chapter 5 (chemical messengers)
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
60 Terms
3 methods of communication for cells:
1-Long distance communication-centers of the body: (it includes 2 systems)
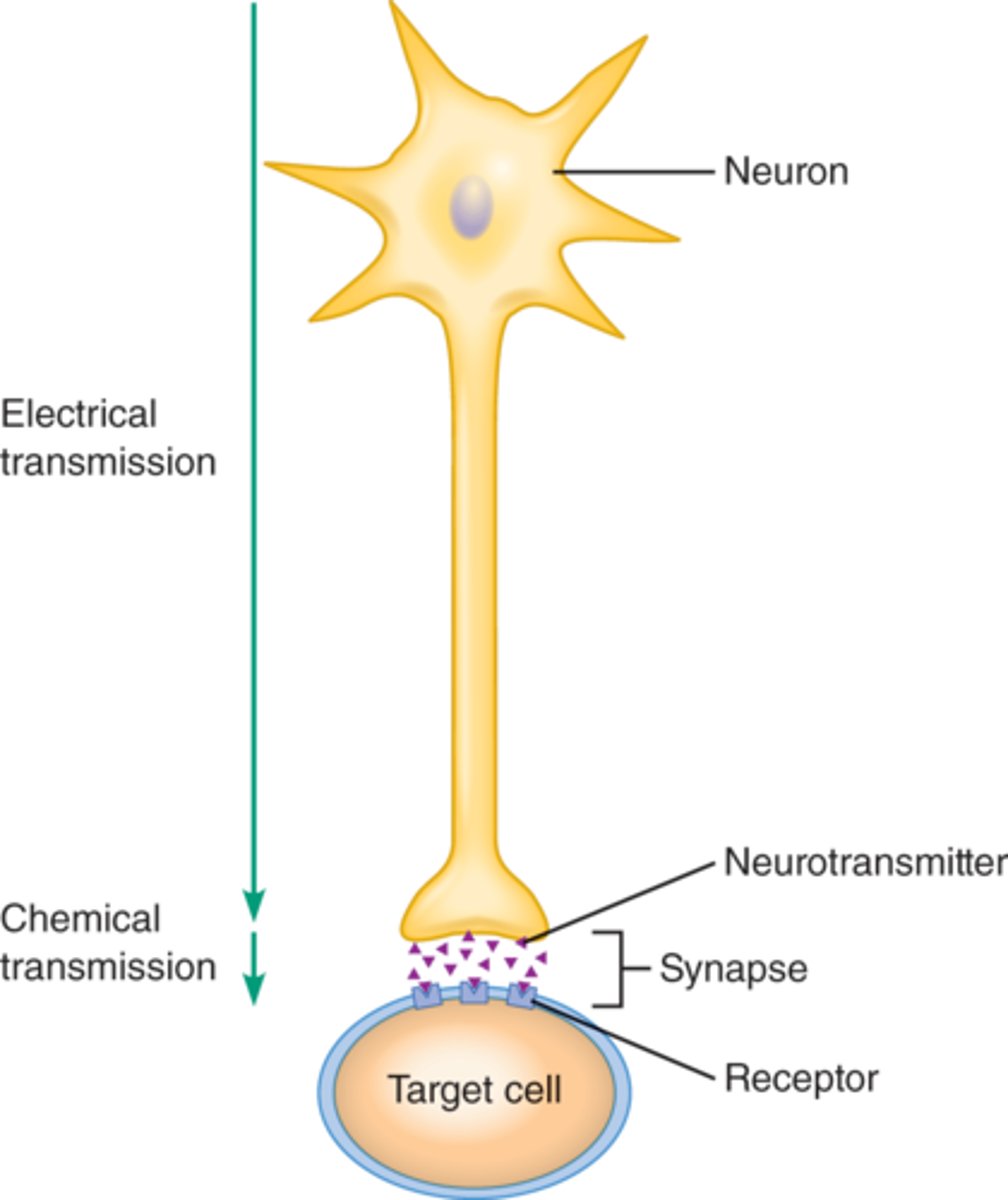
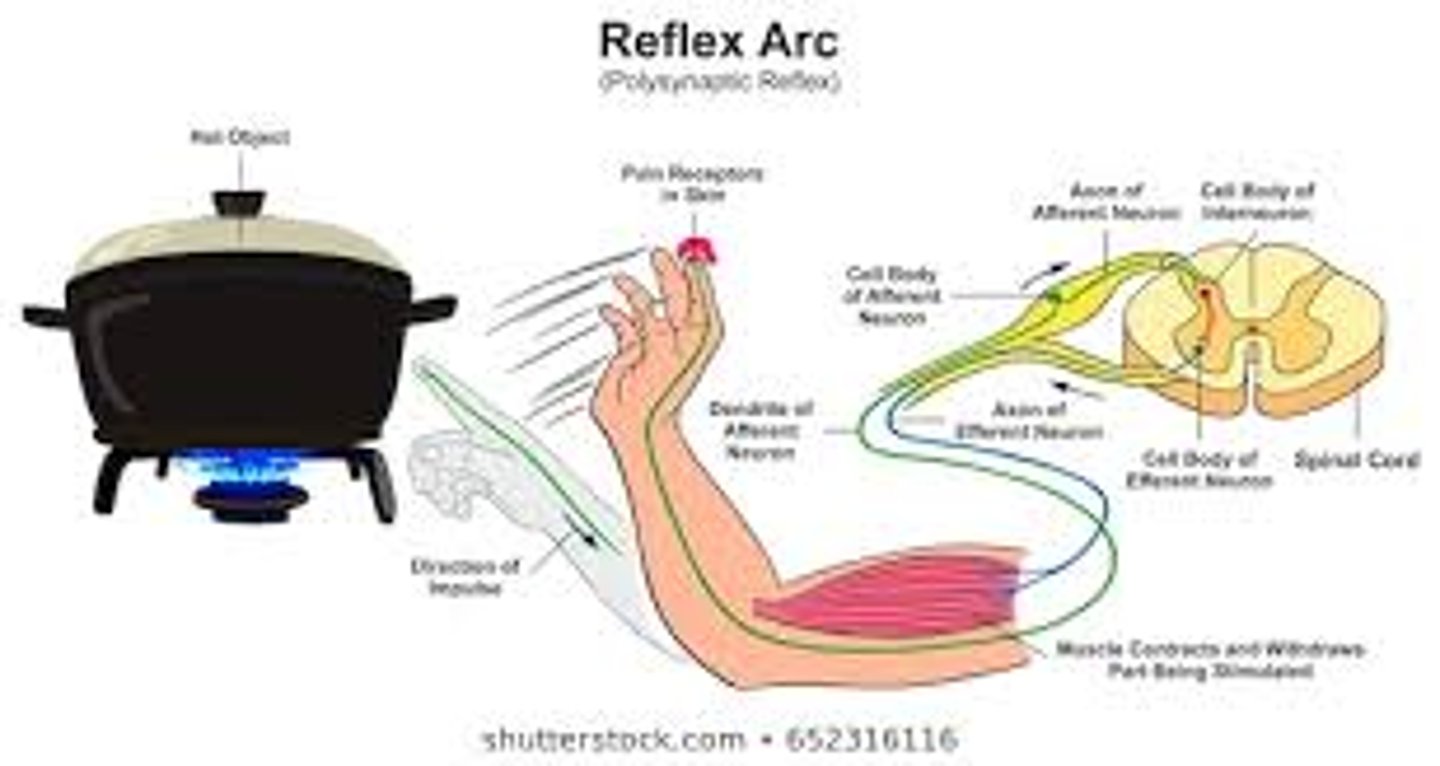
1- nervous system (is instantaneous)
.In the nervous system the Neurons and supporting cells are found in the CNS(central nervous system) and PNS( peripheral nervous system)
.A particular neuron can span a long distance.
. a neuron transmit electrical signals down the length of their axon; and turns into a chemical signal(neurotransmitters) at the axon terminals.
.Is fast communication (but its effects last only short time).
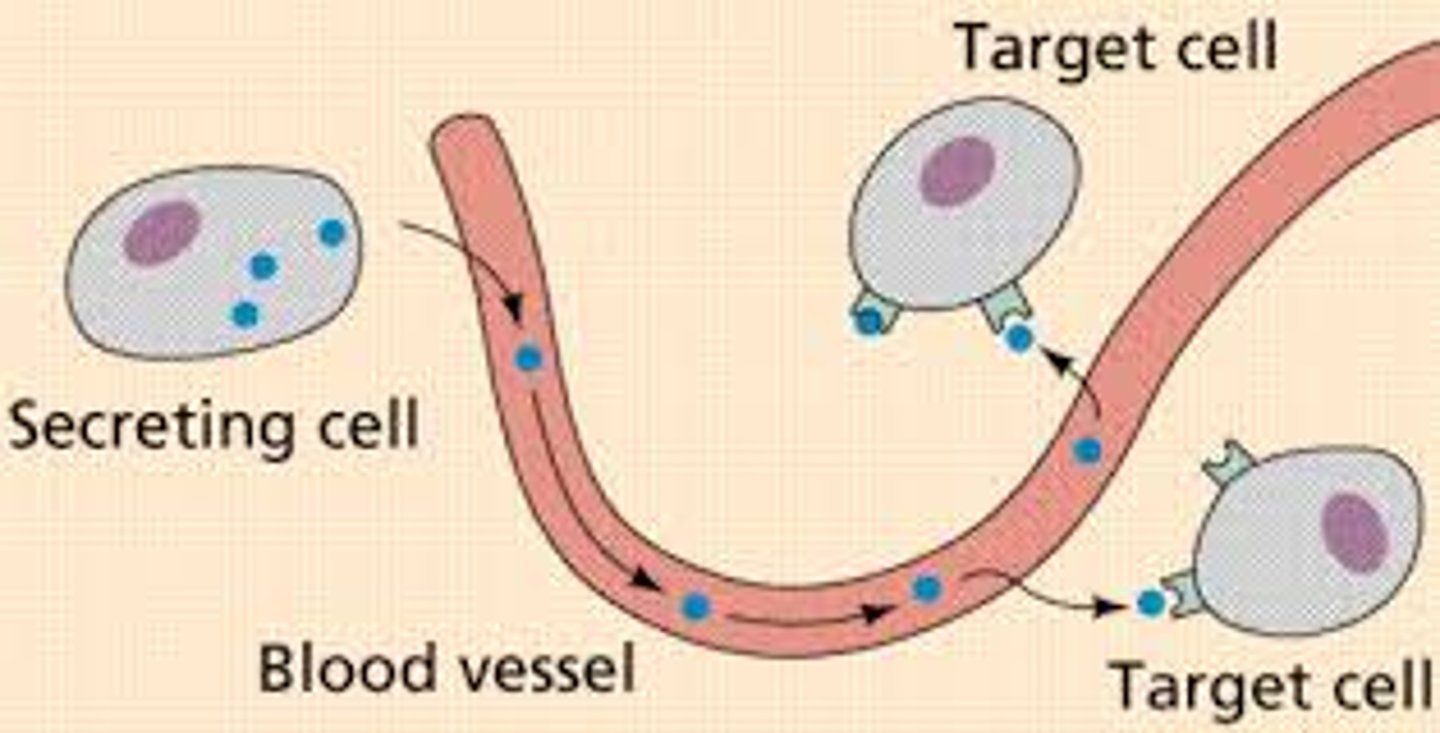
2- Endocrine system(is slower but last longer as well):
-It lacks direct contact with its target, so it relies on hormones that are delivered via the circulatory system(blood).
-It acts slow but it is able to offer communication for prolonged time which is important for coordinating homeostasis (for ex: metabolism, cell growth) and for specialized processes, such as reproduction, and lactation.
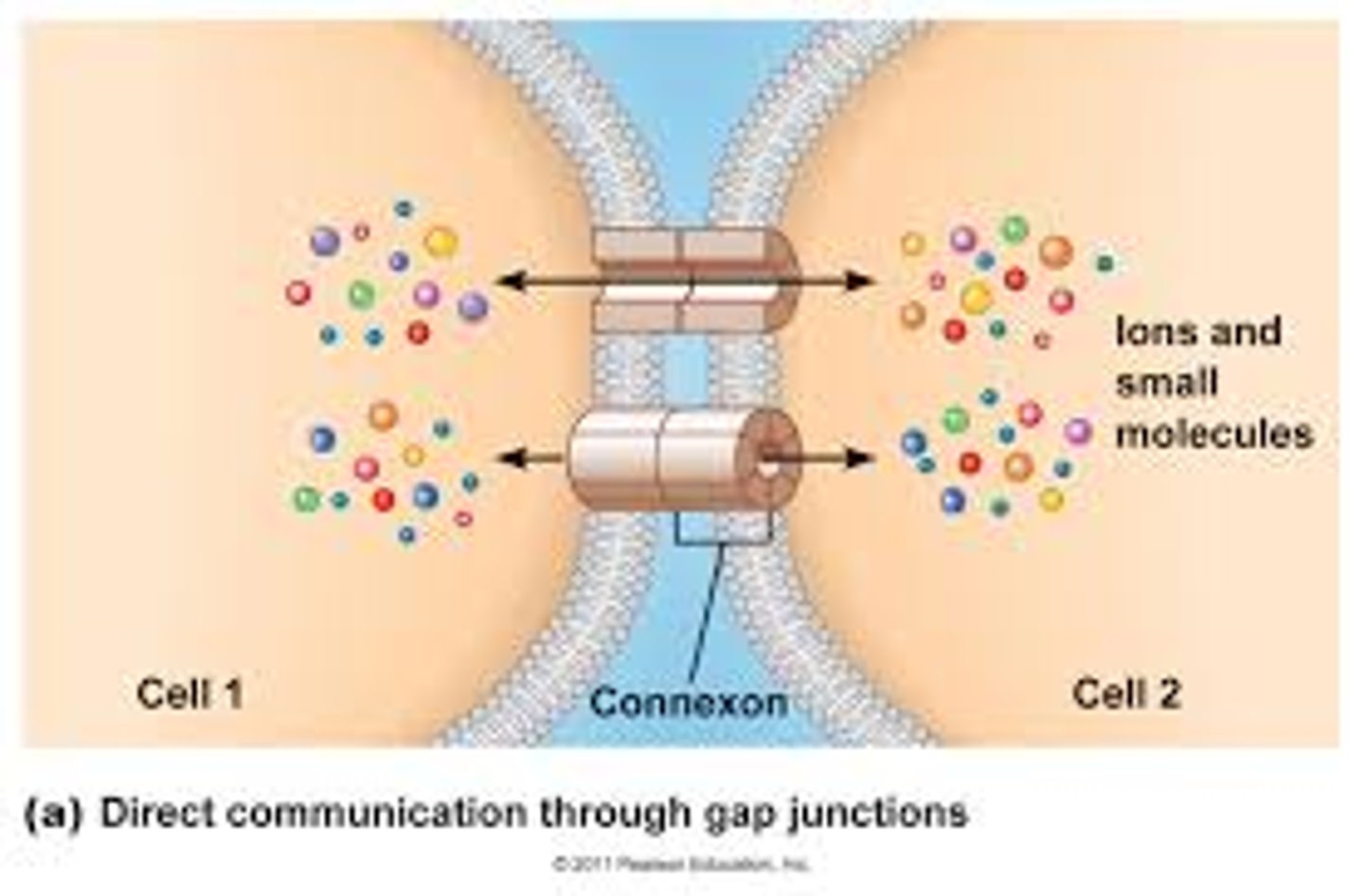
2- Direct communication= via gap junctions
-one of these gap junctions is Connexin : which is made when plasma proteins that come together to form channels.
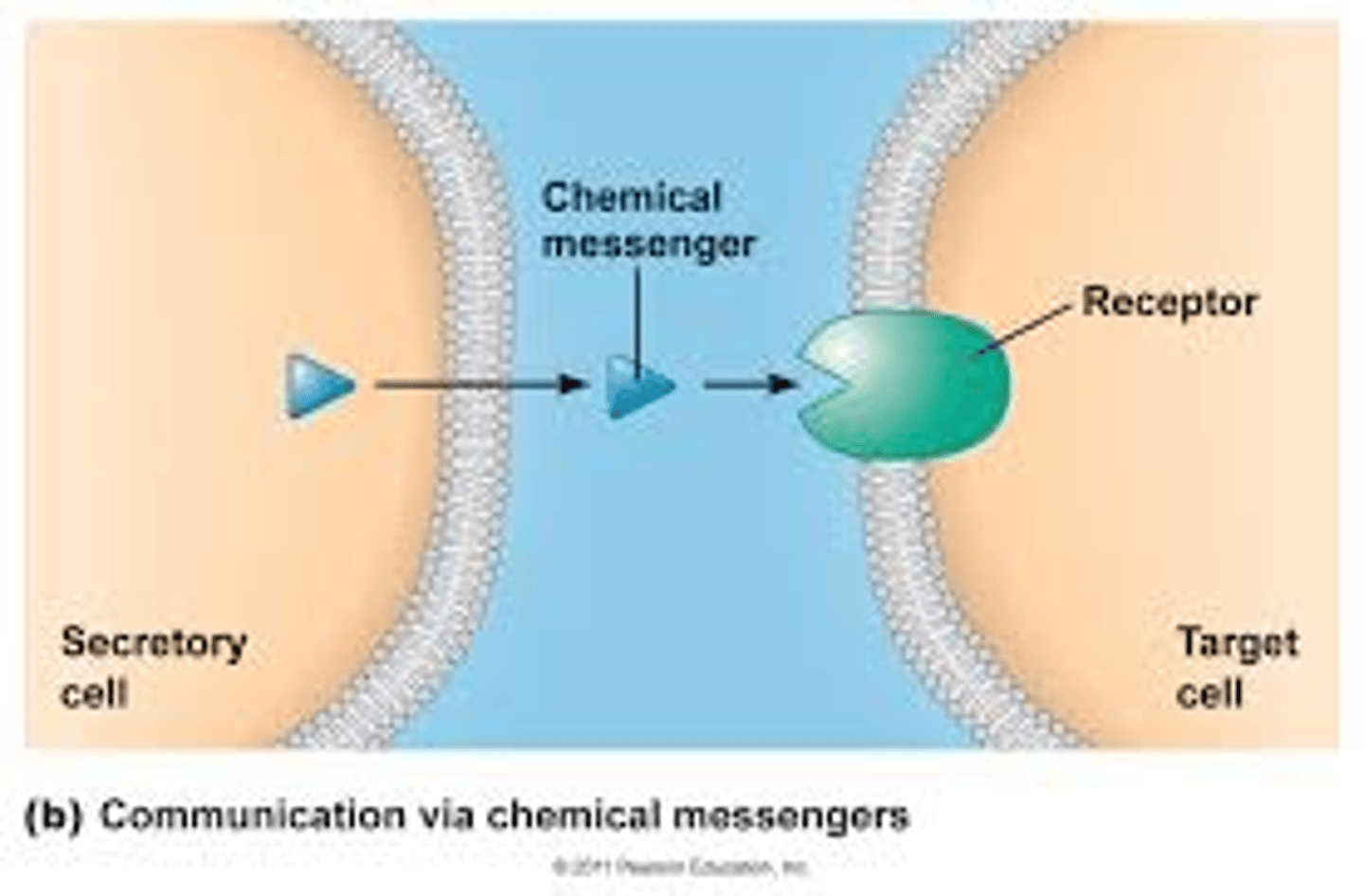
3- Indirect communication=via chemical messengers
General method of communication via chemical messengers:
1-The Ligand(chemical messenger) binds to its receptor on the target cells.
2-Then, the binding of the ligand to its receptor, causes a signal transduction, which:
. It induces changes within proteins that already exist inside of the cell. (cells have and make proteins inside of them at the RER).
. It induces the cell to manufacture new proteins (transcription and translation )
3-Then, The signal transduction cause a physiological response: it refers to the change that occurs as a consequence from the transduction of the signal(ex, the production of glucose transporters when the ligand which in this case is insulin binds to the tyrosine kinase on the cell's plasma membrane.)
3 methods of communication for cells::
1-Long distance communication-centers of the body(is made of 2 systems:
-Nervous system
-Endocrine system
2- Direct communication= through gap junctions
3- Indirect communication= via chemical messengers(ligands)
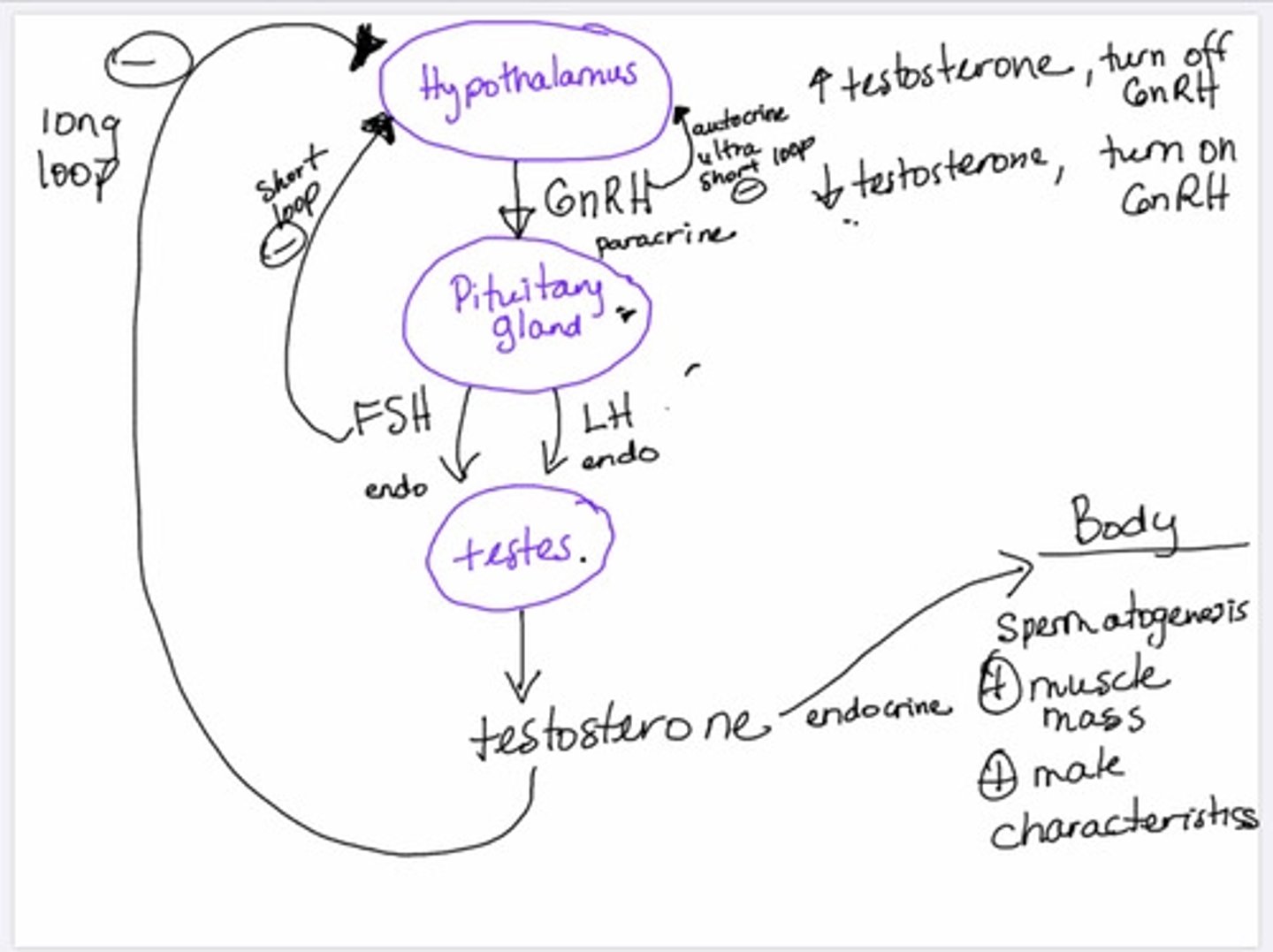
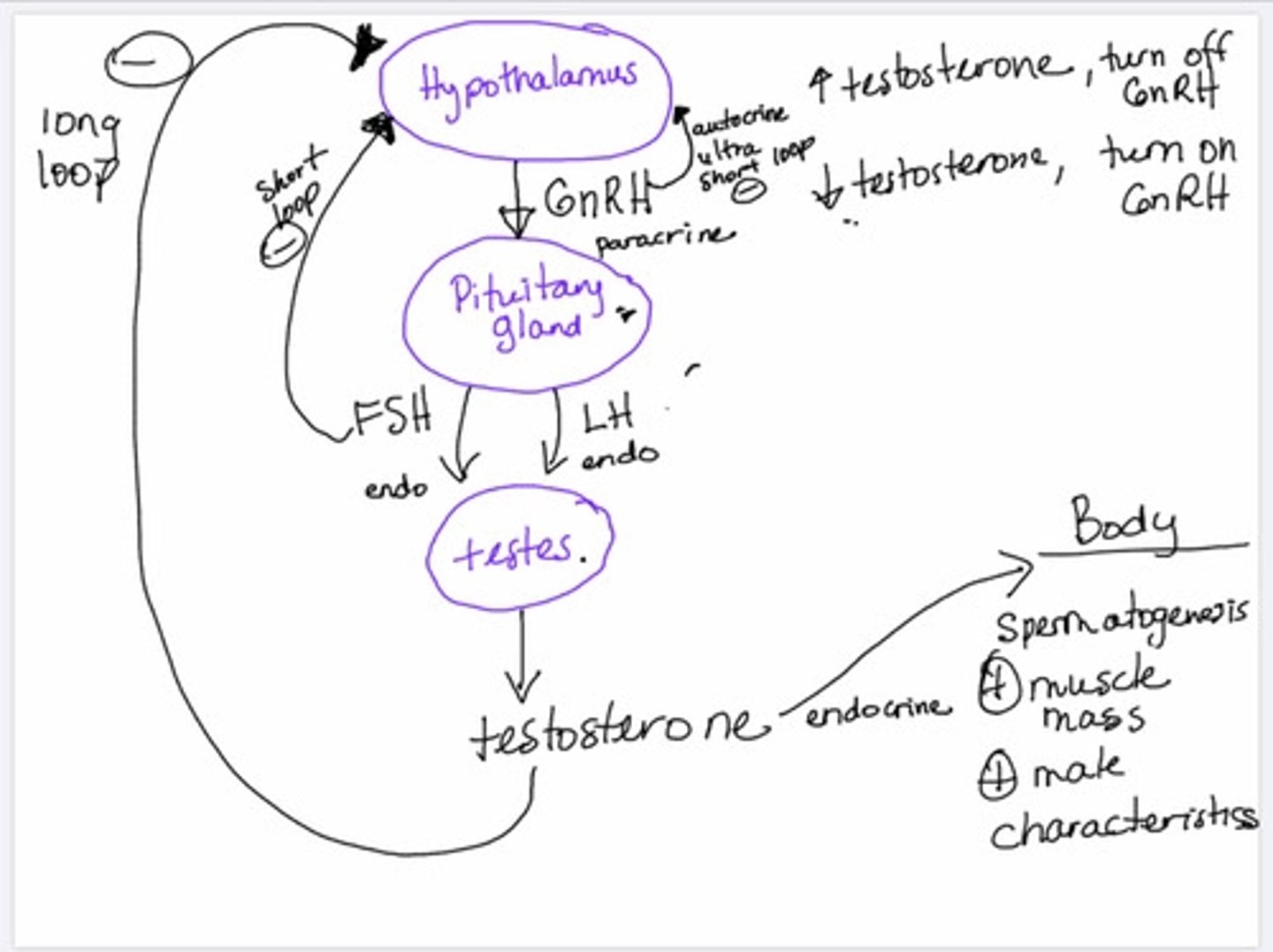
Hormonal negative feedback loop
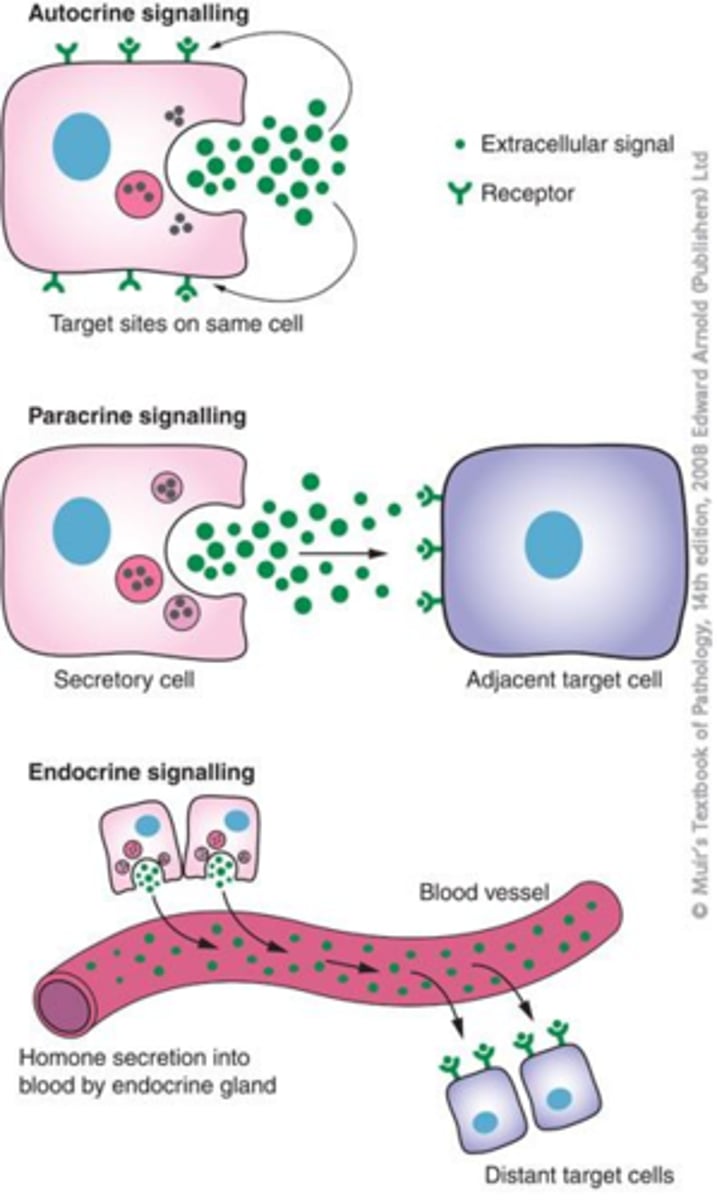
1-autocrine
2-paracrine
3-endocrine
Long distance communication-centers of the body: nervous system and endocrine system
1- nervous system ( which is instantaneous but last for very little time)
2- Endocrine system( which is slower action bus lasts longer)
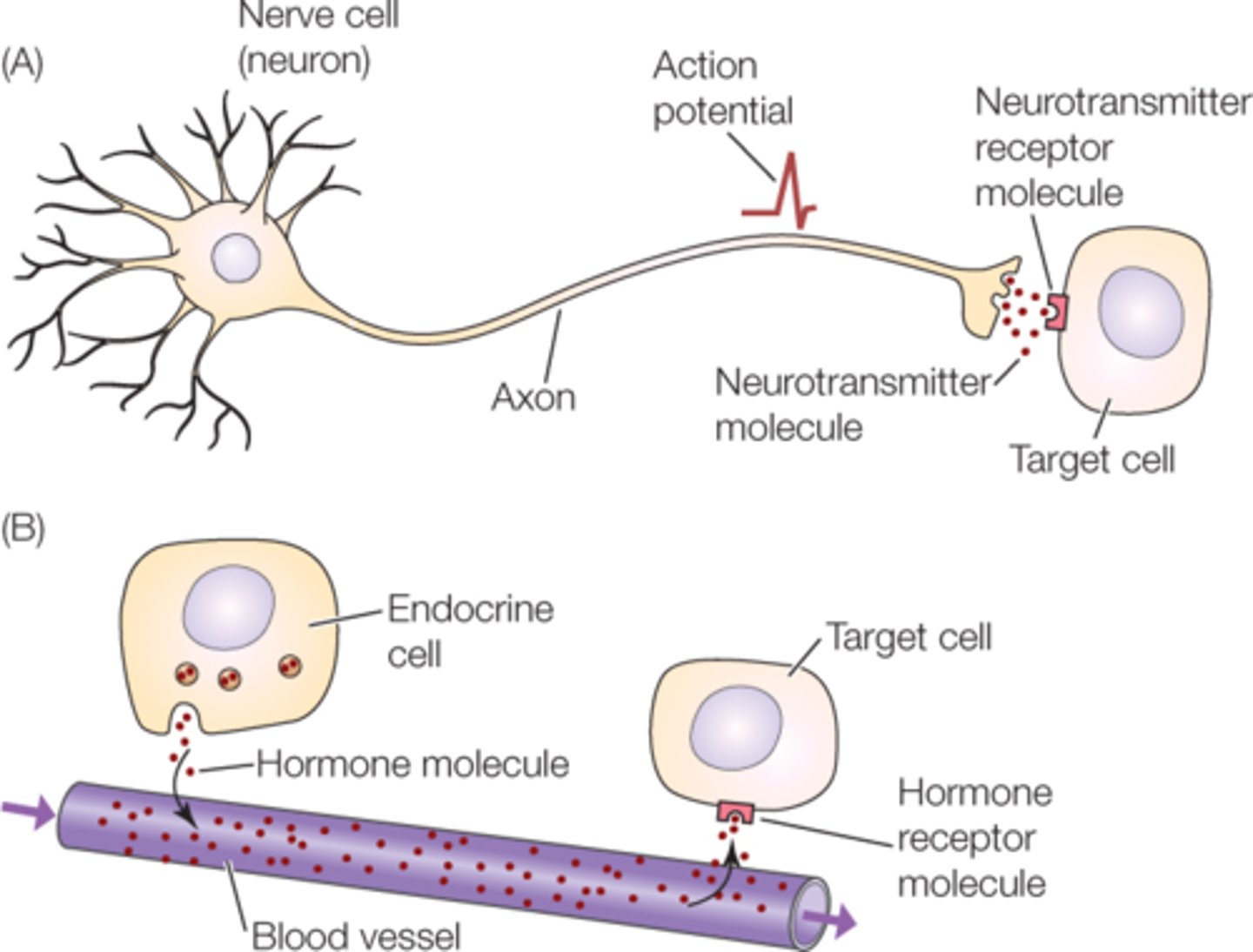
Long distance communication centers of the body: nervous system (4 characteristics)
nervous system (is instantaneous)
1- Neurons and supporting cells are found in the CNS(central nervous system) and PNS ( peripheral nervous system)
2- A particular neuron can span a long distance.
3- Transmit electrical signals down the length of their axon; and at the axon terminals it turns into a chemical signal (which is usually a neurotransmitters).
4-Is fast communication (but its effects last only short time).
Long distance communication centers of the body: Endocrine system:(2 characteristics)
Endocrine system:
1-It lacks direct contact with its target, so it relies on hormones that are delivered (to specific target cell) via the circulatory system(on blood).
2-It acts slow but it is able to offer communication for prolonged time which is important for coordinating homeostasis (for ex: metabolism, cell growth) and for specialized processes, such as reproduction, and lactation.
What is a connexin?
is a type of gap junction protein: is made when plasma proteins come together to form channels.
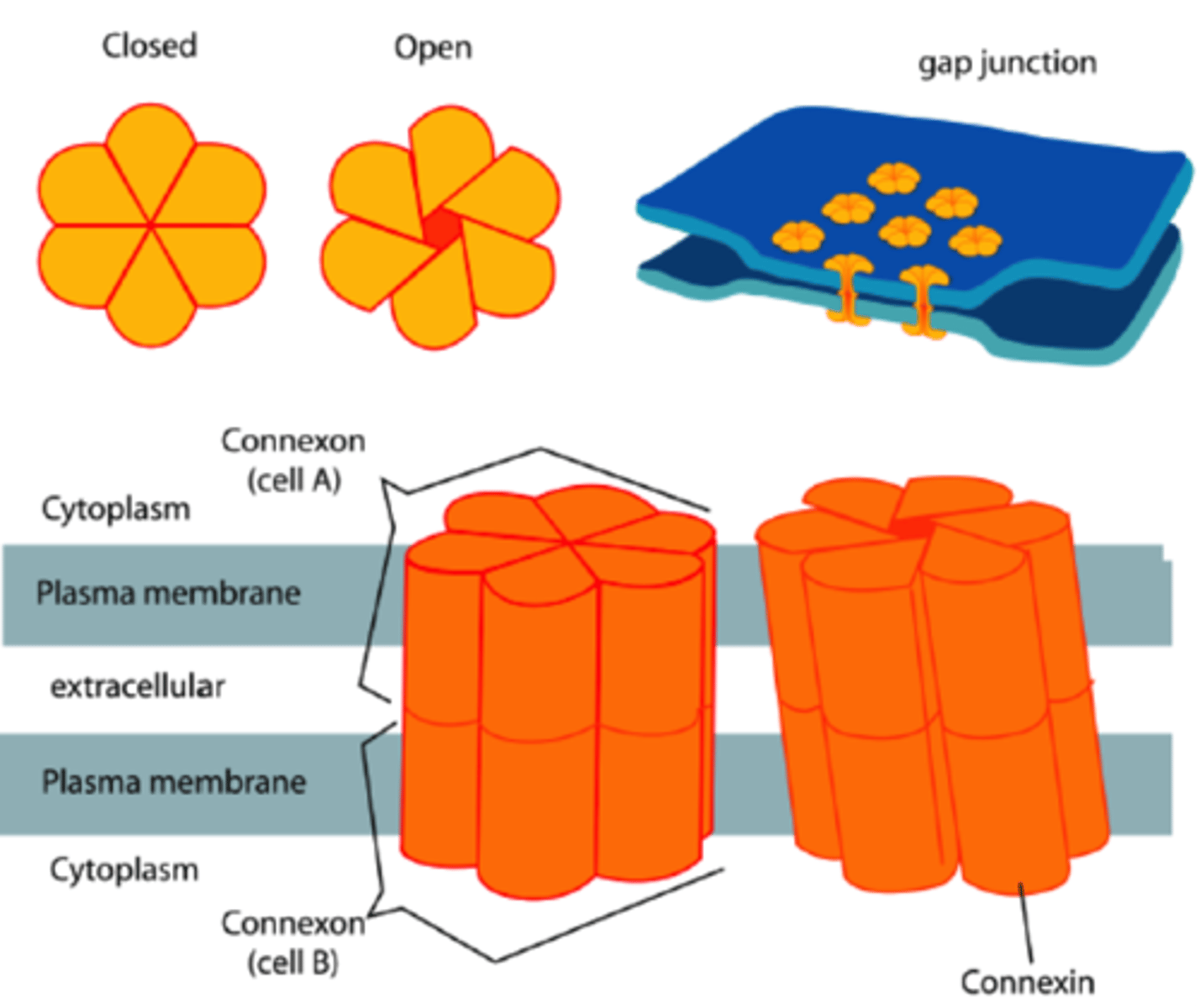
method of communication for cells: Direct communication
is performed through gap junctions
-one of these gap junctions is Connexin : which is made when plasma proteins that come together to form channels.
method of communication for cells: Indirect communication
Is performed via chemical messengers(ligands)
3 steps of General method of communication via chemical messengers:
1-Ligand(which is a chemical messenger) binds to its receptor on the target cell (wherever the receptor is located on the plasma membrane or inside of the cell).
2-Then, the binding of the ligand to its receptor causes a signal transduction. (this transduction is literally passing the signal from the ligand receptor to the nucleus of the cell)
. It induces changes within proteins that already exist inside of the cell. (cells have proteins inside of them and also make proteins inside of them at the RER to sent out of the cell or to keep them inside).
. It also induces the cell to manufacture new proteins (transcription and translation )
3-Then, The signal transduction cause a physiological response: it refers to the change that occurs as a consequence from the transduction of the signal(ex, the production of glucose transporters when the ligand which in this case is insulin binds to its receptor in P.M, then receptor activates the tyrosine kinase enzyme inside of the cell's plasma membrane, the the signal transduction occur and as consequence from it, a physiological response which is the manufacturing of glucose transporters. further more, the glucose will be absorbed into the cell through the Gluts.)
method of communication for cells: 3 steps of General method of communication via chemical messengers
1-Ligand(chemical messenger) binds to its receptor on the target cells.
2-Then, the binding of the ligand to its receptor causes a signal transduction:
. It induces changes within proteins that already exist inside of the cell.
. It induces the cell to manufacture new proteins (transcription and translation )
3-Then, The signal transduction cause a physiological response: (it refers to the change that occurs as a consequence from the transduction of the signal(ex, the production of glucose transporters when the ligand which in this case is insulin binds to its receptor in P.M, then receptor activates the tyrosine kinase enzyme inside of the cell's plasma membrane, the the signal transduction occur and as consequence from it, a physiological response which is the manufacturing of glucose transporters. further more, the glucose will be absorbed into the cell through the Gluts.)
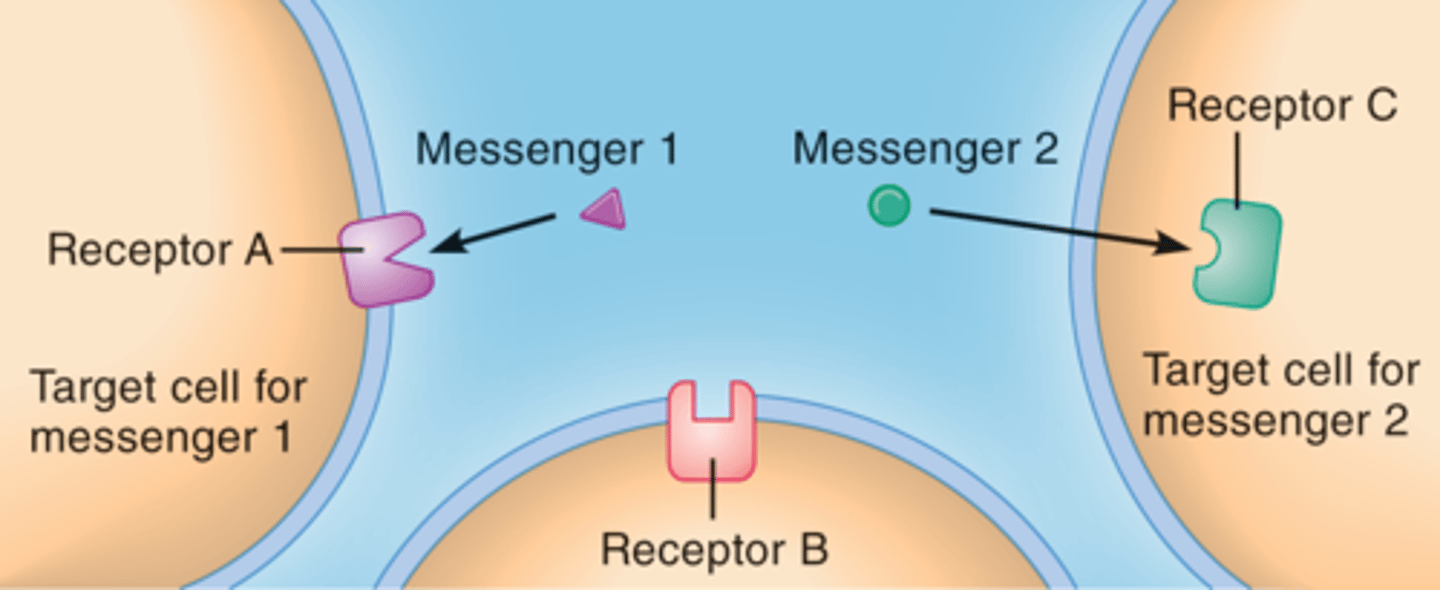
Characteristics of receptors( when referring to cell's communication)
1- location: receptors can be located on:
. on the plasma membrane
. in the cytosol of the cell
. inside of the nucleus
2-Receptors are specific to a given ligand or ligands
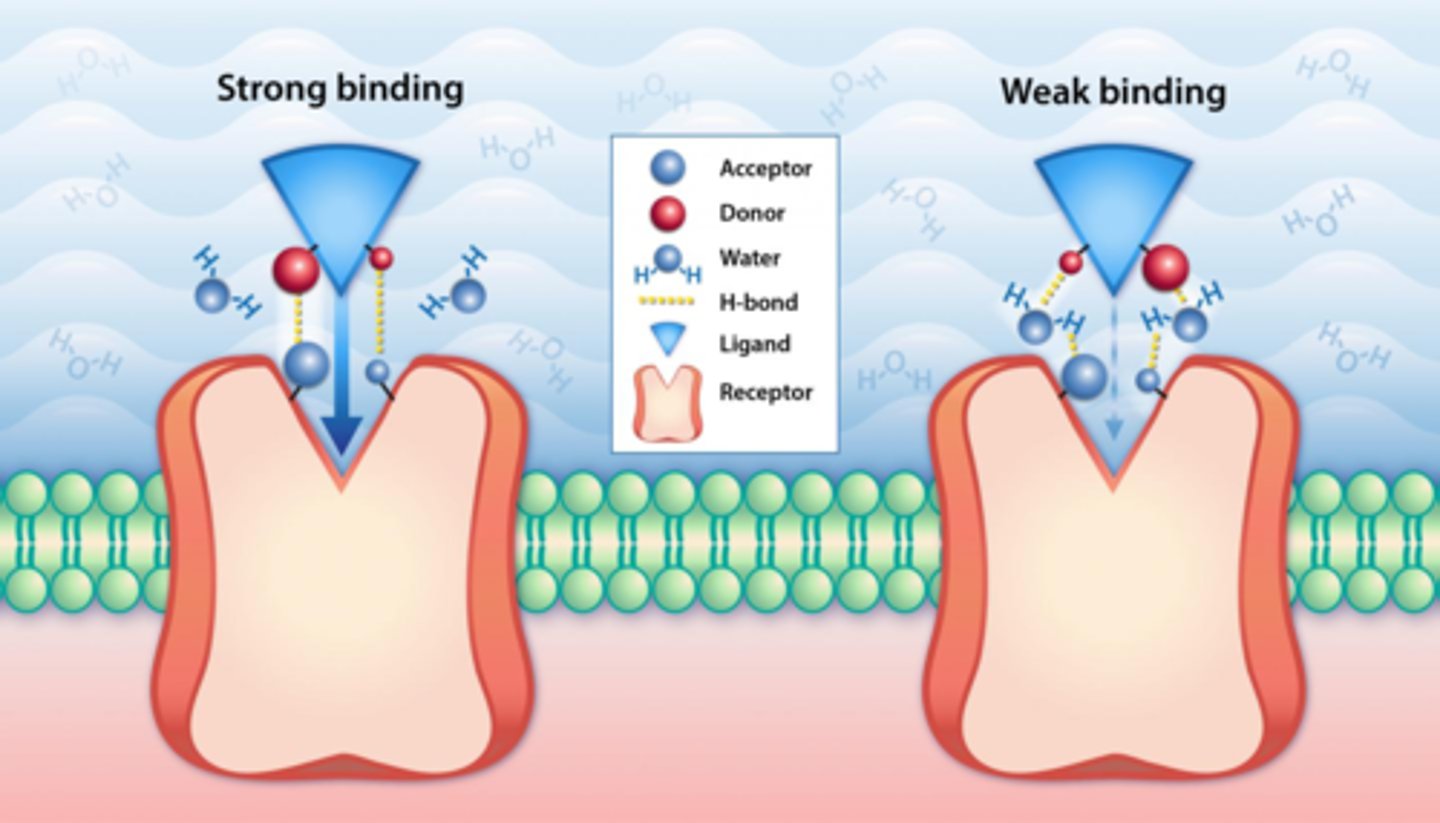
3-they have affinity to a given ligand.
.Affinity: means the strength of the bond between the ligand and its receptor.
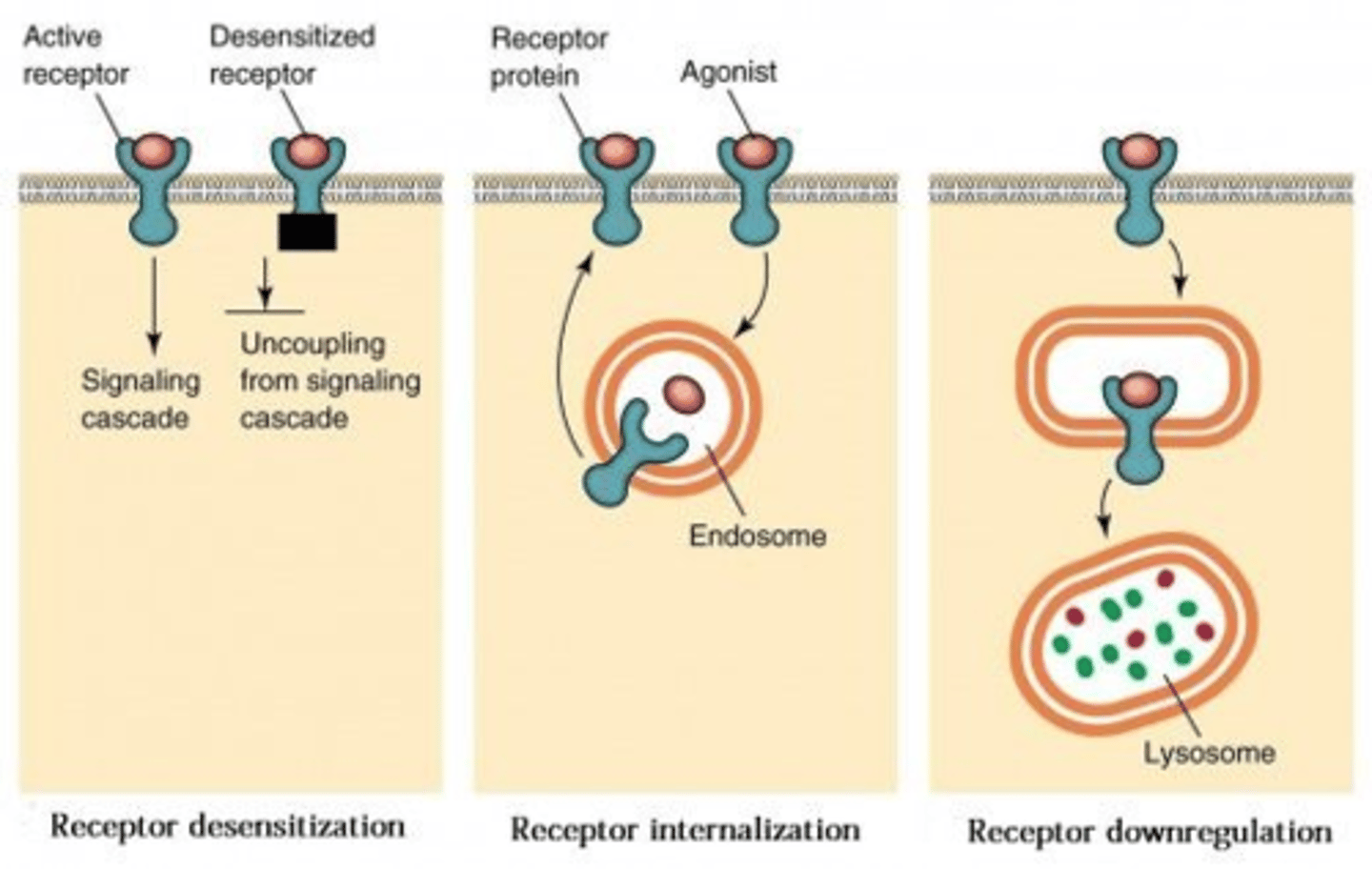
4-The number of available receptors can be regulated:
. upregulated: increase in number
. Downregulated : decrease in number.
4 Characteristics of receptors
1- location
2-Receptors are specific to a given ligand or ligands
3-they have affinity to a given ligand.
4-The number of available receptors can be regulated
Characteristics of receptors :location:(3 locations)
1- are located on the plasma membrane
2-in the cytosol of the cell
3-inside of the nucleus
Characteristics of receptors: Receptors are specific to a given ligand or ligands
Receptors are specific to a given ligand or ligands
Characteristics of receptors: they have affinity to a given ligand.
.Affinity: means the strength of the bond between the ligand and its receptor.
Characteristics of receptors: The number of available receptors can be regulated:
. upregulated: increase in number
. Downregulated : decrease in number.
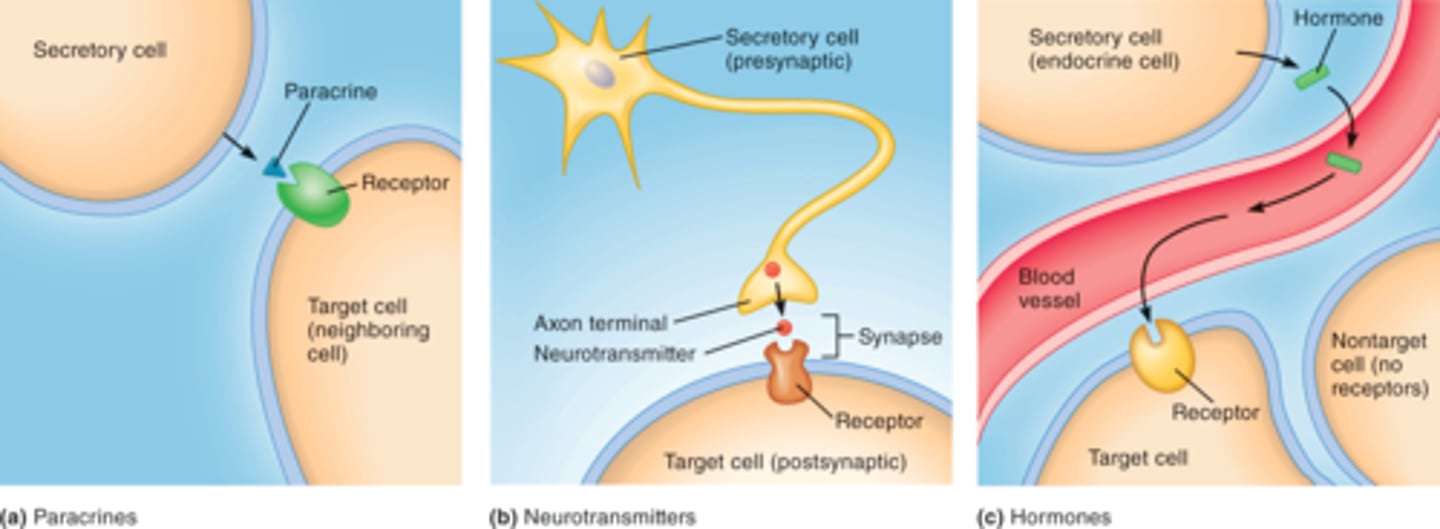
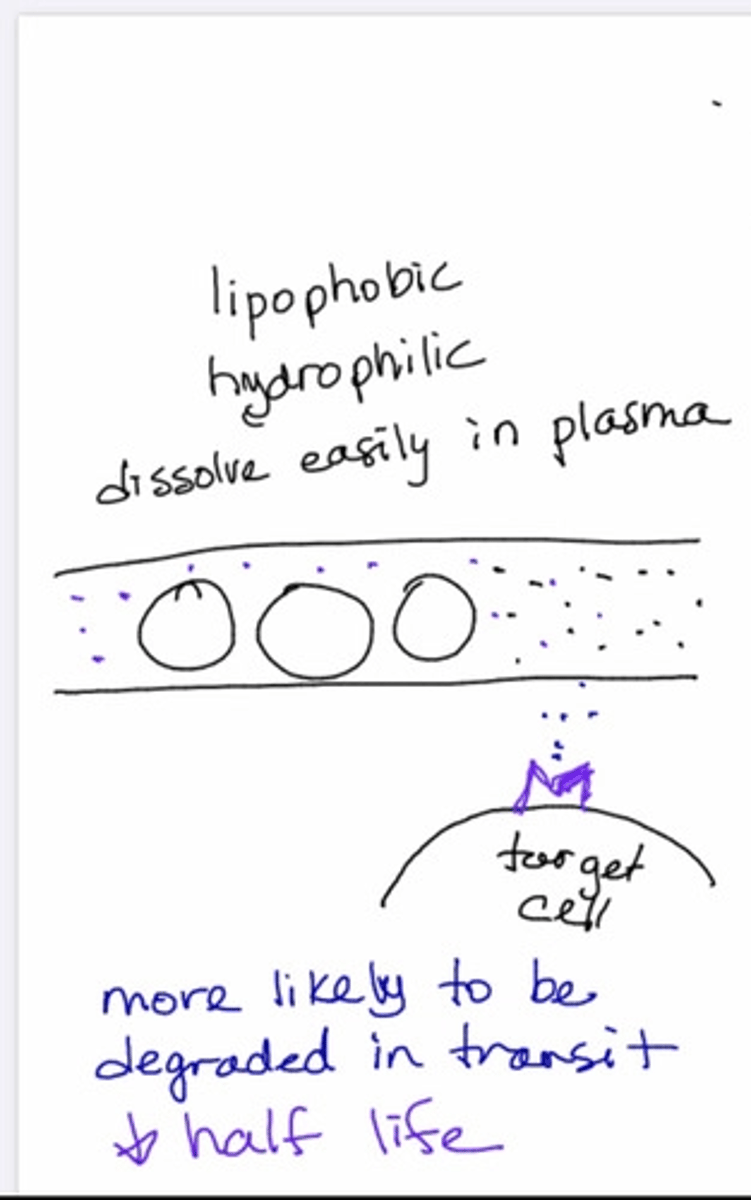
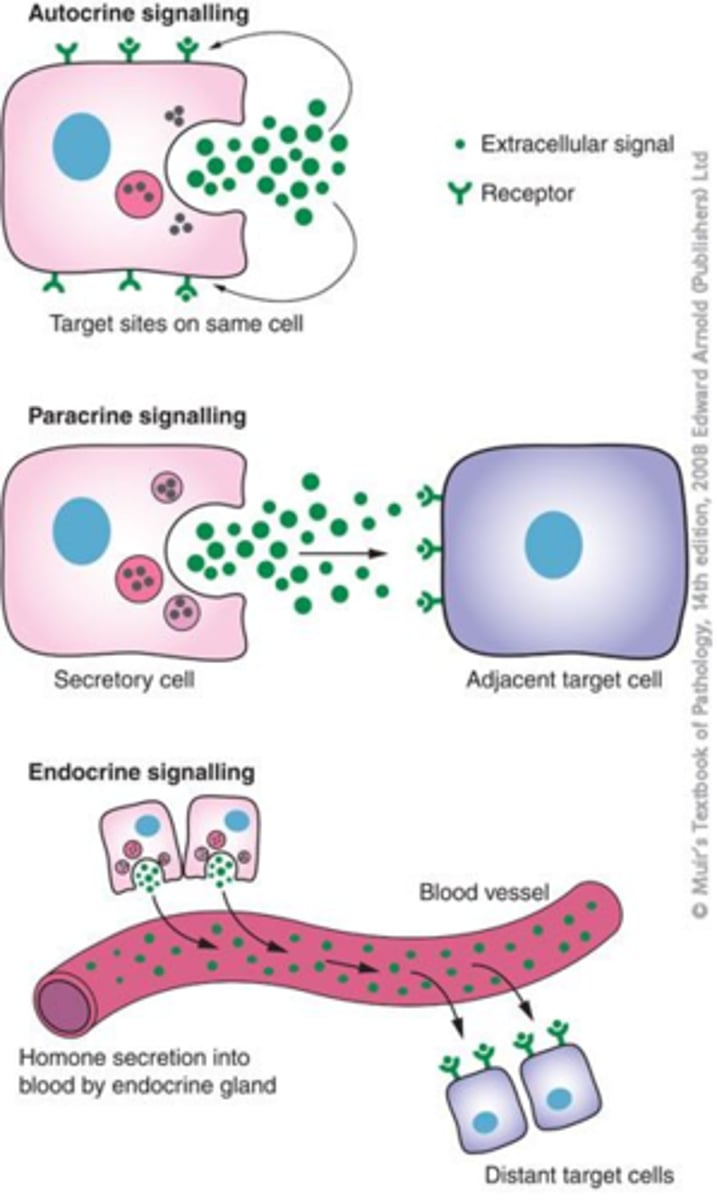
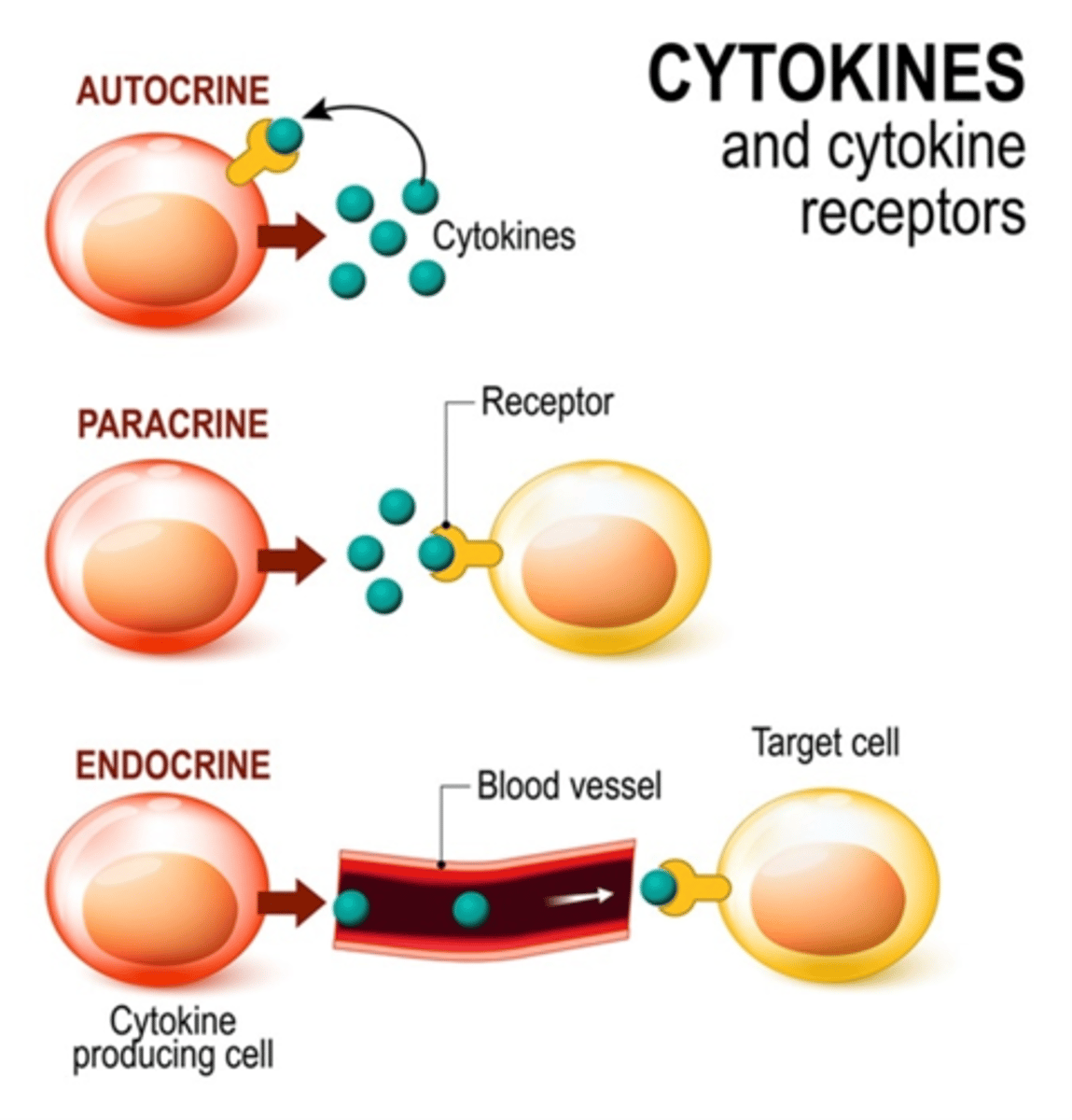
Characteristics of ligands: ( when referring to cell's communication)
1- the distance between the ligand released and the target cell will determines its action.
.Autocrine: ( regulate its-self, the same hormone produced by a gland, will case a negative ultrashort feedback loop)
.Paracrine: (regulates a close neighbor cell for Ex: the hypothalamus and the pituitary gland are neighbors)
.Endocrine: (regulates cells at Distance away/ far away; not self and not neighbors)
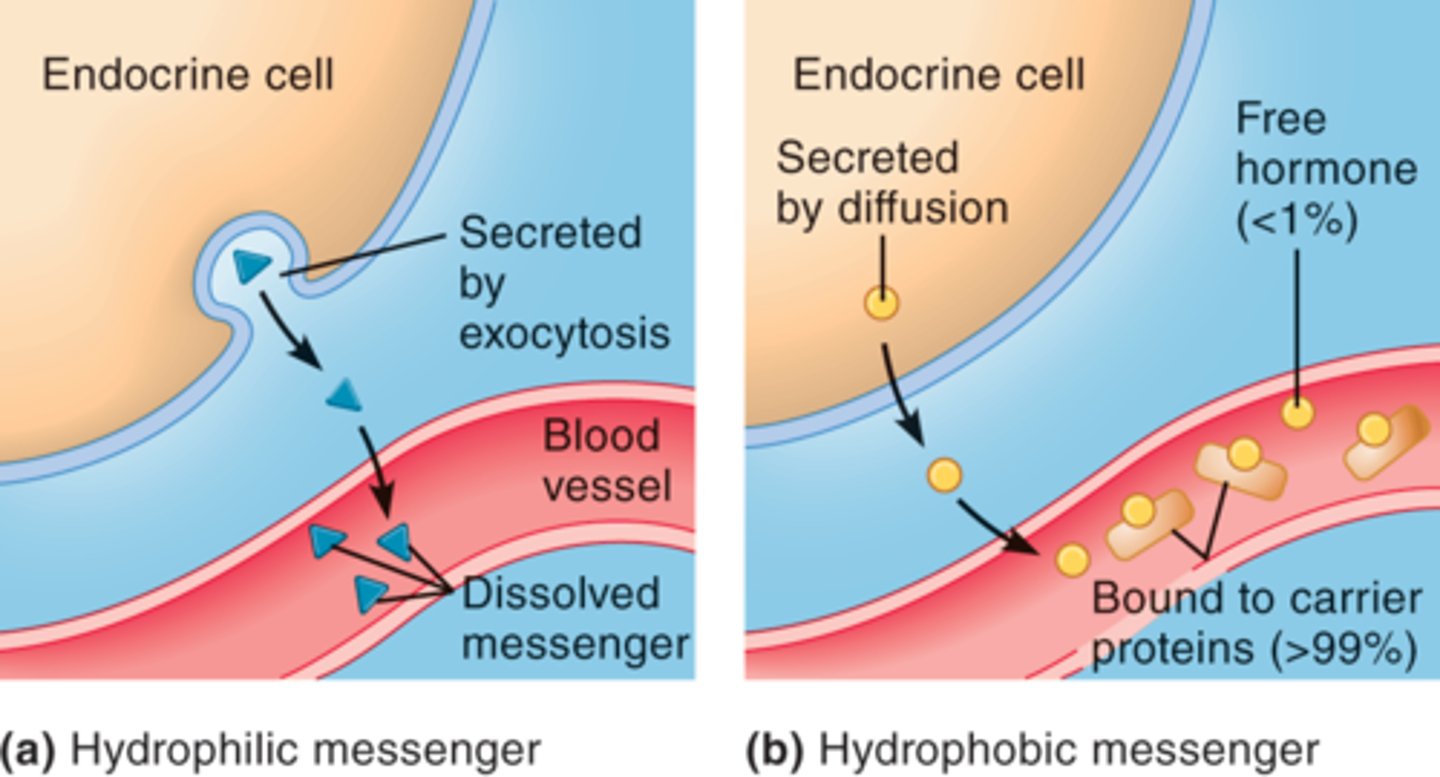
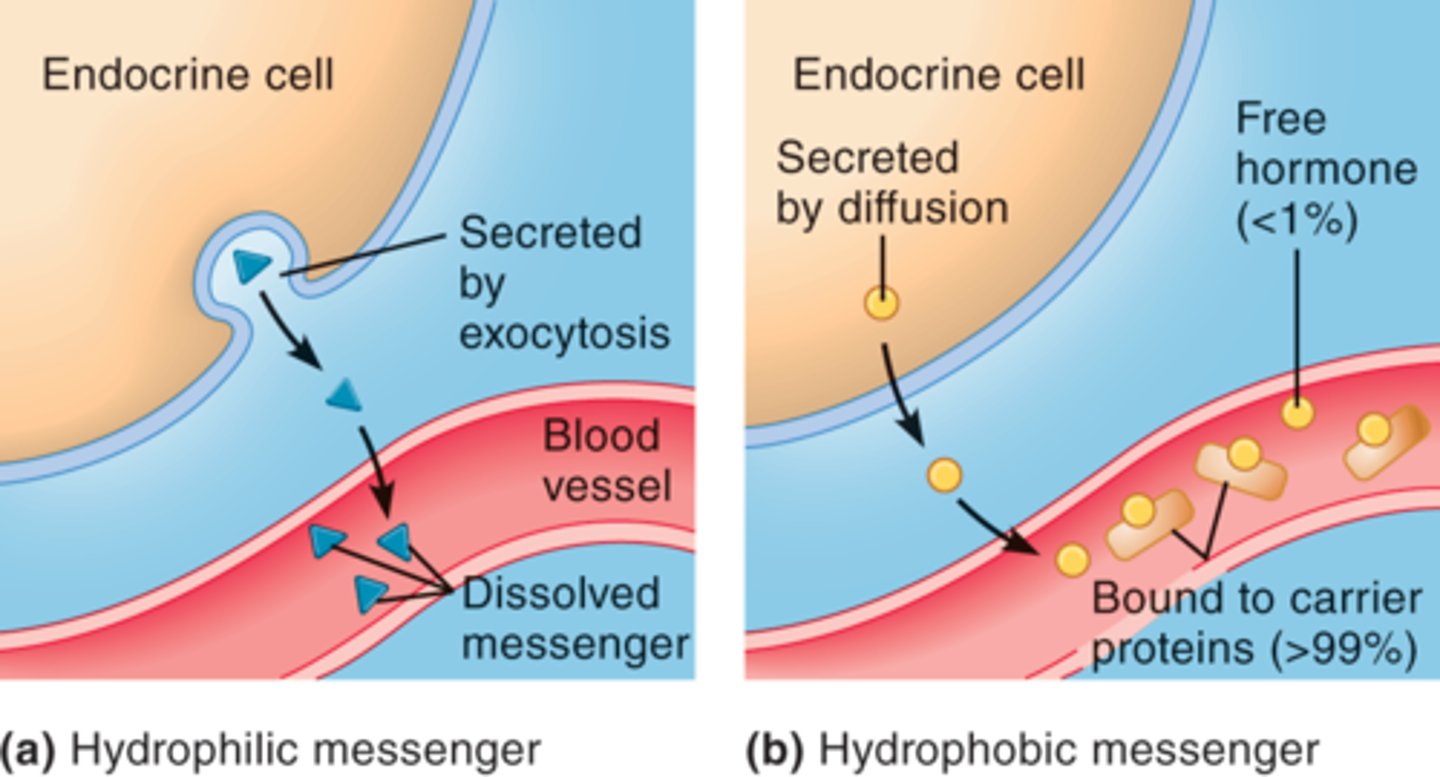
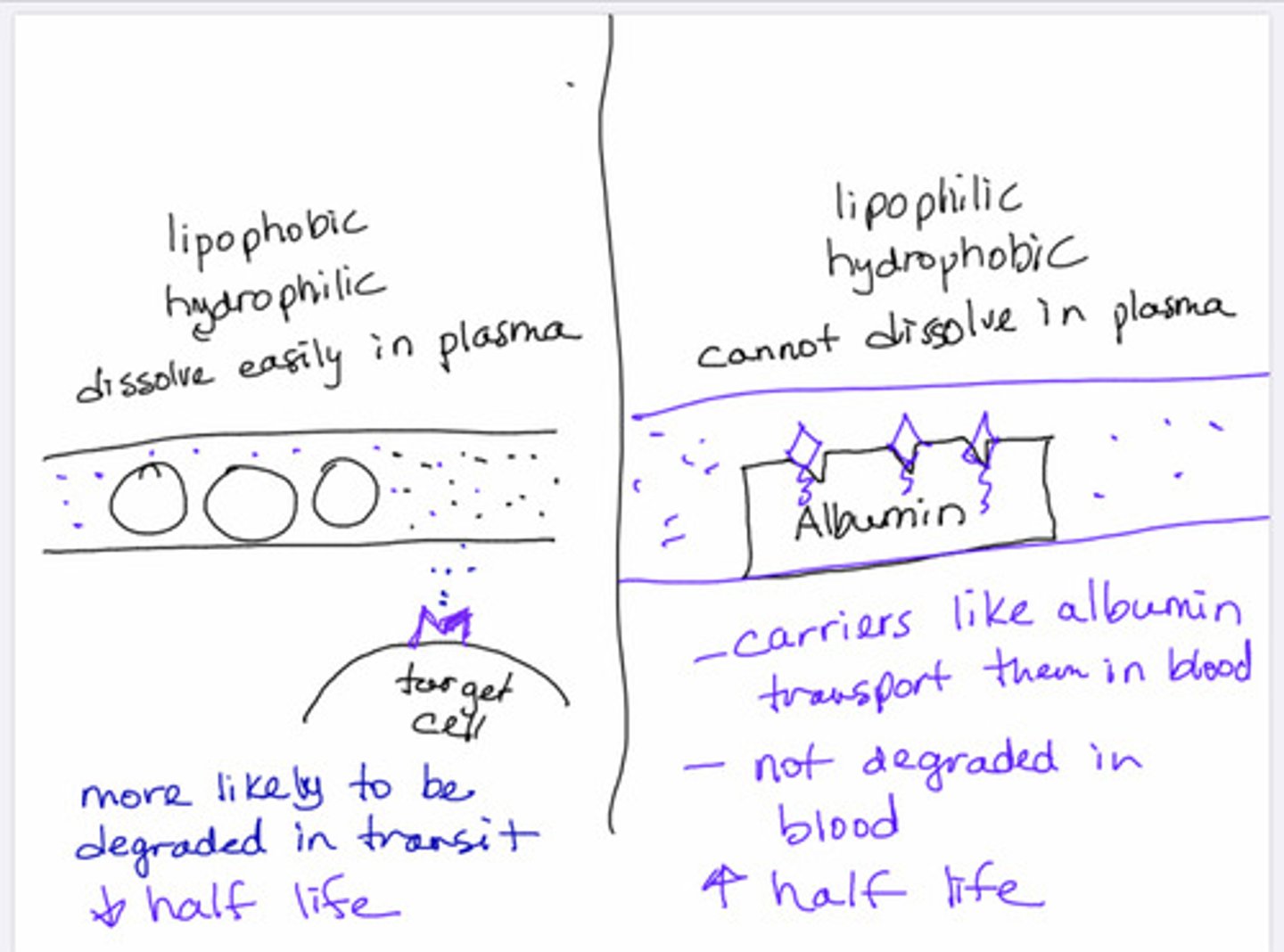
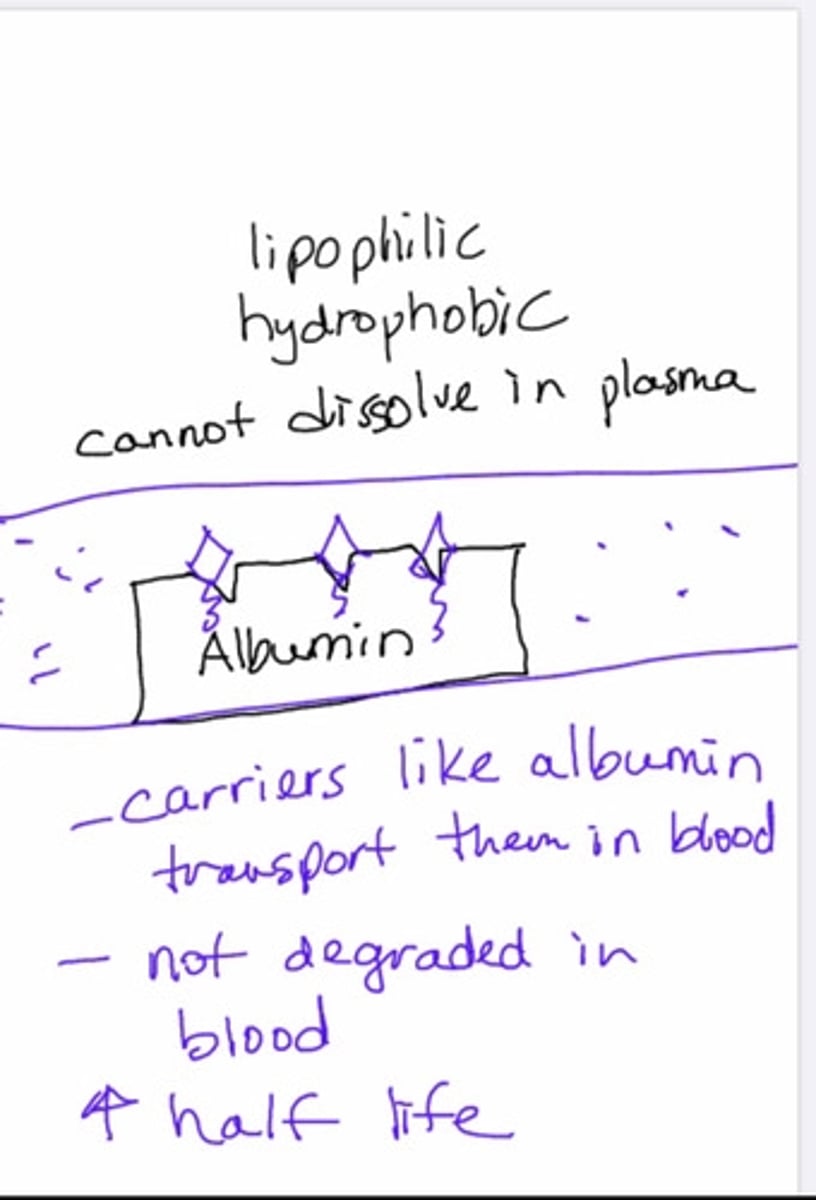
2-The LIgand's chemical structure determines its action:
.Lipophilic/hydrophilic: can easily/freely cross the membrane:
.The receptors for lipophilic/hydrophobic ligands are located on the intracellularly( in the cytosol or nucleus, because is anticipated that these ligands will be able to freely cross the cell's plasma membrane).
.lipophobic/hydrophilic: cannot cross the plasma membrane without assistance:
.the receptors for lipophilic/hydrophilic ligands on the plasma membrane( since they can not cross the plasma membrane)
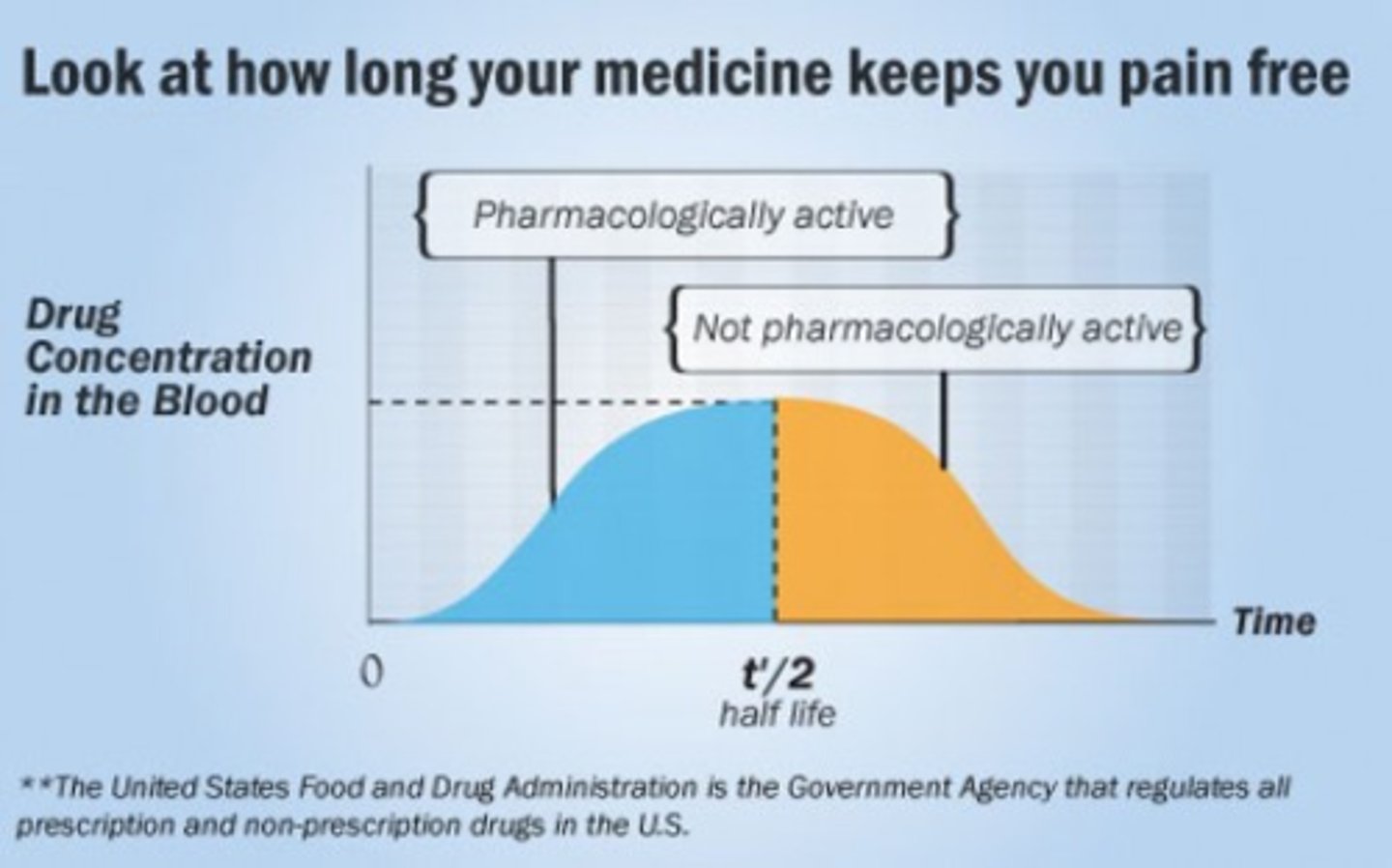
3-Half-life: is the time that it takes for half of the ligand in the plasma to be degraded.( in general half-life means the time that it takes for a medication or any other particle to get reduced to 50% of it in the body.)
- it measures the ligand's lifespan in the body.
-the half-life of autocrine and paracrine ligands are short; the half-life of endocrine hormones is longer.(the closest the target is; the fastest the ligand reaches its target, and also the fastest it does its physiological effect and die off)
- The time of degradation of the ligand, depends on how the ligand is transported.
. lipophobic/hydrophilic ligands dissolve in the ISF(interstitial fluid) they do not require carriers.
.Lipophilic/ hydrophobic ligands use carrier proteins:
.carriers protect them from degradation(they prolong the ligand's half-life)
.Carriers allow the ligands to travel in the ISF and plasma.
.The ligand must separate its self from the carrier in order to be active. (free ligand = active ligand)
2 Types of ligand's carriers:
1- specific: they will only shuttle a specific ligand or class of ligands.
2- general: they will carry a variety of ligands:
. Albumin (is one of may general ligand carriers).
Characteristics of ligands: the distance between the ligand released and the target cell will determines its action.
(APE acronym)
.Autocrine signaling: regulates its-self
.Paracrine signaling: regulates a close neighbor cell (for Ex: the hypothalamus and the pituitary gland)
.Endocrine signaling: regulates cells at Distance away/ fare away
Characteristics of ligands: The LIgand's chemical structure determines its action:
-Lipophilic/hydrophilic ligands can easily cross the membrane:
.The receptors for lipophilic/hydrophobic ligands are located on the intracellularly( for Eicosanoids its in the cytosol, for steroids its in the nucleus, because is anticipated that these ligands will be able to freely cross the cell's plasma membrane).
-lipophobic/hydrophilic ligands cannot cross the plasma membrane without assistance:
.the receptors for lipophilic/hydrophilic ligands on the plasma membrane( since they can not cross the plasma membrane)
Characteristics of ligands: Half-life:
is the time that it takes for half of the ligand in the plasma to be degraded. (half life of endocrine is longer than autocrine and paracrine. half life of lipophilics which are steroids and Eicosanoids is longer that lipophobics)
Characteristics of ligands: Half-life characteristics:
( in general half-life means the time that it takes for a medication, pesticide, gas or any other particle to get reduced to 50% of it in the body or environment.)
1- it measures the ligand's lifespan in the body.
2-the half-life of autocrine and paracrine ligands are short; the half-life of endocrine hormones is longer.
3-The time of degradation of the ligand, depends on how the ligand is transported.
- lipophobic/hydrophilic ligands dissolve in the ISF(interstitial fluid)they do not require carriers.(this ligand loves water which is almost the same of ISF, so this ligand can travel through blood very happy)
- Lipophilic/ hydrophobic ligands use carrier proteins:
.carriers protect them from degradation(they prolong the ligand's half-life)
.Carriers allow the ligands to travel in the ISF and plasma.(this because, since the ligand is hydrophobic it can not be on the ISF for long time or it will die off)
.The ligand must separate its self from the carrier in order to be active. (free ligand = active ligand)
what is used to measure the ligand's lifespan in the body?
half life
which half-life is longer the half life of autocrine and paracrine or the half-life of endocrine hormones ?
-the half-life of endocrine hormones is longer.
-half-life of autocrine and paracrine ligands are short
lipophobic/hydrophilic ligands vs Lipophilic/ hydrophobic ligands
- lipophobic/hydrophilic ligands dissolve in the ISF (interstitial fluid)they do not require carriers.(this ligand loves water which is almost the same of ISF, so this ligand can travel through blood very happy; However since they are just like any other substance in blood, they many of they will be degraded while in the trip, so their half life is less than lipophilics)
- Lipophilic/ hydrophobic ligands use carrier proteins:
.carriers protect them from degradation(they prolong their half life)
.Carriers allow the ligands to travel in the ISF and plasma.(this because, since the ligand is hydrophobic it can not be on the ISF for long time or it will die off)
.The ligand must separate its self from the carrier in order to be active. (free ligand = active ligand)(this will also affect the concentration of hormones in the blood; since this ligands are bound to the carriers, are inactive, so they do not count in concentration)
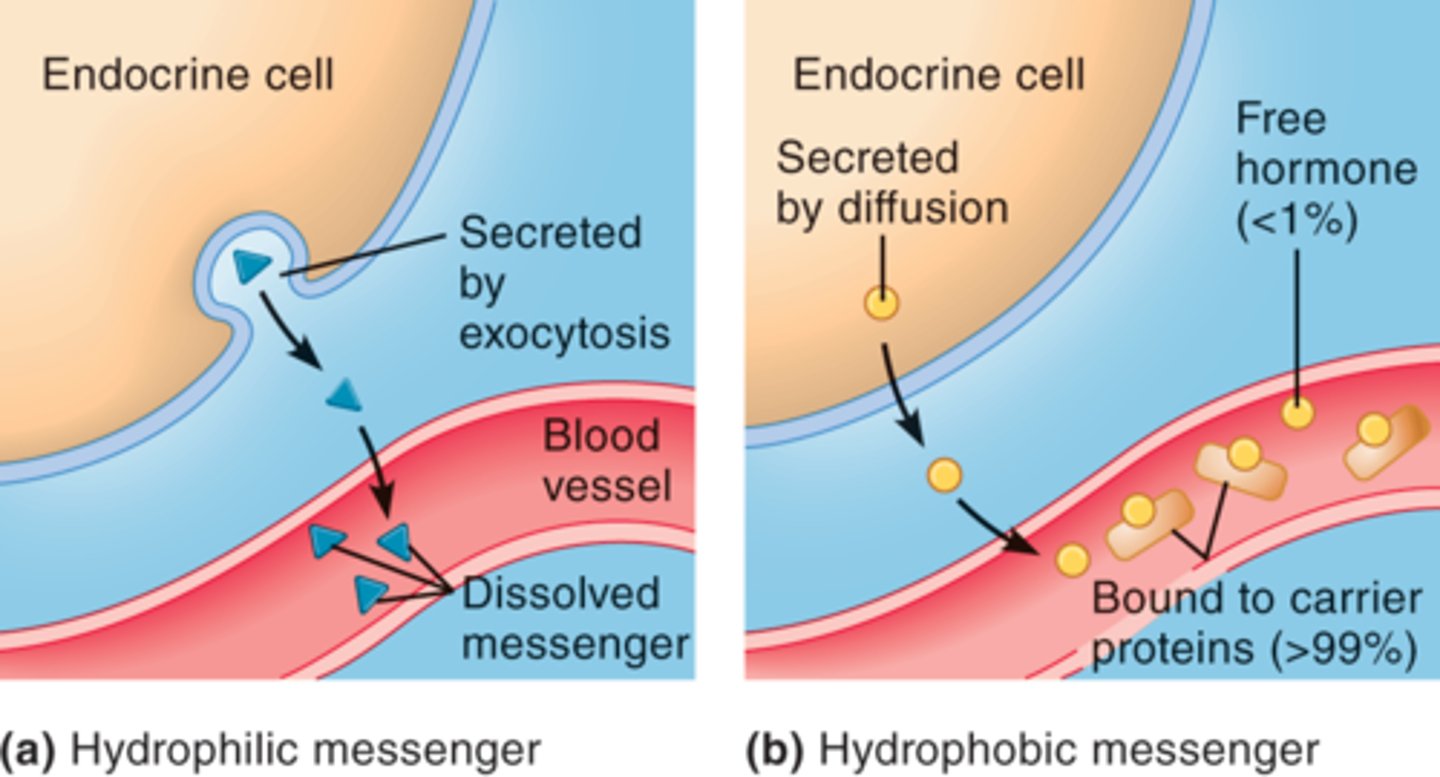
3 characteristics of Lipophilic/ hydrophobic ligands
- Lipophilic/ hydrophobic ligands use carrier proteins:
1- carriers protect them from degradation (they prolong the ligand's half-life)
2-Carriers allow the ligands to travel in the ISF and plasma.(this because, since the ligand is hydrophobic it can not be on the ISF for long time or it will die off)
3-the ligand must separate its self from the carrier in order to be active. (free ligand = active ligand)
2 Types of ligand's carriers:
1- specific carriers: they will only shuttle a specific ligand or class of ligands.
2- general carriers: they will carry a variety of ligands:
. Albumin (is one of many general ligand carriers).
why do cells need to communicate with each other?
(this answer is extra from the book)
Almost all body functions require communication between cells. Seeing an apple requires communication between the cells in the eyes and the neurons in the brain. Fighting an infection requires communication among several cell types in the blood. Moving your hand requires communication between neurons in the brain and spinal cord and the hand's muscle cells. Maintaining a normal blood glucose level requires the pancreas to release chemicals into the blood that communicate with cells throughout the body.
characteristics of lipophobic/hydrophilic ligands
lipophobic/hydrophilic ligands dissolve in the ISF(interstitial fluid)they do not require carriers.(this ligand loves water which is almost the same of ISF, so this ligand can travel through blood very happy; However since they are just like any other substance in blood, some of them will be degraded while in the trip, so their half life is less than lipophilics)
Functional classification of ligands:
Autocrine:
-it regulates its own cellular activity (usually inhibitory; short negative feed-back loop) by secreting ligand into ISF; it diffuses back to its self.
-its fast acting
-has short live
Paracrine:
- It regulates a neighboring cell's activity by secreting ligand into ISF; which diffuses into neighbor cells.
- is fast acting
- has short live
-example: the delta cells of the pancreas modulate the production of glucagon and insulin through somatostatin.
.Alpha cells secrete glucagon
.Beta cells secrete insulin
.Delta cell secrete somatostatin
(these 3 cells Alpha, Beta and Delta are neighbors; even though they are located within the same organ.)
Endocrine: (the ligand travels long distance through the blood)
-it regulates a distant(far away) target cells by releasing a hormone into the bloodstream.
-they take a longer time to action when compared to autocrine and paracrine ligands.
-it has longer half-life when compared to autocrine and paracrine.
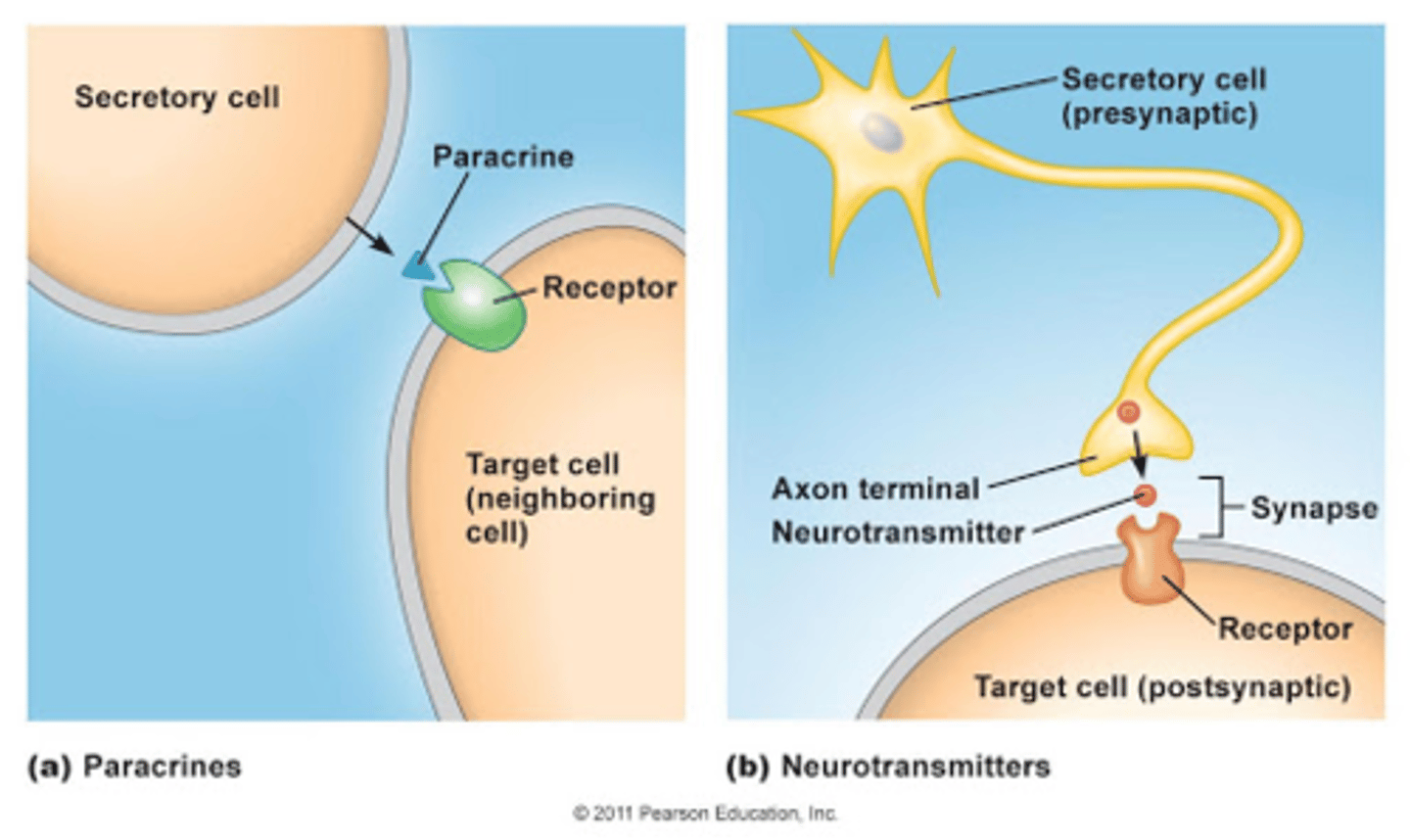
Neurotransmitters:
-Ligand is released into ISF from neurons (from the axon terminals into the synapse cleft)
-ligand is released by axon terminal
-it can affect another neuron or other cell type;
.Presynaptic neuron, then to synapse, then, to postsynaptic neuron.
. Neuromuscular junction (this is and example)
Hormones: (which come from the endocrine)
- Are distributed (sent) to the entire body but will only affect the cells that have the proper receptor.(the receptor for such hormone) ( for ex: ADH hormone is released (sent) to the entire body, but it will only affect the DCT, since it is the only part of the body that has the receptors for ADH).
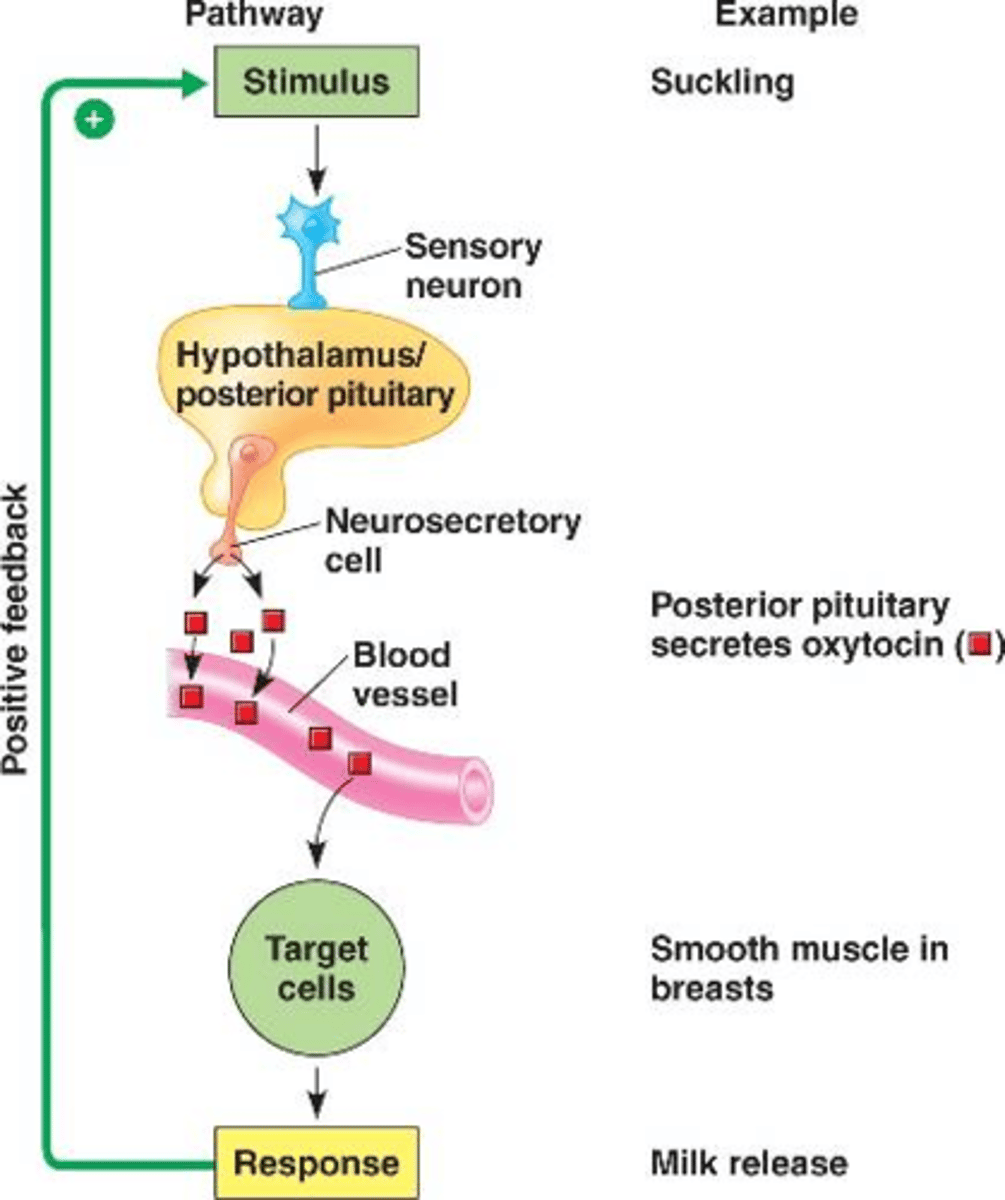
Neurohormone (neuroendocrine): (this hormones(ligands) are secreted by the neurosecretory cell of the posterior pituitary gland, then via neurons are released into the blood stream. any hormone that comes from the posterior pituitary gland is a neurohormone)
- The ligand is released by a neuron into the blood stream.
-Ex: Antidiuretic hormone (ADH) is synthesized by neurosecretory cells of the posterior pituitary gland.
Cytokines:
-are secreted by different cells; including white blood cells(WBC)
-have immune function
-are secreted into the ISF; and diffuses to target
classification of ligands: Autocrine:
-it regulates its own cellular activity (usually inhibitory; ultra short negative feed-back loop) by secreting ligands into ISF; these ligands diffuse back to its self.
-its fast acting
-has short live
7 classifications of ligands:
1-Autocrine
2-paracrine
3-endocrine
4-neurotransmitters
5-Hormones
6-Neurohormones/ Neuroendocrine
7-Cytokines
classification of ligands: Paracrine:
- It regulates a neighboring cell's activity by secreting ligand into ISF; which diffuses into neighbor cells.
- is fast acting
- has short live
-example: the delta cells of the pancreas modulate the production of glucagon and insulin through somatostatin.
.Alpha cells secrete glucagon
.Beta cells secrete insulin
.Delta cell secrete somatostatin
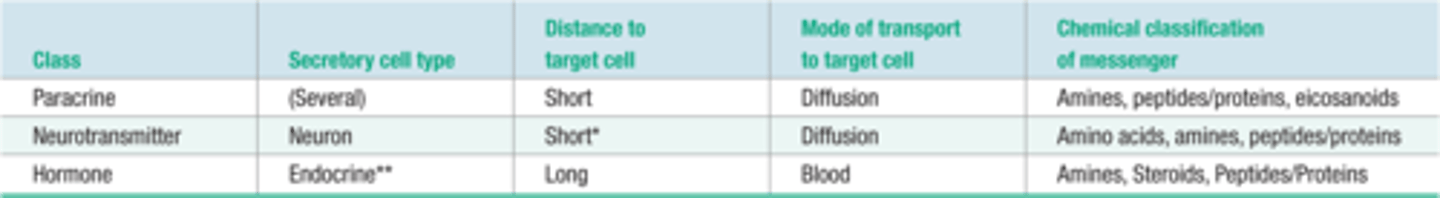
classification of ligands: Endocrine:
-it regulates a distant(far away) target cells by releasing a hormone into the bloodstream.
-they take a longer time to action when compared to autocrine and paracrine ligands.
-it has longer half-life when compared to autocrine and paracrine.
classification of ligands: Neurotransmitters
-Ligand is released into ISF from neurons (from the axon terminals into the synapse cleft)
-ligand is released by axon terminal
-it can affect another neuron or other cell type;
.Presynaptic neuron, then to synapse, then, to postsynaptic neuron.
. Neuromuscular junction (this is and example of when motor neuron transmit a signal to the muscle fiber, causing muscle contraction. this is called neuromuscular junction)
classification of ligands: Hormones:
- Are distributed (sent) to the entire body but will only affect the cells that have the proper receptor.(the receptor for such hormone. Ex: ADH is sent to the entire body, but it will only affect DCT because is the only part that has a receptor for ADH)

classification of ligands: Neurohormone (neuroendocrine):
- The ligand (hormone) is released by a neuron into the blood stream.
-Ex: Antidiuretic hormone (ADH) is synthesized by neurosecretory cells of the posterior pituitary gland. (any hormone that is secreted by the posterior pituitary gland is a neurohormone)
classification of ligands: Cytokines:
-are secreted by different cells; including white blood cells(WBC)
-have immune function
-are secreted into the ISF; and diffuses to target( cytokines are similar to ligands; except that cytokines are more like chemical signals that are used between white blood cells to communicate when there are pathogens that need to be destroyed)
(extra)
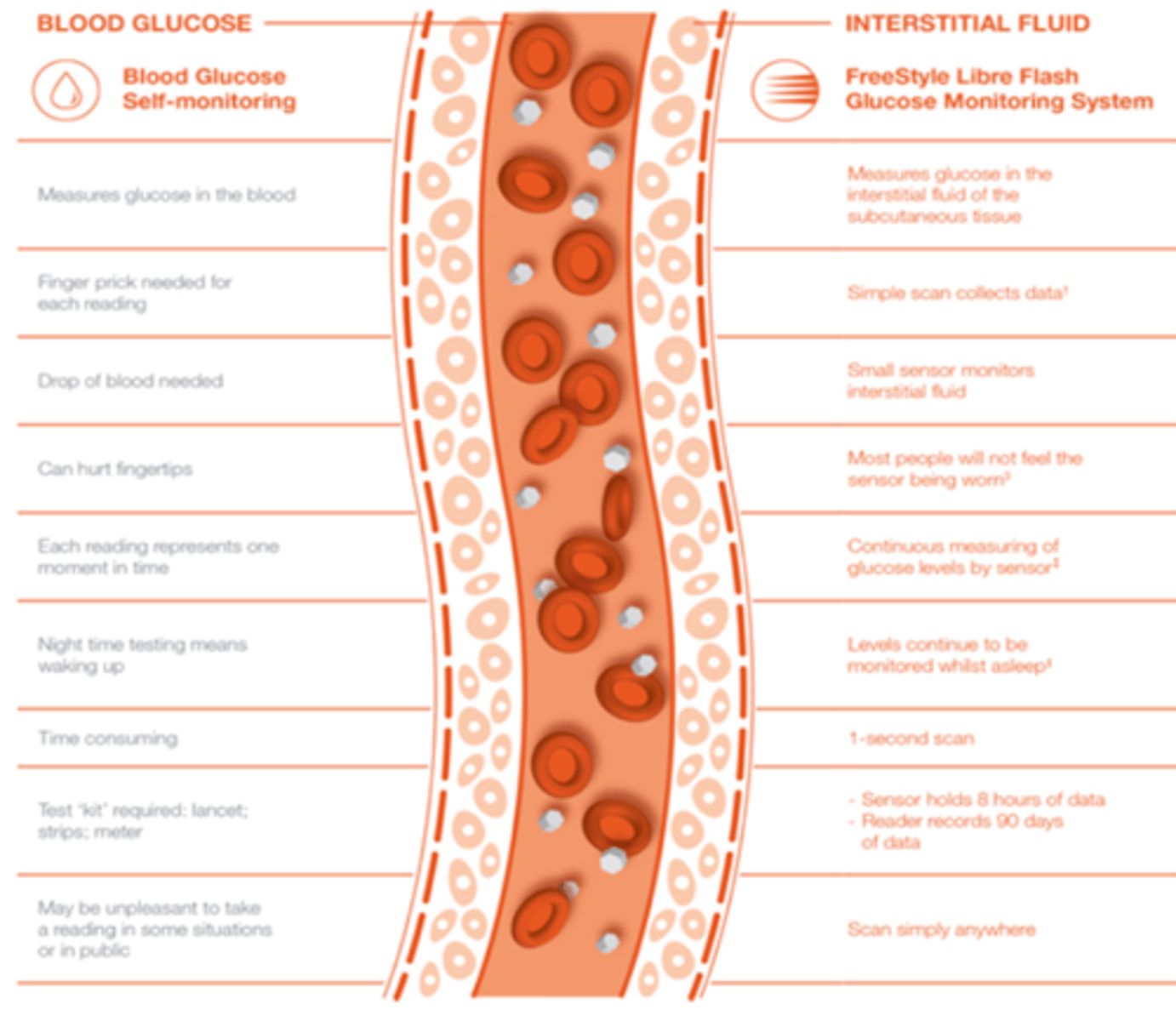
Interstitial fluid (ISF) vs blood
(using glucose as an example)
Blood and ISF differ in a number of aspects with respect to glucose: blood transfers glucose to all body sites while ISF transfers glucose to cells; blood is (relatively) easily accessible whereas ISF is tricky to access; BG levels can be measured with a high reliability—something that is more difficult with ISF
(this is part of the class material, but for this exam is not needed to memorize them)
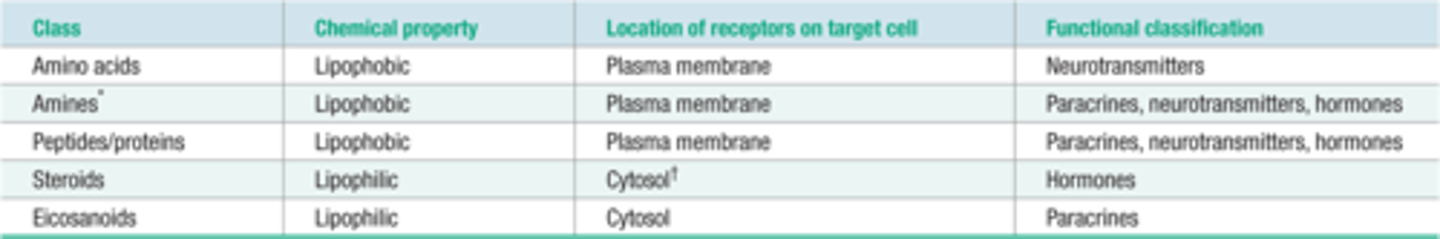
Chemical classes of ligands: (black are lipophobic/hydrophilic and blue shaded color are lipophilic/ hydrophobic)
(black are lipophobic/hydrophilic and blue are lipophilic/ hydrophobic)
1-Amino acids
2-Amines
3-proteins/peptides
4-Steroids
5-Eiconsanoids
Amino acids:
-They act as neurotransmitters (they follow the whole pattern of any neurotransmitter that is released by neurons)
-Are synthesized inside of neurons (since they are acting as neurotransmitters, and neurotransmitters are known to be released by neurons)
-Are stored in vesicles until needed; then released by exocytosis
-Examples of Amino acids are: Glutamate, Aspartate, Glycine, and GABA (gamma-aminobutyric acid)
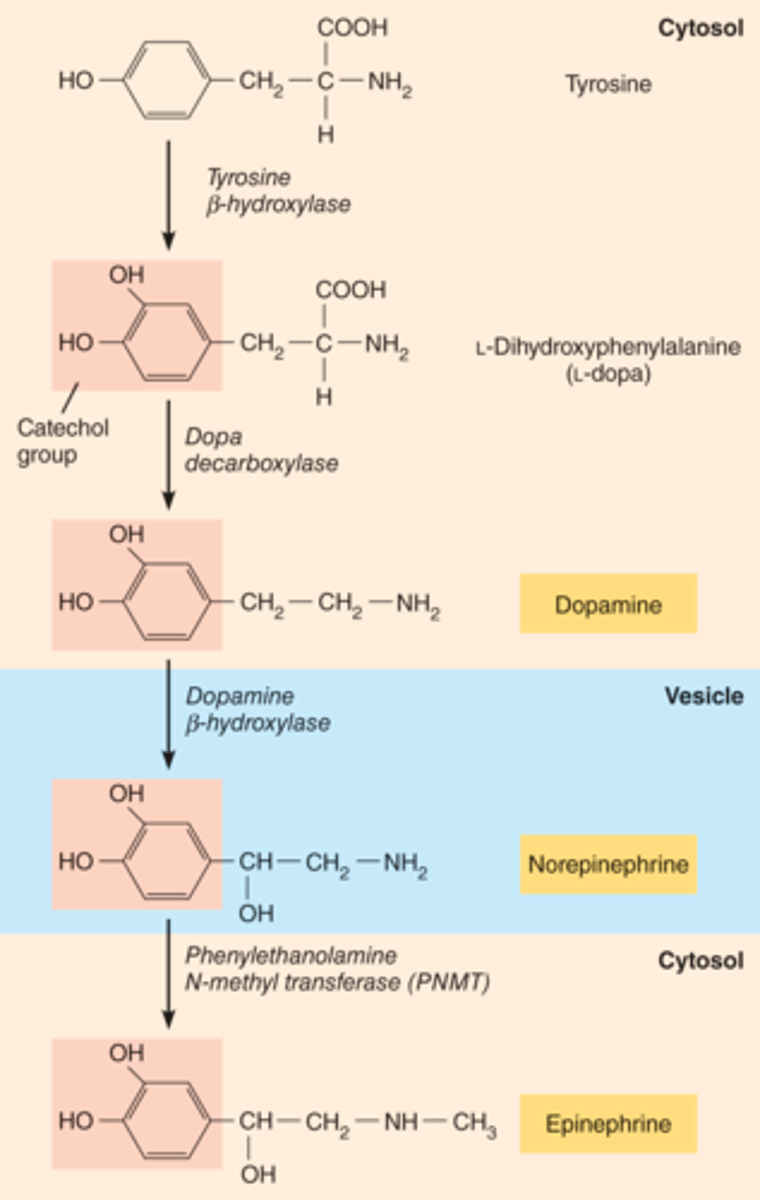
Amines:
-Are derived from Amino acids (AA)
-Are synthesized in the cytosol ( are created by enzymatic reactions in the cytosol)
-Are stored in vesicles until they are needed; then are released via exocytosis.
-Examples or Amines are: catecholamines: which are Norepinephrine (neurotransmitter), Epinephrine(hormone), Dopamine (neurotransmitter), Serotonin (neurotransmitter).
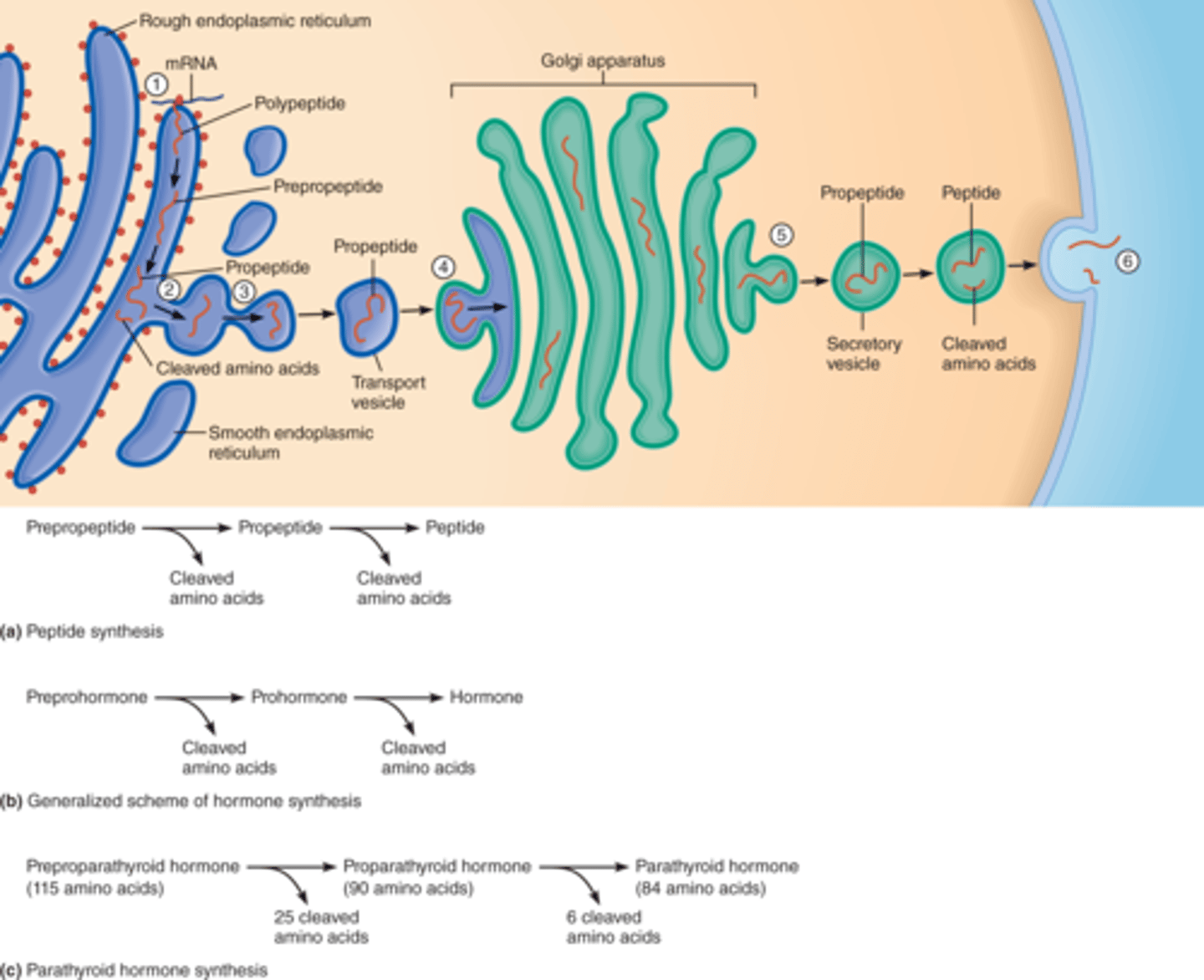
Peptides:
-are a huge class of ligands which includes: Hormones Neurotransmitters, cytokines.
-They are synthesized by classical transcription and translation ( by ribosomes at the Rough endoplasmic reticulum (RER))
-They are stored in vesicles until they are needed; then when needed the will be released via exocytosis.
-They are classified according to their size.
-Examples of peptides are: Insulin and Antidiuretic hormone (ADH).
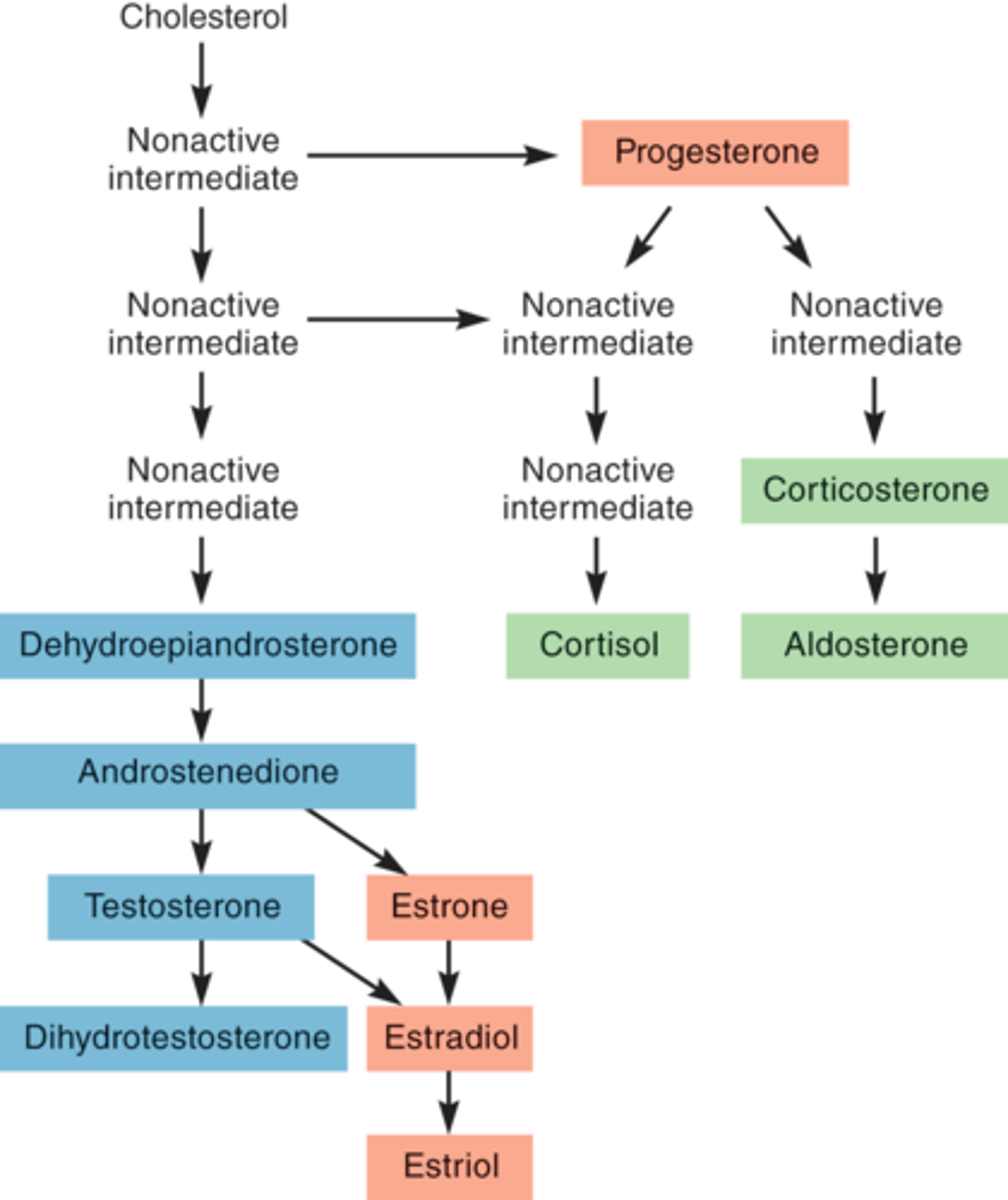
Steroids:
-They are derived from cholesterol; by series of enzymatic reactions, cholesterol is converted into the desired steroid.
-They are synthesized on demand(when they are needed) and immediately released. (since they are needed at that very moment (on demand))
-THEY CANNOT BE STORED INSIDE OF THE CELL. when they are made, they diffuse to outside of the cell.
-They are lipophilic(love fat and hate water).
-Examples of steroids are: Aldosterone, Testosterone, estrogen.
Eicosanoids:
-Are paracrines that are secreted by many different cell types.
-Are synthesized on demand(when they are needed) and then are immediately released(since they are needed at that very moment (on demand)).
-THEY CANNOT BE STORED INSIDE OF THE CELL.
-They are lipophilic(love fat and hate water).
-Examples of Eicosanoids are: Prostaglandins.
5 Chemical classes of ligands
(black are lipophobic/hydrophilic and blue are lipophilic/ hydrophobic)
1-Amino acids
2-Amines
3-proteins/peptides
4-Steroids
5-Eiconsanoids
Chemical classes of ligands: Amino acids
-They act as neurotransmitters
-Are synthesized inside of neurons
-Are stored in vesicles until needed; then released by exocytosis(from axon terminals)
-Examples of Amino acids are: Glutamate, Aspartate, Glycine, and GABA (gamma-aminobutyric acid)
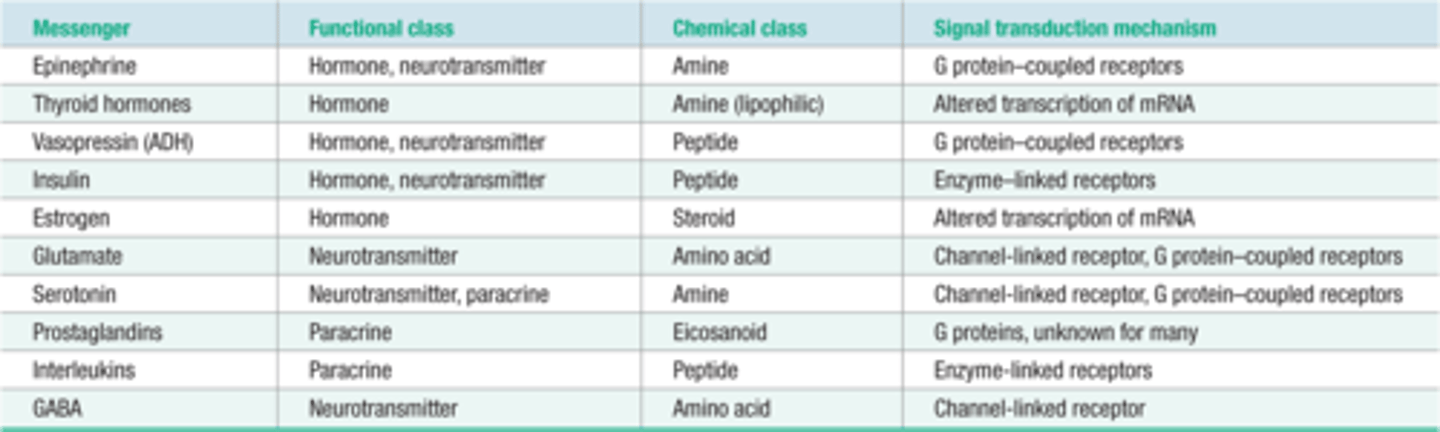
Chemical classes of ligands: Amines
-Are derived from Amino acids (AA)
-Are synthesized in the cytosol ( are created by enzymatic reactions)
-Are stored in vesicles until they are needed; then are released via exocytosis.
-Examples or Amines are: catecholamines: which are Norepinephrine (neurotransmitter), Epinephrine(hormone), Dopamine (neurotransmitter), Serotonin (neurotransmitter).
Chemical classes of ligands: Peptides
-are a huge class of ligands which includes: Hormones Neurotransmitters, cytokines.
-They are synthesized by classical transcription and translation ( by ribosomes at the Rough endoplasmic reticulum (RER))
-They are stored in vesicles until they are needed; then when needed the will be released via exocytosis.
-They are classified according to their size.
-Examples of peptides are: Insulin and Antidiuretic hormone (ADH).
Chemical classes of ligands: Steroids
-They are derived from cholesterol; by series of enzymatic reactions, cholesterol is converted into the desired steroid.
-They are synthesized on demand(only when they are needed) and immediately released. (since they are needed at that very moment(are on demand)
-THEY CANNOT BE STORED INSIDE OF THE CELL. when they are made, they diffuse to outside of the cell.
-They are lipophilic(love fat and hate water).
-Examples of steroids are: Aldosterone, Testosterone, estrogen.
Chemical classes of ligands: Eicosanoids
-Are paracrines that are secreted by many different cell types.
-Are synthesized on demand(when they are needed) and then are immediately released(because they are needed at that very time).
-THEY CANNOT BE STORED INSIDE OF THE CELL.
-They are lipophilic(love fat and hate water).
-Examples of Eicosanoids are: Prostaglandins.
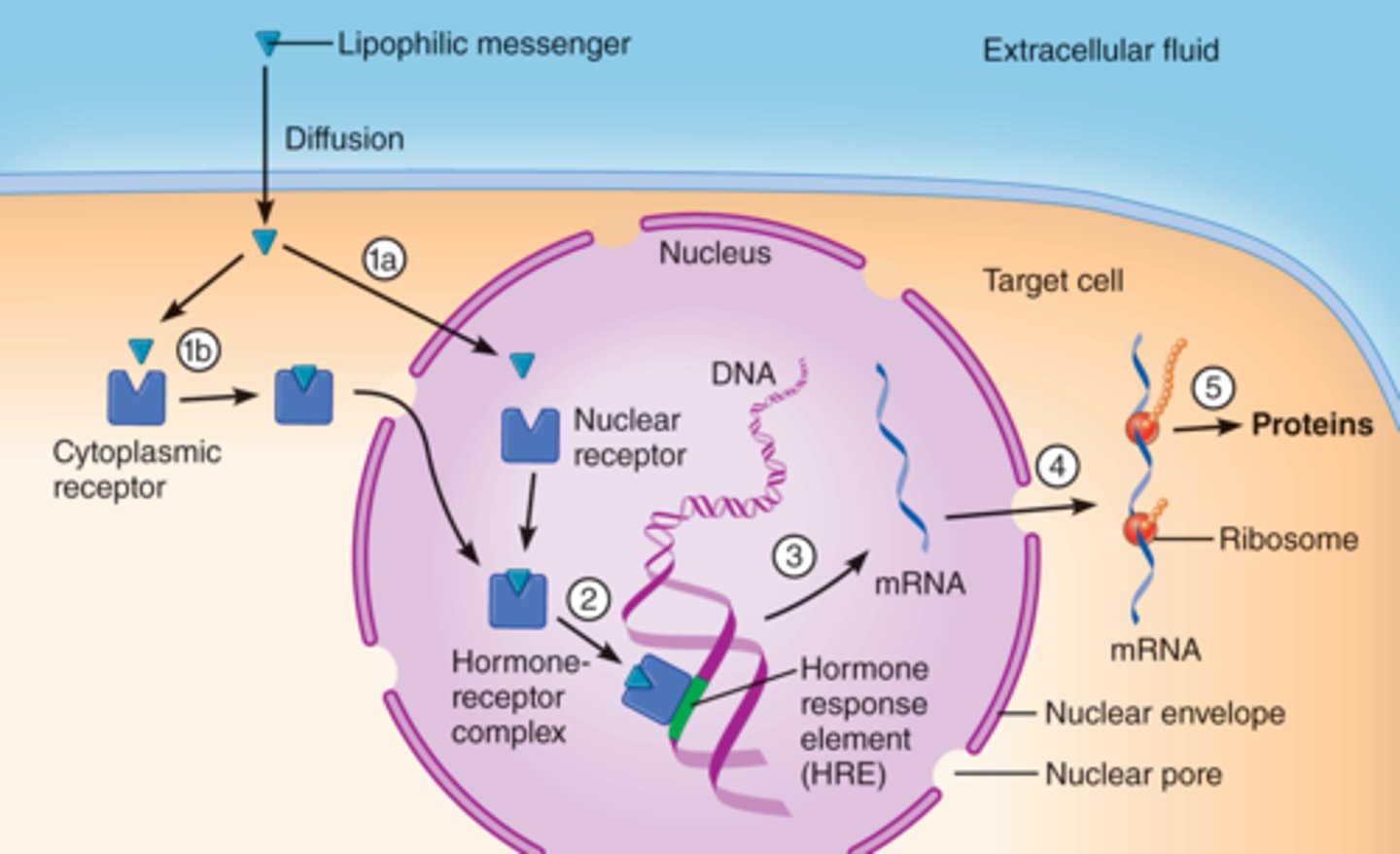
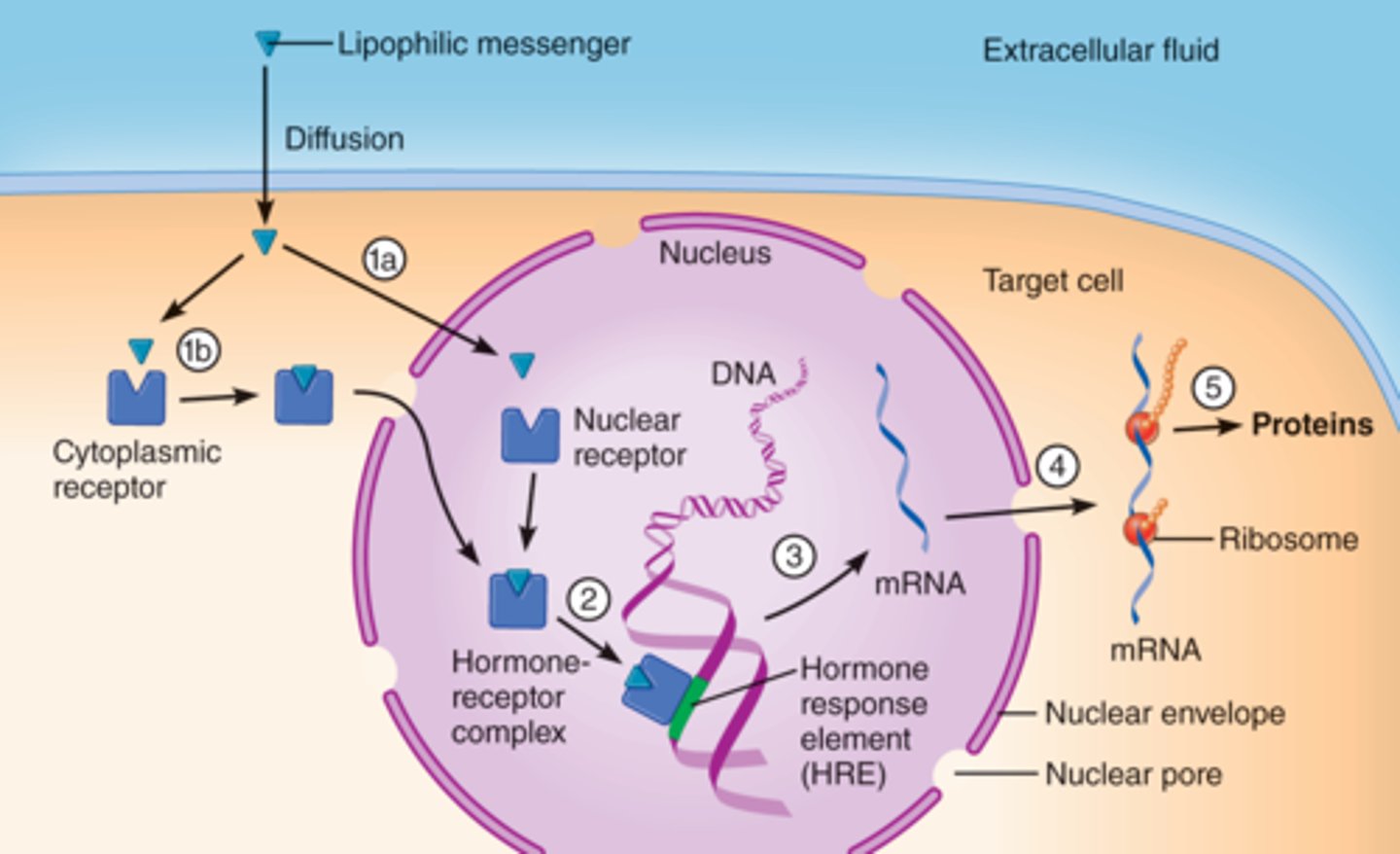
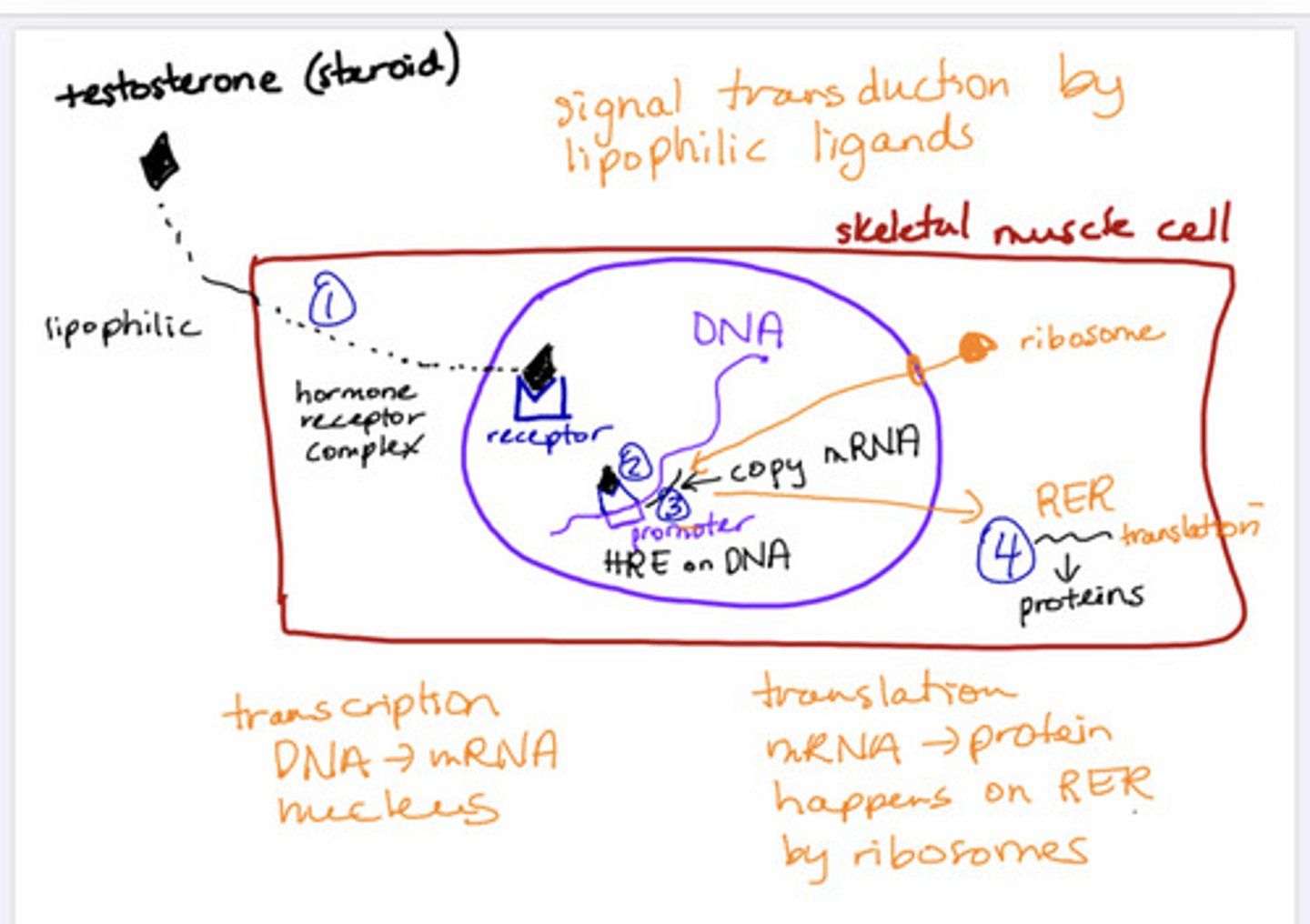
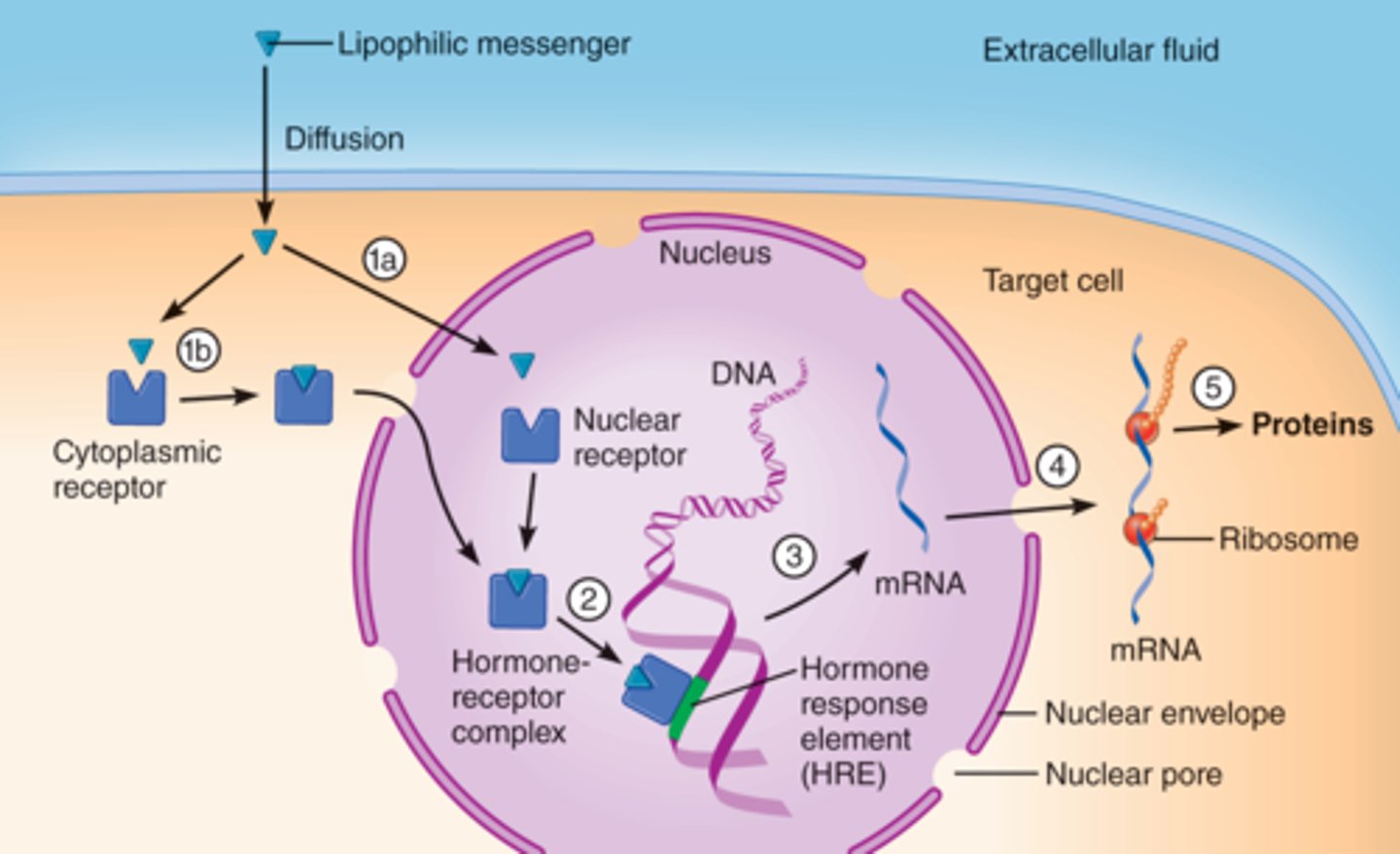
how do Steroids and Eicosanoids work? Steroid action
1- steroid diffuses through cell and binds to its receptor in the nucleus (nuclear receptor)= which is the hormone receptor complex (HR)
2-Then the HR binds to DNA to drive transcription of a particular gene:
. HR binds to hormone response element (HRE)
.HRE is located at the starting sequence of the desired gene.
3-Then transcription proceeds: to mRNA, then mRNA travels into the cytosol.
4- Then translation proceeds: (at the Rough endoplasmic reticulum, with the aid of ribosomes.)
how do Steroids and Eicosanoids work?
Steroid action:
1- steroid diffuses through cell and binds to its receptor in the nucleus (nuclear receptor)= which is the hormone receptor complex (HR) (hormone receptor complex means, that the ligand is bound to the hormone receptor)
2-Then the HR binds to DNA to drive transcription of a particular gene:
. HR binds to hormone response element (HRE)
.HRE is located (close to the promotor)at the starting sequence of the desired gene.
3-Then transcription proceeds: to mRNA, then mRNA travels into the cytosol.
4- Then translation proceeds:
EX; HRE binds to the DNA, close to the promotor, and stars transcription.
then DNA to mRNA= transcription
Then mRNA to Protein = translation.
Eicosanoid action:
1-Eicosanoids bind to their hormone receptors in the cytosol (HR)
2-then the Hormone receptor (HR) diffuses(crosses) into the nucleus.
3-Then the HR(hormone receptor NOT the eicosanoid but HR) binds to the DNA , at the HRE (which is located close to the promotor) to drive the transcription of a particular gene:
.the hormone receptor binds to the hormone response element (HRE)
.The hormone receptor element(HRE) it is located at the starting sequence of the desired gene (which means that here is where the transcription will begin. the Golgi apparatus reads the HRE to know where to send that specific protein).
4-Then the transcription proceeds: mRNA then the mRNA travels from the nucleus into the cytosol.
5-Then in the cytosol translation proceeds:
EX; HRE binds to the DNA, close to the promotor, and stars transcription.
then DNA to mRNA= transcription
Then mRNA to Protein = translation.
what is hormone receptor complex (HRC)?
it simply means: nuclear receptor together with the ligand.
steroid receptor location vs eicosanoid receptor location:
-the steroid's receptor is located in the nucleus
- the Eicosanoid's receptor is located in the cytosol.(after binding to the HR, the HR travel into the nucleus).
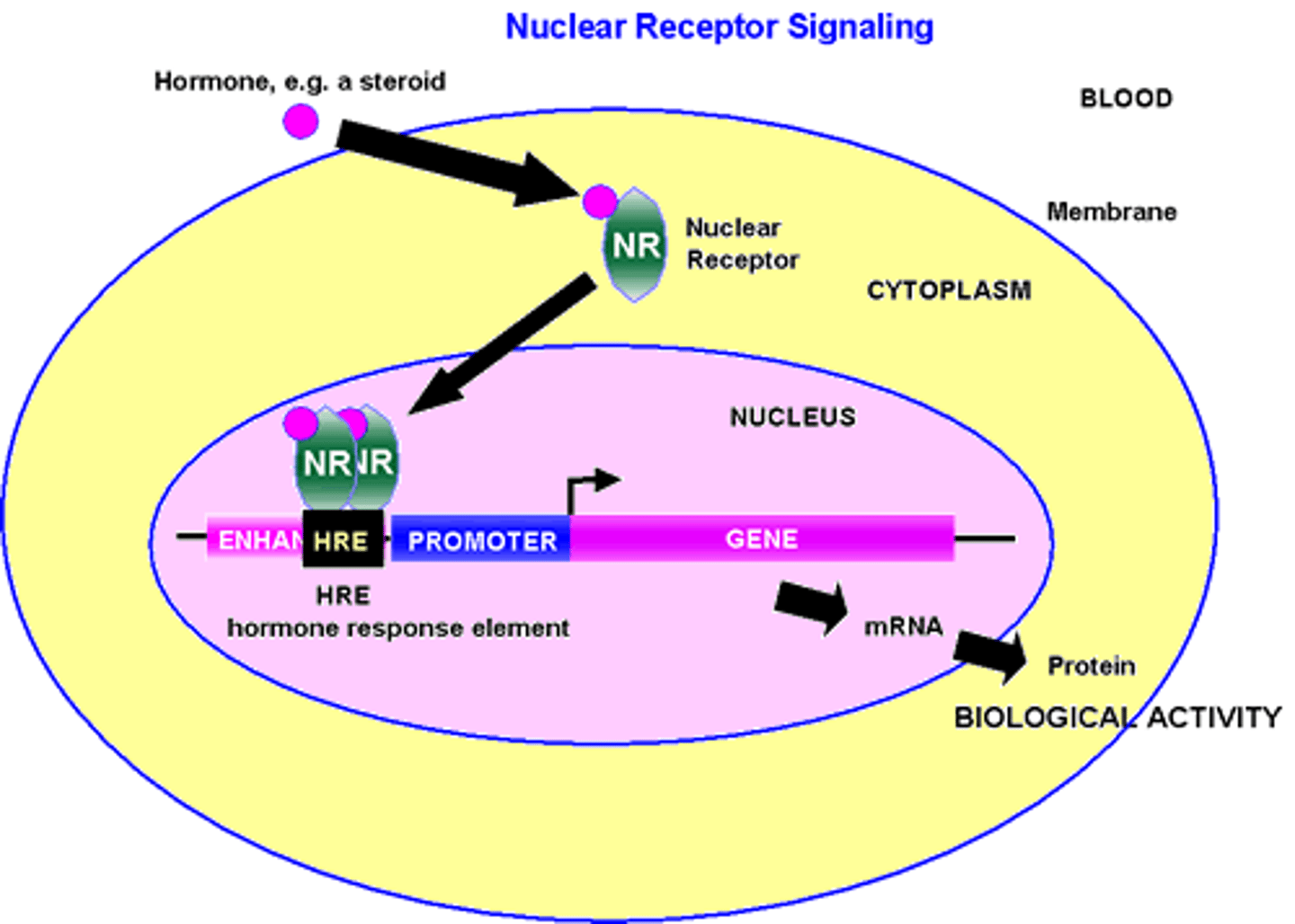
lipophilic ligands (sterols) interaction with DNA vs lipophobic ligands( proteins) interaction with DNA
-Lipophilic ligands do business directly with the DNA, since their cell receptors are located in the nucleus, right where the DNA is allocated.
-Lipophobic ligands can not do business directly with the DNA; they need some help getting to where the DNA is located, since their cell receptors are on the plasma membrane.
how do Steroids and Eicosanoids work? Eicosanoid action
1-Eicosanoids bind to their hormone receptors in the cytosol (HR)
2-then the Hormone receptor (HR) diffuses(crosses) into the nucleus.
3-Then the HR(hormone receptor NOT the eicosanoid but HR) binds to the DNA (at the HRE) to drive the transcription of a particular gene:
.the hormone receptor binds to the hormone response element (HRE)
.The hormone receptor element(HRE) it is located at the starting sequence of the desired gene (which means that here is where the transcription will begin. HRE is what the Golgi apparatus read to know where to send the protein).
4-Then the transcription proceeds: mRNA then the mRNA travels from the nucleus into the cytosol.
5-Then in the cytosol translation proceeds: From mRNA to protein by the ribosome.
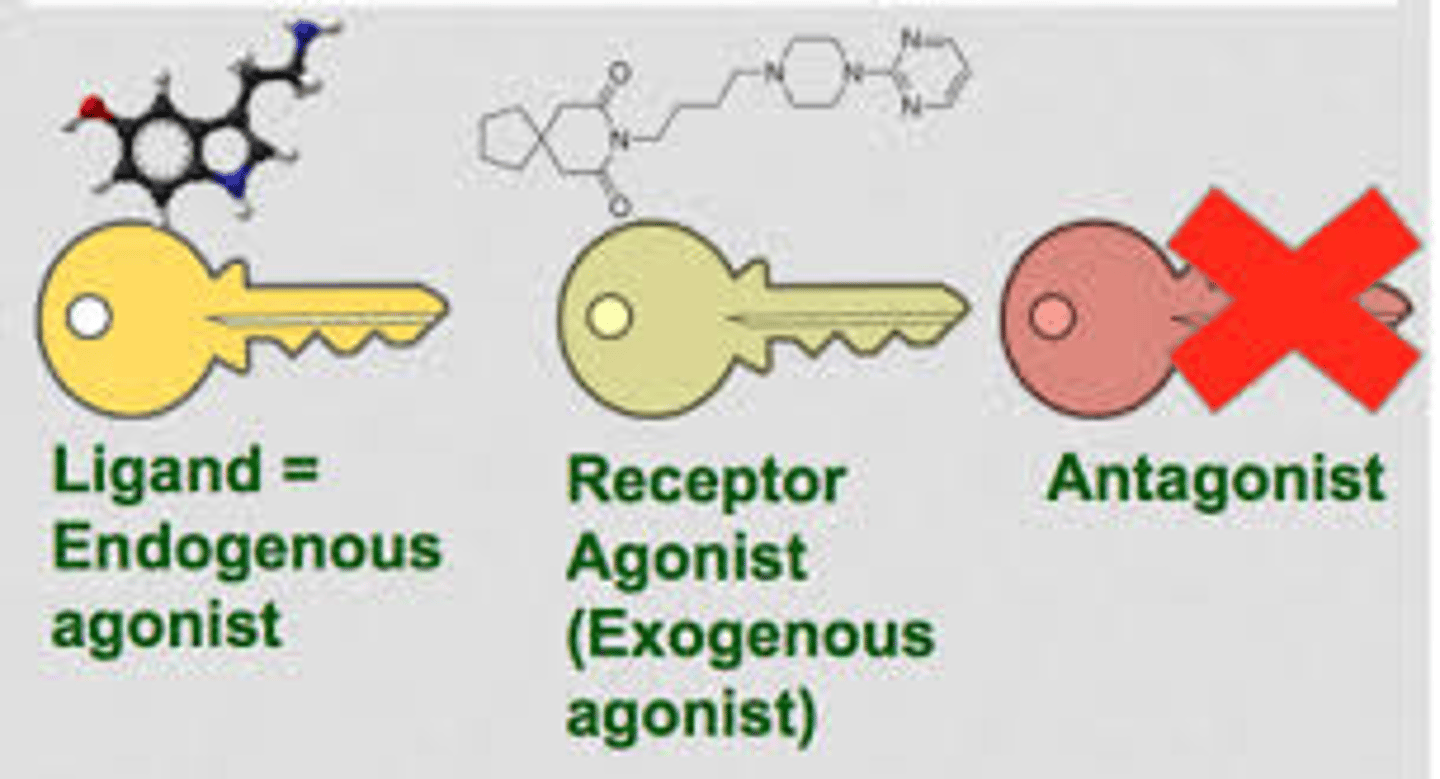
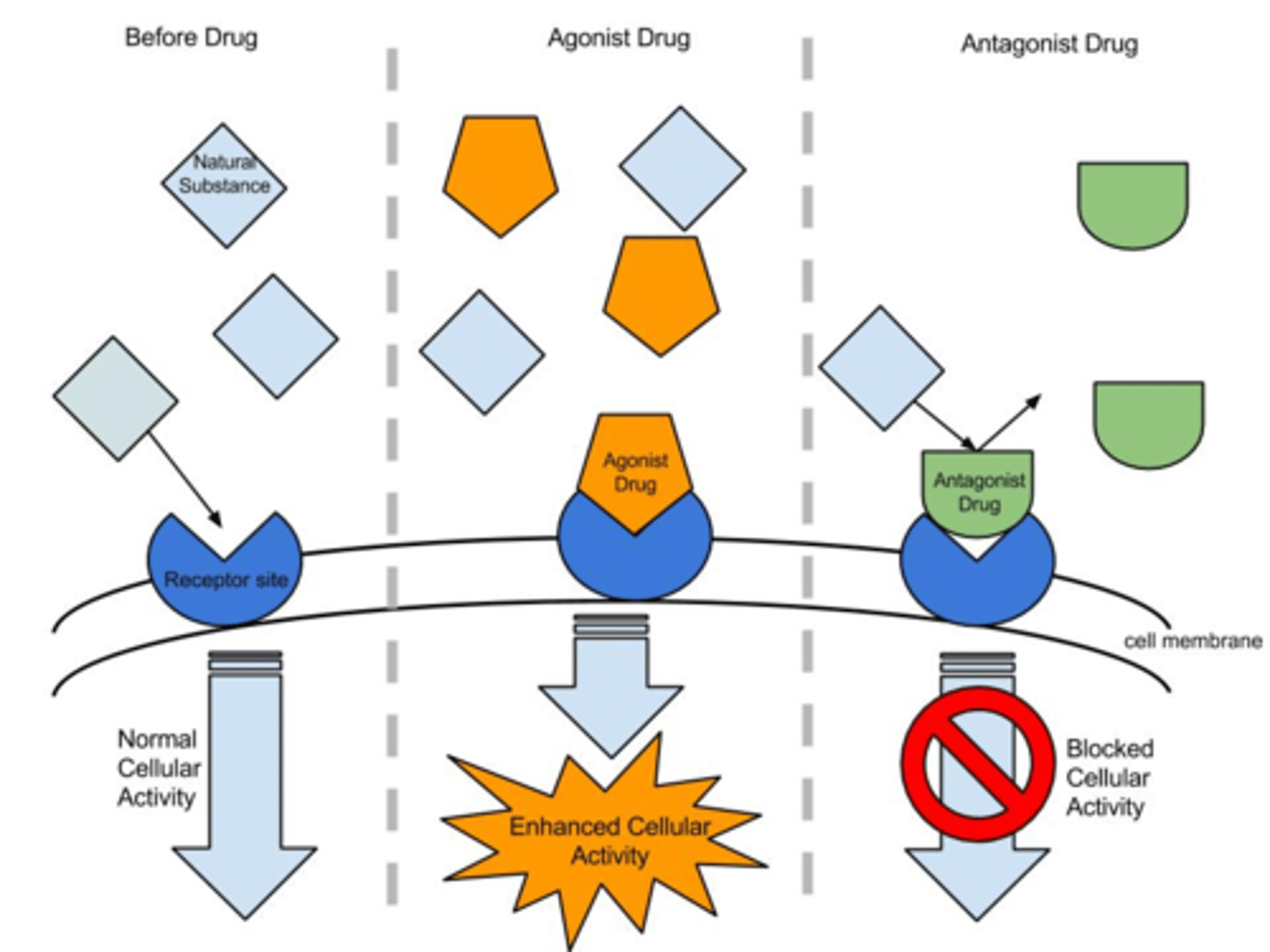
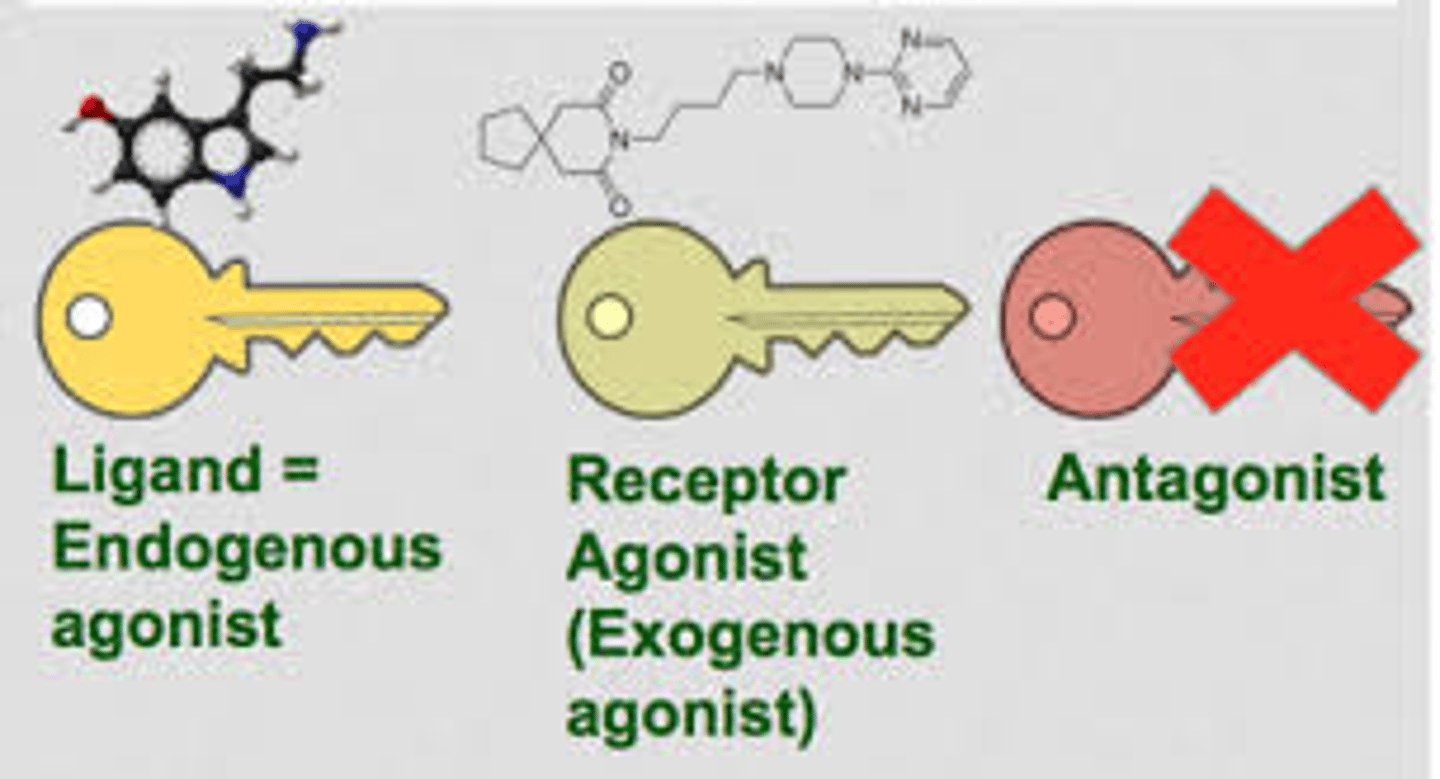
Concept of agonist and antagonist:
-An Agonist: is a ligand that induces a physiological response. (this agonist can be the natural ligand or a replacement of the natural ligand by an exogenous ligand; as long as it is inducing the decided physiological response)
-An Antagonist: is a compound that competes with an agonist(ligand) for a given receptor but it does not induce a physiological response/it only inhibits the physiological response( this is a type of competitive inhibition; similar, in concept, to sulfanilamide competitive inhibition PABA in bacteria)
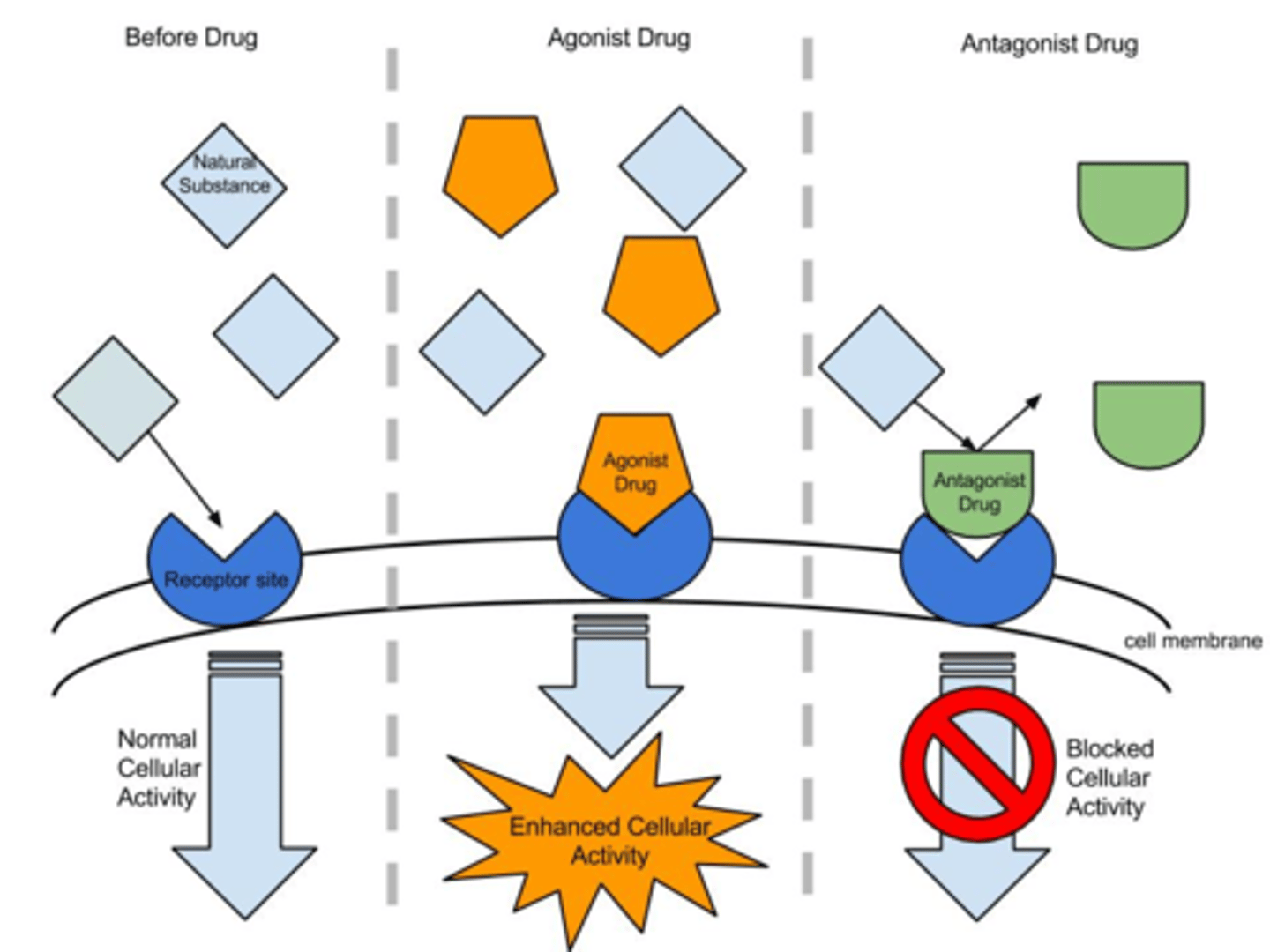
Concept of agonist and antagonist: An Agonist
is a ligand that induces a physiological response.
(this agonist can be the natural ligand or a replacement of the natural ligand by an exogenous ligand; as long as it is inducing the decided physiological response)
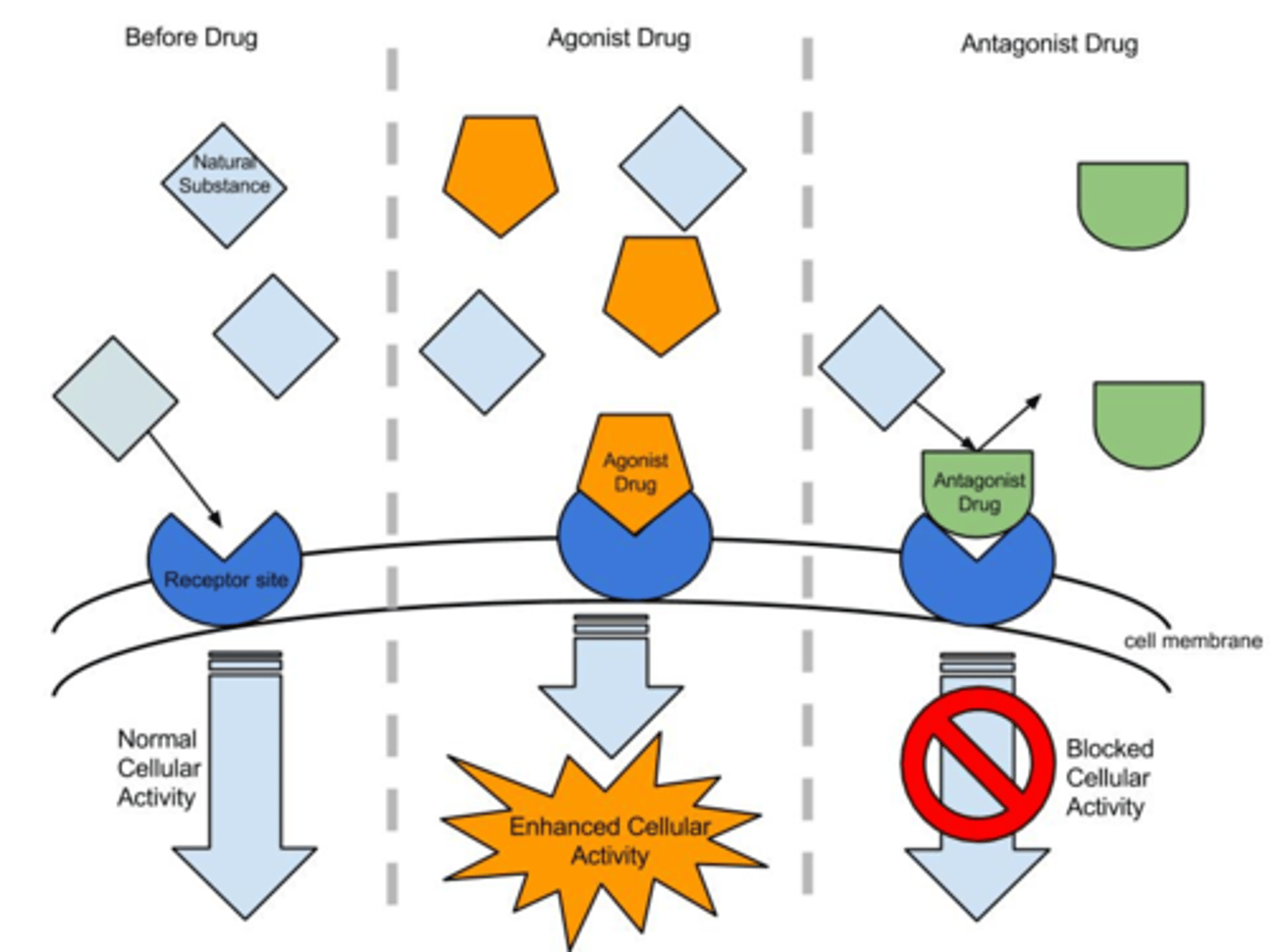
Concept of agonist and antagonist: An Antagonist
is a compound that competes with an agonist(ligand) for a given receptor but it does not induce a physiological response/it inhibits the physiological response( this is a type of competitive inhibition; similar, in concept, to sulfanilamide competitive inhibition PABA in bacteria and in humans an Ex: is Angiotensin converter enzyme (ACE) inhibitors, ACE is an exogenous antagonist that inhibits the the formation of angiotensin 1 into angiotensin 2)
concept of exogenous and endogenous:
-Exogenous: comes from outside of the body( ex: exogenous insulin, is a synthetic made insulin that is administered to patients that their body cannot make its own insulin; so this insulin that comes from the outside is an exogenous agonist).
-Endogenous: Produced by the body (ex: insulin in healthy patients, is made by the body. the body makes it by its self).
how are these concepts of antagonist and agonist- and-exogenous and endogenous, used in medicine?
Example of exogenous agonist:
-Type 1 diabetics take insulin, this is an exogenous agonist.
-Asthma patients take inhalers, these are exogenous agonists of epinephrine (which will dilate the airway, so that patients can breath)
Example of exogenous antagonist:
-Hypertensive(high blood pressure) patients take exogenous antagonist of the RAAS cascade and epinephrine. (when the RAAS cascade is inhibited, it prevents the formation of angiotensin 2 which constrict blood vessels( since it is a powerful constrictor) and increases the blood pressure and also the formation of aldosterone which induces the reabsorption of sodium and water into blood to increase blood pressure and concentration. Epinephrine is released in situations of fight or flight response; epinephrine will also constrict blood vessels to increase blood pressure and flow to the parts that where it is needed to either get involve in the fight or flight away; never the less Hypertensive patients already have their blood pressure high and if the RAAS cascade and epinephrine which are normal body processes are not inhibited, their blood pressure will go higher than what already is, and will make their heart work very hard and possible experience a heart attack due to too much pressure).
what other processes could medicine target to increase or prevent the physiological response to a given ligand?
Medications for type 2 diabetes increases the cell signal cascade to up-regulate GLUTs(glucose transporters) without using insulin (stimulate tyrosine kinase directly). (this is an exogenous agonist.)
Example of exogenous agonist:
-Type 1 diabetics take insulin, this is an exogenous agonist.
-Asthma patients take inhalers, these are exogenous agonists of epinephrine (which will dilate the airway, so that patients can breath)
Example of exogenous antagonist:
-Hypertensive(high blood pressure) patients take exogenous antagonist of the RAAS cascade and epinephrine. -Hypertensive(high blood pressure) patients take exogenous antagonist of the RAAS cascade and epinephrine. (when the RAAS cascade is inhibited, it prevents the formation of angiotensin 2 which constrict blood vessels( since it is a powerful constrictor) and increases the blood pressure and also the formation of aldosterone which induces the reabsorption of sodium and water into blood to increase blood pressure and concentration. Epinephrine is released in situations of fight or flight response; epinephrine will also constrict blood vessels to increase blood pressure and flow to the parts that where it is needed to either get involve in the fight or flight away; never the less Hypertensive patients already have their blood pressure high and if the RAAS cascade and epinephrine which are normal body processes are not inhibited, their blood pressure will go higher than what already is, and will make their heart work very hard and possible experience a heart attack due to too much pressure).