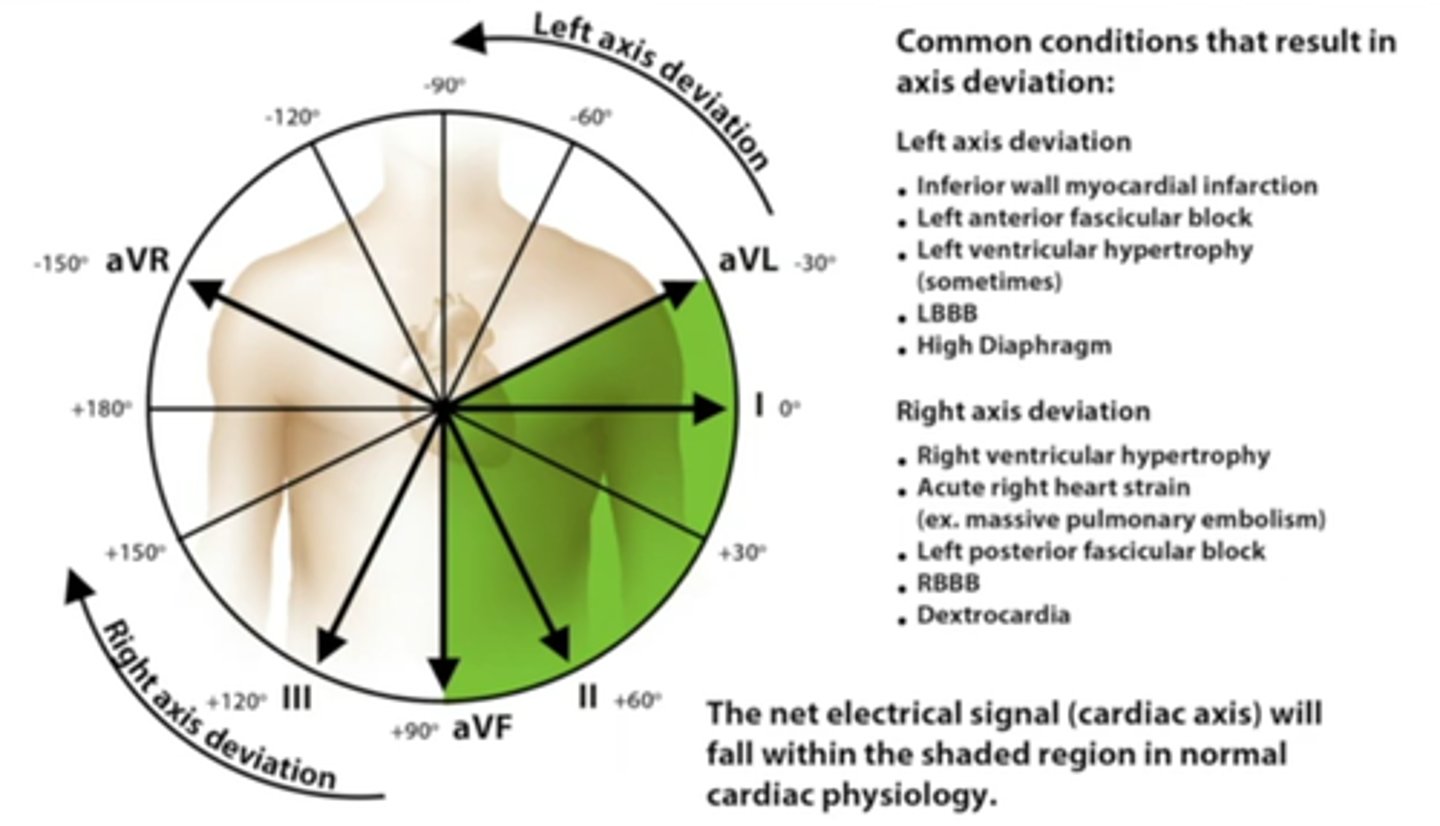
Where do right and left axis deviations show up on a mean electrical axis? What are some causes of each?
Right Axis Deviation:
→ Bottom left quadrant (Lead I is downward and aVF is upright)
→RV hypertrophy
→Infants
→Tall and thin
Left Axis Deviation:
→Top right quadrant (Lead I is upright and aVF is downward)
→Obesity
→Pregnancy
→LV hypertrophy
What is an extreme axis deviation? Why might this occur?
Extreme axis deviation- top left quadrant.
→Depolarizing the ventricles in the opposite direction of normal
→People who have a pacemaker (depolarizing from the apex up)
→When someone has dexicardia (heart is flipped)
How would you go about finding the mean electrical axis using the geometric method?
1) Measure magnitude of QRS
2) Mark on circle of axes, (Ex. +2 units at 60° (lead II) and 1 unit at 30° (negative direction on aVR))
3) Draw two perpendicular lines
4) Connect centre of circle with intersection of two perpendiculars
5) Estimate axis of yellow arrow (ex. about 95°)