Control of Ventilation
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
22 Terms
PCO2 levels in the peripheral blood that are…
Too high: hypercapnia
Too low: hypocapnia
Reduced levels of O2…
In the tissues or a specific tissue: hypoxia
In peripheral blood (PO2): hypoxemia
Blood pH that is too…
Low (high CO2): acidosis
High (low CO2): alkalosis
Heart rate that is…
Slow: bradycardia
Rapid: tachycardia
Neural control of ventilation can be…
Involuntary and voluntary
Involuntary neural control of ventilation
ANS influences bronchioles
PNS: acetylcholine causes bronchoconstriction
SNS: norepinephrine causes bronchodilation
Several centers located in the medulla oblongata and pons
Control expired minute volume → adjust frequency and depth of ventilation
Receive info from lungs/respiratory tract/body
Voluntary neural control of ventilation
Cerebral cortex can regulate both:
Respiratory centers in medulla and pons
Motor neurons that innervate the respiratory muscles
Big picture neural control of ventilation
Respiratory control centers are located in the medulla oblongata and pons
Efferent pathways: motor neurons to the muscles of respiration
Afferent signals:
Chemoreceptors located in the brain (central) and periphery (aortic and carotid bodies)
Mechanoreceptors in lung and muscle
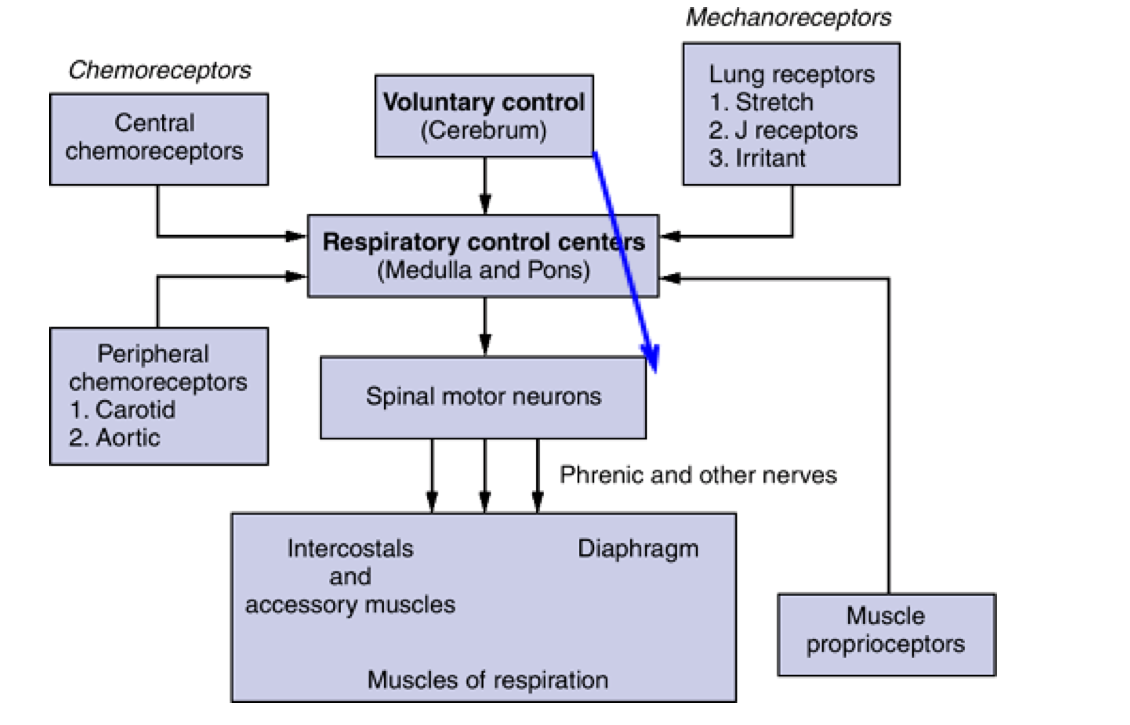
Medulla oblongata → directly control the muscles of ventilation
Respiratory rhythmicity centers (a pair of centers)
DRG and VRG
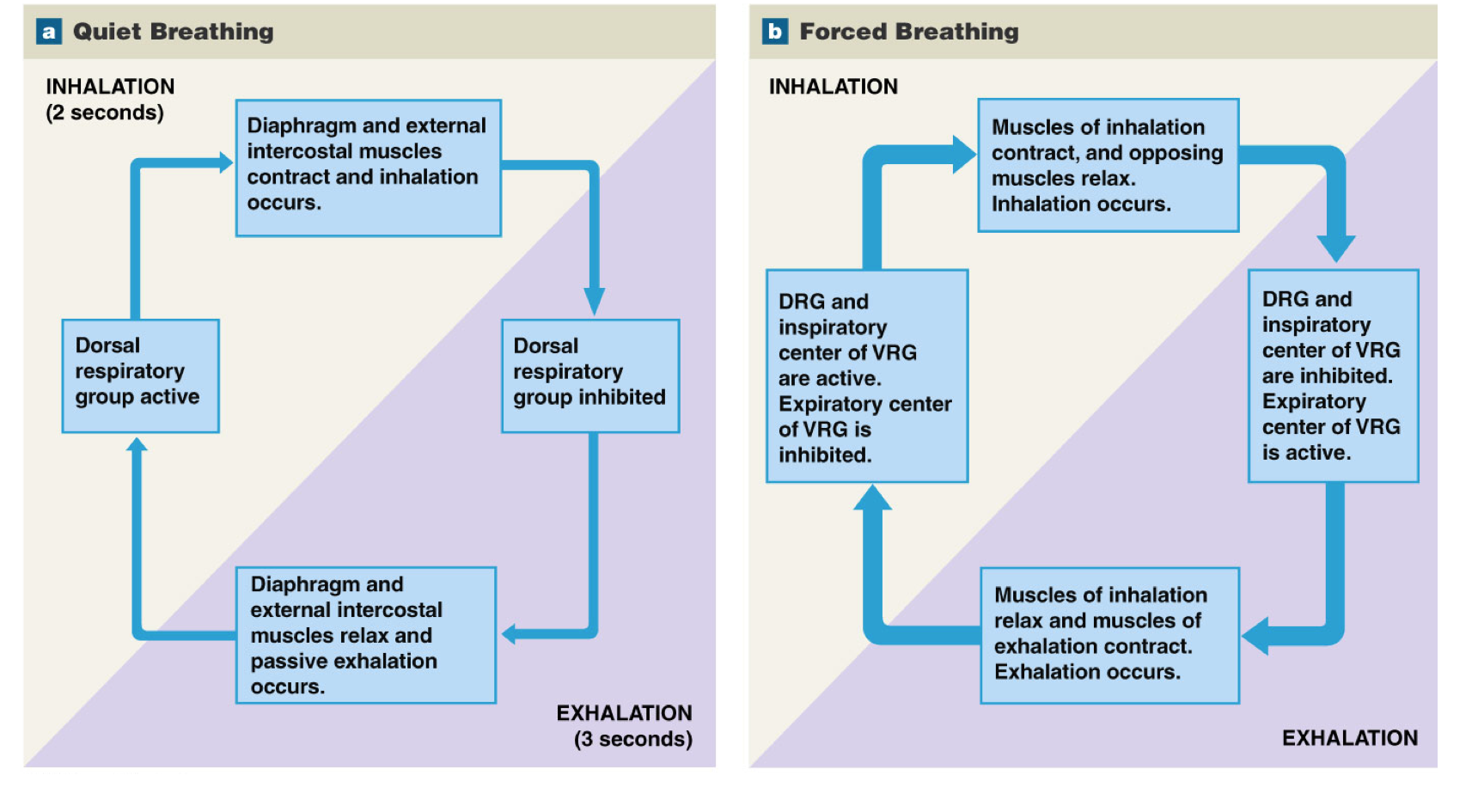
DRG
Dorsal respiratory group
Functions in every respiratory cycle
Neurons regulating inspiration
Controlling motor neurons to external intercostals and diaphragm
Predominant role in integrating afferent input
VRG
Ventral respiratory group
Functions only during forced breathing
Expiratory center: controls accessory motor neurons used during forced exhalation
Inspiratory center: controls accessory motor neurons used during forced inhalation
Cerebrum and pons
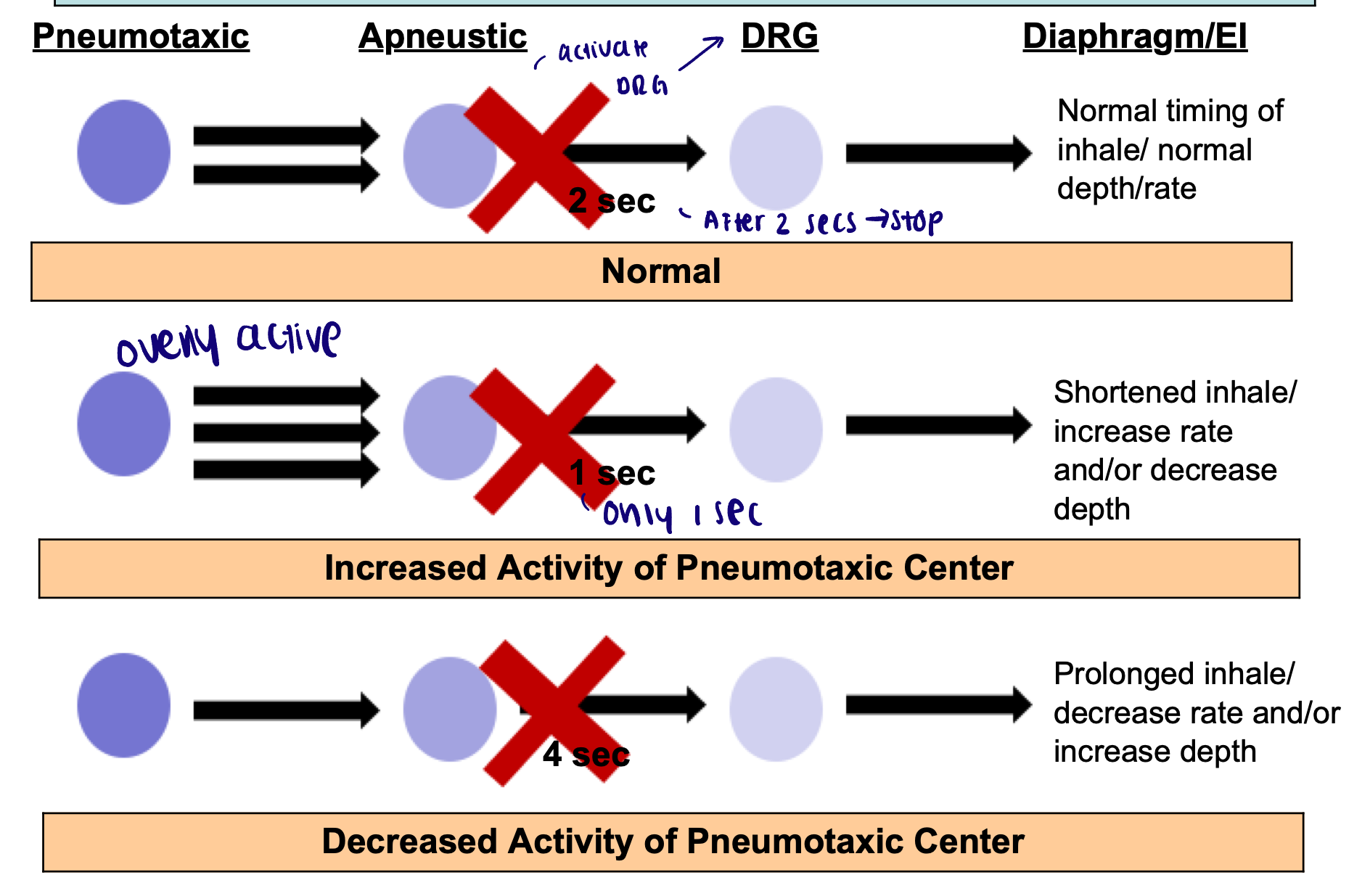
Pontine respiratory centers: regulate rate and depth of breath (influenced by sensory and higher center information)
Apneustic center: excites the DRG. Inhibited by pneumotaxic center
Pneumotaxic center: inhibits the apneustic center. Inhibited/excited by higher centers
Pneumotaxic center control
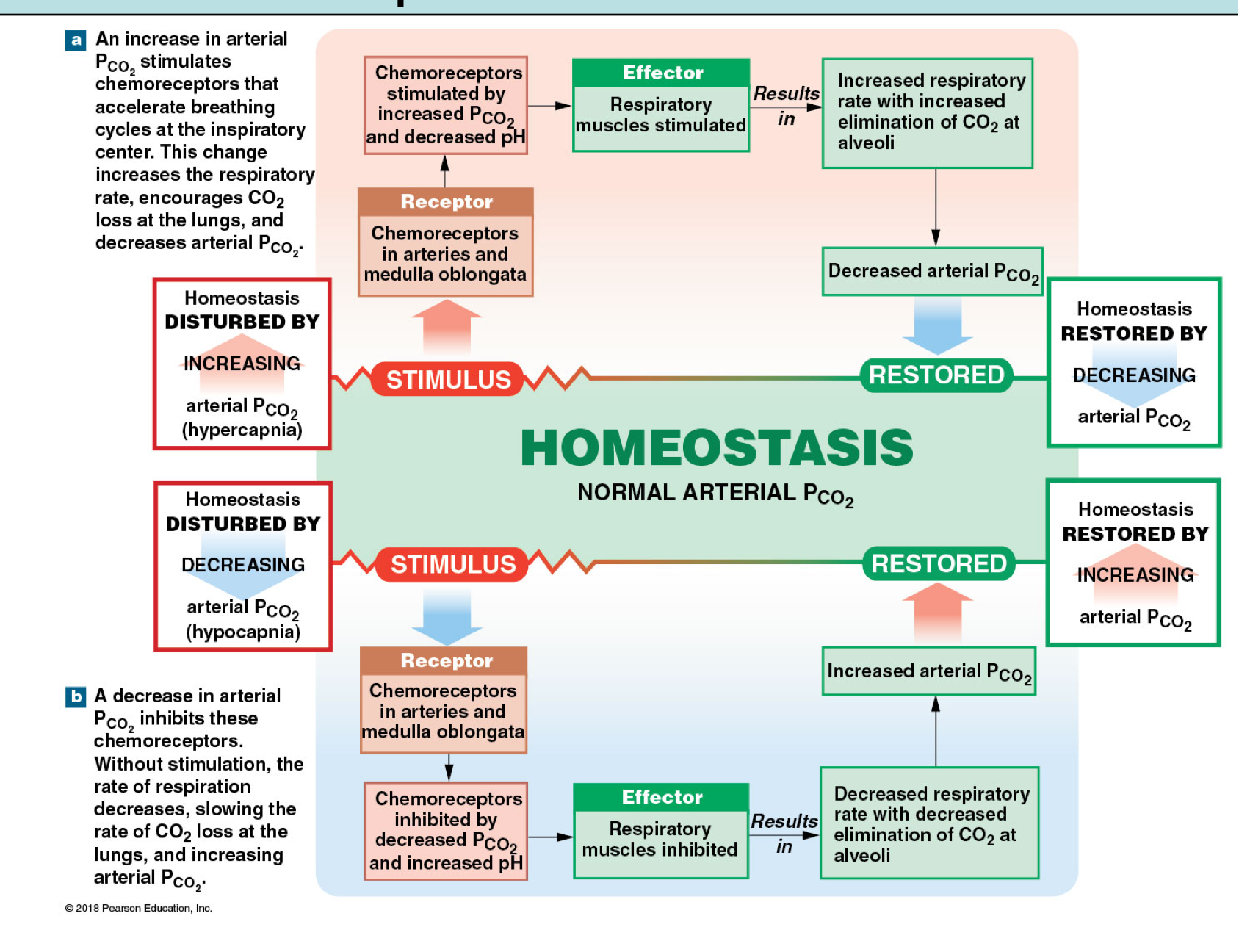
Central chemoreceptors
Hypercapnia will stimulate an increase in ventilation
Diffusion of CO2 into CSF
Note: H+ cannot cross BBB
Formation of H+
Diffusion of H+ into medullary interstitial fluid, stimulation of central chemoreceptor
Increased H+ signals respiratory center to increase ventilation
Increased PaCO2 = hypercapnia
Peripheral chemoreceptors
Hypercapnia and hypoxemia will stimulate an increase in ventilation
Aortic bodies and carotid bodies:
Aortic body (near aortic sinus) → respiratory control centers via vagus nerve
Carotid bodies (near carotid sinus) → respiratory control centers via glossopharyngeal nerve
Sensitive to changes in:
Arterial PO2:
Respond when PO2 drops
Decrease in PaO2 → stimulate ventilation
Arterial pH:
Directly responsive to changes in pH
Increased PaCO2 → decreased pH
Decreased pH → stimulate ventilation
Decreases in pH and PO2 will also stimulate vasomotor and cardiac control centers in medulla oblongata: vasoconstriction and tachycardia
Feedback loop for PCO2 levels in the blood
Hering-Breuer Reflexes
Inflation reflex
Deflation reflex
Inflation reflex
Goal: prevent over expansion of lungs during forced inhale
Sensory: stretch receptors within smooth muscle of bronchioles
Pathway: vagus to respiratory centers
Effect: inhibit DRG, activate expiratory center of VRG
Deflation reflex
Goal: prevent over deflation during forced exhale
Sensor: recoil receptors within the alveolar walls
Pathway: vagus to respiratory centers
Effect: inhibit expiratory center of VRG, activate inspiratory centers
High altitude
Hypoxia
Mount Everest → death zone
Atmospheric Air PO2 = atmospheric pressure FIO2 = 250 × 0.21 = 53 mmHg
Inspired air: PIO2 = (250-47) * 0.21 = 43 mmHg
Exposure to altitude → immediate
Decrease in PIAO2 below 60 mmHg → PaO2 decrease to below 60 mmHg → hypoxemia: stimulates hyperventilation → PaO2 increases but PaCo2 decreases → alkalosis: inhibits ventilation
Net effect: → → ventilation
Note: if only had hypoxia and no alkalosis: → → → ventilation
Also → tachycardia
Altitude: acclimatization (days/weeks)
Kidney: secretes (gets rid of) bicarbonate and conserves H+
Decrease in pH
Counter-acts alkalosis (increased respiration)
Kidney: hypoxia stimulates increased production of erythropoietin
Increased production of red blood cells
Increased oxygen carrying capacity of the blood
RBC: increased production of *BPG
*2,3- bisphosphoglycerate is a metabolite in RBCs that increases with hypoxemia
BPG binds to deoxyhemoglobin
Shifts oxygen-hemoglobin dissociation curve to the right
Facilitates unloading of oxygen to the tissues