Respiratory - Pearson
1/84
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
85 Terms
During inhalation,
the diaphragm and rib muscles contract.
air moves up the trachea.
the diaphragm relaxes.
the volume of the thoracic cavity decreases.
oxygen molecules move into the lungs, and carbon dioxide molecules move out of the lungs.
the diaphragm and rib muscles contract.
From which structures do oxygen molecules move from the lungs to the blood?
Bronchi
Trachea
Nose
Alveoli
Bronchioles
Alveoli
Which statement is correct?
Carbon dioxide diffuses from the alveoli into surrounding capillaries.
Oxygen is released from the mitochondria as a product of cellular respiration.
Oxygen diffuses from large blood vessels into the body's cells.
In the blood, oxygen is bound to hemoglobin, a protein found in red blood cells.
As oxygen diffuses from the lungs into capillaries, blood becomes deoxygenated.
In the blood, oxygen is bound to hemoglobin, a protein found in red blood cells.
After blood becomes oxygenated,
it returns to the heart, and is then pumped to the lungs.
it does not return to the heart, but goes directly to the lungs.
it does not return to the heart, but goes directly to capillaries that supply the body's cells with oxygen.
it does not return to the heart, but goes to the nose and mouth.
it returns to the heart, and is then pumped to body cells.
it returns to the heart, and is then pumped to body cells.
Hemoglobin
- has five subunits.
- is found in blood plasma.
- is a protein that can bind four molecules of oxygen.
- is the site of cellular respiration.
- uses ATP to move oxygen from blood to body cells.
is a protein that can bind four molecules of oxygen.
Which of the following descriptions accurately describes Boyle's law?
The pressure of gas in your lungs is inversely proportional to the volume in your lungs.
How well a gas dissolves in a liquid such as blood depends on both its partial pressure and its solubility.
The partial pressure of a gas in the air you breathe in is equal to the total atmospheric pressure times the fractional concentration of the gas.
The pressure of gas in your lungs is inversely proportional to the volume in your lungs.
Which muscles, when contracted, would increase the volume of air in the thoracic cavity?
internal intercostals and external oblique
diaphragm and external intercostals
diaphragm and internal intercostals
diaphragm and external intercostals
Which pressure is the result of the natural tendency of the lungs to decrease their size (because of elasticity) and the opposing tendency of the thoracic wall to pull outward and enlarge the lungs?
atmospheric pressure
intrapulmonary pressure
intrapleural pressure
intrapleural pressure
During an allergic reaction, which of the following would aid respiration?
epinephrine
an increase in the parasympathetic nervous system
histamine
acetylcholine (ACh)
epinephrine
Yes, during an allergic reaction, there is increased resistance in the bronchioles and epinephrine dilates the bronchioles, thus making it easier to breathe. Epinephrine is released from the adrenal gland during stressful situations. People with severe allergies carry an EpiPen in case the allergic reaction produces anaphylaxis.
If the transpulmonary pressure equals zero, what will happen to the lung?
lungs will inflate
lung volume will stay the same
lungs will collapse
lungs will collapse
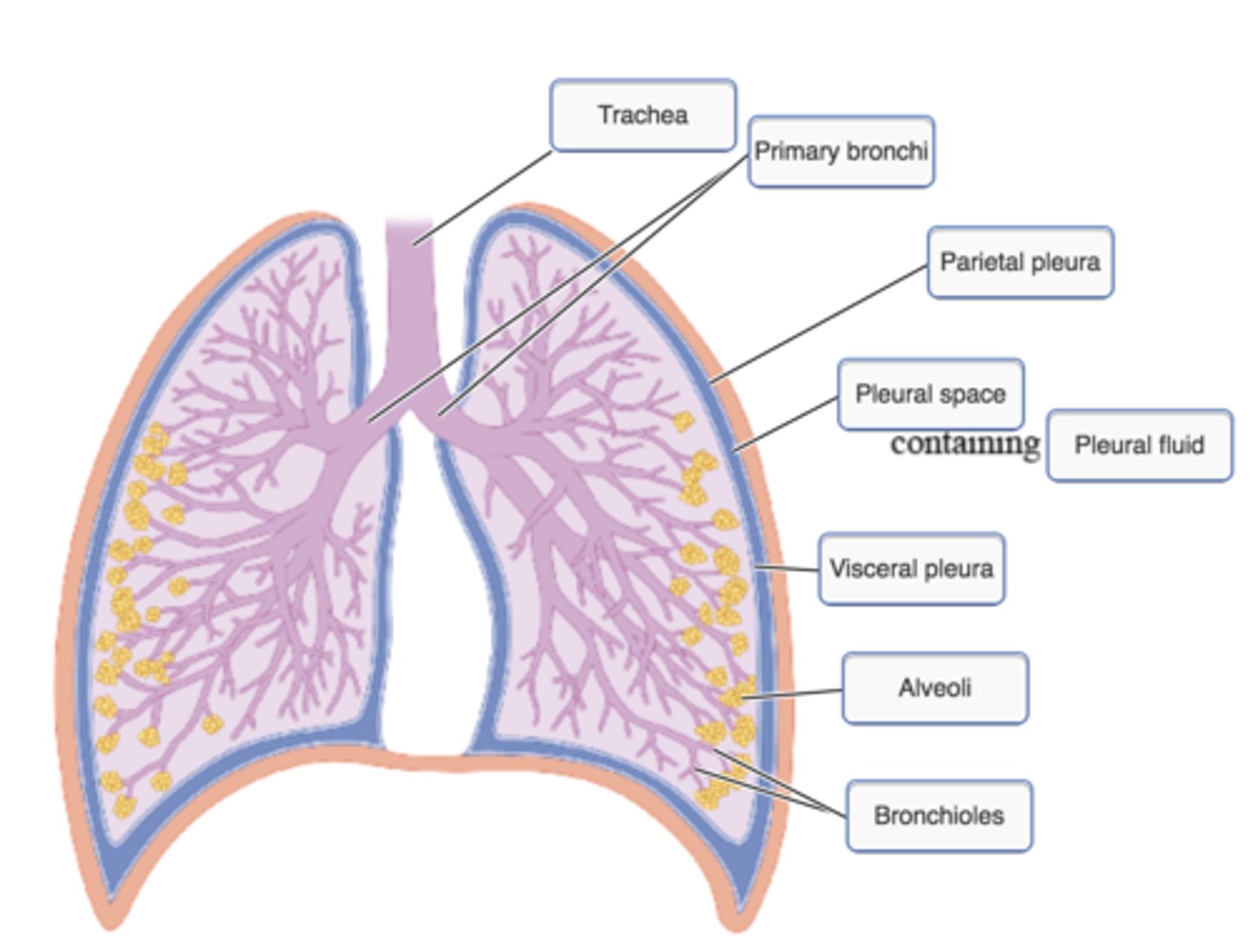
label the pleural cavity
collapsed lungs what happens
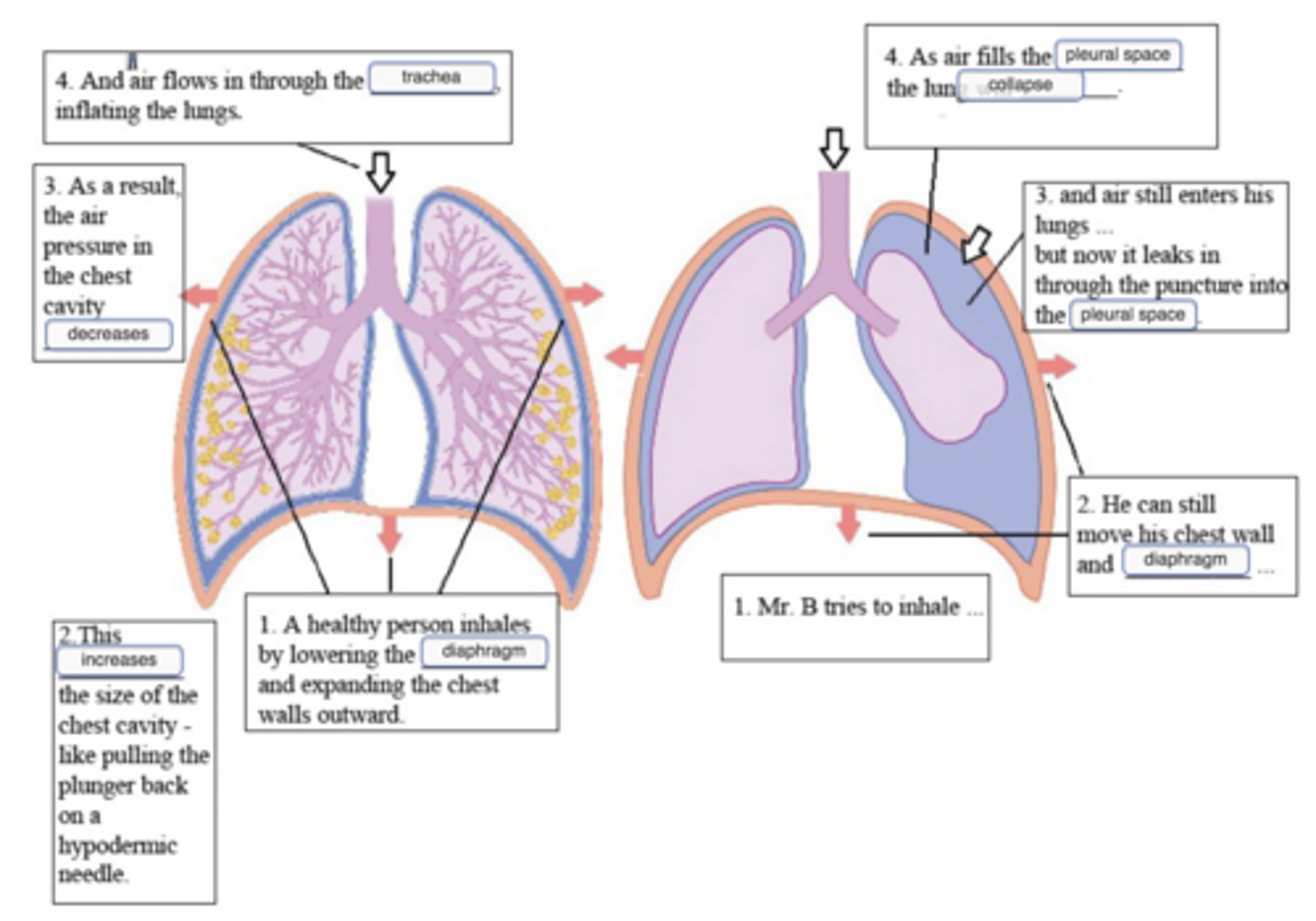
As the two of you move him into the bed, you notice that his chest tube bottle is lying on its side on the gurney, with air going into it. You see air start bubbling through the fluid right away. "They lost the water seal, and air was going into his chest from the bottle." You have trouble detecting his lung sounds on the left. His apical heart sound is in the wrong place - it is over toward the right side of his chest. "Let's give him a little oxygen."
Why would accumulation of air in his pleural space cause his heart sounds to be in the wrong place?
Because the left side of Mr. B's chest is filling up with air, the organs in his chest are being pushed over to the right.
The air in Mr. B's chest is making his heart collapse - an emergency!
Mr. B's heart has not really moved, but the air in his chest is making it sound different.
Because Mr. B's right lung collapsed, his heart moved over into the empty spac
Because the left side of Mr. B's chest is filling up with air, the organs in his chest are being pushed over to the right.
As Mr. B's left pleural cavity fills up with air, the organs in his chest will be pushed over to the right. If it gets bad enough, you will actually be able to see his trachea slanting toward the right as it runs down his neck. This condition is called a deviated mediastinum; the mediastinum is the big bundle of trachea, blood vessels, and heart that normally hangs in the center of the chest.
Choose the three best explanations for why Mrs. H's alveoli might collapse if she does not do her deep breathing with the incentive spirometer.
-The anesthesia was toxic to her lung cells, and she needs to clear it out of her alveoli as fast as she can.
-With her gall bladder removed, she cannot produce the soapy substance that lines alveoli and makes them easier to inflate.
-When she is lying down, it is harder for her to expand her chest cavity anyway.
-Shallow breathing that does not fill her lungs will only move air into the alveoli in the upper part of her lungs, letting those in the lower part stay closed.
-The alveoli are lined with water, and attraction between the water molecules pulls them together. This surface tension will pull the alveoli closed if she does not open them with deep breathing.
-Surgery stimulated her sympathetic system
When she is lying down, it is harder for her to expand her chest cavity anyway.
Shallow breathing that does not fill her lungs will only move air into the alveoli in the upper part of her lungs, letting those in the lower part stay closed.
The alveoli are lined with water, and attraction between the water molecules pulls them together. This surface tension will pull the alveoli closed if she does not open them with deep breathing.
nurses need physiology: collapsed lungs
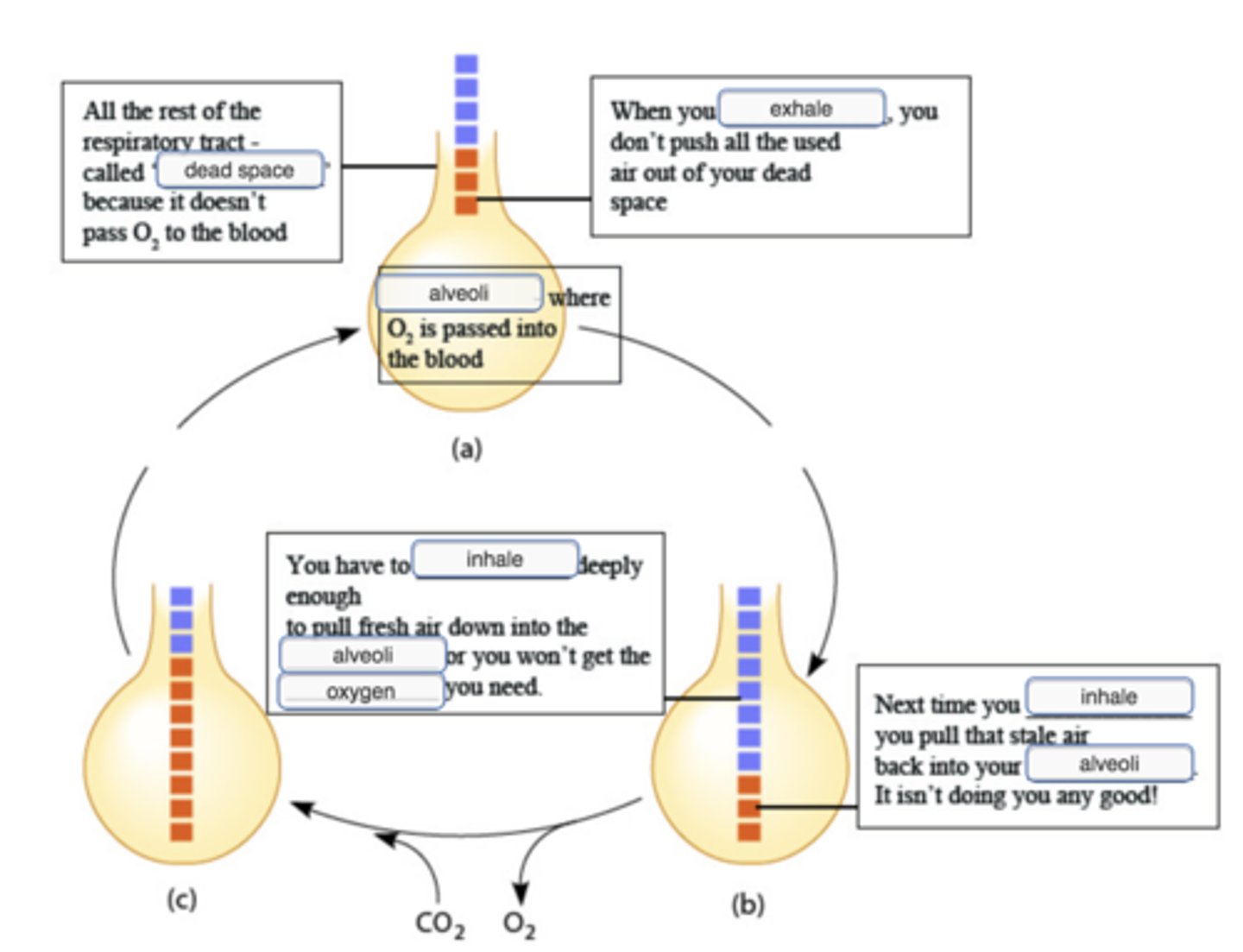
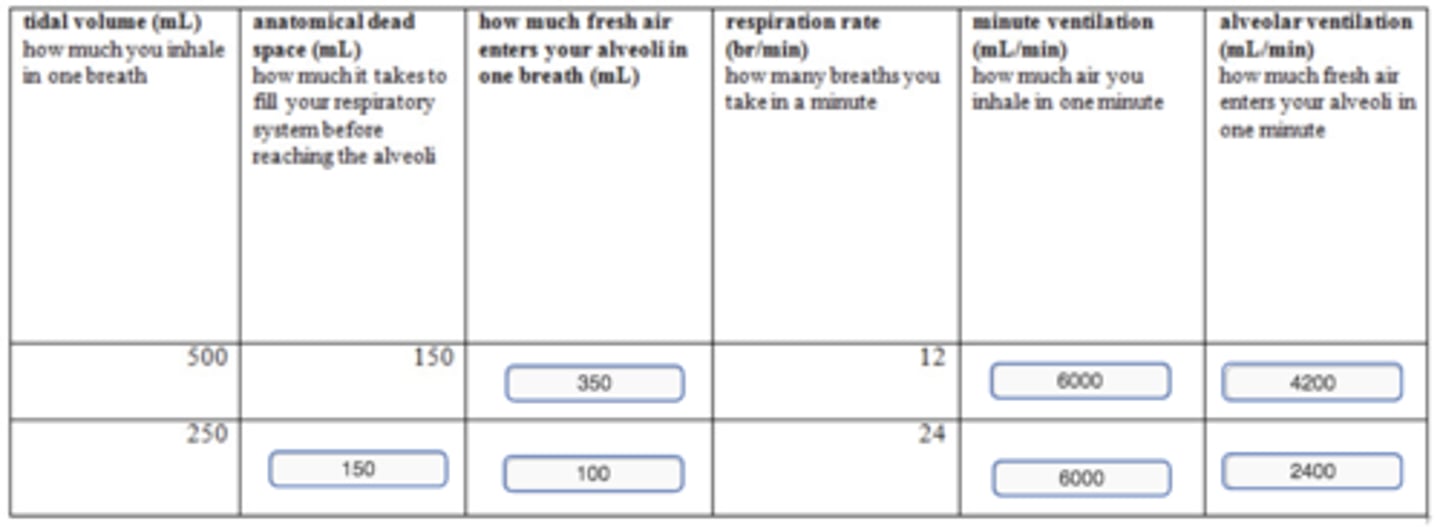
calculating alveolar ventilation
What does a surfactant do?
The alveoli are lined with water molecules, which are attracted to one another and tend to move closer together, making the alveoli collapse.
Surfactant molecules get in between the water molecules, keeping them apart.
Surfactant is the fluid between the visceral and parietal layers of the pleura, holding them together. If it were not present, when someone tried to breathe, the chest wall would move, but the lungs would not.
Surfactant is the watery fluid that keeps respiratory mucus from becoming so thick that it blocks the airway. Without it, a person would not be able to move air through the airway into the lungs, and they would collapse.
Surfactant is a slippery substance that keeps the walls of collapsed alveoli from sticking together.
The alveoli are lined with water molecules, which are attracted to one another and tend to move closer together, making the alveoli collapse.
Surfactant molecules get in between the water molecules, keeping them apart.
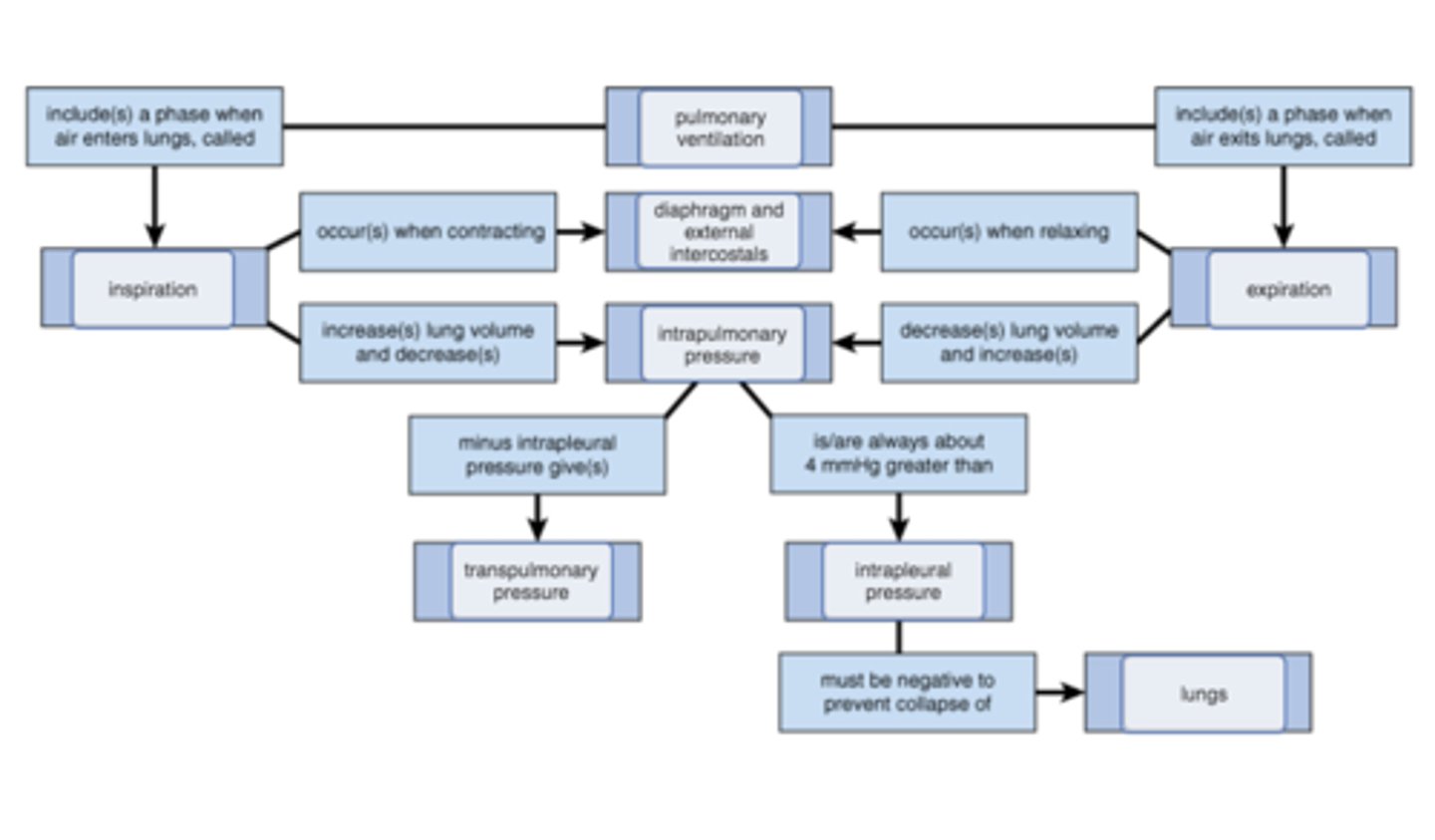
complete concept map to explain the roles of respiratory muscles and lung elasticity
Which of the following best describes how Boyle's law relates to the mechanics of breathing?
If lung volume increases, intrapleural pressure increases, forcing air out of the lungs.
If lung volume increases, intrapleural pressure decreases, drawing air into the lungs.
If lung volume decreases, intrapleural pressure increases, forcing air into the lungs.
If lung volume decreases, intrapleural pressure decreases, forcing air out of the lungs.
If lung volume increases, intrapleural pressure decreases, drawing air into the lungs.
Which of the following statements accurately describes transpulmonary pressure?
Transpulmonary pressure reflects the pressure of air surrounding the body at any given time.
Transpulmonary pressure is the pressure in the pleural cavity during breathing phases.
Transpulmonary pressure is the pressure in the alveoli during breathing phases.
Transpulmonary pressure is usually near 4 mm Hg
.
Transpulmonary pressure is usually near 4 mm Hg
Transpulmonary pressure is the difference between intrapulmonary and intrapleural pressures. Because intrapleural pressure is always about 4 mm Hgmm Hg lower than the intrapulmonary pressure, transpulmonary pressure tends to remain close to 4 mm Hgmm Hg.
Which of the following could be responsible for an increase in intrapulmonary pressure?
a decrease in lung volume
a decrease in intrapleural pressure
inspiration
an increase in lung volume
a decrease in lung volume
Which of the following would likely result in a collapsed lung?
an opening in the chest wall that allows the intrapleural pressure to equal atmospheric pressure
a decrease in intrapulmonary pressure to atmospheric pressure
an increase in transpulmonary pressure
a strong enough contraction of the diaphragm
an opening in the chest wall that allows the intrapleural pressure to equal atmospheric pressure
Complete the Concept Map to explain and compare the various lung volumes and capacities.
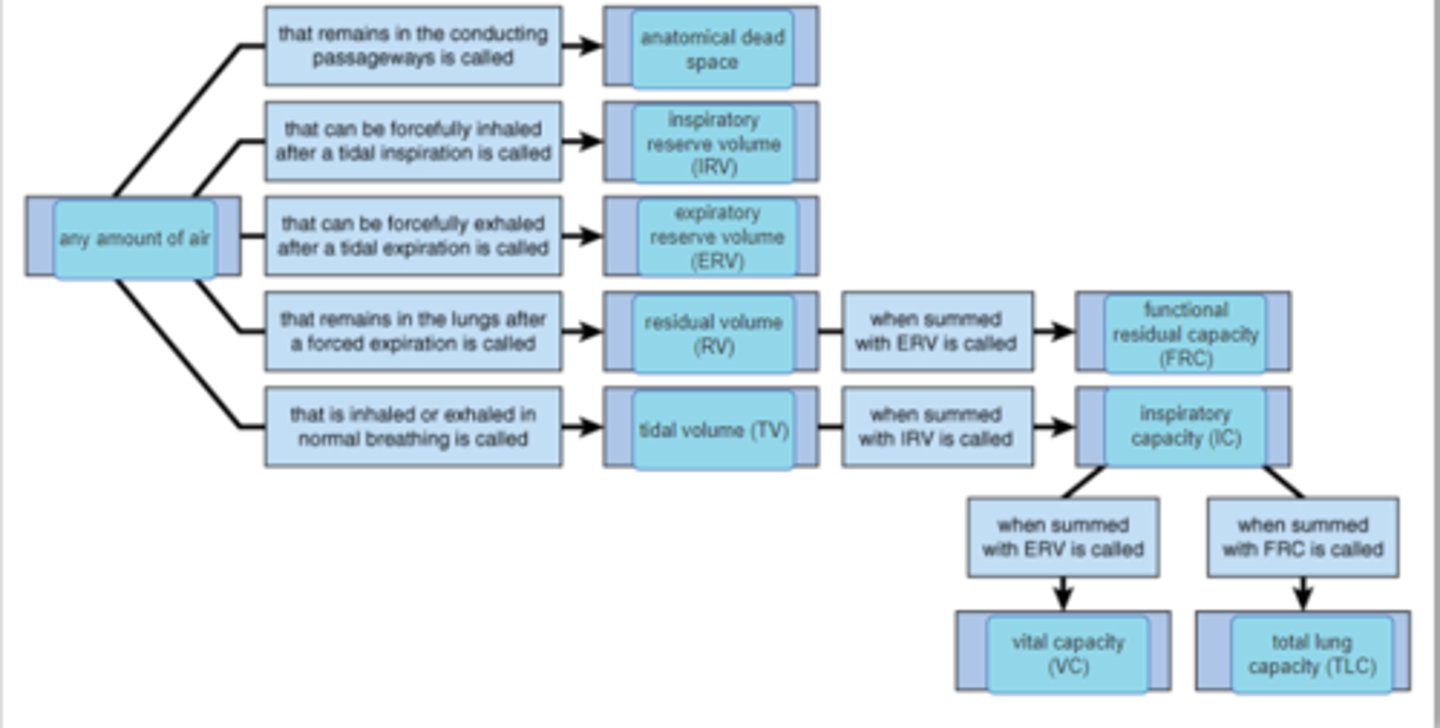
This lung volume CANNOT be directly measured using a spirometer.
residual volume
inspiratory reserve volume
tidal volume
expiratory reserve volume
residual volume
Which lung volume tends to be the largest in healthy male and female adults?
inspiratory reserve volume
tidal volume
expiratory reserve volume
residual volume
inspiratory reserve volume
A patient with a restrictive lung disease such as tuberculosis is likely to see an increase in his or her __________.
vital capacity
breathing rate
residual volume
functional residual capacity
breathing rate
Which of the following behaviors would most likely result in an increased alveolar ventilation rate as compared to that of normal breathing?
breathing rapidly into a paper bag
rapid, shallow breathing
slow, deep breathing
breathing slowly into a paper bag
slow, deep breathing
Slow breathing provides adequate time for gases to pass into the alveoli, while breathing deeply increases the number of alveoli being utilized. The combination of these factors increases effective ventilation, or alveolar ventilation rate.
functional residual capacity
- maximum amount of air that you can inhale and then exhale
- minimal lung volume that cannot be expired
- the amount of air inhaled and exhaled with each breath
- resting lung volume in which the respiratory muscles are relaxed
- the volume of air occupying the airways without alveoli
resting lung volume in which the respiratory muscles are relaxed
residual volume is :
- maximum amount of air that you can inhale and then exhale
- minimal lung volume that cannot be expired
- the amount of air inhaled and exhaled with each breath
- resting lung volume in which the respiratory muscles are relaxed
- the volume of air occupying the airways without alveoli
minimal lung volume that cannot be expired
tidal volume
-maximum amount of air that you can inhale and then exhale
- minimal lung volume that cannot be expired
- the amount of air inhaled and exhaled with each breath
- resting lung volume in which the respiratory muscles are relaxed
- the volume of air occupying the airways without alveoli
- the amount of air inhaled and exhaled with each breath
anatomical deadspace
-maximum amount of air that you can inhale and then exhale
- minimal lung volume that cannot be expired
- the amount of air inhaled and exhaled with each breath
- resting lung volume in which the respiratory muscles are relaxed
- the volume of air occupying the airways without alveoli
the volume of air occupying the airways without alveoli
vital capacity
-maximum amount of air that you can inhale and then exhale
- minimal lung volume that cannot be expired
- the amount of air inhaled and exhaled with each breath
- resting lung volume in which the respiratory muscles are relaxed
- the volume of air occupying the airways without alveoli
maximal amount of air that can be expired in one breath
Emphysema is a disease process associated with cigarette smoking. It results in the destruction of the elastic fibers in the extracellular matrix and makes the lungs floppy and not firm, impacting compliance. Alveoli are also reduced in numbers as fewer large diameter alveoli replace more numerous smaller diameter alveoli.
Functional residual capacity will increase because of greater compliance so they are breathing at a larger lung volume.
Resting tidal volume will decrease because the increase in resistance along the airways during inspiration decreases airflow.
Vital capacity will increase because lung volume increases more easily with contraction of inspiratory muscles.
Residual volume will decrease because of fewer large diameter alveoli, so that their resting lung volume actually decreases.
Functional residual capacity will increase because of greater compliance so they are breathing at a larger lung volume.
Which pressure is a result of the natural tendency of the lungs to decrease their size or recoil, which is opposed by the natural tendency of the elastic chest wall to pull outward, enlarging the lungs?
Hydrostatic pressure
Intrapulmonary pressure
Atmospheric pressure
Intrapleural pressure
Intrapleural pressure
Which volume of air within the lungs is a result of the maximal contraction of the expiratory muscles?
Functional residual capacity
Tidal volume
Residual volume
Vital capacity
Residual volume
Maximal contraction of the expiratory muscles reduces the lung volume below functional residual capacity to the residual volume. The residual volume represents the volume of air in the lungs that can not be expelled with maximal contraction of the expiratory muscles. This volume of air helps keep the airways and alveoli from collapsing.
Intrapulmonary pressure is less than atmospheric pressure and lung volume is increasing.
- lungs at rest before expiration
-expiration
-lungs at rest before inspiration
-inspiration
inspiration
Intrapulmonary pressure is equal to atmospheric pressure and lung volume is low.
- lungs at rest before expiration
-expiration
-lungs at rest before inspiration
-inspiration
Lungs at rest before inspiration
Intrapulmonary pressure is equal to atmospheric pressure and lung volume is high.
- lungs at rest before expiration
-expiration
-lungs at rest before inspiration
-inspiration
lungs at rest before expiration
Intrapulmonary pressure is greater than atmospheric pressure and lung volume is decreasing
- lungs at rest before expiration
-expiration
-lungs at rest before inspiration
-inspiration
expiration
Makes ventilating the alveoli harder because the alveoli tend to collapse as occurs with respiratory distress syndrome.
-increased surface tension
-increased compliance
-decreased surface tension
- decreased compliance
-decreased resistance
- increased resistance
-increased surface tension
Makes breathing easier because lungs will easily stretch with the expansion of the thoracic wall during inspiration.
-increased surface tension
-increased compliance
-decreased surface tension
- decreased compliance
-decreased resistance
- increased resistance
increased compliance
Makes inflating the alveoli easier because the alveoli will open more easily with inspiration.
-increased surface tension
-increased compliance
-decreased surface tension
- decreased compliance
-decreased resistance
- increased resistance
decreased surface tension
Requires increased breathing effort during inspiration because the lungs will not stretch as easily, as occurs with pulmonary fibrosis.
-increased surface tension
-increased compliance
-decreased surface tension
- decreased compliance
-decreased resistance
- increased resistance
decreased compliance
: Increases air flow to the alveoli because air can flow easily through the airways, as occurs with exercise and the release of epinephrine.
-increased surface tension
-increased compliance
-decreased surface tension
- decreased compliance
-decreased resistance
- increased resistance
decreased resistance
Decreases air flow to the alveoli because it's harder for the air to flow through the airways, as occurs with the release of acetylcholine or histamine.
-increased surface tension
-increased compliance
-decreased surface tension
- decreased compliance
-decreased resistance
- increased resistance
increased resistance
_______ has a greater partial pressure in the pulmonary capillaries than in the alveoli, so it diffuses into the _______.
View Available Hint(s)for Part A
O2; pulmonary cavities
CO2; alveoli
O2; alveoli
CO2; pulmonary capillaries
CO2; alveoli
Yes, CO2CO2 diffuses along its partial pressure gradient from the pulmonary capillaries into the alveoli until equilibrium is reached.
Despite the fact that the partial pressure difference is so much smaller for CO2
, why is there as much CO2
exchanged between the alveoli and blood as there is O2
, ?
The capillary walls are more permeable to CO2 than O2
.
CO2
is a smaller molecule and diffuses faster than O2
.
CO2
is much more soluble in blood than O2
.
CO2
is much more soluble in blood than O2
Yes, because CO2CO2 is very soluble in blood, it does not require as large a pressure gradient as O2O2.
How would the partial pressures of O2
and CO2
change in an exercising muscle?
The partial pressures of O2
and CO2
would remain unchanged.
The partial pressure of O2
would decrease, and the partial pressure of CO2
would increase.
The partial pressure of O2
would increase, and the partial pressure of CO2
would decrease.
The partial pressure of O2
would decrease, and the partial pressure of CO2 would increase
Yes, cells use O2O2 and produce CO2CO2 during cellular respiration to produce ATP. Exercising muscles need more ATP.
Which way would O2
and CO2
diffuse during internal respiration?
O2
would diffuse into the pulmonary capillaries and CO2
would diffuse into the alveoli.
O2
would diffuse into the cells, and CO2
would diffuse into the systemic capillaries.
O2
would diffuse into the systemic capillaries, and CO2
would diffuse into the cells.
Both O2
and CO2
would diffuse into the systemic capillaries.
O2
would diffuse into the cells, and CO2
would diffuse into the systemic capillaries.
Yes, the PO2PO2 would be higher in the systemic capillaries, and the PCO2PCO2 would be higher in the tissues.
Internal and external respiration depends on several factors. Which of the following is NOT an important factor in gas exchange?
the molecular weight of the gas
rate of blood flow through the tissue
partial pressure of the gases
available surface area
the molecular weight of the gas
Yes, molecular weight is not an important factor in gas exchange.
Which statement is correct?
During external respiration, oxygen is unloaded from the blood.
During external respiration, equilibrium is reached for O2
when the partial pressure for O2
in the pulmonary capillaries and the alveoli are the same.
The greater the available surface area the lower the amount of gas exchange during internal respiration.
During internal respiration, carbon dioxide is unloaded from the blood.
During external respiration, equilibrium is reached for O2
when the partial pressure for O2
in the pulmonary capillaries and the alveoli are the same.
Yes, equilibrium is reached for O2O2 when the partial pressure of O2O2 in the pulmonary capillaries and the tissue cells are the same.
Which of the following represents a correct statement about data presented in the graph?
A. In blood with 60% oxygen saturation of hemoglobin, each individual hemoglobin binds ~2.5 oxygens.
B. In blood with 30% oxygen saturation of hemoglobin, there is a PO2PO2 of ~60 mm Hg in surrounding fluid.
C. In blood with a PO2PO2 of 30 mm Hg, the average saturation of all hemoglobin proteins is 60%.
D. Blood with three oxygens per hemoglobin represents a saturation of PO2PO2 at ~30 mm Hg.
C. In blood with a PO2PO2 of 30 mm Hg, the average saturation of all hemoglobin proteins is 60%.
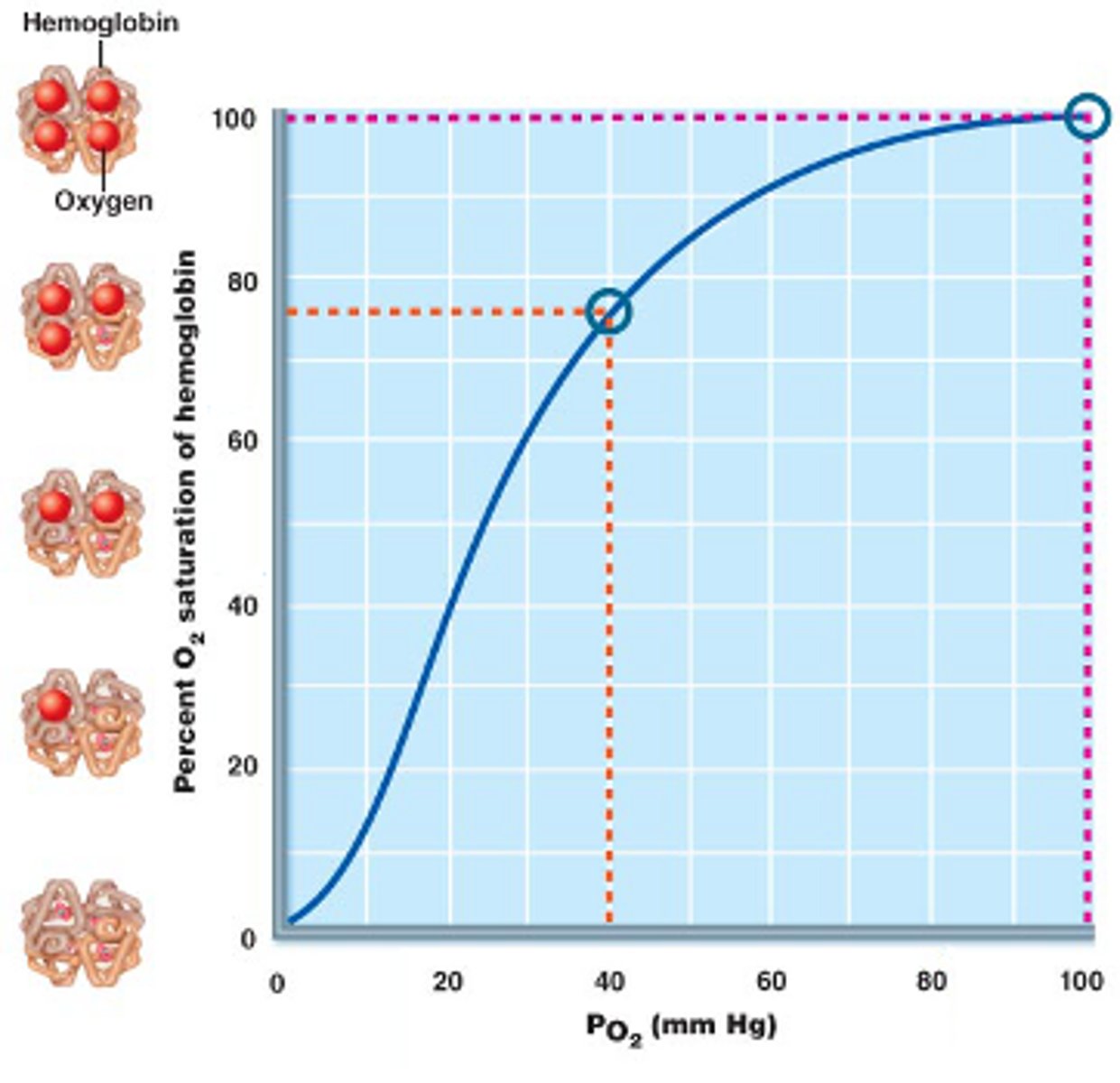
Using the same graph as in Part A, what is the average number of oxygens bound to hemoglobin at a saturation of 50%?
four
one
three
two
two
Using the graph in Part A as reference, drag the correct value item of PO2PO2 mm Hg to the correct target molecule of hemoglobin. Remember that the y-axis indicates how much O2 is bound to hemoglobin.
PO2 0 mm Hg: No bound O2
PO2 15 mm Hg: One bound O2
PO2 25 mm Hg: Two bound O2
PO2 40 mm Hg: Three bound O2
PO2 100 mm Hg: Four bound O2
Part D - Hemoglobin Saturation in the Lungs
Focus your attention on the graph shown, from the top right box, "In the lungs," of the Focus Figure.
Drag and drop the numerical terms to the appropriate blank target locations in the sentences.
The PO2 in the lungs at sea level is PO2 of ~100 mm Hg.
The saturation of hemoglobin in the lungs at sea level is ~98 O2 saturation at PO2 ~100 mm Hg.
The saturation of hemoglobin in the lungs at high altitude of PO2 ~80 mm Hg is ~95% O2 saturation.
The saturation of hemoglobin in the lungs at an altitude representing PO2 ~60 mm Hg is closest to ~90% O2 saturation.
The PO2 in the lungs at high altitude is PO2 of ~80 mm Hg.
Part E - Comparison of Oxygen Binding in Resting and Metabolic Tissue
Focus your attention on the graph shown, from the lower right box, "In the tissues," of the Focus Figure.
Sort the correct pressures into the appropriate bins that represent tissue descriptions. Each bin should contain a value for PO2 and a value for Hb.
answer in image:
Resting Tissue = PO2 ~40 mm Hg, Hb ~75% O2 saturation
Metabolically Active tissue = PO2 ~20 mm Hg, Hb ~40% O2 saturation
Neither = PO2 ~30 mm Hg, Hb ~50% O2 saturation
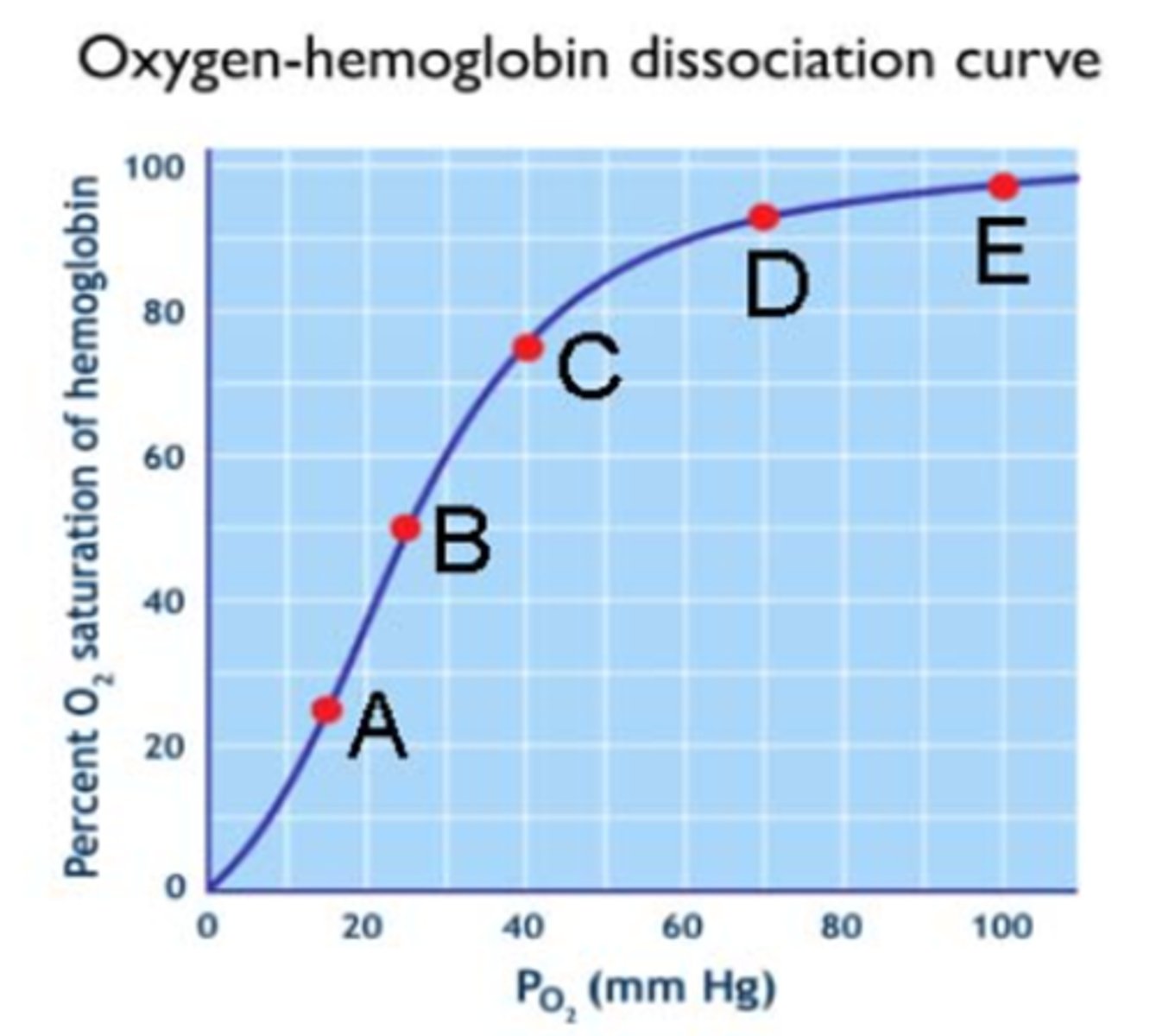
A firefighter breathes in air normally as he enters a building following an explosion and fire. He has a meter that predicts the PO2
will approximate 15 mm Hg in his tissue fluids as he actively moves about the room.
Select the best statement.
The firefighter is at about 10% hemoglobin O2
saturation, and he requires an external air tank.
The large changes in PO2
tissue environments cause only very small changes in hemoglobin O2
saturation, and no oxygen is needed.
The S-shaped saturation curve of hemoglobin is flat at this PO2
, and O2
saturation doesn't change much with PO2
changes in mm Hg.
The firefighter's hemoglobin saturation will be about one oxygen per hemoglobin, and he will require an external air tank.
The firefighter's hemoglobin saturation will be about one oxygen per hemoglobin, and he will require an external air tank.
Which of the following statements correctly describes the diffusion of oxygen during pulmonary gas exchange?
PO2
is greater in the alveolus than the blood, so oxygen diffuses into the blood.
PO2
is greater in the blood than the body tissues, so oxygen diffuses into the body tissues.
PO2
is greater in the blood than the alveolus, so oxygen diffuses into the alveolus.
PO2
is greater in the body tissues than the blood, so oxygen diffuses into the blood.
PO2 is greater in the alveolus than the blood, so oxygen diffuses into the blood.
PO2
Which of the following would occur if lung cancer restricts the airflow to a group of alveoli?
The PO2
in the affected alveoli would increase, and their arterioles would vasodilate.
The PO2
in the affected alveoli would decrease, and their arterioles would vasoconstrict.
The PO2
in the affected alveoli would decrease, and their arterioles would vasodilate.
The PO2
in the affected alveoli would increase, and their arterioles would vasoconstrict.
The PO2
in the affected alveoli would decrease, and their arterioles would vasoconstrict.
Correct
A restriction in airflow would decrease the PO2PO2 in the affected alveoli, which would cause nearby arterioles to vasoconstrict. As a result, the affected alveoli would receive less blood, and blood would flow preferentially to better-ventilated alveoli with a higher PO2PO2.
Using the figure below match the location of the oxygen-hemoglobin dissociation curve to the correct statement regarding percentage of oxygen saturation of hemoglobin.
A. Point showing the percent oxygen saturation of hemoglobin in the venous blood leaving a vigorously exercising muscle. Most of the hemoglobin in this blood is in the form of deoxyhemoglobin.
B. Point showing a relatively equal ratio of oxyhemoglobin and deoxyhemoglobin in the blood.
C. Point showing the percentage oxygen saturation hemoglobin in the venous blood leaving the resting muscle.
D. Point showing the percent oxygen saturation of hemoglobin in the blood leaving the lungs of a person at moderately high altitude.
E. Point showing the percent oxygen saturation of hemoglobin in blood leaving the lungs at sea level.
Arrange these events related to oxygen transport and exchange in sequence from earliest (at the lungs) to latest (at the body tissues).
1.Oxygen diffuses from alveoli into plasma. 2. Oxygen diffuses rom plasma into red blood cells. 3. Oxygen is loaded onto hemoglobin, forming oxyhemoglobin. 4. Oxygen is transported from the pulmonary circulation to the systemic circulation. 5. Oxygen is unloaded from hemoglobin, forming deoxyhemoglobin. 6. Oxygen diffuses from red blood cells into the plasma. 7. Oxygen diffuses from the plasma into body tissues.
Drag the factors to their respective locations (bins) to indicate whether they would tend to increase or decrease oxygen loading or unloading.
Increased Loading:
Increased surface area of respiratory membrane
Increased PO2 in the alveoli
Decreased Loading"
Increased thickness of the respiratory membrane
Decreased atmospheric pressure
Decreased ventilation of alveoli
Increased Unloading:
Increased PCO2in the tissues
Decreased PO2in the tissues
Decreased pH in the tissues
Decreased Unloading:
Decreased temperature in the tissues
Decreased concentration of BPG
Which of the following statements correctly describes the diffusion of carbon dioxide during tissue gas exchange?
PCO2 is greater in the blood of pulmonary capillaries than in the alveoli, so carbon dioxide diffuses into the alveoli.
PCO2 is greater in the blood of systemic capillaries entering tissues than in the tissue cells, so carbon dioxide diffuses into the tissue cells.
PCO2 is greater in the alveoli than in the blood of pulmonary capillaries, so carbon dioxide diffuses into the blood. PCO2 is greater in the tissue cells than in the blood of systemic capillaries entering tissues, so carbon dioxide diffuses into the blood.
PCO2 is greater in the tissue cells than in the blood of systemic capillaries entering tissues, so carbon dioxide diffuses into the blood.
During tissue gas exchange, carbon dioxide will diffuse down its partial pressure gradient from body tissues into the blood until the partial pressure is equal in both locations.
Select the statement that is TRUE comparing oxygen exchange and carbon dioxide transport and exchange at body tissues.
The partial pressure gradient is greater for oxygen than for carbon dioxide. However, carbon dioxide is more soluble in blood plasma, allowing for a large diffusion of carbon dioxide at body tissues.
The partial pressure gradient is greater for carbon dioxide than for oxygen. However, oxygen is more soluble in blood plasma, allowing for a large diffusion of oxygen at body tissues.
The partial pressure gradient is greater for oxygen than for carbon dioxide, and oxygen is more soluble in blood plasma, allowing for a large diffusion of oxygen at body tissues.
The partial pressure gradient is greater for carbon dioxide than for oxygen, and carbon dioxide is more soluble in blood plasma, allowing for a large diffusion of carbon dioxide at body tissues.
The partial pressure gradient is greater for oxygen than for carbon dioxide. However, carbon dioxide is more soluble in blood plasma, allowing for a large diffusion of carbon dioxide at body tissues.
What is the purpose of the chloride shift
The chloride shift helps maintain electrical neutrality as bicarbonate ions move out of red blood cells.
The chloride shift helps maintain electrical neutrality by increasing the formation of carbonic acid.
The chloride shift helps maintain electrical neutrality by increasing the formation of carbaminohemoglobin.
The chloride shift helps maintain electrical neutrality as hydrogen ions move out of red blood cells.
The chloride shift helps maintain electrical neutrality as bicarbonate ions move out of red blood cells.
enzyme that catalyzes the formation of carbonic acid inside red blood cells.
carbonic anhydrase
: forms from the dissociation of carbonic acid.
bicarbonate ions and hydrogen ions
responsible for approximately 20% of the transport of carbon dioxide in the blood.
carbaminohemoglobin
enters red blood cells with the movement of bicarbonate ions out of red blood cells.
chloride ions
: molecules that combine in red blood cells, forming carbonic acid.
carbon dioxide and water
: most important means of transporting carbon dioxide in the blood plasma, responsible for approximately 70%
bicarbonate ions
buffered by hemoglobin in the red blood cell, preventing a change in pH.
hydrogen ions
initially formed when carbon dioxide combines with water.
carbonic acid
: responsible for approximately 7-10% of the transport of carbon dioxide in the blood plasma.
dissolved carbon dioxide
tissue co2 effect
bohr effect
hemoglobin binds to CO2
PCO2 increases in the blood
chloride ion moves into red blood cell in exchange for bicarbonate ion
CO2 diffuses into the blood
carbonic anhydrase catalyzes the formation of carbonic acid
pulmonary co2 exchange
haldane effect
hemoglobin releases co2
pco2 decreases in the blood plasma
hemoglobin releases co2
chloride ion moves out of red blood cell in exchange for bicarbonate ion
co2 diffuses out of the blood
carbonic anhydrase catalyzes the breakdown of carbonic aicd
What area in the brain sets the respiratory rhythm?
dorsal respiratory group (DRG)
hypothalamus
ventral respiratory group (VRG)
pontine respiratory group (PRG)
ventral respiratory group (VRG)
Inspiratory neurons send information to the diaphragm via what nerve?
glossopharyngeal nerve
intercostal nerves
phrenic nerve
vagus nerve
phrenic nerve
What directly stimulates the central chemoreceptors, thus increasing respiration?
H+ (hydrogen ions)
high pH
low O2 (oxygen)
high CO2 (carbon dioxide)
H+ (hydrogen ions)
Yes, hydrogen ions (H+) stimulate the central chemoreceptors. CO2 is converted to H+ in the extracellular fluid of the brain.
As a result of hyperventilation, what will happen to the partial pressures of CO2 (pCO2) and pH?
increased pCO2 and decreased pH
increased pCO2 and increased pH
decreased pCO2 and decreased pH
decreased pCO2 and increased pH
decreased pCO2 and increased pH
Yes, pCO2 would decrease and pH would increase. As CO2 is blown off, H+ would decrease, thus increasing pH.
Which receptors inhibit inspiration during hyperinflation of the lungs?
pulmonary stretch receptors
peripheral chemoreceptors
irritant receptors
Hypothalamic receptors
pulmonary stretch receptors
What stimulates increased respiration at the beginning of exercise?
increased hydrogen ion levels
decreased plasma oxygen levels
increased plasma carbon dioxide levels
sensory input from receptors in joints, neural input from the motor cortex, and other factors
sensory input from receptors in joints, neural input from the motor cortex, and other factors
Yes, at the beginning of exercise, blood gases have not changed; thus, other factors such as anticipation of exercise contribute to the increase in respiration.
A homeostatic control mechanism controls respiration. What acts as the effector(s) in this system?
peripheral chemoreceptors
medulla oblongata
respiratory muscles
central chemoreceptors
respiratory muscles
Yes, the respiratory muscles change the volume of the thoracic cavity (and thus the pressure), resulting in inspiration and expiration.
Emphysema is a disease process that can be caused by cigarette smoking. Not only are the lungs more inflated at rest due to loss of elasticity (elastic recoil), but the alveoli are also reduced in numbers as fewer, large diameter alveoli replace more numerous, smaller diameter alveoli. As a consequence, patients with emphysema are often given supplemental oxygen to assist with their changed breathing pattern. What is the main objective in administering supplemental oxygen?
Increase the PO2
in the alveoli to decrease the alveolar PCO2
.
Increase the PO2
of pulmonary blood above 100 mm Hg so that more oxygen can be carried by hemoglobin.
Increase the PO2
in the alveoli to increase the diffusion of oxygen across the respiratory membrane.
Increase the PO2
of pulmonary blood above 100 mm Hg so that more oxygen can be carried as dissolved oxygen in the plasma.
Increase the PO2
in the alveoli to increase the diffusion of oxygen across the respiratory membrane.
Increase the PO2
Emphysema affects both the ventilation of alveoli and the surface area of the alveoli available for pulmonary gas exchange. Consequently, both the PO2PO2 of the alveoli and the total surface area available for oxygen diffusion will be reduced. Supplemental oxygen increases the PO2PO2 of the inhaled air, which in turn raises the PO2PO2 in the alveoli. This should compensate for the reduced ventilation and decreased surface area of the alveoli. The goal is to raise the pulmonary capillary PO2PO2 enough to achieve a hemoglobin saturation of at least 95%.
Emphysema is a disease process that causes the lungs to be more inflated at rest due to loss of elasticity, or elastic recoil. The alveoli are reduced in number as well because fewer, large-diameter alveoli replace more numerous, smaller-diameter alveoli. As a consequence, patients with emphysema are often given supplemental oxygen to assist with their changed breathing pattern. Although this treatment helps increase oxygen in the blood, how would it affect the transport and exchange of carbon dioxide in the blood?
Treatment with supplemental oxygen will dilute the concentration of CO2
in the alveoli, and the decreased alveolar PCO2
will increase the removal of CO2
from the blood. This is similar to hyperventilation.
Even with supplemental oxygen, overinflated lungs will still retain CO2
, and the increased alveolar PCO2
will slow the diffusion of carbon dioxide from the blood. This is similar to rebr
Even with supplemental oxygen, overinflated lungs will still retain CO2
, and the increased alveolar PCO2
will slow the diffusion of carbon dioxide from the blood. This is similar to rebreathing from a paper bag.