Basic wound management
1/25
Earn XP
Description and Tags
SA
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
What are the three phases of normal wound healing?
Lag or inflammatory phase (abt 5d)
Repair phase (abt 6-18d)
Connective tissue repair
Wound contraction
Epithelialisation
Remodelling phase
(Considerable overlap between phases)
List the local factors that effect wound healing?
Wound perfusion
Hypovolaemia, hypotension, vessel injury, pain
Tissue viability
Trauma, dehydration, osmotic injury, envenomation, chemical injury
Wound fluid accumulation
Haematoma or seroma
Infection
Mechanical factors
Tension, motion, pressure
List the systemic factors that affect wound healing?
Immunosuppression
Systemic disease (FIV, hyperadrenocorticism)
Glucocorticoid administration
Neoplasia
Residual disease
Cytotoxic drugs / radiotherapy
Cachexia (metabolic state where breaking down tissue instead of generating new)
What is taken into consideration in order to classify wounds?
Degree of contamination
Aetiology
Location
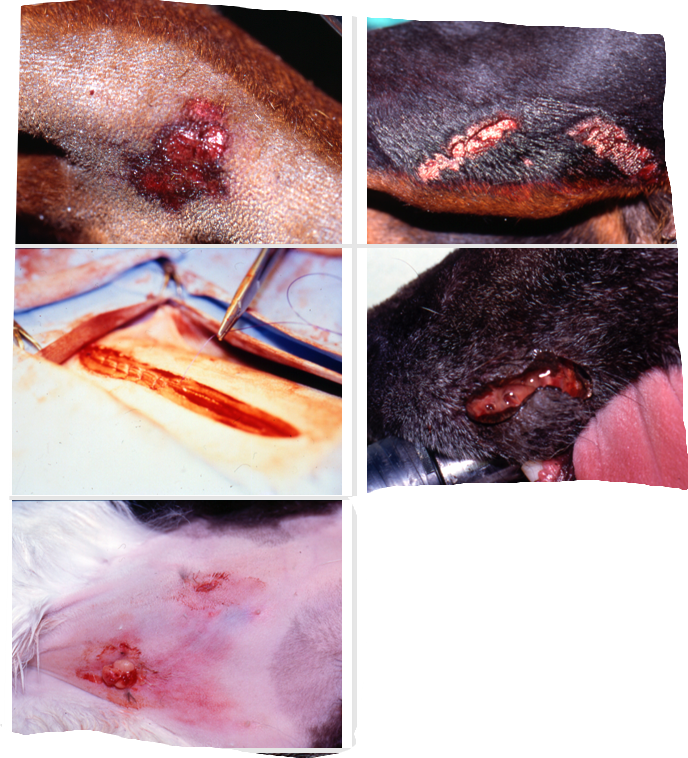
Recall the classification of wounds in terms of degree of contamination

Define
Abrasion
Avulsion
De gloving
Incision
Laceration
Puncture wound
Abrasion: A partial thickness wound with loss of epidermis and part of dermis
Avulsion: Tearing of tissue from its attachments
Degloving injury: Low-velocity avulsion of skin due to rotational forces (typically in road accidents).
Incision: Sharp trauma resulting in a smooth-edged wound with minimal tissue trauma.
Laceration: Sharp trauma resulting in an irregular wound with tearing of tissue and trauma of underlying tissue.
Puncture wound: Penetration by a missile or sharp object. Often minimal superficial damage with substantial damage to deeper structures
How to prepare wound for treatment?
Take swabs for bacteriology before cleaning
Prevent further contamniation by covering with sterile, water soluble gel or sterile saline-soaked swabs
Begin clipping at wound edges and work away (minimises hair contamination)
Can prepare skin with but DO NOT allow surgical scrub to enter wound
Lavage (decrease bacteria + remove debris)
What are the aims of lavage?
Decrease the number of bacteria in the wound
Remove debris
Prevent further contamination
Prevent transformation of acute clean-contaminated or contaminated wounds into infected wounds
Convert contaminated or clean-contaminated wounds into wounds suitable for primary closure
How to carry out pressure irrigation for hydrodynamic debridement (lavage)?
Using a 20ml syringe with an 18g needle
Antiseptics can be added to the final lavage: they must not contain detergent
How does hydromechanical debridement work?
Amorphouse hydrogel dressing (e.g.- Intrasite)
Promote hydration and autolysis of necrotic tissue, absorb sloughing tissue, allow optimum cell migration and proliferation
Contain bacteriostatic propylene gel
(when first take dressing off may appear worse because gel has absorbed pus)
How does surgical debridement work?
Use aseptic technique to avoid further infection
Evaluate viability of issues based on colour, pulse and bleeding
Remove all devitalised tissue and foreign material (scalpel not scissors), preserve important structures for function unless very obviously necrotic and non viable
Lavage again after debridement
What to do if unsure about viability of tissues?
Manage as open wound for 48-72 hours until obvious demarcation of devitalised tissues occur
Immediate debridement is only essential in massive, deep or grossly necrotic wounds that may cause sepsis
After debridement how do we decide and appropriate management technique? List these techniques and what they require
Reassess and recategorise

What is open wound management?
Combines continued debridement by lavage, repeated surgical debridement or use of topical preparations and dressings and protection of the wound to provide an optimum environment for healing
What are the different types of wound closure?
primary closure (clean/clean-contaminated wounds)
delayed primary closure (close partly + daily lavage + debridement)
secondary closure (>5d after injury —> when granulation tissue formed, contaminated/dirty wounds)
Outline open wound management
continued debridement
lavage
surgical
hydromechanical
dressing
protection of wound to provide optimum conditions for healing (dressings)
How many layers are there in a dressing?
3 layers
Primary (contact)
Adherent (no longer standard of care) or Non adherent
Secondary
Tertiary
What does the choice of primary layer depend on?
Desired function
For debridement you would choose nonadherent dressing with hydrogel
For protection of wound and maintenance of optimum enviroment for healing you would you simple non adherent dressing
What factors do you consider when choosing the type of non adherent primary layer?
Amount of exudate production (prevent drying out + allow excess moisture to escape)- more exudate requires more absorbable or permeable dressing
If wound in infected require more frequent dressing changes (at least daily)
What are the classifications of non adherent dressings and what is the aim?
Semi occlusive or occlusive
All aim to allow excess exudate to drain but to keep wound moist
List the types of non adherent dressings and their general features
Calcium alginate
absorb exudate and water on contact with wound surface + become gel
Fenestrate polyester film dressing (Melolin)
Polyester film stops dressing adhering to tissue
Hydrocellular dressings (Allevyn)
Extremely absorbent but do not transmit liquids to secondary layer
Hydrocolloid dressings
Mainly composed of cellulose that absorbs moisture and exudate becomes gel
Polyethylene/polyurethane film dressings
Non-absorben but some pass water vapour into secondary layer
Petrolatum-impregnated gauze
Non absorbent and hydrophobic
Hyperosmolar agents
Honey and home-made sugar dressing which are hyperosmolar and dehydrate bacteria
Maggots
Larvae of lucilia sericata —> efficient debriders + stimulate healing
Silver dressings
release bactericidal silver ions
When is each non adherent dressing used?
Calcium alginate
Wounds at any stage of healing with moderate to heavy exudation
Fenestrate polyester film dressing (Melolin)
Protecting wounds with intact epithelial surface
Hydrocellular dressings (Allevyn)
Surface wounds or cavities
Hydrocolloid dressings
Can handle wide range of exudate volumes
Polyethylene/polyurethane film dressings
Indicated for protection of wounds with an intact epithelial surface
Petrolatum-impregnated gauze
Wounds in later stages of repair because may slow epitheliasation- mainly used for protecting wounds with an intact surface but fragile epidermis
Hyperosmolar agents
Maggots
May be more useful as antibacterial resistance becomes more common
Silver dressings
What are the roles of the secondary layer?
Absorbs excess fluid from wound
Secures primary layer
Obliterates dead space
Protects wound
List some types of secondary layer
Cast padding, disposable nappies, absorbent pads and cotton wool
What are the functions of the tertiary layer?
Secures rest of dressing
Keeps dressing clean and dry
Ensure not too tight
Use sufficient secondary layer
Distribute tension evenly
Estimate pressure manually
Monitor the patient after application
What is commonly used for the tertiary layer?
Gauze bandage (elastic or nonelastic) covered by surgical tape or a self-adhesive elastic bandage e.g. Vetrap