Pharm E2- Ortho/Pain
1/90
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
91 Terms
What is the most reliable indicator of pain?
patient’s description (subjective experience)
What kind of pain is a burning, tingling, or shooting pain sensation caused by nerve damage?
Neuropathic pain
What kind pain is sharp, dull, aching, or throbbing and can be somatic (skin/bone/joint/CT) or visceral (internal organs, mucosal lining)?
Nociceptive pain
What kind of morbidity do half of chronic pain patients experience?
Psychiatric comorbidity
What is the first line therapy for low back pain and OA?
APAP
What drug?
analgesic & antipyretic used for mild-mod pain
no anti-inflammatory properties
more potent centrally; inactivated by peroxides in inflamed tissue
opioid sparing (need fewer opioids to tx pain)
Acetaminophen (APAP)
What is the max dose of Acetaminophen (APAP) a patient can receive per day?
4 g
What SE is seen with APAP?
dose dependent hepatic necrosis
What drugs?
analgesic, antipyretic, & anti-inflammatory
inhibit COX 1 & 2 enzymes; decrease PG synthesis
ex: ibuprofen, naproxen, indomethacin, ketorolac, tolmetin, ASA
NSAIDs
What SEs are seen with NSAIDs?
GI ulcers, bleeding, hypersensitivity rxns, asthma / bronchospasm
prolonged gestation & premature closure of ductus arteriosus
increase liver enzymes & dec renal function
What drug?
salicylate; antiplatelet (irreversible)
nonselective COX 1 & 2 (more dangerous than other NSAIDs)
oral absorption, crosses placenta & breast milk; modified in liver & excreted through kidneys
ASA
What SEs are seen with salicylates (ASA)?
bleeding, GI upset, tinnitus, hypersensitivity, etc
preeclampsia & growth retardation in pregnancy, reye’s syndome
What are contraindications to ASA?
bleeding disorders, pregnancy, children w/ fever associated with viral dz (chicken pox/influenza)
What condition?
fatty liver encephalopathy - vomiting, progressive CNS damage (stupor → convulsions & coma), hepatic injury
hypoglycemia, metabolic acidosis, inc aminotransfersase, ammonia, & prothrombin time
can be seen in children with viral illness who were given ASA
Reye’s Syndrome
What is the treatment for Reye’s syndrome?
glucose and mannitol
What drugs are propionic acid derivatives?
Ibuprofen, Naproxen, Ketoprofen, Fenoprofen, Flurbiprofen, Oxaprozin
What drugs?
category of nonselective NSAIDs
orally absorbed, hepatic conjugation & renal excretion
Less severe GI SEs but more severe renal & hepatic toxicity
high protein binding & more potent
Proprionic acid derivatives
Which propionic acid derivative would be ideal for chronic pain patients due to the long half life of 40-60 hours?
Oxaprozin (Daypro)
What drug?
slowly reversible & noncompetitive NSAID; mos potent CNS & peripheral
closes ductus arteriosus
higher incidence of SEs- GI, HAs, dizzy, hematologic toxicity
decrease effects of diuretics
Indomethacin (Indocin)
What drug?
slowly reversible noncompetitive IV NSAID; less effective anti-inflammatory agent
go to for acute pain
opioid sparing
Ketorolac (Toradol)
What BBW is associated with Ketorolac?
GI effects
How many days should the use of Ketorolac be limited to?
(** Test Q)
5 days
What drug?
analgesic, antipyretic, & anti-inflammatory
more potent than ASA
SEs- GI, anticoagulant effects
Tolmetin (Tolectin)
What drug?
rapidly reversible & competitive NSAID
used to tx arthritis
equipotent to ASA & Naproxen
fewer & mild GI SEs
Piroxicam (Feldene)
What NSAID has a 10 fold selectivity for COX 2 & less GI toxicity?
Meloxicam (Mobic)
What drug?
prodrug & active metabolite used to tx RA & OA pain
some COX 2 seletivity
SE: stomach cramps, diarrhea
Nabumetone (Relafen)
What drug?
anti-inflammatory w/ some COX 2 selectivity used to tx RA pain
topical formula available
SE: bleeding, ulcers
Diclofenac (Voltaren)
What SEs are associated with COX-2 inhibitors (except celecoxib)?
CV events, heart attack, stroke, hypersensitivity & skin rxns
less risk for GI ulcers**
What agents are COX-2 inhibitors?
Etoricoxib, Celecoxib (go to), Etodolac
Valdecoxib & Rofecoxib removed from market
What drugs inhibit PG12 production more than TXA2 production in epithelial cells of blood vessels, increasing the risk for MIs & strokes?
Cox-2 inhibitors
What opioid receptor affects afferent neurons in dorsal spinal cord to inhibit transmission & dec cAMP, & also is associated with analgesia, respiratory depression, & euphoria?
Mu
What term is being described?
occurrence of withdrawal syndrome when stopping opioids (N, V, dysphoria, sweating) that is not fatal & not correlated with addiction
every experiences this if on opioids long enough
Physical dependance
What term is being described?
psychological dependence to opioids
cravings (DA reward system in brain), compulsive & impaired control of drug use
continued use despite known harm/consequences
Addiction
What term is being described?
state of adaptation where drug’s effectiveness diminishes over time
(get used to drug & need more to maintain effectiveness)
Tolerance
What is pseudotolerance?
change in pain state due to increased activity or disease progression, NOT because the meds aren’t working as well
What term is being described?
usually due to undertreatment
can be confused with drug seeking behavior, but behaviors will stop once dose is increased because pain is better
Pseudoaddiction
Pseudoaddiction or addiction?
drug seeking behaviors go away once the dosage is increased
individual regains function
Pseudoaddiction
Pseudoaddiction or addiction?
constant drug seeking behavior, no change with increased dose
individual loses function
Addiction
What is the limit for prescribing opioids for acute pain?
3 days (can extend to 7 days if written “acute pain exemption”)
What is the limit to prescribing opioids for chronic pain?
no refills but can write for total of 90 days with 3 separate scripts (must write “non acute pain”)
What drug?
converted to morphine via CYP2D6 in liver
less potent then morphine; weakest opioid; used for mild-mod pain
CV or CIII**
Codeine (Tylenol #3)
What is the BBW associated with Codeine?
ultra rapid CYP2D6 metabolizing in children w/ T&A (risk resp depression)
What opioid is NOT a CII?
Codeine
How would a patient deficient in CYP2D6 enzyme respond to Codeine?
less effective; more resistance to the dangerous SEs
What drug?
opioid available IV, PO, IR, & ER
hepatic metabolism via glucuronidation
renal excretion (*caution w/ elderly & renal failure pts)
can cause pruritus from significant histamine release
Morphine (MS Contin, Duramorph)
What should be done for a patient who experiences pruritus after receiving morphine?
switch agent or pretreat with antihistamines
What drug?
semisynthetic opioid
converted to hydromorphone (Dilaudid) via CYP2D6
usually in combo w/ APA but can be used alone (Zohydro ER)
frequently #1 prescribed med in US
Hydrocodone (Norco, Lortab)
What drug?
2x as potent as PO morphine bc of improved bioavailability
only PO dosages - long acting (Oxycontin), short acting, or with APAP (Percocet)
metabolized to oxymorphone via P450 2D6
Oxycodone (Roxicodone)
What drug?
metabolized via glucuronidation
very potent but shorter half life than morphine
less histamine please = less pruritus
Hydromorphine (Dilaudid)
What drug?
synthetic opioid 100x more potent than morphine
IV for acute pain or long acting for chronic pain
also TD, TM, IN
Fentanyl (Sublimaze)
What drug is useful for pain patients who have true allergies to phenanthrene opioids (ex- morphine, oxycodone)?
Fentanyl
What drug?
opioid receptor full agonist; NMDA receptor antagonist; inhibit reuptake of NE & 5HT
long acting - 50+ hr half life
not used for breakthrough pain
used for chronic pain & opioid addiction (can prevent withdrawal sx)
multiple conversion ratios
Methadone
What SE is associated with Methadone?
prolong QTc (check elytes & EKG!)
What drug?
metabolized to normeperidine (a toxic metabolite that’s renally cleared)
drug interaction d/t MAO inhibition
pts can develop tolerance quickly
avoid use in elderly & renal imapired (should almost never be used)
Meperidine (Demerol)
What drug can be used for rigors (shivers) in a surgical setting?
Meperidine (Demerol)
What drug?
partial agonist - tight binding affinity at Mu receptors
available SL (37 hr half life), TD, & implant
used in opioid addiction
start once withdrawal sx begin & full agonist out of system (can induce withdrawal if taken w/ full agonist or opioids due to potential to displace from receptor)
Buprenorphine (Suboxone, Subutex)
What should Buprenorphine be compounded with to deter IV abuse (counter reacts & opioids don’t work as well)?
Naloxone
When converting opioids, why would you want to start at 50-75% of the dosage of medication a patient is currently on?
incomplete cross tolerance (not as tolerant to the drug they are switching to, need to work them back up)
What must all opioids be converted to first when switching drugs?
PO morphine
What device provides a continuous hourly infusion (basal rate) of opioids & allows additional dosage when a patient pushes a button?
IV patient controlled analgesia (PCA)
What PCA dosage setting is most effective for persistent pain?
basal rate + on demand dose (1/4-1/3 of basal rate)
What SEs are seen with opioids?
MC: constipation, N, V, sedation, histamine release (pruritus)
LC: delirium, resp Depression, abuse & diversion
What opioid SE would a patient NEVER be able to develop a tolerance to?
Constipation
How can constipation as an SE of opioids be treated (start prophylactically)?
Mush & push - stool softener & stimulant laxative
(fiber, fluid, Senna + Docusate, etc)
What drug?
Mu opioid receptor antagonist - reverse opioid induced resp/CNS depression
crosses BBB
IV, IM, or IN (no oral bioavailability)
fast onset & short half life
can induce withdraw if too much
Naloxone (Narcan)
What drugs?
Mu receptor antagonist - peripherally acting agents
does not cross BBB; works at GI tract for constipation
reverse GI SEs but won’t block analgesic effects on brain
Alvimopan (Entereg)
Methylnaltrexone (Registor)
Naloxegol (Movantik)
What SEs are seen with anti epileptics?
sedation, mental clouding, dizziness, N, unsteadiness
What agents are antiepileptics that can be used to treat neuropathic pain?
Carbamazepine, Gabapentin, Lamotrigine, Pregabalin
What drug blocks the reuptake of NE to modulate pain & is the gold standard for neuropathic pain management?
TCAs
What SEs are seen with TCAs?
anticholinergic, cardiac abnormalities, sexual dysfunction, wt gain
How to local anesthetics work to treat neuropathic pain like in post herpetic neuralgia?
Block neuronal Na channels preventing signal conduction
What are examples of topical local anesthetics used for neuropathic pain?
EMLA cream (lido + prilocaine) & 5% lidocaine patch
What epidural / local anesthetic blocks that are opioid sparing?
Ropivacaine, Bupivacaine
What drugs are skeletal muscle relaxants?
Baclofen (Lioresal)
Cyclobenzaprine (Flexeril)
Metaxalone (Skelaxin)
Methocarbamol (Robaxin)
Tizanidine (Zanaflex)
Carisoprodol (Soma)
How do skeletal muscle relaxants work to treat pain associated with muscle spasms?
agonizes GABA-B receptors centrally & increase Cl- flow
(doesn’t directly inhibit muscles, turns down CNS signal telling them to spasm)
What SEs are associated with muscle relaxants?
drowsiness & sedation (don’t give w/ opioids), dizziness, light headedness, fatigue
What drug?
topical cream for analgesia
have to apply consistently → activates pain fibers to release substance P & desensitizes them once substance P runs out
use for minor aches & pains of muscles/joints, localized neuropathic conditions (postherpetic neuralgia)
Capsaicin
What SEs are associated with Capsaicin?
temporary burning/stinging after application that resolves in few days-wks
lipophilic → stays on hands; with soap and water!
What drug?
partial opioid Mu agonist & weak inhibition of NE & 5HT
use for mod-severe pain
better tolerated than opioids but still abuse potential (Mu binding)
C-IV
combine w/ APAP → Ultracet
Tramadol (Ultram)
What SEs are associated with Tramadol (Ultram)?
dizziness, N, constipation, somnolence
Is Tramadol fully reversible with Naloxone (opioid antagonist)?
No
What is the main psychoactive compound in medical marijuana?
THC
Which cannabinoid receptor is primarily in CNS?
CB1
Which cannabinoid receptor is in peripheral tissues?
CB2
What SEs are associated with medical marijuana?
acute: impaired short term memory, motor coordination, judgement (no driving)
chronic: can affect developing brain (impaired memory, low IQ)
rare: paranoia, psychotic sx
worsen pulm sx (bronchitis, PNA), MI, stroke, PVD possible
What must an appropriate candidate for medical marijuana have?
debilitating metical condition
multiple failed trials of 1st & 2nd line agents
failed FDA approved cannabinoid (dronabinol, nabilone)
no active substance abuse, psychotic disorder, unstable mood/anxiety disorder
Patient presents with 10/10 pain after MVA & needs pain relief but has a morphine allergy (anaphylaxis). What treatment choice do you go with?
(*example test Q)
Fentanyl
Which manifestation of a venous thromboembolism is more likely to be fatal, PE or DVT?
Pulmonary embolism
What are risk factors for venous thromboembolisms (VTE)?
age, previous hx VTE,
venous stasis (obesity/paralysis/immobile),
vascular injury (hip/knee replacement)
hypercoagulable state (factor def, pregnancy)
drugs (estrogen containing)
How do you prevent a VTE?
physical activity, compression, early ambulation after surgery, Unfractionated Heparin / Enoxaparin / Fondaparinux
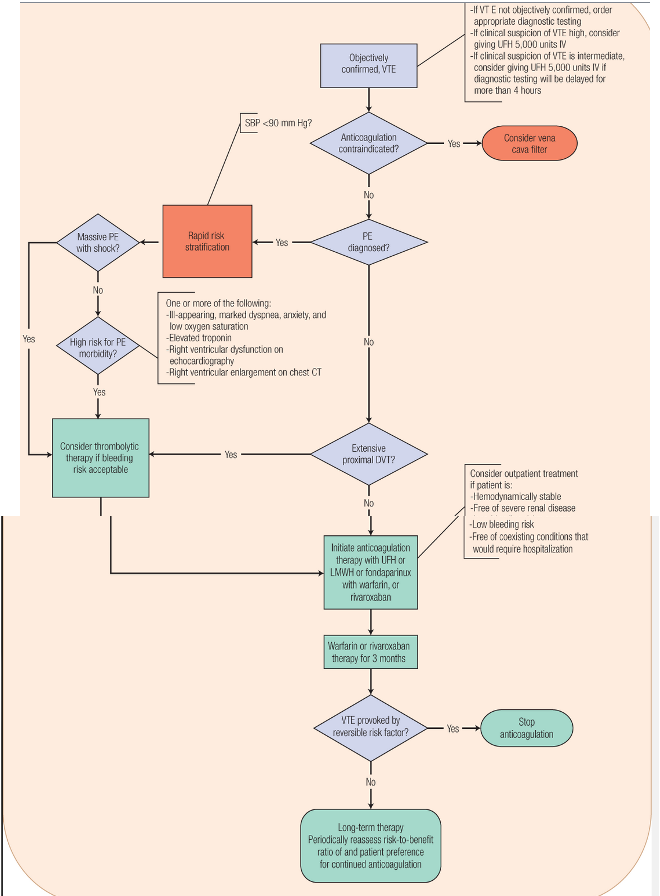
VTE algorithm